Abstract
Background/Objectives: The field of tracheal reconstruction has undergone significant developments in the last few decades. Accordingly, this bibliometric review aims to identify the most influential publications within the field and their citation characteristics. Methods: A comprehensive search for “tracheal reconstruction” was conducted with the Clarivate’s Web of Science database. The resulting search results were filtered for relevant publications and evaluated to identify the 50 publications with the highest citation counts. Further analysis of these publications was conducted based on the following parameters: authorship, institutional affiliations, country of origin, citation density, year of publication, article type, and level of evidence. VOSviewer (version 1.6.20) was utilized to create co-occurrence maps of authors and keywords. Results: The top 50 publications were cited a total of 6449 times with an average of 128.98 citations per publication. The top three most cited articles were all by Grillo (primarily focused on tracheal stent repair and post-oncologic reconstruction). The majority of the top cited publications articles featured in The Annals of Thoracic Surgery (n = 10) were basic science in nature (32%) and had a level of evidence of Level IV (62%). The publication with the greatest citation density was by Kang et al. focusing on tracheal tissue engineering (TTE). Conclusions: This bibliometric review provides a thorough overview of the key publications that have influenced the field of tracheal reconstruction. Most predominantly, our analysis highlights a shift in focus from primary tracheal reconstruction techniques to more innovative repair paradigms such as TTE.
1. Introduction
Tracheal reconstruction is a surgical intervention primarily indicated for patients with malignancies, congenital anomalies, or traumatic injuries leading to airway compromise [1,2]. In the United States alone, approximately 1617 tracheal reconstructions are performed annually [3]. Post-intubation tracheal stenosis accounts for about 75% of all tracheal reconstruction cases and has a reported annual incidence between 0.5% and 3% [4,5,6,7]. Traditional surgical methods, such as segmental resection with end-to-end anastomosis, remain the gold standard for managing short-segment lesions; however more extensive tracheal defects have necessitated alternative techniques like tracheal patching, autologous tissue grafts, or synthetic prostheses [1,8]. However, these methods have faced limitations related to graft integration, mechanical stability, and long-term functionality [1,9]. A notable advancement in recent years has been the implementation of tracheal transplantation utilizing vascularized composite allografts (VCAs). This method offers a promising solution for longer-segment tracheal defects as the blood supply is kept intact, enhancing graft integration, maintaining structural integrity, and eliminating the need for revascularization, a historical barrier to successful tracheal transplantation [10]. Moreover, this approach has also shown efficacy in overcoming other prior limitations, such as mucus plugging and mechanical erosion associated with extended tracheostomies and alloplastic stents [11]. Research on tracheal scaffolds and their impact on extracellular matrix (ECM) components has been crucial for the development of VCA as it provides insights into optimizing decellularization protocols to reduce immunogenicity and improve graft integration [12]. Accordingly, the field of tracheal reconstruction is dynamic and continuing to evolve.
Bibliometric reviews are systematic analyses of the scientific literature that provide insight into publication trends, influential articles, and emerging areas of research to evaluate academic productivity in a particular field. These reviews leverage quantitative analysis of bibliographic data, such as citation counts and author collaborations, to evaluate the trajectory of a discipline, identify research gaps, and offer a roadmap for future studies [13,14]. In growing fields like tracheal reconstruction, this form of analysis can uncover important information on the current state of research and predict future directions. Despite the critical nature of tracheal reconstruction for managing complex airway pathologies, no comprehensive bibliometric review has been conducted to examine this field as a whole. Identifying under-researched areas, trends in publication activity, and the influence of key studies is crucial to guiding researchers and clinicians in optimizing tracheal reconstruction techniques. This study aims to address this gap by presenting the first bibliometric review of the tracheal reconstruction literature, offering an evidence-based perspective on the field’s trajectory.
2. Methods
On 17 June 2024, a comprehensive search was conducted using Clarivate Analytics Web of Science to gather the relevant literature. The search query applied was “tracheal reconstruction OR laryngotracheal reconstruction,” with no filters applied initially. This search yielded 2831 results. These results were sorted by citation count, from highest to lowest. Exclusions were applied to remove non-relevant document types such as proceeding papers, book chapters, and abstracts, as well as studies where tracheal reconstruction was not a central focus or not written in English. From this filtered set, the 200 most-cited articles were exported to an Excel spreadsheet for further review. In cases where relevance could not be determined from the title alone, abstracts and full-text articles were reviewed. Subsequently, the 50 most-cited articles were selected for detailed analysis. The full-text versions of these top 50 articles were evaluated to determine the level of evidence (LOE), as defined by the Oxford Center for Evidence-Based Medicine (OCEBM) guidelines. Two reviewers were trained in the use of the LOE and independently reviewed and scored articles. Cohen’s kappa statistic was used to assess interrater reliability. The following criteria were used:
- Level 1: Systematic reviews of randomized trials, or systematic reviews of inception cohort studies.
- Level 2: Systematic reviews of cohort studies, inception cohort studies, cross-sectional studies, randomized trials, or observational studies with significant impact.
- Level 3: Retrospective cohort studies or epidemiological/observational studies.
- Level 4: Case–control studies, low-impact cohort studies, or animal studies.
- Level 5: Simulations, models, or mechanism-based reasoning.
The articles were also evaluated and placed into the following categories: Basic Science, Surgical Technique, Patient Outcomes, Review, or Treatment Guidelines. The following variables were extracted and analyzed from the Web of Science database for each selected article: primary author, country of origin, total number of citations, average citations per year, year of publication, and the journal in which the study was published. VOSviewer (version 1.6.20) was utilized to create co-occurrence maps of authorships and keywords. Data was exported from the Web of Science database as a text file and imported into VOSviewer for bibliometric network analysis and visualization. The software generated overlay visualizations to demonstrate temporal trends, with color gradients representing the chronological distribution of term occurrence. The relative frequency of terms is represented by the size of their respective labels and circles, while the thickness of connecting lines indicates the strength of correlation between terms.
