Relationship between the Superior Attachment of the Uncinate Process and Pneumatization of the Middle Turbinate—A Radiological Study
Abstract
:1. Introduction
2. Methods
2.1. Data Source
2.2. Image Study
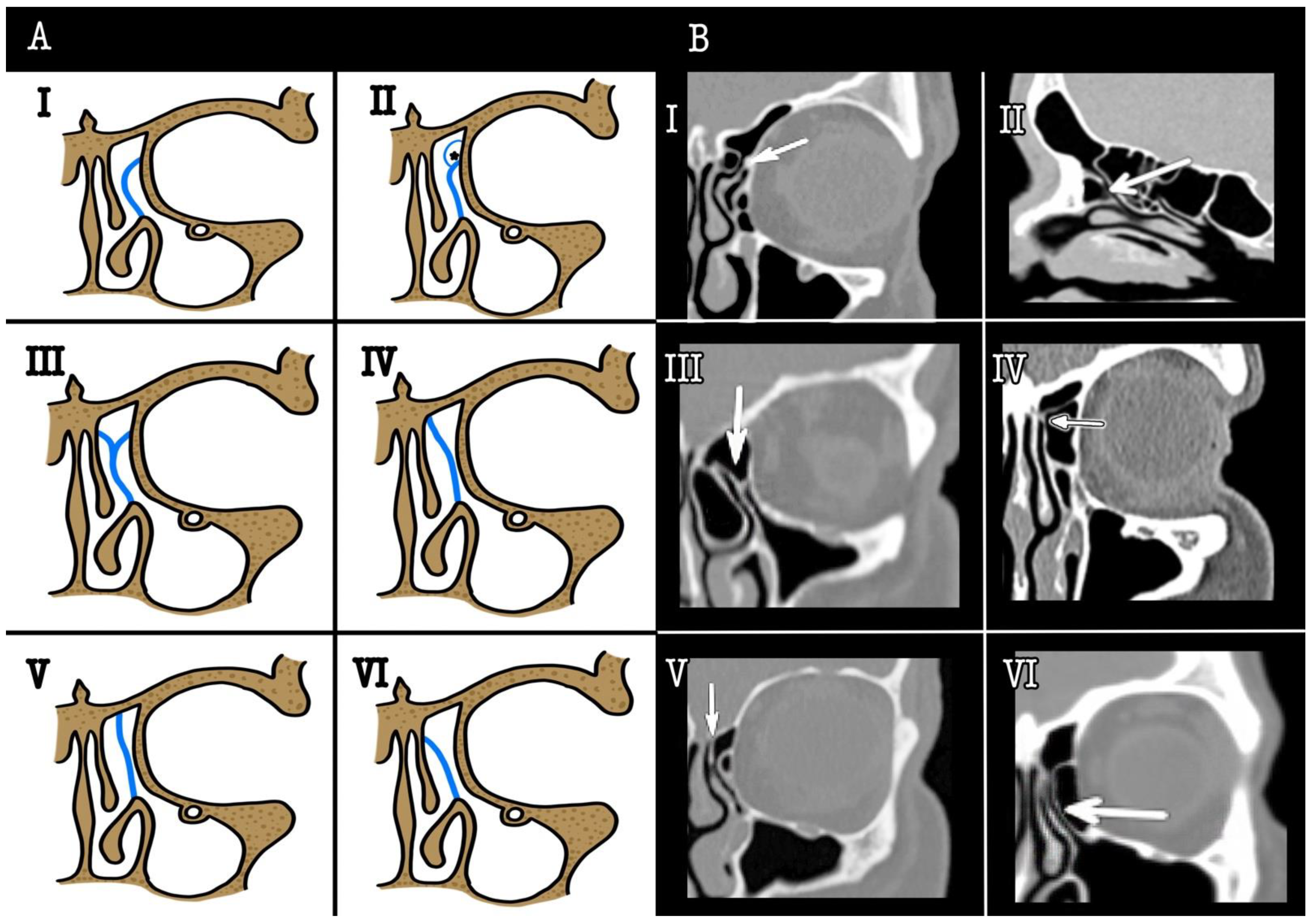
2.3. Concha Bullosa Classification
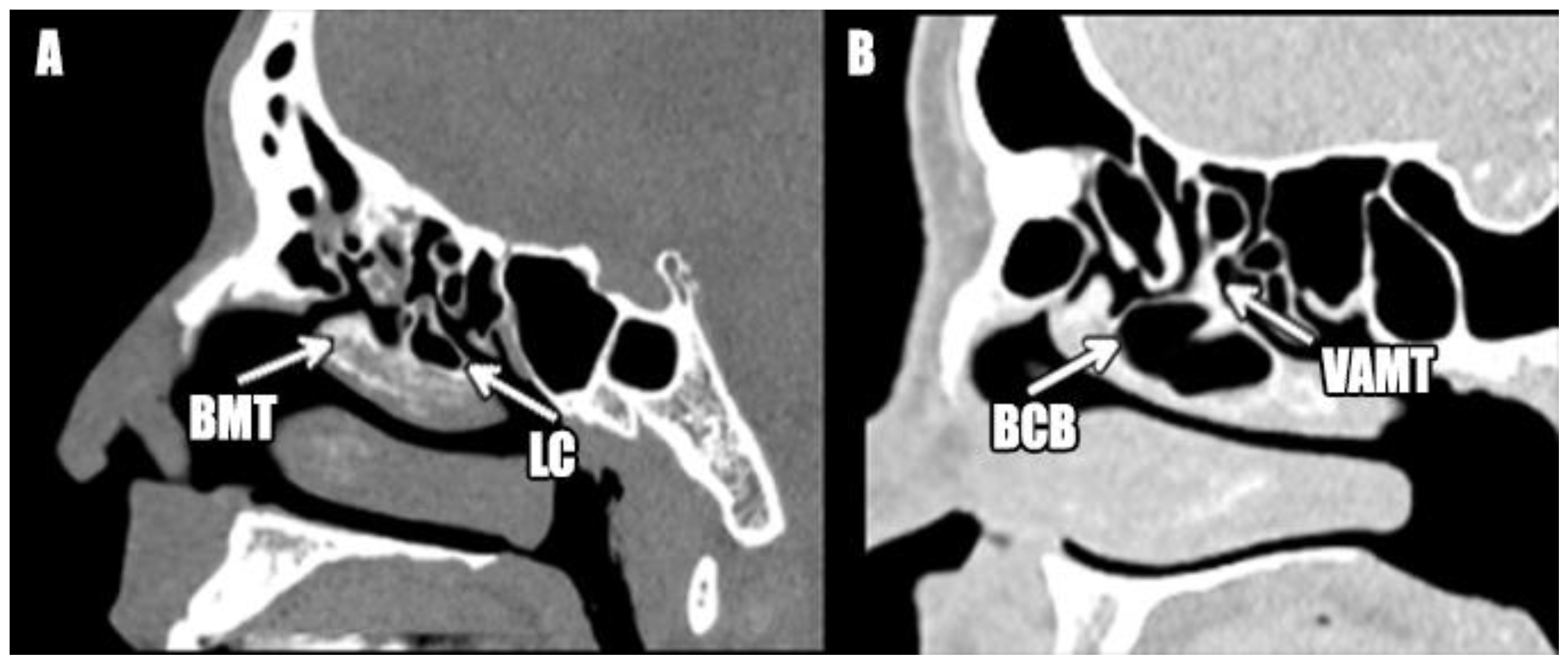
2.4. Lamellar Cell Classification
2.5. Statistical Analysis
2.6. IRB Approval
3. Results
3.1. Participants
3.2. SAUP Type Prevalencez
3.3. SAUP and Lamellar Cell
3.4. SAUP and Concha Bullosa
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nayak, D.R.; Balakrishnan, R.; Murty, K.D. Functional anatomy of the uncinate process and its role in endoscopic sinus surgery. Indian J. Otolaryngol. Head Neck Surg. Off. Publ. Assoc. Otolaryngol. India 2001, 53, 27–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fombeur, J.P.; Koubbi, G.; Seguin, D.; Ebbo, D.; Lecomte, F.; Laurier, J.N. Indications, technics and results of middle meatotomy. Apropos of 94 cases. Ann. Oto-Laryngol. Chir. Cervico Faciale Bull. Soc. Oto-Laryngol. Hopitaux Paris 1989, 106, 515–517. [Google Scholar]
- Friedman, M.; Landsberg, R.; Schults, R.A.; Tanyeri, H.; Caldarelli, D.D. Frontal sinus surgery: Endoscopic technique and preliminary results. Am. J. Rhinol. 2000, 14, 393–403. [Google Scholar] [CrossRef] [PubMed]
- Landsberg, R.; Friedman, M. A computer-assisted anatomical study of the nasofrontal region. Laryngoscope 2001, 111, 2125–2130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mahmutoğlu, A.S.; Çelebi, I.; Akdana, B.; Bankaoğlu, M.; Çakmakçi, E.; Çelikoyar, M.M.; Başak, M. Computed tomographic analysis of frontal sinus drainage pathway variations and frontal rhinosinusitis. J. Craniofac. Surg. 2015, 26, 87–90. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.-C.; Wang, C.-H.; Wang, H.-W. Prevalence of the uncinate process, agger nasi cell and their relationship in a Taiwanese population. Rhinology 2010, 48, 239–244. [Google Scholar] [CrossRef]
- Zhang, L.; Han, D.; Ge, W.; Xian, J.; Zhou, B.; Fan, E.; Liu, Z.; He, F. Anatomical and computed tomographic analysis of the interaction between the uncinate process and the agger nasi cell. Acta Otolaryngol. 2006, 126, 845–852. [Google Scholar] [CrossRef]
