Nurses’ Perspectives of Geophagic Women of Childbearing Age Accessing Healthcare in the Reproductive Healthcare Services in Tshwane District, Gauteng Province: An Exploratory Study
Abstract
1. Introduction
2. Results
2.1. Socio-Demographics Information of Participants
2.2. The Nurses’ Perspectives Regarding Geophagic Women
2.2.1. Motivation by Food and Nutrition Deficiencies
“They lack proper knowledge and information on how to manage their cravings and deficiencies in their body”. “Most people do not understand how a human body functions, the nutrient, vitamin, and mineral deficiencies… they respond mostly to every desire they feel. They do not eat healthy food that are also rich in iron intake and clay soil causes them to lose appetite, some start developing iron deficiency symptoms… the person would become pale especially when you check their hands and nail” (A 50 years old professional nurse).
“They have iron deficiency. They lack knowledge of dealing with pregnancy cravings and sometimes, it is the issue of these patients taking the pills provided to them during the consultation and putting them at home without drinking them. Then when they experience shortage of iron in their bodies, they start with soil eating” (A 55 years old professional nurse).
2.2.2. Geophagic Practice Triggered by Mental Health and Substance Use Disorders
“In my assessment, I think they have some sort of mental health situation. It is some sort of abnormality. How can you eat soil? Something is wrong—they don’t think well. Yes because… We know that soil is associated with filth—we urinate there, we defecate there. So, how can a normal person take a decision to eat soil?” (A 42 years old professional nurse).
“I believe soil addiction has something to do with mental health disorder that occurs when one start experiencing uncontrollable cravings. People living with addictions find it difficult to resist the urge to feed their cravings. Other people start eating soil as a form of distraction and coping mechanism when they are faced with stressful situations that they scared to confront in their lives” (A 34 years old professional nurse).
2.2.3. Practice Caused by Iron Deficiency
“They have lack of iron (iron deficiency anaemia) and lack proper knowledge. They need to be taught about the dangers of eating clay soil because the pregnancy of someone who eat soil is different to the pregnancy of a patient who is not a consumer” (A 58 years old nurse).
“They have iron deficiency/anaemia mostly; hence they start craving clay soil. Such patients most have low (Hemoglobin) Hb” (A 39 years old enrolled nurse).
“They have anaemia, and they need assistance to prevent them to have a difficult pregnant journey” (A 56 years old professional nurse).
2.2.4. Ingestion Exacerbated by the Absence of Health Education and Promotion Programs on Geophagy
“They lack knowledge because soil eating can cause many unnecessary health conditions, sometimes people develop worms. There is a risk of developing appendicitis because of soil eating… so it is a dangerous practice that people are not aware of” (A 49 years old nursing assistant).
“I think they need assistance; they lack knowledge because they eat dirt. They risk having complications during their pregnancy. Some are mis-informed they eat soil thinking there are benefits” (A 58 years old professional nurse).
“I think it is lack of knowledge about the dangers of eating soil especially during pregnancy that leads women of childbearing age to practice geophagy” (A 41 years old registered nurse).
“They lack awareness of the health effects and dangers of eating soil” (A 55 years old nurse).