3. Results
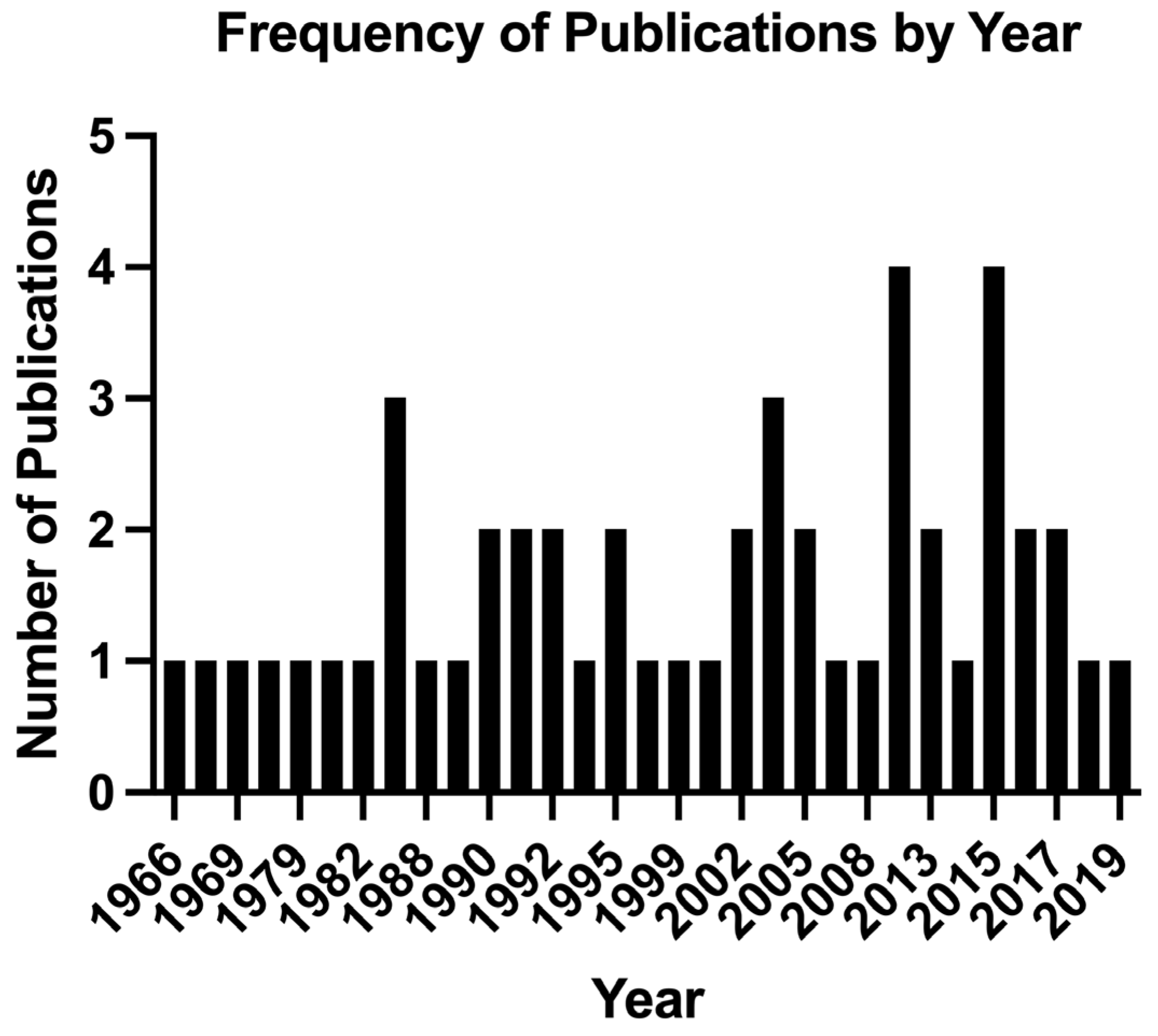
The 50 publications analyzed in this study were cited a total of 6449 times with an average of 128.98 citations per publication as listed in Table 1. The most-cited article in this analysis was cited 421 times, while the least-cited article in the top 50 had 74 citations. The most recent publication included in the analysis was from 2019, while the oldest dated back to 1966. The years 2015 and 2014 were the most prolific in terms of output, each contributing 4 of the top 50 publications (Figure 1). This was followed by 2003 and 1986, with three publications each. Nine other years were tied with two publications each.

Table 1.
Top 50 publications regarding tracheal reconstruction with greatest number of citations.
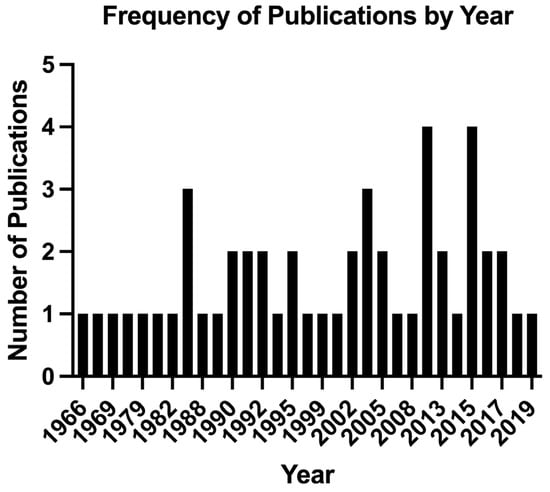
Figure 1.