- Orlandi, R.R.; Kennedy, D.W. Revision endoscopic frontal sinus surgery. Otolaryngol. Clin. N. Am. 2001, 34, 77–90. [Google Scholar] [CrossRef]
- Kirtane, M.V.; Gautham, K.; Upadhyaya, S.R. Endoscopic CSF rhinorrhea closure: Our experience in 267 cases. Otolaryngol. Head Neck Surg. Off. J. Am. Acad. Otolaryngol.-Head Neck Surg. 2005, 132, 208–212. [Google Scholar] [CrossRef]
- Turgut, S.; Ercan, I.; Sayin, I.; Başak, M. The relationship between frontal sinusitis and localization of the frontal sinus outflow tract: A computer-assisted anatomical and clinical study. Arch. Otolaryngol. Head Neck Surg. 2005, 131, 518–522. [Google Scholar] [CrossRef] [Green Version]
- Cheng, S.-Y.; Yang, C.-J.; Lee, C.-H.; Liu, S.-C.; Kuo, C.-Y.; Lee, J.-C.; Shih, C.-P. The association of superior attachment of uncinate process with pneumatization of middle turbinate: A computed tomographic analysis. Eur. Arch. Oto-Rhino-Laryngol Off. J. Eur. Fed. Oto-Rhino-Laryngol Soc. EUFOS Affil. Ger. Soc. Oto-Rhino-Laryngol-Head Neck Surg. 2017, 274, 1905–1910. [Google Scholar] [CrossRef] [PubMed]
- Calvo-Henríquez, C.; Mota-Rojas, X.; Ruano-Ravina, A.; Martinez-Capoccioni, G.; Lattomus, K.; Martin-Martin, C. Concha bullosa. A radiological study and a new classification. Acta Otorrinolaringol. Esp. 2019, 70, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Calvo-Henríquez, C.; Ruano-Ravina, A.; Martinez-Capoccioni, G.; Huaranca, M.; Lattomus, K.; Martin-Martin, C. The lamellar cell: A radiological study and a new classification proposal. Eur. Arch. Oto-Rhino-Laryngol Off. J. Eur. Fed. Oto-Rhino-Laryngol Soc. EUFOS Affil. Ger. Soc. Oto-Rhino-Laryngol-Head Neck Surg. 2018, 275, 2713–2717. [Google Scholar] [CrossRef] [PubMed]
- Close, L.G.; Stewart, M.G. Looking around the corner: A review of the past 100 years of frontal sinusitis treatment. Laryngoscope 2009, 119, 2293–2298. [Google Scholar] [CrossRef]
- Daniels, D.L.; Mafee, M.F.; Smith, M.M.; Smith, T.L.; Naidich, T.P.; Brown, W.D.; Bolger, W.E.; Mark, L.P.; Ulmer, J.L.; Hacein-Bey, L.; et al. The frontal sinus drainage pathway and related structures. AJNR Am. J. Neuroradiol. 2003, 24, 1618–1627. [Google Scholar] [PubMed]
