Pleural Effusion following Yoga: A Report of Delayed Spontaneous Chylothorax and a Brief Review of Unusual Cases in the Literature
Abstract
:1. Introduction
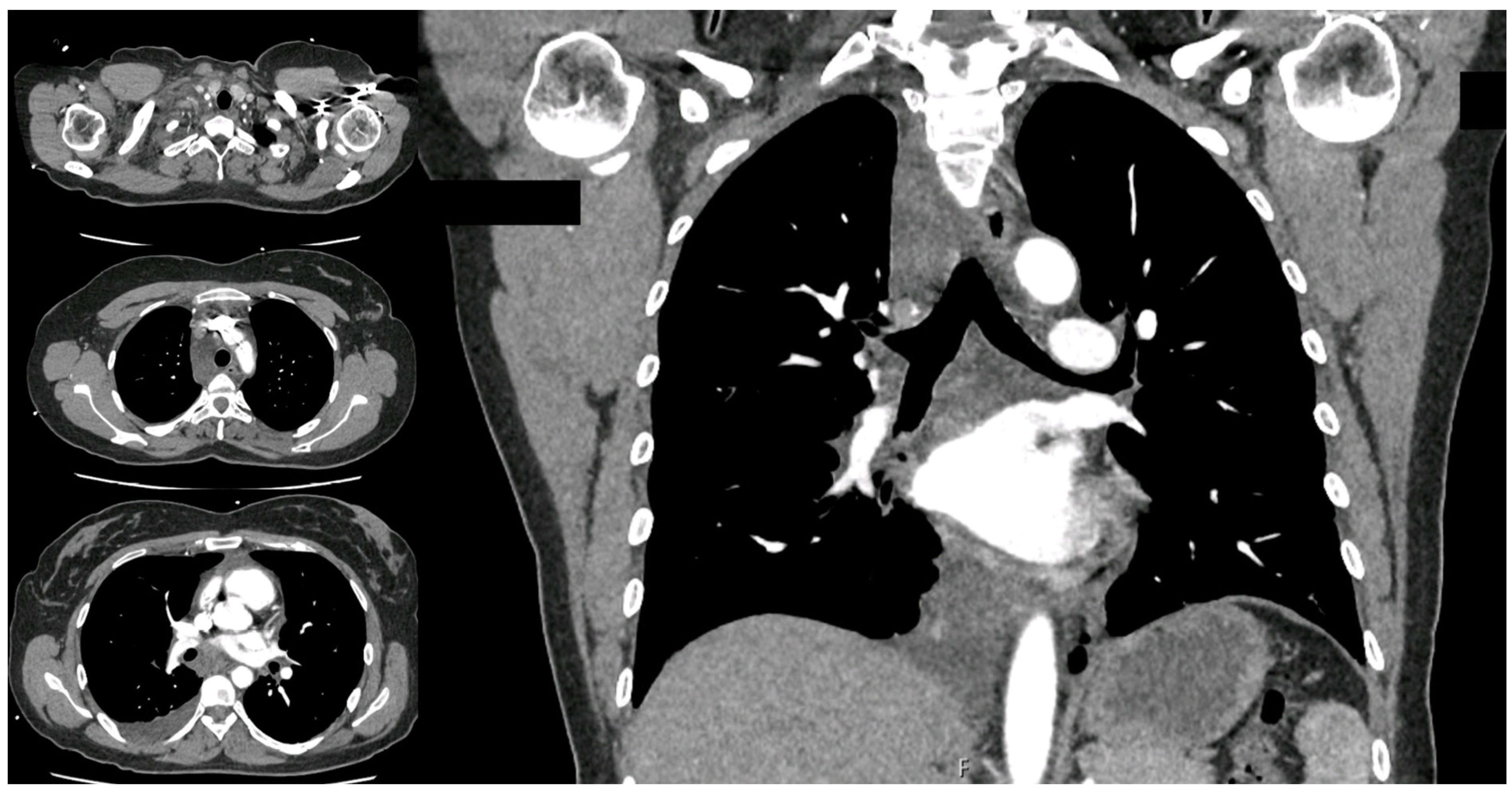
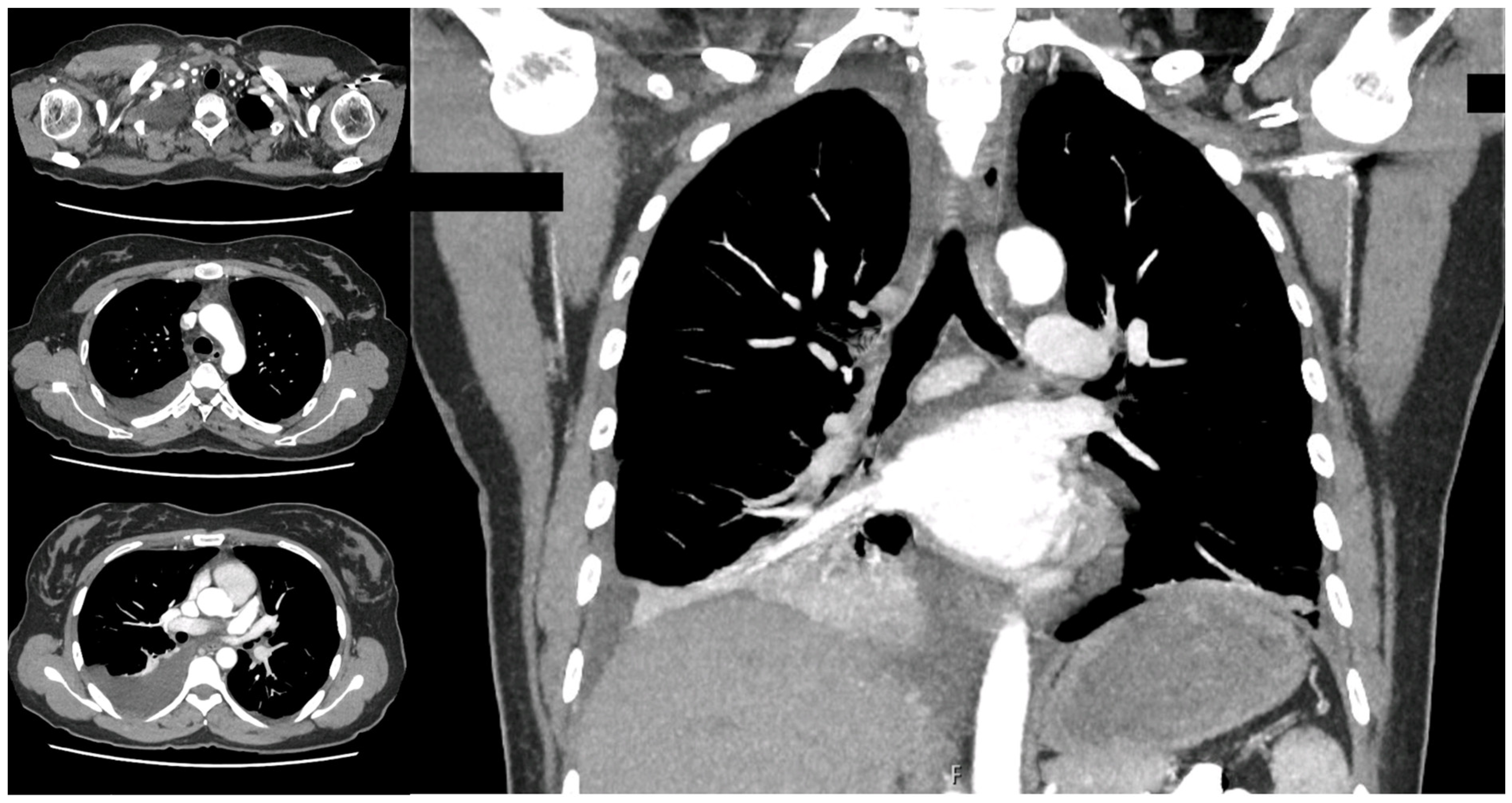
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Doerr, C.H.; Miller, D.L.; Ryu, J.H. Chylothorax. Semin. Respir. Crit. Care Med. 2001, 22, 617–626. [Google Scholar] [CrossRef] [PubMed]
- Doerr, C.H.; Allen, M.S.; Nicholas, F.C. Etiology of chylothorax in 203 patients. Mayo Clin. Proc. 2005, 80, 867. [Google Scholar] [CrossRef] [PubMed]
- Bender, B.; Murthy, V.; Chamberlin, R.S. The changing management of chylothorax in in the modern era. Eur. J. Cardiothorac. Surg. 2016, 49, 18–24. [Google Scholar] [CrossRef]
- Lama, A.; Ferreiro, L.; Toubes, M.E.; Golpe, A.; Gude, F.; Álvarez-Dobaño, J.M.; González-Barcala, F.J.; San José, E.; Rodríguez-Núñez, N.; Rábade, C.; et al. Characteristics of patients with pseudochylothorax—A systematic review. J. Thorac. Dis. 2016, 8, 2093–2101. [Google Scholar] [CrossRef] [PubMed]
- Sassoon, C.S.; Light, R.W. Chylothorax and pseudochylothorax. Clin. Chest Med. 1985, 6, 163–171. [Google Scholar] [CrossRef]
- McCray, S.P.C. Nutritional management of chyle leaks: An update. Pract. Gastroentrol. Ser. 2011, 94, 12–32. [Google Scholar]
- Huggins, J.T. Chylothorax and cholesterol pleural effusion. Semin. Respir. Crit. Care Med. 2010, 31, 743–750. [Google Scholar] [CrossRef] [PubMed]
- Riley, L.E.; Ataya, A. Clinical approach and review of causes of chylothorax. Respir. Med. 2019, 157, 7–13. [Google Scholar] [CrossRef]
- Ferrari, P.A.; Fusaro, F.; Ferrari, A.; Tamburrini, A.; Grimaldi, G.; Santoru, M.; Zappadu, S.; Tanda, E.; Nemolato, S.; Comelli, S.; et al. Refractory Chylothorax Secondary to Sizeable Azygos Vein Hemangioma: Tailored Multimodal Treatment of a Challenging Case Report. Medicina 2022, 59, 91. [Google Scholar] [CrossRef]
- McGrath, E.E.; Blades, Z.; Anderson, P.B. Chylothorax: Aetiology, diagnosis and therapeutic options. Respir. Med. 2010, 104, 1–8. [Google Scholar] [CrossRef]
- Staats, B.A.; Ellefson, R.D.; Budahn, L.L.; Dines, D.E.; Prakash, U.B.; Offord, K. The lipoprotein profile of chylous and nonchylous pleural effusion. Mayo Clin. Proc. 1980, 55, 700–704. [Google Scholar]