Top 50 cited publications regarding tracheal reconstruction by frequency each year.
The most-cited publication was “Postintubation Tracheal Stenosis. Treatment and Results” (1995) by Grillo et al. The second most-cited publication was “Tracheal Replacement: A Critical Review” (2002), by Grillo. The third most-cited publication was “Primary Tracheal Tumors: Treatment and Results” (1990), by Grillo and Mathisen. The author with the highest number of contributions was Grillo, with 10 publications in the top 50 (Supplemental Table S1). Cotton contributed five articles, while Neville and Martinod each contributed two. The remaining authors each had a single publication included in the analysis. Harvard/Massachusetts General Hospital (MGH) led the institutional contributions with 14 publications, followed by the University System of Ohio with three (Supplemental Table S2). Four other institutions each contributed two articles. The United States emerged as the leading country in terms of publication output, contributing 28 of the top 50 articles (Supplemental Table S3). France and China tied for second place, each with four publications. Japan and Canada followed, each contributing two publications. The majority of publications were featured in The Annals of Thoracic Surgery (n = 10), followed by The Journal of Thoracic and Cardiovascular Surgery (n = 7) and Laryngoscope (n = 6).
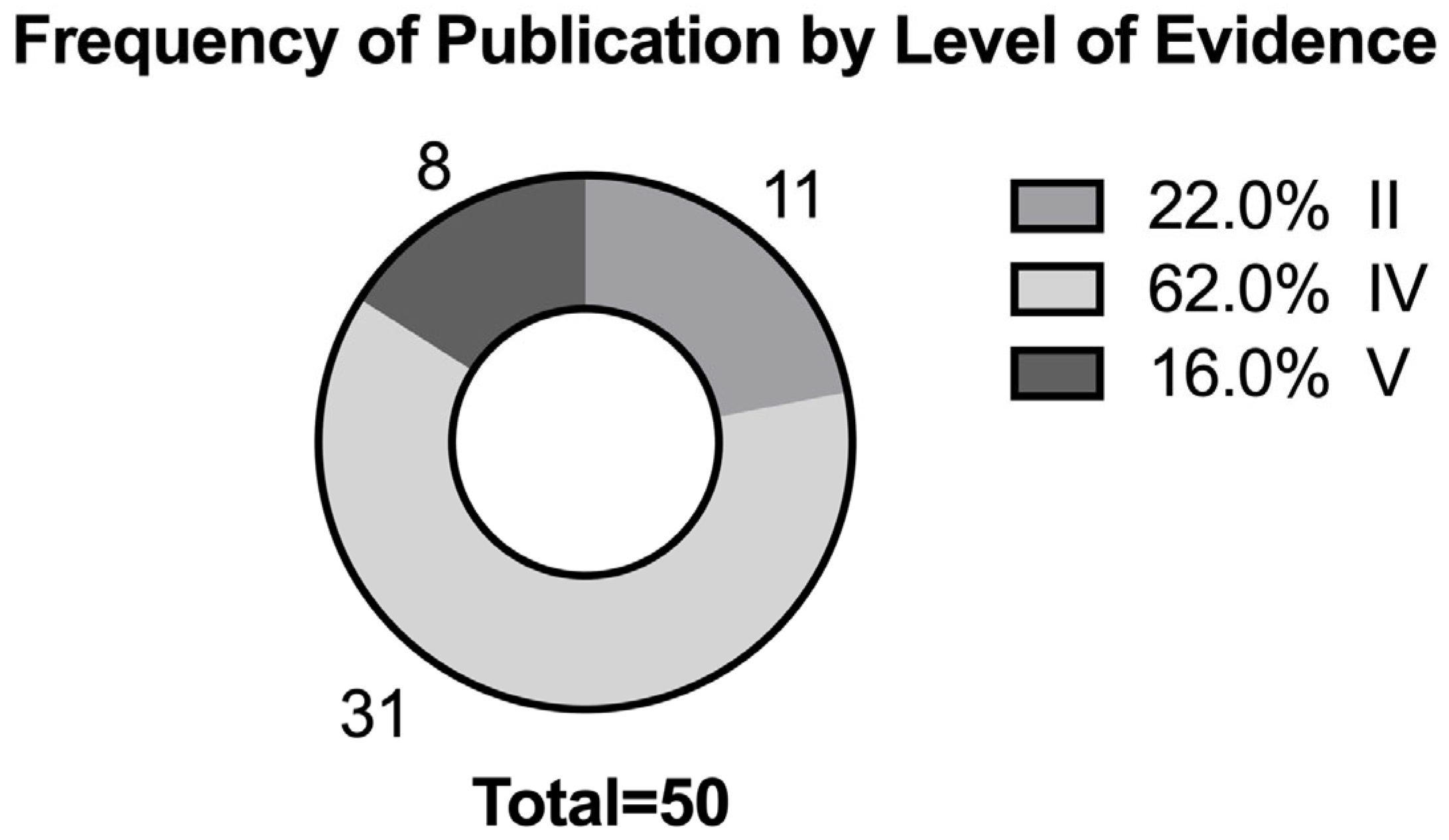
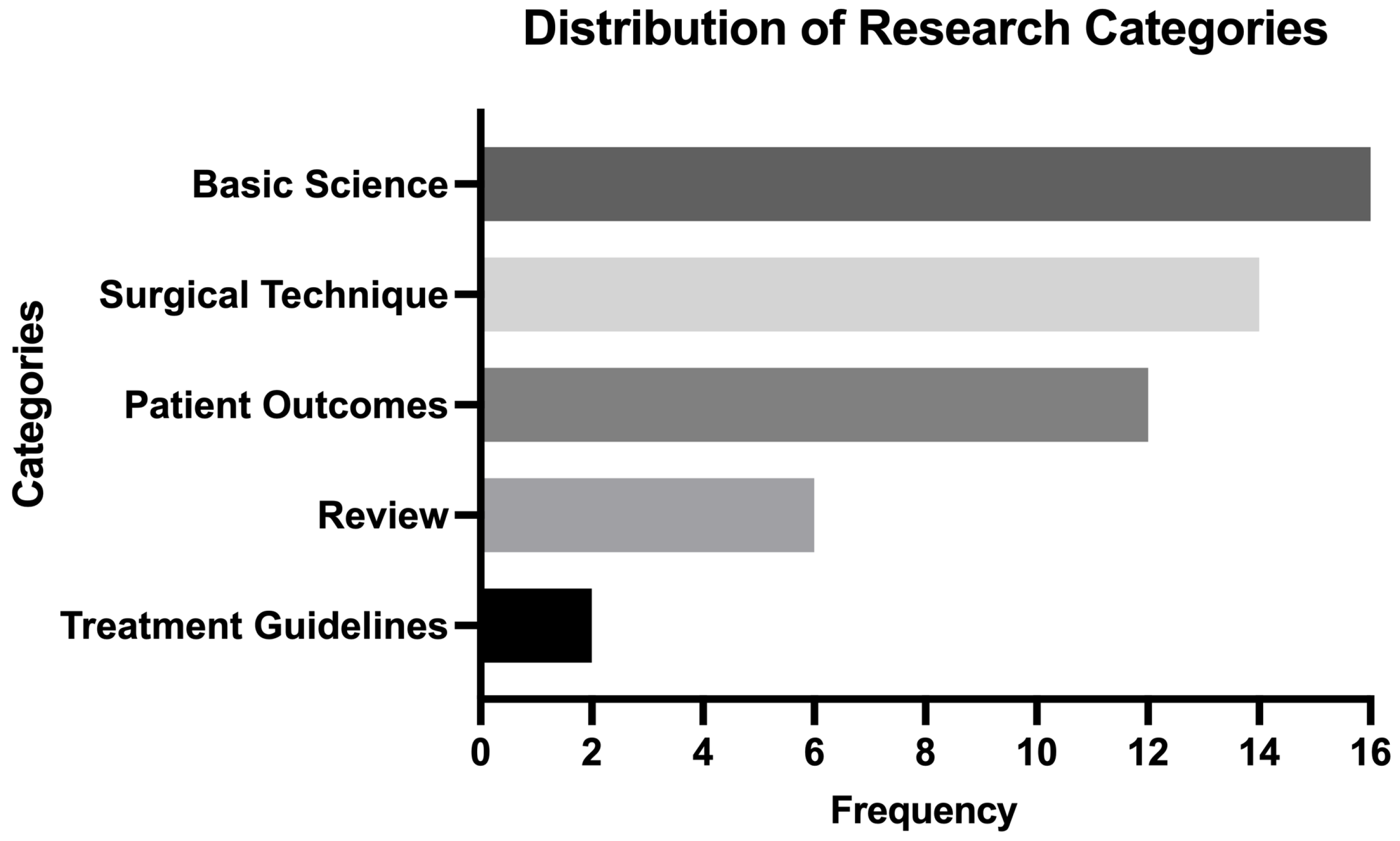
