Impact of the Treatment of Serenoa repens, Solanum lycopersicum, Lycopene and Bromelain in Combination with Alfuzosin for Benign Prostatic Hyperplasia. Results from a Match-Paired Comparison Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Statement of Human Rights
2.2. Patients Selection
2.3. Study Design and Clinical Outcomes
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Roehrborn, C.G. Male Lower Urinary Tract Symptoms (LUTS) and Benign Prostatic Hyperplasia (BPH). Med. Clin. N. Am. 2011, 95, 87–100. [Google Scholar] [CrossRef]
- Russo, A.; Capogrosso, P.; La Croce, G.; Ventimiglia, E.; Boeri, L.; Briganti, A.; Damiano, R.; Montorsi, F.; Salonia, A. Serenoa repens, selenium and lycopene to manage lower urinary tract symptoms suggestive for benign prostatic hyperplasia. Expert Opin. Drug Saf. 2016, 15, 1661–1670. [Google Scholar] [CrossRef]
- Abdollah, F.; Briganti, A.; Suardi, N.; Castiglione, F.; Gallina, A.; Capitanio, U.; Montorsi, F. Metabolic Syndrome and Benign Prostatic Hyperplasia: Evidence of a Potential Relationship, Hypothesized Etiology, and Prevention. Korean J. Urol. 2011, 52, 507–516. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tindall, D.J.; Rittmaster, R.S. The Rationale for Inhibiting 5α-Reductase Isoenzymes in the Prevention and Treatment of Prostate Cancer. J. Urol. 2008, 179, 1235–1242. [Google Scholar] [CrossRef] [Green Version]
- Manohar, C.M.S.; Nagabhushana, M.; Karthikeyan, V.S.; Sanjay, R.P.; Kamath, A.J.; Keshavamurthy, R. Safety and efficacy of tamsulosin, alfuzosin or silodosin as monotherapy for LUTS in BPH—a double-blind randomized trial. Cent. Eur. J. Urol. 2017, 70, 148–153. [Google Scholar]
- Pagano, E.; Laudato, M.; Griffo, M.; Capasso, R. Phytotherapy of Benign Prostatic Hyperplasia. A Minireview. Phytother. Res. 2013, 28, 949–955. [Google Scholar] [CrossRef] [PubMed]
- Cicero, A.F.; Allkanjari, O.; Busetto, G.M.; Cai, T.; Larganà, G.; Magri, V.; Perletti, G.; Della Cuna, F.S.R.; Russo, G.I.; Stamatiou, K.; et al. Nutraceutical treatment and prevention of benign prostatic hyperplasia and prostate cancer. Arch. Ital. Urol. Androl. 2019, 91. [Google Scholar] [CrossRef] [PubMed]
- Di Maida, F.; Mari, A.; Rubino, R.; Minervini, A.; Carini, M.; Siena, G. A Prospective, Open-Label Comparison of Tamsulosin plus Serenoa repens and Bovine Colostrum versus Tamsulosin Alone in the Treatment of Benign Prostatic Hyperplasia. Urol. Int. 2020, 104, 351–355. [Google Scholar] [CrossRef]