- Madaniah, A.A. Spontaneous idiopathic chylothorax in adults. Saudi Med. J. 2005, 26, 145–146. [Google Scholar] [PubMed]
- Cholet, C.; Delalandre, C.; Monnier-Cholley, L.; Le Pimpec-Barthes, F.; El Mouhadi, S.; Arrivé, L. Nontraumatic Chylothorax: Nonenhanced MR Lymphography. Radiographics 2020, 40, 1554–1573. [Google Scholar] [CrossRef] [PubMed]
- Savla, J.J.; Itkin, M.; Rossano, J.W.; Dori, Y. Post-Operative Chylothorax in Patients with Congenital Heart Disease. J. Am. Coll. Cardiol. 2017, 69, 2410–2422. [Google Scholar] [CrossRef] [PubMed]
- Weissler, J.M.; Cho, E.H.; Koltz, P.F.; Carney, M.J.; Itkin, M.; Laje, P.; Levin, L.S.; Dori, Y.; Kanchwala, S.K.; Kovach, S.J. Lymphovenous Anastomosis for the Treatment of Chylothorax in Infants: A Novel Microsurgical Approach to a Devastating Problem. Plast. Reconstr. Surg. 2018, 141, 1502–1507. [Google Scholar] [CrossRef] [PubMed]
- Aalami, O.O.; Allen, D.B.; Organ, C.H., Jr. Chylous ascites: A collective review. Surgery 2000, 128, 761–778. [Google Scholar] [CrossRef] [PubMed]
- Breslin, J.W.; Yang, Y.; Scallan, J.P.; Sweat, R.S.; Adderley, S.P.; Murfee, W.L. Lymphatic vessel network structure and physiology. Compr. Physiol. 2018, 9, 207–299. [Google Scholar] [PubMed]
- Torrejais, J.C.; Rau, C.B.; de Barros, J.A.; Torrejais, M.M. Spontaneous chylothorax associated with light physical activity. J. Bras. Pneumol. 2006, 32, 599–602. [Google Scholar] [CrossRef] [PubMed]
- Kolbaş, I.; Tezel, Y.; Coşgun, T.; Baysungur, V.; Tezel, C. Chylothorax Due to Weight Lifting: A Rare Etiology. South. Clin. Ist. Euras. 2020, 31, 75–77. [Google Scholar] [CrossRef]
- Akbar, S.; Advani, R.; Aggarwal, R. Bilateral spontaneous chylothorax presenting as a left-sided neck mass. BMJ Case Rep. 2021, 14, e240320. [Google Scholar] [CrossRef]
- Garcia-Aparicio, J.; Herrero-Herrero, J.-I.; Corral-Gudine, L.; Jorge-Sanchez, R.-J. Bilateral idiopathic chylothorax associated with light exercise. Resp. Med. CME 2009, 2, 68–69. [Google Scholar] [CrossRef]
- Bottet, B.; Melki, J.; Levesque, H.; Baste, J.M.; Roussel, E.; Peillon, C. Stretching et chylothorax. Rev. Mal. Respir. 2019, 36, 742–746. [Google Scholar] [CrossRef] [PubMed]