In terms of the level of evidence (LOE), the most common classification was Level IV, with 31 publications (62%) falling into this category (Figure 2). Inter-rater agreement between reviewers for LOE scoring was high (kappa value of 0.91). Among the analyzed articles, basic science research represented the largest category with 16 articles (32%), closely followed by surgical technique descriptions with 14 articles (28%). Patient outcome studies constituted twelve articles (24%), while review articles and treatment guidelines made up smaller proportions with six (12%) and two (4%) articles, respectively (Figure 3). As outlined in Table 2, when the top 50 publications list was assorted by citation density (citations per year since year or publication), Kang et al.’s “Tissue-Engineered Trachea Consisting of Electrospun Patterned sc-PLA/GO- g-IL Fibrous Membranes with Antibacterial Property and 3D-Printed Skeletons with Elasticity” (2019) had the highest citation density (n = 25.50). Butler et al.’s “Rapid Expansion of Human Epithelial Stem Cells Suitable for Airway Tissue Engineering” (2016) had the second highest citation density (n = 21.57), and Grillo’s “Tracheal Replacement: A Critical Review” (2002) had the third highest citation density (n = 19.76). Supplemental Figures S1 and S2 provide association maps of authors and key search terms, respectively, of the top 50 publications for tracheal reconstruction.
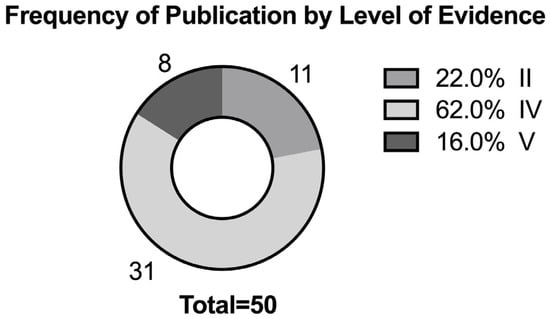
Figure 2.
Top 50 cited publications regarding tracheal reconstruction by level of evidence.
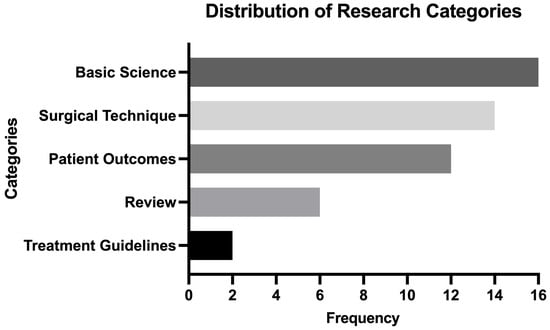
Figure 3.