- Vella, M.; Abrate, A.; Costanzo, A.; D’Amato, F.; Tarantino, M.L.; Simonato, A. Predictive variables of spontaneous micturition recovery after acute urinary retention in men with benign prostatic enlargement: An observational prospective study. LUTS Low. Urin. Tract Symptoms 2018, 11, 104–108. [Google Scholar] [CrossRef]
- Vela-Navarrete, R.; Alcaraz, A.; Rodríguez-Antolín, A.; López, B.M.; Fernández-Gómez, J.M.; Angulo, J.C.; Diaz, D.C.; Romero-Otero, J.; Brenes, F.J.; Carballido, J.; et al. Efficacy and safety of a hexanic extract of Serenoa repens (Permixon®) for the treatment of lower urinary tract symptoms associated with benign prostatic hyperplasia (LUTS/BPH): Systematic review and meta-analysis of randomised controlled trials and obser. BJU Int. 2018, 122, 1049–1065. [Google Scholar] [CrossRef] [Green Version]
- Morgia, G.; Russo, G.I.; Voce, S.; Palmieri, F.; Gentile, M.; Giannantoni, A.; Blefari, F.; Carini, M.; Minervini, A.; Ginepri, A.; et al. Serenoa repens, lycopene and selenium versus tamsulosin for the treatment of LUTS/BPH. An Italian multicenter double-blinded randomized study between single or combination therapy (PROCOMB trial). Prostate 2014, 74, 1471–1480. [Google Scholar] [CrossRef] [PubMed]
- Morgia, G.; Cimino, S.; Favilla, V.; Russo, G.I.; Squadrito, F.; Mucciardi, G.; Masieri, L.; Minutoli, L.; Grosso, G.; Castelli, T. Effects of Serenoa repens, selenium and lycopene (Profluss®) on chronic inflammation associated with benign prostatic hyperplasia: Results of “FLOG” (Flogosis and Profluss in Prostatic and Genital Disease), a multicentre Italian study. Int. Braz. J. Urol. 2013, 39, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Morgia, G.; Mucciardi, G.; Galì, A.; Madonia, M.; Marchese, F.; Di Benedetto, A.; Romano, G.; Bonvissuto, G.; Castelli, T.; Macchione, L.; et al. Treatment of chronic prostatitis/chronic pelvic pain syndrome category IIIA with Serenoa repens plus selenium and lycopene (Profluss) versus S. repens alone: An Italian randomized multicenter-controlled study. Urol. Int. 2010, 84, 400–406. [Google Scholar] [CrossRef]
- Palin, M.-F.; Faguy, M.; Lehoux, J.-G.; Pelletier, G. Inhibitory Effects of Serenoa repens on the Kinetic of Pig Prostatic Microsomal 5α-Reductase Activity. Endocrine 1998, 9, 65–70. [Google Scholar] [CrossRef]