3. Discussion
4. Materials and Methods
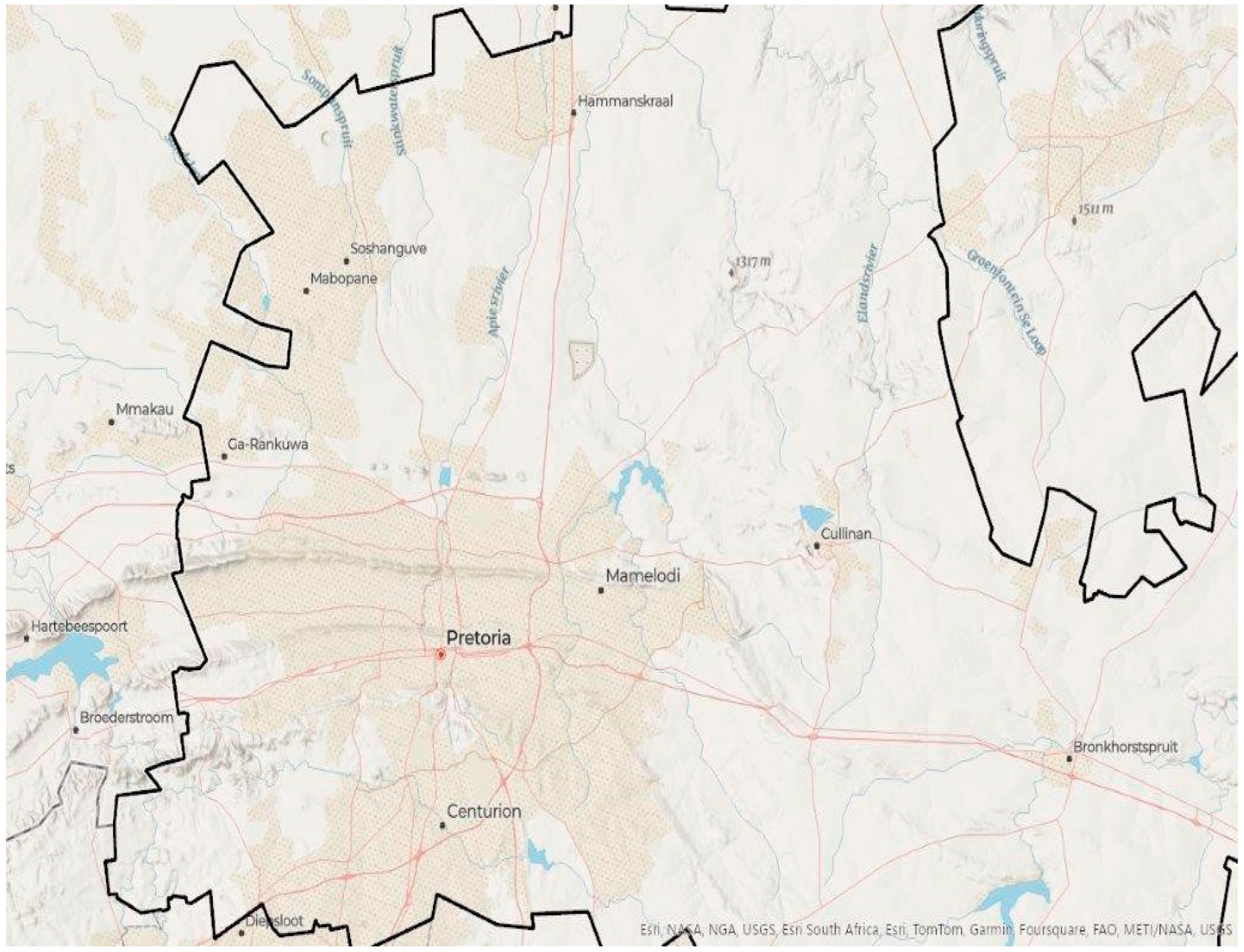
4.1. Study Setting
4.2. Study Design
4.3. Study Population
4.4. Sample Size and Sampling Technique
4.5. Recruitment
4.6. Data Collection Process
4.7. Data Analysis
4.8. Trustworthiness
4.9. Ethical Considerations
5. Conclusions
6. Study Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bernardo, B.; Candeias, C.; Rocha, F. Geophagic Materials Characterization and Potential Impact on Human Health: The Case Study of Maputo City (Mozambique). Appl. Sci. 2022, 12, 4832. [Google Scholar] [CrossRef]
- Kortei, N.K.; Koryo-Dabrah, A.; Akonor, P.T.; Manaphraim, N.Y.B.; Ayim-Akonor, M.; Boadi, N.O.; Essuman, E.K.; Tettey, C. Potential health risk assessment of toxic metals contamination in clay eaten as pica (geophagia) among pregnant women of Ho in the Volta Region of Ghana. BMC Pregnancy Childbirth 2020, 20, 160. [Google Scholar] [CrossRef] [PubMed]
- Mouri, H.; Malepe, R.E.; Candeias, C. Geochemical composition and potential health risks of geophagic materials: An example from a rural area in the Limpopo Province of South Africa. Environ. Geochem. Health 2023, 45, 6305–6322. [Google Scholar] [CrossRef]
- Pain, S.; Fauconneau, B.; Bouquet, E.; Vasse-Terrier, L.; Pérault-Pochat, M.-C. Severe craving associated with kaolin consumption. Eating and Weight Disorders-Studies on Anorexia. Bulim. Obes. 2019, 24, 379–381. [Google Scholar]
- Getachew, M.; Yeshigeta, R.; Tiruneh, A.; Alemu, Y.; Dereje, E.; Mekonnen, Z. Soil-transmitted helminthic infections and geophagia among pregnant women in Jimma town health institutions, Southwest Ethiopia. Ethiop. J. Health Sci. 2021, 31, 5. [Google Scholar] [CrossRef]
- Gupta, A. Geophagia: History, Epidemiology, and Etiology; CRC Press: Boca Raton, FL, USA, 2019. [Google Scholar]
- Malepe, R.E.; Candeias, C.; Mouri, H. Geophagy and its potential human health implications-A review of some cases from South Africa. J. Afr. Earth Sci. 2023, 200, 104848. [Google Scholar] [CrossRef]
- Islam, M.S.; De, A. Geophagy is a worldwide health hazard for pregnant women: A view. Res. Cardiovasc. Med. 2022, 11, 57. [Google Scholar]
- Mashao, U.; Ekosse, G.-I.; Odiyo, J.; Bukalo, N. Geophagic practice in Mashau Village, Limpopo Province, South Africa. Heliyon 2021, 7, e06497. [Google Scholar] [CrossRef] [PubMed]
- Kambunga, S.N.; Candeias, C.; Hasheela, I.; Mouri, H. Review of the nature of some geophagic materials and their potential health effects on pregnant women: Some examples from Africa. Environ. Geochem. Health 2019, 41, 2949–2975. [Google Scholar] [CrossRef] [PubMed]
- Narh, C.T.; Dzamalala, C.P.; Mmbaga, B.T.; Menya, D.; Mlombe, Y.; Finch, P.; Nyakunga, G.; Schüz, J.; McCormack, V.; Team, E. Geophagia and risk of squamous cell esophageal cancer in the African esophageal cancer corridor: Findings from the ESCCAPE multicountry case-control studies. Int. J. Cancer 2021, 149, 1274–1283. [Google Scholar] [CrossRef]