Top 50 cited publications regarding tracheal reconstruction by distribution of research categories.

Table 2.
Publications regarding tracheal reconstruction with greatest citation density (number of citations per year since publication year).
4. Discussion
This bibliometric analysis helped identify the most influential publications and emerging research directions for tracheal reconstruction. From the impactful, early publications of Grillo highlighting surgical approaches for tracheal stenosis and cancers to the more recent focus on advanced techniques, including vascularized composite allograft transplantation and tissue engineering, the rapid evolution of the field is apparent [15,16]. Accordingly, the aim of this study was to capture this evolution and not only provide a temporal accounting of its context but highlight its significance toward advancing the field of tracheal reconstruction in the future.
In 1995, Grillo et al. published the top-cited article on tracheal reconstruction, titled “Postintubation Tracheal Stenosis: Treatment and Results” [17]. This retrospective cohort study analyzed data from 503 patients who underwent a total of 521 tracheal resections and reconstructions between 1965 and 1992, making it one of the largest studies to systematically assess surgical outcomes in this patient population. This study was monumental in defining the surgical management of postintubation stenosis, highlighting specific approaches based on the etiology and anatomical location of stenosis, including cuff lesions, stomal lesions, and complex laryngeal injuries. Importantly, this study demonstrated a high success rate for tracheal resections and reconstruction, providing robust evidence for their efficacy in treating this condition and serving as a foundational reference for surgical techniques and postoperative care in tracheal reconstruction [18]. Collectively, Grillo’s collective studies demonstrated the feasibility of resecting up to 50% of the trachea with primary anastomosis, providing a solution for conditions such as postintubation stenosis and primary tracheal tumors [19]. His research also addressed the challenges of tracheal replacement and transplantation, critically reviewing advancements in tissue-engineered grafts and autologous transplants [20].
In 2002, Grillo et al. published “Tracheal Replacement: A Critical Review,” the second most cited publication regarding tracheal reconstruction [20]. This review provided a comprehensive examination of the experimental and clinical efforts to develop viable tracheal substitutes. Specifically, it categorized tracheal replacement approaches into synthetic prostheses, autologous tissue grafts, and bioengineered constructs, critically evaluating their respective advantages and limitations. In general, the authors concluded that while synthetic prostheses offered mechanical strength, they often failed due to infection and poor integration. In contrast, autologous tissue grafts demonstrated better biocompatibility but faced challenges with airway rigidity and availability. The review played a valuable role in highlighting the unmet need for functional and durable replacements, inspiring future advancements in bioengineered scaffolds and tissue-engineered tracheas. In 1990, Grillo and Mathisen published “Primary Tracheal Tumors: Treatment and Results,” a landmark study analyzing surgical outcomes for tracheal tumors that was the third most cited publication on tracheal reconstruction [21]. This paper detailed the management of 198 patients with primary tracheal tumors over 26 years, focusing on the surgical resection and reconstruction of the resulting defects. The authors provided several therapeutic recommendations, including that benign and intermediate-aggressiveness tumors are best managed through surgical resection with airway reconstruction, thus playing a significant role in setting the modern treatment paradigm for the treatment of such tumors. They also emphasize the importance of performing extensive tracheal reconstructions, particularly those involving the carina, at specialized centers to optimize outcomes. This work significantly advanced the understanding of tracheal tumors and surgical techniques, establishing a gold standard for the surgical management of these challenging tumors.
Largely a result of Grillo’s tenure and legacy at the institution, Harvard/MGH unsurprisingly emerged as the leading institution, contributing 14 of the most-cited publications to tracheal reconstruction. More broadly, the United States (U.S.) also definitively led in publication output (28/50 articles), followed by France and China (4 each). The U.S. contributed predominantly to surgical and clinical studies; however, contributions from France and China have focused more on tissue engineering and novel biomaterials. Basic science studies (32%) and surgical technique reports (28%) represented the largest categories, followed by patient outcomes (24%). Level IV evidence dominated the field (62%), comprising case–control studies. This prevalence aligns with the experimental nature of tracheal reconstruction, where novel techniques and materials are being evaluated in preclinical or observational settings before widespread clinical adoption [22]. The relative scarcity of treatment guidelines and systematic reviews highlights the ongoing developmental phase of this field, particularly in areas like tissue engineering and regenerative techniques [23].
A temporal trend was also observed with a significant concentration of publications between the mid-2000s and 2015. This period coincides with a steady increase in the investigation of the tracheal tissue engineering (TTE) methodology—a trend supported by an external review by Zhu et al. [23]. Our own results identified that publications from Butler et al. and Kang et al. (both published in the mid-2010s) had the highest citation density and both were focused on scientific models of TTE (Table 2) [24,25]. Butler et al. presented a scalable method for generating human airway basal epithelial cells using a combination of mitotically inactivated fibroblasts and Rho-associated protein kinase (ROCK) inhibition to generate large numbers of functional airway cells for tissue engineering. These cells demonstrated multipotent differentiation, normal ciliary function, and successful repopulation of tracheal scaffolds in a xenograft model, demonstrating potential suitability for clinical tracheal reconstruction applications. Kang et al. developed a tissue-engineered trachea scaffold by integrating electrospun stereocomplex polylactide (sc-PLA) membranes with graphene oxide (GO)-grafted ionic liquid (IL) to provide antibacterial properties, mechanical strength, and cell infiltration, alongside a 3D-printed thermoplastic polyurethane (TPU) skeleton for structural elasticity. The in vivo rabbit model confirmed the biocompatibility and tissue regeneration potential of the scaffold and suggested its suitability for tracheal reconstruction applications. The recency and high citation density of these papers suggest that topics of bioengineered scaffolds and tissue engineering are emerging as the predominant areas of exploration, ultimately shaping the current research frontiers in tracheal reconstruction. Specifically, TEE is enabling the development of patient-specific, bioengineered tracheal grafts that better replicate native airway structure and function. These technologies allow for customized scaffold fabrication, improved cell integration, and preoperative surgical planning. As a result, they are shaping current clinical strategies toward more precise, regenerative, and less immunogenic approaches to tracheal reconstruction [26,27,28,29,30,31,32,33].