- Kaplan, S.A. Re: Serenoa repens for Lower Urinary Tract Symptoms/Benign Prostatic Hyperplasia: Current Evidence and its Clinical Implications in Naturopathic Medicine. J. Urol. 2018, 199, 1372–1373. [Google Scholar] [CrossRef]
- Perry, R.; Milligan, G.; Anderson, P.; Gillon, A.; White, M. Real-World Use of Permixon® in Benign Prostatic Hyperplasia—Determining Appropriate Monotherapy and Combination Treatment. Adv. Ther. 2012, 29, 538–550. [Google Scholar] [CrossRef]
- Macdonald, R.; Tacklind, J.W.; Rutks, I.; Wilt, T.J. Serenoa repens monotherapy for benign prostatic hyperplasia (BPH): An updated Cochrane systematic review. BJU Int. 2012, 109, 1756–1761. [Google Scholar] [CrossRef] [PubMed]
- Morgia, G.; Vespasiani, G.; Pareo, R.M.; Voce, S.; Madonia, M.; Carini, M.; Ingrassia, A.; Terrone, C.; Gentile, M.; Carrino, M.; et al. Serenoa repens + selenium + lycopene vs tadalafil 5 mg for the treatment of lower urinary tract symptoms secondary to benign prostatic obstruction: A Phase IV, non-inferiority, open-label, clinical study (SPRITE study). BJU Int. 2018, 122, 317–325. [Google Scholar] [CrossRef] [Green Version]
- Cai, T.; Cui, Y.; Yu, S.; Li, Q.; Zhou, Z.; Gao, Z. Comparison of Serenoa repens with Tamsulosin in the Treatment of Benign Prostatic Hyperplasia: A Systematic Review and Meta-Analysis. Am. J. Men’s Health 2020, 14, 155798832090540. [Google Scholar] [CrossRef]
- Barry, M.J.; Meleth, S.; Lee, J.Y.; Kreder, K.J.; Avins, A.L.; Nickel, J.C.; Roehrborn, C.G.; Crawford, E.D.; Foster, H.E., Jr.; Kaplan, S.A.; et al. Effect of increasing doses of saw palmetto extract on lower urinary tract symptoms: A randomized trial. JAMA—J. Am. Med. Assoc. 2011, 306, 1344–1351. [Google Scholar] [CrossRef] [Green Version]
- Andriole, G.L.; McCullum-Hill, C.; Sandhu, G.S.; Crawford, E.D.; Barry, M.J.; Cantor, A. CAMUS Study Group the Effect of Increasing Doses of Saw Palmetto Fruit Extract on Serum Prostate Specific Antigen: Analysis of the CAMUS Randomized Trial. J. Urol. 2013, 189, 486–492. [Google Scholar] [CrossRef] [PubMed]
- Ryu, Y.W.; Lim, S.W.; Kim, J.H.; Ahn, S.H.; Choi, J.D. Comparison of Tamsulosin Plus Serenoa repens with Tamsulosin in the Treatment of Benign Prostatic Hyperplasia in Korean Men: 1-Year Randomized Open Label Study. Urol. Int. 2015, 94, 187–193. [Google Scholar] [CrossRef]