- Decaudin, P.; Kanagaratnam, L.; Kmiec, I.; Nguyen, Y.; Migault, C.; Lebrun, D.; Hentzien, M.; Bertin, E.; Drame, M.; Bani-Sadr, F. Prevalence of geophagy and knowledge about its health effects among native Sub-Saharan Africa, Caribbean and South America healthy adults living in France. Eating and Weight Disorders-Studies on Anorexia. Bulim. Obes. 2020, 25, 465–469. [Google Scholar]
- Phakoago, M.; Ekosse, G.; Odiyo, J. The prevalence of geophagic practices and causative reasons for geophagia in Sekhukhune area, Limpopo Province, South Africa. Trans. R. Soc. S. Afr. 2019, 74, 19–26. [Google Scholar] [CrossRef]
- Madziva, C.; Chinouya, M.J.; Njoroge, K. Experiences of geophagy during pregnancy among African migrant women in London: Implications for public health interventions. SSM-Qual. Res. Health 2024, 5, 100431. [Google Scholar] [CrossRef]
- Mireku, M.O.; Davidson, L.L.; Zoumenou, R.; Massougbodji, A.; Cot, M.; Bodeau-Livinec, F. Consequences of prenatal geophagy for maternal prenatal health, risk of childhood geophagy and child psychomotor development. Trop. Med. Int. Health 2018, 23, 841–849. [Google Scholar] [CrossRef]
- Bonglaisin, J.N.; Kunsoan, N.B.; Bonny, P.; Matchawe, C.; Tata, B.N.; Nkeunen, G.; Mbofung, C.M. Geophagia: Benefits and potential toxicity to human—A review. Front. Public Health 2022, 10, 893831. [Google Scholar] [CrossRef] [PubMed]
- Macheka, L.R.; Olowoyo, J.O.; Matsela, L.; Khine, A.A. Trace metals in blood and urine of pregnant women practicing geophagia at Dr. George Mukhari Academic Hospital, Pretoria, South Africa. Med. Technol. SA 2016, 30, 45–48. [Google Scholar]
- Mireku, M.O.; Cot, M.; Massougbodji, A.; Bodeau-Livinec, F. Relationship between stunting, wasting, underweight and geophagy and cognitive function of children. J. Trop. Pediatr. 2020, 66, 517–527. [Google Scholar] [CrossRef]
- Nakiyemba, O.; Obore, S.; Musaba, M.; Wandabwa, J.; Kiondo, P. Covariates of Pica among Pregnant Women Attending Antenatal Care at Kawempe Hospital, Kampala, Uganda: A Cross-Sectional Study. Am. J. Trop. Med. Hyg. 2021, 105, 909–914. [Google Scholar] [CrossRef]
- Davies, T.C. Current status of research and gaps in knowledge of geophagic practices in Africa. Front. Nutr. 2023, 9, 1084589. [Google Scholar] [CrossRef]
- Francis, S.; Jagadeesh, N.S.; Singaravelu, R.; Subramaniam, A. The influence of pica practice on nutritional status, stress and anxiety of pregnant women. Clin. Epidemiol. Glob. Health 2022, 17, 101133. [Google Scholar] [CrossRef]
- Ekosse, G.I.; Nkeng, G.E.; Bukalo, N.; Oyebanjo, O. Geophagic clays from cameroon: Provenance, metal contamination and health risk assessment. Int. J. Environ. Res. Public Health 2021, 18, 8315. [Google Scholar] [CrossRef] [PubMed]
- Kimassoum, D.; Ngum, N.L.; Bechir, M.; Haroun, A.; Tidjani, A.; Frazzoli, C. Geophagy: A survey on the practice of soil consumption in N’Djamena, Chad. J. Glob. Health Rep. 2023, 7, e2023010. [Google Scholar] [CrossRef]
- Norman, I.D.; Binka, F.N.; Godi, A.H. Geophagia: A cultural-nutrition health-seeking behaviour with no redeeming psycho-social qualities. South East. Eur. J. Public Health 2023, 3, 2014–2038. [Google Scholar] [CrossRef]