Author collaboration maps revealed limited connectivity between research groups, indicating that the field remains relatively fragmented. Of the 230 authors there were only 26 that were co-authored on two or more papers. The Japanese group of Kobayashi, Nakamura, Nomoto, Omori, Suzuki, and Tada was the largest group, consisting of six linked co-authors. This lack of collaborative efforts across institutions may hinder the pace of innovation and translation. Increasing interdisciplinary and global partnerships could accelerate advancements in tracheal reconstruction. Keyword co-occurrence analysis identified that before the mid-2000s, the most prominent terms revolved around the core elements of tracheal reconstruction “anastomosis” and “graft” and “resection”, for example, suggesting that most interest was on exploring the technical aspect of managing airway defects. More recent, prominent terms such as “tissue engineering”, “revascularization”, and “stem cells” have emerged, reflecting the field’s growing focus on regenerative medicine and the search for a viable tracheal replacement. Terms like “fabrication” and “scaffolds” arise mostly post-2015, supporting the shift toward engineered scaffolds and 3D printing regenerative medicine as the tracheal substitute solution of intrigue. These findings align with the recent literature highlighting the potential of additive manufacturing and advanced biomaterials to overcome current limitations [34,35]. The future of tracheal reconstruction seems to lie in combining advanced biomaterials with tissue engineering to create functional tracheal substitutes [36]. Emerging technologies, such as 3D printing, stem cell-based therapies, and improved decellularization, revascularization, or re-epithelialization techniques are expected to play a pivotal role in developing biocompatible grafts with enhanced integration and mechanical properties [37]. Moving forward, large-scale, multicenter clinical trials are essential to validate these innovations and establish standardized protocols for their clinical application.
5. Limitations
This study has several notable limitations. Searching for specific keywords (i.e., “tracheal reconstruction”) within a citation database such as Web of Science can result in potential biasing of the results. Not all relevant publications may be captured by the broad search terms and omission of influential papers may be possible if they were additionally published in non-indexed journals. Additionally, because the search was conducted in English only, influential publications in languages other than English were excluded which may have impacted the publication representation by countries outlined in this analysis. This analysis should be repeated in future studies utilizing related but alternative keywords or in languages other than English to further contextualize the global bibliometric history and evolution of tracheal reconstruction. This study utilized citation count as a guiding metric for identifying the most impactful/influential publications in field of tracheal reconstruction. While this understanding has been accepted as the basis of bibliometric reviews, in general, it should be noted that citation counts can be subject to artificial inflation through practices such as self-citation and citation stacking which can skew the true impact of a given publication. Finally, it should be noted that publication counts are dependent on time (greater time since publication offer greater opportunity to accrue citations). As a result, more recently published articles may have been excluded from our top 50 analysis despite their possible distinction/promise for advancing the field. However, our sub-analysis examining the top 10 citations with the greatest citation density helps to provide additional context to this limitation.
6. Conclusions
Ultimately, this bibliometric review provided invaluable insights into the most influential publications and recent topics that have defined the field of tracheal. The descriptive findings of our analysis spotlight the impactful work Grillo has had in advancing the field, especially in his contributions understanding the techniques and outcomes for tracheal reconstruction following stenosis or tumor excision. In accordance with his contributions, the U.S. emerged as a significant contributor to the past half-century of trachea reconstruction advancements. However, among more recent publications, a shift in focus was identified toward investigation of TTE techniques such as bioengineered scaffolds and utilization of tracheal grafts. These techniques offer exciting clinical implications for revolutionizing tracheal reconstruction by providing patients more individualized and robust treatment options with decreased morbidity. Despite this promise, critical gaps remain in the clinical translation of these modern tracheal reconstruction techniques, the most notable being a lack of long-term outcome data. As the majority of work conducted has been limited to individual case reports, continued effort must be directed toward developing high-level, multi-center, clinical research studies within this growing and evolving field in order to fully realize its potential for patient care.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/surgeries6030062/s1. Figure S1: Author association map of the top 50 cited publications regarding tracheal reconstruction. Figure S2: Key terms association map of the top 50 cited publications regarding tracheal reconstruction. Table S1: Number of publications produced by most influential authors. Only authors with two or more publications are included. Table S2: Institutions that produced the most influential publications. Only institutions with two or more publications are included. Table S3: Countries that produced the most influential publications. Only countries with two or more publications are included.