- Bocquel, V.; Girard, P.; Fournel, P.; Vergnon, J.M. Spontaneous chylothorax. Apropos of a further case. Rev. Mal. Respir. 1997, 14, 395–396. [Google Scholar] [PubMed]
- Hematti, H.; Mehran, R.J. Anatomy of the thoracic duct. Thorac. Surg. Clin. 2011, 21, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Meade, R.H. Spontaneous chylothorax. Arch. Intern. Med. 1972, 90, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Reilly, K.M.; Tsou, F. Bilateral chylothorax: A case report following episodes of stretching. JAMA 1975, 233, 536–537. [Google Scholar] [CrossRef] [PubMed]
- Gullane, P.J.; Marsh, A.S. Bilateral spontaneous chylothorax presenting as a neck mass. J. Otolaryngol. 1984, 13, 4. [Google Scholar]
- Tankanow, L.B.; Petrozzi, C.; Ward, J.C.; Bower, G.C. Idiopathic Bilateral Chylothorax Presenting as a Left-Sided Neck Swelling. Henry Ford. Hosp. Med. J. 1986, 34, 130–131. [Google Scholar] [PubMed]
- Fehr, M.; Lehmann, T.; Kuhn, M. Idiopathic chylothorax while vacuum cleaning. Schweiz Med. Forum. 2007, 7, 630–632. [Google Scholar]
- Bellini, C.; Cabano, R.; De Angelis, L.C.; Bellini, T.; Calevo, M.G.; Gandullia, P.; Ramenghi, L.A. Octreotide for congenital and acquired chylothorax in newborns: A systematic review. J. Paediatr. Child. Health 2018, 54, 840–847. [Google Scholar] [CrossRef]
- Anger, M.; Hofmann, J.; Ruf, B.; Steinborn, M.; Reber, D.; Warncke, K.; Rieber, N. Cough-induced chylothorax in a two-year-old boy—case report and review of the literature. BMC Pediatr. 2023, 23, 416. [Google Scholar] [CrossRef] [PubMed]
- Madhavan, S.; Nakao, M. How efficacious are Octreotide and Somatostatin in the management of chylothorax in congenital cardiac surgical patients? Interact. Cardiovasc. Thorac. Surg. 2021, 33, 773–778. [Google Scholar] [CrossRef] [PubMed]
- Al-Zubairy, S.A.; Al-Jazairi, A.S. Octreotide as a therapeutic option for management of chylothorax. Ann. Pharmacother. 2003, 37, 679–682. [Google Scholar] [CrossRef] [PubMed]
- Kalomenidis, I. Octreotide and chylothorax. Curr. Opin. Pulm. Med. 2006, 12, 264–267. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Deng, X.F.; Duan, C.M.; Chen, C.; Xiang, J.L.; Lu, Y.L.; Ma, O.F. Somatostatin receptors SSTR2 and SSTR5 are expressed in the human thoracic duct. Lymphology 2011, 44, 21–28. [Google Scholar] [PubMed]