- Asim, M.; Ahmed, Z.H.; Nichols, A.R.; Rickman, R.; Neiterman, E.; Mahmood, A.; Widen, E.M. What stops us from eating: A qualitative investigation of dietary barriers during pregnancy in Punjab, Pakistan. Public Health Nutr. 2022, 25, 760–769. [Google Scholar] [CrossRef]
- Singh, P.K.; Dubey, R.; Singh, L.; Kumar, C.; Rai, R.K.; Singh, S. Public health interventions to improve maternal nutrition during pregnancy: A nationally representative study of iron and folic acid consumption and food supplements in India. Public Health Nutr. 2020, 23, 2671–2686. [Google Scholar] [CrossRef] [PubMed]
- Attarha, B.O.; Mikulic, S.; Harris, C.; Scolapio, J.S. Kaolin Clay Anemia. Cureus 2021, 13, e13796. [Google Scholar] [CrossRef]
- Onyenweaku, E.O. Geophagia in Nigeria: Perceptions and Practices of Pregnant Mothers versus Possible Health Outcomes. J. Gizi Dan Pangan 2023, 18, 187–196. [Google Scholar] [CrossRef]
- Madziva, C.; Chinouya, M.J. Clay ingestion during pregnancy among black African women in a north london borough: Understanding cultural meanings, integrating indigenous and biomedical knowledge systems. Front. Sociol. 2020, 5, 20. [Google Scholar] [CrossRef] [PubMed]
- Huebl, L.; Leick, S.; Guettl, L.; Akello, G.; Kutalek, R. Geophagy in Northern Uganda: Perspectives from consumers and clinicians. Am. J. Trop. Med. Hyg. 2016, 95, 1440. [Google Scholar] [CrossRef] [PubMed]
- Gebremichael, T.G.; Welesamuel, T.G. Adherence to iron-folic acid supplement and associated factors among antenatal care attending pregnant mothers in governmental health institutions of Adwa town, Tigray, Ethiopia: Cross-sectional study. PLoS ONE 2020, 15, e0227090. [Google Scholar] [CrossRef]
- Sanghvi, T.G.; Nguyen, P.H.; Forissier, T.; Ghosh, S.; Zafimanjaka, M.; Walissa, T.; Mahmud, Z.; Kim, S. Comprehensive Approach for Improving Adherence to Prenatal Iron and Folic Acid Supplements Based on Intervention Studies in Bangladesh, Burkina Faso, Ethiopia, and India. Food Nutr. Bull. 2023, 44, 183–194. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, T.; Roces, R.E.D.; Ladines-Llave, C.; Tuliao, M.T.R.; Kamau, M.W.; Yamada, C.; Tanaka, Y.; Shimazawa, K.; Iwamoto, S.; Matsuo, H. Maternal knowledge associated with the prevalence of iron and folic acid supplementation among pregnant women in Muntinlupa, Philippines: A cross-sectional study. Patient Prefer. Adherence 2021, 15, 501–510. [Google Scholar] [CrossRef] [PubMed]
- Moeti, T.; Mokhele, T.; Weir-Smith, G.; Dlamini, S.; Tesfamicheal, S. Factors Affecting Access to Public Healthcare Facilities in the City of Tshwane, South Africa. Int. J. Environ. Res. Public Health 2023, 20, 3651. [Google Scholar] [CrossRef] [PubMed]
- Geramian, N.; Gharaat, L.; Taheri, S.A.; Mohebpour, F.; Nahvizadeh, M.; Farajzadegan, Z.; Heidari, K. Development of a questionnaire to assess drug abuse among high school students of Isfahan province, Iran: An action research. Int. J. Prev. Med. 2014, 5 (Suppl. S2), S146. [Google Scholar] [CrossRef] [PubMed]