Author Contributions
Conceptualization, S.B., A.L. and A.Z.V.; Methodology, S.B., A.L. and G.C.; Software, S.B. and A.L.; Validation, G.C. and E.G.; Formal Analysis, S.B., A.L., E.G. and A.Z.V.; Investigation, S.B., A.L., G.C. and E.G.; Resources, E.G. and A.Z.V.; Data Curation, S.B., A.L. and E.G.; Writing—Original Draft Preparation, S.B., A.L. and E.G.; Writing—Review and Editing, L.K., F.J.K. and S.H.; Visualization, L.K., F.J.K. and S.H.; Supervision, L.K., F.J.K. and S.H.; Project Administration, L.K., F.J.K. and S.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data generated for this research was accessed through the publicly available Web of Science database.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Etienne, H.; Fabre, D.; Caro, A.G.; Kolb, F.; Mussot, S.; Mercier, O.; Mitilian, D.; Stephan, F.; Fadel, E.; Dartevelle, P. Tracheal replacement. Eur. Respir. J. 2018, 51, 1702211. [Google Scholar] [CrossRef]
- Genden, E.M.; Laitman, B.M. Human Tracheal Transplantation. Transplantation 2023, 107, 1698–1705. [Google Scholar] [CrossRef]
- Stanifer, B.P.; Andrei, A.C.; Liu, M.; Meyerson, S.L.; Bharat, A.; Odell, D.D.; DeCamp, M.M. Short-Term Outcomes of Tracheal Resection in The Society of Thoracic Surgeons Database. Ann. Thorac. Surg. 2018, 106, 1612–1618. [Google Scholar] [CrossRef]
- Elsayed, H.; Mostafa, A.M.; Soliman, S.; Shoukry, T.; El-Nori, A.A.; El-Bawab, H.Y. First-line tracheal resection and primary anastomosis for postintubation tracheal stenosis. Ann. R. Coll. Surg. Engl. 2016, 98, 425–430. [Google Scholar] [CrossRef]
- Kim, S.S.; Khalpey, Z.; Hsu, C.; Little, A.G. Changes in Tracheostomy- and Intubation-Related Tracheal Stenosis: Implications for Surgery. Ann. Thorac. Surg. 2017, 104, 964–970. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Johnson, R.F.; Bradshaw, S.; Jaffal, H.; Chorney, S.R. Estimations of Laryngotracheal Stenosis After Mechanical Ventilation: A Cross-Sectional Analysis. Laryngoscope 2022, 132, 1723–1728. [Google Scholar] [CrossRef] [PubMed]
- Farzanegan, R.; Zangi, M.; Abbasidezfouli, A.; Pejhan, S.; Sadeghbeigee, F.; Daneshvarkakhki, A.; Sheikhy, K.; Saghebi, S.R.; Nazemy, S.; Jahanshahi, N.; et al. Postintubation Multisegmental Tracheal Stenosis: A 24-Year Experience. Ann. Thorac. Surg. 2021, 112, 1101–1108. [Google Scholar] [CrossRef] [PubMed]
- Rich, J.T.; Gullane, P.J. Current concepts in tracheal reconstruction. Curr. Opin. Otolaryngol. Head Neck Surg. 2012, 20, 246–253. [Google Scholar] [CrossRef]
- Greaney, A.M.; Niklason, L.E. The History of Engineered Tracheal Replacements: Interpreting the Past and Guiding the Future. Tissue Eng. Part B Rev. 2021, 27, 341–352. [Google Scholar] [CrossRef]
- Haykal, S.; Salna, M.; Waddell, T.K.; Hofer, S.O. Advances in tracheal reconstruction. Plast. Reconstr. Surg. Glob. Open. 2014, 2, e178. [Google Scholar] [CrossRef]
- Zhang, Y.; Wei, S.; Li, M.; Lv, G. Revolutionizing tracheal reconstruction: Innovations in vascularized composite allograft transplantation. Front. Bioeng. Biotechnol. 2024, 12, 1452780. [Google Scholar] [CrossRef] [PubMed]
- Haykal, S.; Soleas, J.P.; Salna, M.; Hofer, S.O.; Waddell, T.K. Evaluation of the structural integrity and extracellular matrix components of tracheal allografts following cyclical decellularization techniques: Comparison of three protocols. Tissue Eng. Part C Methods 2012, 18, 614–623. [Google Scholar] [CrossRef] [PubMed]
- Kumar, L.M.; George, R.J.; Anisha, P.S. Bibliometric Analysis for Medical Research. Indian J. Psychol. Med. 2023, 45, 277–282. [Google Scholar] [CrossRef]
- Ninkov, A.; Frank, J.R.; Maggio, L.A. Bibliometrics: Methods for studying academic publishing. Perspect. Med. Educ. 2022, 11, 173–176. [Google Scholar] [CrossRef]
- Hondt, M.D.; Vranckx, J.J. Reconstruction of defects of the trachea. J. Mater. Sci. Mater. Med. 2017, 28, 24. [Google Scholar] [CrossRef]
- Perryman, M.C.; Kraft, S.M.; Kavookjian, H.L. Laryngotracheal Reconstruction for Subglottic and Tracheal Stenosis. Otolaryngol. Clin. N. Am. 2023, 56, 769–778. [Google Scholar] [CrossRef]
- Grillo, H.C.; Donahue, D.M.; Mathisen, D.J.; Wain, J.C.; Wright, C.D. Postintubation tracheal stenosis: Treatment and results. J. Thorac. Cardiovasc. Surg. 1995, 109, 486–493. [Google Scholar] [CrossRef]
- Austen, W.G.; Burke, J.F.; Mathisen, D.J.; Russell, P.S.; Wilkins, E.W., Jr. Hermes C. Grillo. Harvard Gazette. 2007. Available online: https://news.harvard.edu/gazette/story/2007/11/hermes-c-grillo/ (accessed on 11 November 2024).