- Buettiker, V.; Hug, M.I.; Burger, R.; Baenziger, O. Somatostatin: A new therapeutic option for the treatment of chylothorax. Intensive Care Med. 2001, 27, 1083–1086. [Google Scholar] [CrossRef] [PubMed]
- Ismail, N.A.; Gordon, J.; Dunning, J. The use of octreotide in the treatment of chylothorax following cardiothoracic surgery. Interact. Cardiovasc. Thorac. Surg. 2015, 20, 848–854. [Google Scholar] [CrossRef]
- Mitchell, K.; Weiner, A.; Ramsay, P.; Sahni, M. Use of Propranolol in the Treatment of Chylous Effusions in Infants. Pediatrics 2021, 148, e2020049699. [Google Scholar] [CrossRef] [PubMed]
- Jindal, R.; Singh, J.; Garg, L.; Gupta, M. Diagnosis and management of traumatic bilateral chylothorax: A clinical conundrum. BMJ Case Rep. 2019, 12, e229400. [Google Scholar] [CrossRef] [PubMed]
- Cope, C.; Kaiser, L.R. Management of unremitting chylothorax by percutaneous embolization and blockage of retroperitoneal lymphatic vessels in 42 patients. J. Vasc. Interv. Radiol. 2002, 13, 1139–1148. [Google Scholar] [CrossRef]
- Itkin, M.; Kucharczuk, J.C.; Kwak, A.; Trerotola, S.O.; Kaiser, L.R. Nonoperative thoracic duct embolization for traumatic thoracic duct leak: Experience in 109 patients. J. Thorac. Cardiovasc. Surg. 2010, 139, 584–589. [Google Scholar] [CrossRef] [PubMed]
- Nadolski, G.J.; Itkin, M. Thoracic duct embolization for nontraumatic chylous effusion: Experience in 34 patients. Chest 2013, 143, 158–163. [Google Scholar] [CrossRef] [PubMed]
- Boffa, D.J.; Sands, M.J.; Rice, T.W.; Murthy, S.C.; Mason, D.P.; Geisinger, M.A.; Blackstone, E.H. A critical evaluation of a percutaneous diagnostic and treatment strategy for chylothorax after thoracic surgery. Eur. J. Cardiothorac. Surg. 2013, 33, 435–439. [Google Scholar] [CrossRef] [PubMed]
- Laslett, D.; Trerotola, S.O.; Itkin, M. Delayed complications following technically successful thoracic duct embolization. J. Vasc. Interv. Radiol. 2012, 23, 76–79. [Google Scholar] [CrossRef] [PubMed]
- Kim, P.H.; Tsauo, J.; Shin, J.H. Lymphatic interventions for chylothorax: A systematic review and meta-analysis. J. Vasc. Interv. Radiol. 2018, 29, 194–202. [Google Scholar] [CrossRef]