- Hızlı, F.; Uygur, M.C. A prospective study of the efficacy of Serenoa repens, Tamsulosin, and Serenoa repens plus Tamsulosin treatment for patients with benign prostate hyperplasia. Int. Urol. Nephrol. 2007, 39, 879–886. [Google Scholar] [CrossRef]
- Argirović, A.; Argirović, D. da li dodavanje Serenoa repens tamsulosinu poboljšava njegovu terapeutsku efikasnost kod benigne hiperplazije prostate? Vojn. Pregl. 2013, 70, 1091–1096. [Google Scholar]
- Busetto, G.M.; Giovannone, R.; Antonini, G.; Rossi, A.; Del Giudice, F.; Tricarico, S.; Ragonesi, G.; Gentile, V.; De Berardinis, E. Short-term pretreatment with a dual 5α-reductase inhibitor before bipolar transurethral resection of the prostate (B-TURP): Evaluation of prostate vascularity and decreased surgical blood loss in large prostates. BJU Int. 2014, 116, 117–123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Latil, A.; Libon, C.; Templier, M.; Junquero, D.; Lantoine-Adam, F.; Nguyen, T. Hexanic lipidosterolic extract of Serenoa repens inhibits the expression of two key inflammatory mediators, MCP-1/CCL2 and VCAM-1, in vitro. BJU Int. 2012, 110, e1470–e1474. [Google Scholar] [CrossRef] [PubMed]
- Strum, S.B. Serenoa repens (Saw Palmetto) for Lower Urinary Tract Symptoms (LUTS): The Evidence for Efficacy and Safety of Lipidosterolic Extracts. Part III. Uro 2021, 1, 155–179. [Google Scholar] [CrossRef]
- Busetto, G.M.; Giovannone, R.; Ferro, M.; Tricarico, S.; Del Giudice, F.; Deliu, V.M.; De Cobelli, O.; Gentile, V.; De Berardinis, E. Chronic bacterial prostatitis: Efficacy of short-lasting antibiotic therapy with prulifloxacin (Unidrox®) in association with saw palmetto extract, lactobacillus sporogens and arbutin (Lactorepens®). BMC Urol. 2014, 14, 53. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.H.; Baek, M.J.; Sun, H.Y.; Lee, B.; Li, S.; Khandwala, Y.; Del Giudice, F.; Chung, B.I. Efficacy and safety of 5 alpha-reductase inhibitor monotherapy in patients with benign prostatic hyperplasia: A meta-analysis. PLoS ONE 2018, 13, e0203479. [Google Scholar] [CrossRef]
- Ford, N.A.; Elsen, A.C.; Zuniga, K.; Lindshield, B.L.; Erdman, J. Lycopene and Apo-12′-Lycopenal Reduce Cell Proliferation and Alter Cell Cycle Progression in Human Prostate Cancer Cells. Nutr. Cancer 2011, 63, 256–263. [Google Scholar] [CrossRef]