- Mulliken, J.B.; Grillo, H.C. The limits of tracheal resection with primary anastomosis: Further anatomical studies in man. J. Thorac. Cardiovasc. Surg. 1968, 55, 418–421. [Google Scholar] [CrossRef]
- Grillo, H.C. Tracheal replacement: A critical review. Ann. Thorac. Surg. 2002, 73, 1995–2004. [Google Scholar] [CrossRef]
- Grillo, H.C.; Mathisen, D.J. Primary tracheal tumors: Treatment and results. Ann. Thorac. Surg. 1990, 49, 69–77. [Google Scholar] [CrossRef]
- Chen, D.; Britt, C.J.; Mydlarz, W.; Desai, S.C. A novel technique for tracheal reconstruction using a resorbable synthetic mesh. Laryngoscope 2018, 128, 1567–1570. [Google Scholar] [CrossRef]
- Zhu, J.; Lu, Y.; Shan, Y.; Yuan, L.; Wu, Q.; Shen, Z.; Sun, F.; Shi, H. Global Bibliometric and Visualized Analysis of Tracheal Tissue Engineering Research. Tissue Eng. Part B Rev. 2024, 30, 198–216. [Google Scholar] [CrossRef] [PubMed]
- Butler, C.R.; Hynds, R.E.; Gowers, K.H.; Lee, D.D.H.; Brown, J.M.; Crowley, C.; Teixeira, V.H.; Smith, C.M.; Urbani, L.; Hamilton, N.J.; et al. Rapid Expansion of Human Epithelial Stem Cells Suitable for Airway Tissue Engineering. Am. J. Respir. Crit. Care Med. 2016, 194, 156–168. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.; Wang, C.; Qiao, Y.; Gu, J.; Zhang, H.; Peijs, T.; Kong, J.; Zhang, G.; Shi, X. Tissue-Engineered Trachea Consisting of Electrospun Patterned sc-PLA/GO- g-IL Fibrous Membranes with Antibacterial Property and 3D-Printed Skeletons with Elasticity. Biomacromolecules 2019, 20, 1765–1776. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.W.; Park, S.A.; Park, J.K.; Kim, Y.; Shin, Y.S.; Kim, C. Tissue-engineered tracheal reconstruction using three-dimensionally printed artificial tracheal graft: Preliminary report. Artif. Organs 2014, 38, E95–E105. [Google Scholar] [CrossRef]
- Park, J.H.; Hong, J.M.; Ju, Y.M.; Jung, J.W.; Kang, H.-W.; Lee, S.J.; Yoo, J.J.; Kim, S.W.; Kim, S.H.; Cho, D.-W. A novel tissue-engineered trachea with a mechanical behavior similar to native trachea. Biomaterials 2015, 62, 106–115. [Google Scholar] [CrossRef]
- Kobayashi, K.; Suzuki, T.; Nomoto, Y.; Tada, Y.; Miyake, M.; Hazama, A.; Wada, I.; Nakamura, T.; Omori, K. A tissue-engineered trachea derived from a framed collagen scaffold, gingival fibroblasts and adipose-derived stem cells. Biomaterials 2010, 31, 4855–4863. [Google Scholar] [CrossRef]
- Dikina, A.D.; Strobel, H.A.; Lai, B.P.; Rolle, M.W.; Alsberg, E. Engineered cartilaginous tubes for tracheal tissue replacement via self-assembly and fusion of human mesenchymal stem cell constructs. Biomaterials 2015, 52, 452–462. [Google Scholar] [CrossRef]
- Luo, X.; Liu, Y.; Zhang, Z.; Tao, R.; Liu, Y.; He, A.; Yin, Z.; Li, D.; Zhang, W.; Liu, W.; et al. Long-term functional reconstruction of segmental tracheal defect by pedicled tissue-engineered trachea in rabbits. Biomaterials 2013, 34, 3336–3344. [Google Scholar] [CrossRef]
- Remlinger, N.T.; Czajka, C.A.; Juhas, M.E.; Vorp, D.A.; Stolz, D.B.; Badylak, S.F.; Gilbert, S.; Gilbert, T.W. Hydrated xenogeneic decellularized tracheal matrix as a scaffold for tracheal reconstruction. Biomaterials 2010, 31, 3520–3526. [Google Scholar] [CrossRef]
- Bader, A.; Macchiarini, P. Moving towards in situ tracheal regeneration: The bionic tissue engineered transplantation approach. J. Cell. Mol. Med. 2010, 14, 1877–1889. [Google Scholar] [CrossRef]
- Kanzaki, M.; Yamato, M.; Hatakeyama, H.; Kohno, C.; Yang, J.; Umemoto, T.; Kikuchi, A.; Okano, T.; Onuki, T. Tissue engineered epithelial cell sheets for the creation of a bioartificial trachea. Tissue Eng. 2006, 12, 1275–1283. [Google Scholar] [CrossRef]
- Khalid, U.; Uchikov, P.; Hristov, B.; Kraev, K.; Koleva-Ivanova, M.; Kraeva, M.; Batashki, A.; Taneva, D.; Doykov, M.; Uchikov, A. Surgical Innovations in Tracheal Reconstruction: A Review on Synthetic Material Fabrication. Medicina 2024, 60, 40. [Google Scholar] [CrossRef]
- Shen, Z.; Sun, F.; Shan, Y.; Lu, Y.; Wu, C.; Zhang, B.; Wu, Q.; Yuan, L.; Zhu, J.; Wang, Q.; et al. Construction of a novel cell-free tracheal scaffold promoting vascularization for repairing tracheal defects. Mater. Today Bio. 2023, 23, 100841. [Google Scholar] [CrossRef]
- Kapat, K.; Gondane, P.; Kumbhakarn, S.; Takle, S.; Sable, R. Challenges and Opportunities in Developing Tracheal Substitutes for the Recovery of Long-Segment Defects. Macromol. Biosci. 2024, 24, e2400054. [Google Scholar] [CrossRef]
- Mizuno, K.; Ohnishi, H.; Kishimoto, Y.; Okuyama, H.; Kawai, Y.; Kitano, M.; Hayashi, Y.; Omori, K. Transplantation of Human Induced Pluripotent Stem Cell-Derived Airway Epithelia at Different Induction Stages into Nude Rat. Cell. Reprogram. 2024, 26, 156–163. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).