- McLaughlin, R.B.; Rehl, R.M.; Lanza, D.C. Clinically relevant frontal sinus anatomy and physiology. Otolaryngol. Clin. N. Am. 2001, 34, 1–22. [Google Scholar] [CrossRef]
- Lund, V.J.; Stammberger, H.; Fokkens, W.J.; Beale, T.; Bernal-Sprekelsen, M.; Eloy, P.; Georgalas, C.; Gerstenberger, C.; Hellings, P.; Herman, P.; et al. European position paper on the anatomical terminology of the internal nose and paranasal sinuses. Rhinol. Suppl. 2014, 24, 1–34. [Google Scholar]
- Hatipoğlu, H.G.; Cetin, M.A.; Yüksel, E. Concha bullosa types: Their relationship with sinusitis, ostiomeatal and frontal recess disease. Diagn. Interv. Radiol. Ank. Turk. 2005, 11, 145–149. [Google Scholar]
- Balikci, H.H.; Gurdal, M.M.; Celebi, S.; Ozbay, I.; Karakas, M. Relationships among concha bullosa, nasal septal deviation, and sinusitis: Retrospective analysis of 296 cases. Ear Nose Throat J. 2016, 95, 487–491. [Google Scholar] [CrossRef] [Green Version]
- Al-Qudah, M.; Mardini, D. Computed tomographic analysis of frontal recess cells in pediatric patients. Am. J. Rhinol. Allergy 2015, 29, 425–429. [Google Scholar] [CrossRef]
- Yang, Q.-T.; Shi, J.-B.; Kang, Z.; Chen, H.-X.; Wang, T.; Lü, J.-T.; Xu, G. Computer-assisted anatomical study of nasofrontal region. Zhonghua Er Bi Yan Hou Ke Za Zhi 2004, 39, 349–352. [Google Scholar] [PubMed]
- Han, D.; Zhang, L.; Ge, W.; Tao, J.; Xian, J.; Zhou, B. Multiplanar computed tomographic analysis of the frontal recess region in Chinese subjects without frontal sinus disease symptoms. ORL J. Oto-Rhino-Laryngol Its Relat. Spec. 2008, 70, 104–112. [Google Scholar] [CrossRef] [PubMed]
- Srivastava, M.; Tyagi, S. Role of Anatomic variations of Uncinate Process in Frontal Sinusitis. Indian J. Otolaryngol. Head Neck Surg. Off. Publ. Assoc. Otolaryngol. India 2016, 68, 441–444. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ercan, I.; Cakir, B.O.; Sayin, I.; Başak, M.; Turgut, S. Relationship between the superior attachment type of uncinate process and presence of agger nasi cell: A computer-assisted anatomic study. Otolaryngol. Head Neck Surg Off. J. Am. Acad Otolaryngol.-Head Neck Surg. 2006, 134, 1010–1014. [Google Scholar] [CrossRef]