- Pamarthi, V.; Stecker, M.S.; Schenker, M.P.; Baum, R.A.; Killoran, T.P.; Han, A.S.; O’Horo, S.K.; Rabkin, D.J.; Fan, C.M. Thoracic duct embolization and disruption for treatment of chylous effusions: Experience with 105 patients. J. Vasc. Interv. Radiol. 2014, 25, 1398–1404. [Google Scholar] [CrossRef] [PubMed]
- Binkert, C.A.; Yucel, E.K.; Davison, B.D.; Sugarbaker, D.J.; Baum, R.A. Percutaneous treatment of high-output chylothorax with embolization or needle disruption technique. J. Vasc. Interv. Radiol. 2005, 16, 1257–1262. [Google Scholar] [CrossRef] [PubMed]
- Jun, H.; Hur, S.; Jeong, Y.S.; Kang, C.H.; Lee, H. Thoracic duct embolization in treating postoperative chylothorax: Does bail-out retrograde access improve outcomes? Eur. Radiol. 2022, 32, 377–383. [Google Scholar] [CrossRef] [PubMed]
- Higgins, M.C.; Park, A.W.; Angle, J.F. Chylothorax: Percutaneous Embolization of the Thoracic Duct. Oper. Tech. Thorac. Cardiovasc. Surg. 2015, 20, 402–412. [Google Scholar] [CrossRef]
- Pillay, T.G.; Singh, B. A review of traumatic chylothorax. Injury 2016, 47, 545–550. [Google Scholar] [CrossRef]
- Fernández Alvarez, J.R.; Kalache, K.D.; Graŭel, E.L. Management of spontaneous congenital chylothorax: Oral medium-chain triglycerides versus total parenteral nutrition. Am. J. Perinatol. 1999, 16, 0415–0420. [Google Scholar] [CrossRef] [PubMed]
- Seitelman, E.; Arellano, J.J.; Takabe, K.; Barrett, L.; Faust, G.; Angus, L.G. Chylothorax after blunt trauma. J. Thorac. Dis. 2012, 4, 327–330. [Google Scholar] [PubMed]

| Authors, Year | Subjects (n) | Supposed Cause | Location of Chyle Leakage | Intervention |
|---|---|---|---|---|
| Meade RH, 1972 [25] | 5 | Hyperextension of the spine | Unilateral chylothorax | N/A |
| Reilly et al., 1975 [26] | 1 | Hyperextension of the spine during stretching exercise and yawning | Bilateral chylothorax | Conservative |
| Gullane et al., 1984 [27] | 1 | Hyperextension of the spine while swimming | Bilateral chylothorax | Conservative |
| Tankanow et al., 1986 [28] | 1 | Hyperextension of the spine while climbing into a bathtub | Bilateral chylothorax | Conservative |
| Bocquel et al., 1997 [23] | 1 | Overstretch of subclavius and anterior scalenus muscle during stretching exercise | Unilateral chylothorax | Conservative |