- Nowell, L.S.; Norris, J.M.; White, D.E.; Moules, N.J. Thematic analysis: Striving to meet the trustworthiness criteria. Int. J. Qual. Methods 2017, 16, 1609406917733847. [Google Scholar] [CrossRef]
- Cope, D.G. Methods and meanings: Credibility and trustworthiness of qualitative research. Oncol. Nurs. Forum 2014, 41, 89–91. [Google Scholar] [CrossRef] [PubMed]
| Variable | Frequency |
|---|---|
| Gender | |
| Male | 1 |
| Female | 19 |
| Age | |
| (30–39) | 6 |
| (40–49) | 5 |
| (50–59) | 8 |
| (60–69) | 1 |
| Marital status | |
| Single | 11 |
| Married | 8 |
| Divorced | 1 |
| Occupation | |
| Nursing assistant | 1 |
| Nurse | 5 |
| Registered nurse | 2 |
| Enrolled nurse | 4 |
| Professional nurse | 8 |
| Working experience in years | |
| (1–9) | 7 |
| (10–19) | 5 |
| (20–29) | 6 |
| (30–39) | 2 |
| Theme | Sub-Theme | Category |
|---|---|---|
| Motivation by food and nutrition deficiencies | Vitamins, minerals, and nutrients deficiencies | Nutritional factors |
| Low iron food intake | ||
| Geophagic practice triggered by mental health and substance use disorders | Underlying life problems | Psychosocial factors |
| Mental disorder challenges | ||
| Stress | ||
| Practice caused by iron deficiency | Low hemoglobin | Clinical factors |
| Increased desire for iron intake | ||
| Ingestion exacerbated by absence of Health Education and Promotion programs on geophagy | Lack of geophagy health education at antenatal care and family planning units | Community education factors |
| Lack of knowledge and understanding on the chemical composition of clay soil, geophagy potential health risks, and soil dangers. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malebatja, M.F.; Randa, M.B.; Mokgatle, M.M.; Oguntibeju, O.O. Nurses’ Perspectives of Geophagic Women of Childbearing Age Accessing Healthcare in the Reproductive Healthcare Services in Tshwane District, Gauteng Province: An Exploratory Study. Women 2024, 4, 541-551. https://doi.org/10.3390/women4040040
Malebatja MF, Randa MB, Mokgatle MM, Oguntibeju OO. Nurses’ Perspectives of Geophagic Women of Childbearing Age Accessing Healthcare in the Reproductive Healthcare Services in Tshwane District, Gauteng Province: An Exploratory Study. Women. 2024; 4(4):541-551. https://doi.org/10.3390/women4040040
Chicago/Turabian StyleMalebatja, Mohora Feida, Moreoagae Bertha Randa, Mathildah Mpata Mokgatle, and Oluwafemi Omoniyi Oguntibeju. 2024. "Nurses’ Perspectives of Geophagic Women of Childbearing Age Accessing Healthcare in the Reproductive Healthcare Services in Tshwane District, Gauteng Province: An Exploratory Study" Women 4, no. 4: 541-551. https://doi.org/10.3390/women4040040
APA StyleMalebatja, M. F., Randa, M. B., Mokgatle, M. M., & Oguntibeju, O. O. (2024). Nurses’ Perspectives of Geophagic Women of Childbearing Age Accessing Healthcare in the Reproductive Healthcare Services in Tshwane District, Gauteng Province: An Exploratory Study. Women, 4(4), 541-551. https://doi.org/10.3390/women4040040