- Netto, B.; Piltcher, O.B.; Meotti, C.D.; Lemieszek, J.; Isolan, G.R. Computed tomography imaging study of the superior attachment of the uncinate process. Rhinology 2015, 53, 187–191. [Google Scholar] [CrossRef]

| Concha Bullosa | Lamellar Cell | |||
|---|---|---|---|---|
| All Types | Anterior Types | All Types | Anterior Types | |
| Middle turbinate SAUP | p = 0.782 | p = 0.665 | p = 0.235 | p = 0.237 |
| Lateral SAUP | p = 0.944 | p = 0.884 | p = 0.029 | p = 0.057 |
| Author/Year | Sample | SAUP Type (%) | ||||||
|---|---|---|---|---|---|---|---|---|
| I | II | III | IV | V | VI | Others | ||
| Calvo-Henríquez (this study) | 379 | 43.80 | 22.16 | 16.36 | 3.69 | 9.76 | 4.22 | - |
| Mahmutoğlu (2015) [5] | 919 | 28.2 | 36.1 | 4.1 | 0.9 | 0.7 | 17.4 | |
| Netto B (2015) [25] | 292 | 63.5 | 9.5 | 9.5 | 6.3 | 6.3 | 0.9 | |
| Ercan (2006) [24] | 371 | 62.6 | 3.1 | 11.6 | 14.4 | 8.3 | - | |
| Landsberg (2001) [4] | 173 | 52 | 18.5 | 17.5 | 7 | 3.6 | 1.4 | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calvo-Henriquez, C.; Mayo-Yañez, M.; Chiesa-Estomba, C.M.; Martinez-Capoccioni, G.; Martin-Martin, C. Relationship between the Superior Attachment of the Uncinate Process and Pneumatization of the Middle Turbinate—A Radiological Study. Surgeries 2022, 3, 134-141. https://doi.org/10.3390/surgeries3020015
Calvo-Henriquez C, Mayo-Yañez M, Chiesa-Estomba CM, Martinez-Capoccioni G, Martin-Martin C. Relationship between the Superior Attachment of the Uncinate Process and Pneumatization of the Middle Turbinate—A Radiological Study. Surgeries. 2022; 3(2):134-141. https://doi.org/10.3390/surgeries3020015
Chicago/Turabian StyleCalvo-Henriquez, Christian, Miguel Mayo-Yañez, Carlos M. Chiesa-Estomba, Gabriel Martinez-Capoccioni, and Carlos Martin-Martin. 2022. "Relationship between the Superior Attachment of the Uncinate Process and Pneumatization of the Middle Turbinate—A Radiological Study" Surgeries 3, no. 2: 134-141. https://doi.org/10.3390/surgeries3020015
APA StyleCalvo-Henriquez, C., Mayo-Yañez, M., Chiesa-Estomba, C. M., Martinez-Capoccioni, G., & Martin-Martin, C. (2022). Relationship between the Superior Attachment of the Uncinate Process and Pneumatization of the Middle Turbinate—A Radiological Study. Surgeries, 3(2), 134-141. https://doi.org/10.3390/surgeries3020015