| Torrejais et al., 2006 [18] | 1 | Hyperextension of the neck during light physical activity at a fitness center | Bilateral neck swelling and bilateral chylothorax | Conservative |
| Fehr et al., 2007 [29] | 1 | Hyperextension of the neck and overstretch of thoracic outlet during routine vacuum cleaning | Left-sided neck swelling and bilateral chylothorax | Conservative |
| Garcìa-Aparicio et al., 2009 [21] | 1 | Hyperextension of the neck during light physical activity | Bilateral chylothorax | Conservative |
| Bottet et al., 2019 [22] | 1 | Overstretch of subclavius and anterior scalenus muscle during stretching exercise | Bilateral chylothorax | Conservative |
| Kolbas et al., 2020 [19] | 1 | Overstretch of subclavius and anterior scalenus muscle while lifting 40 kg at a fitness center | Left-sided chylothorax | Conservative |
| Akbar et al., 2021 [20] | 1 | Hyperextension of the spine during stretching exercise | Left-sided neck swelling and bilateral chylothorax | Conservative |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hunduma, G.; Ferrari, P.A.; Alreshaid, F.; Kiran, T.; Alzetani, A.; Tamburrini, A. Pleural Effusion following Yoga: A Report of Delayed Spontaneous Chylothorax and a Brief Review of Unusual Cases in the Literature. Surgeries 2024, 5, 288-296. https://doi.org/10.3390/surgeries5020026
Hunduma G, Ferrari PA, Alreshaid F, Kiran T, Alzetani A, Tamburrini A. Pleural Effusion following Yoga: A Report of Delayed Spontaneous Chylothorax and a Brief Review of Unusual Cases in the Literature. Surgeries. 2024; 5(2):288-296. https://doi.org/10.3390/surgeries5020026
Chicago/Turabian StyleHunduma, Gabriel, Paolo Albino Ferrari, Farouk Alreshaid, Tayyeba Kiran, Aiman Alzetani, and Alessandro Tamburrini. 2024. "Pleural Effusion following Yoga: A Report of Delayed Spontaneous Chylothorax and a Brief Review of Unusual Cases in the Literature" Surgeries 5, no. 2: 288-296. https://doi.org/10.3390/surgeries5020026
APA StyleHunduma, G., Ferrari, P. A., Alreshaid, F., Kiran, T., Alzetani, A., & Tamburrini, A. (2024). Pleural Effusion following Yoga: A Report of Delayed Spontaneous Chylothorax and a Brief Review of Unusual Cases in the Literature. Surgeries, 5(2), 288-296. https://doi.org/10.3390/surgeries5020026