| Clinical Features | Treatment Group (Af + SeR + SL + Ly + Br) (n = 125) | Control Group (Af) (n = 125) | p-Value |
|---|---|---|---|
| Age (median, IQR) | 61 (52–69) | 63 (53–70) | 0.57 |
| N° of daytime micturition (median, IQR) | 8 (6–9) | 8 (6–10) | 0.37 |
| N° of night-time micturition (median, IQR) | 3 (1–4) | 2 (1–4) | 0.77 |
| Prostate volume (cc) (median, IQR) | 51 (33–68) | 52 (35–69) | 0.39 |
| Qmax (mL/s) (median, IQR) | 11.3 (10–15) | 12.5 (11–14) | 0.48 |
| Qave (mL/s) (median, IQR) | 11 (10–12) | 10 (9–12) | 0.36 |
| PVR (cc) (median, IQR) | 127 (98–139) | 125 (96–143) | 0.68 |
| Total PSA (ng/mL) (median, IQR) | 3.4 (2.2–4.2) | 3.6 (2.5–4.6) | 0.52 |
| Total IPSS (median, IQR) | 17 (14–19) | 15 (13–17) | 0.74 |
| Storage subscore (median, IQR) | 7(4–9) | 7 (5–9) | 0.85 |
| Voiding subscore (median, IQR) | 9 (6–11) | 10 (8–13) | 0.72 |
| IPSS-QoL (median, IQR) | 4 (3–5) | 4 (4–6) | 0.88 |
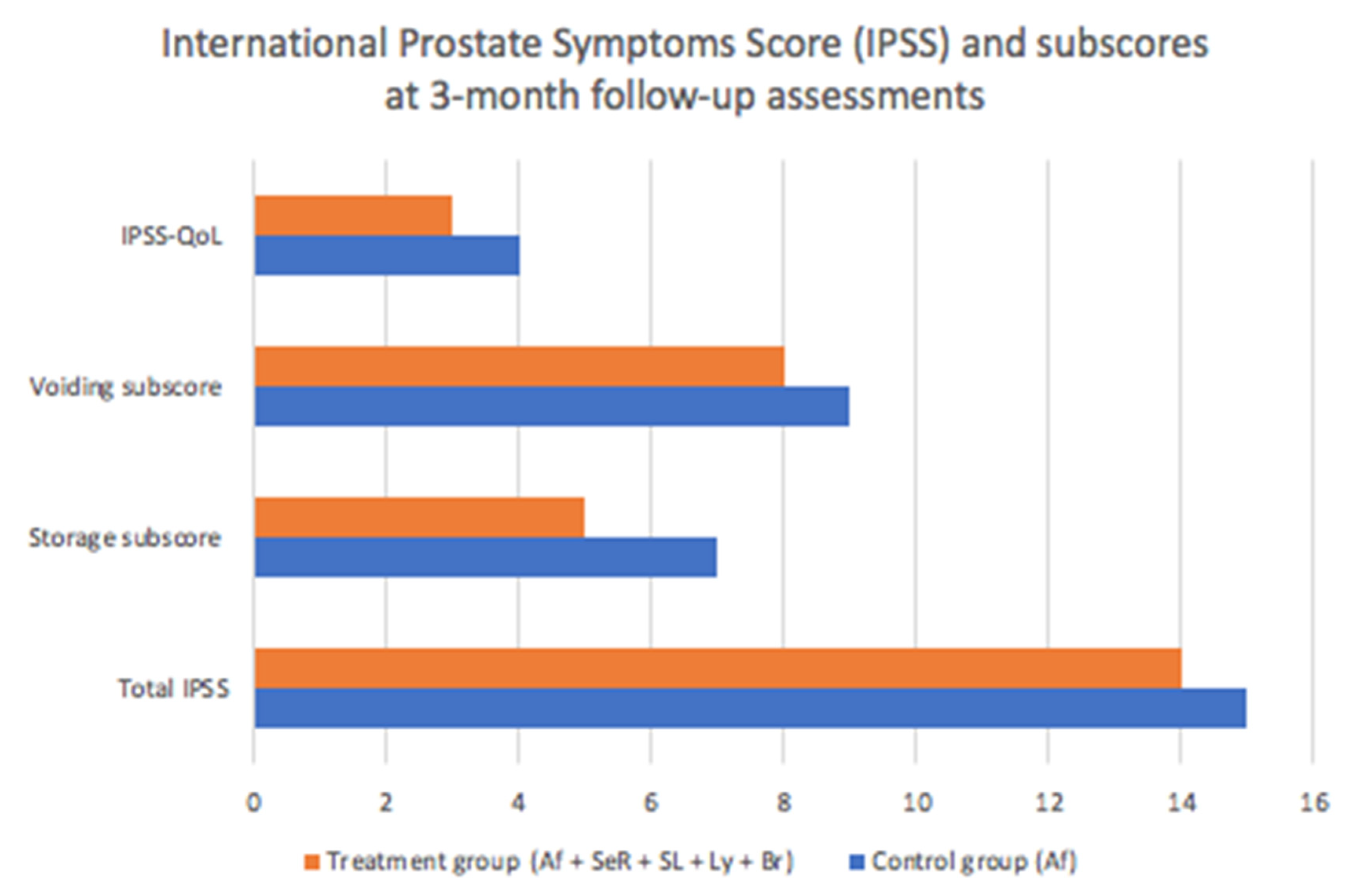
| Patients Reporting Questionnaires a | Control Group (Af) (n = 125) | Treatment Group (Af + SeR + SL + Ly + Br) (n = 125) | p-Value |
| Total IPSS (median, IQR) | 15 (11–18) | 14 (10–16) | 0.07 |
| Storage subscore (median, IQR) | 7 (5–9) | 5(4–9) | 0.03 |
| Voiding subscore (median, IQR) | 9 (7–11) | 8 (6–9) | 0.06 |
| IPSS-QoL (median, IQR) | 4 (4–6) | 3 (2–4) | 0.05 |
| Patients Reporting Questionnaires b | Control Group (Af) (n = 125) | Treatment Group (Af + SeR + SL + Ly + Br) (n = 125) | p-Value |
| Total IPSS (median, IQR) | 15 (12–20) | 12 (9–14) | 0.02 |
| Storage subscore (median, IQR) | 7 (4–9) | 4 (2–7) | 0.001 |
| Voiding subscore (median, IQR) | 8 (6–10) | 6 (3–9) | 0.03 |
| IPSS-QoL (median, IQR) | 4 (4–6) | 2 (1–4) | 0.001 |
| Clinical Features a | Control Group (Af) (n = 125) | Treatment Group (Af + SeR + SL + Ly + Br) (n = 125) | p-Value |
| N° of daytime micturition (median, IQR) | 8 (6–11) | 7 (6–9) | 0.07 |
| N° of nighttime micturition (median, IQR) | 2 (1–4) | 1 (1–2) | 0.03 |
| Prostate volume (cc) (median, IQR) | 52 (42–64) | 50 (43–63) | 0.39 |
| Qmax (mL/s) (median, IQR) | 13.4 (11–15) | 14.9 (12–18) | 0.08 |
| Qave (mL/s) (median, IQR) | 10 (8–12) | 11.5 (10–14) | 0.09 |
| PVR (cc) (median, IQR) | 119 (96–143) | 112 (75–140) | 0.05 |
| PSA (ng/mL) (median, IQR) | 3.6 (2.5–4.6) | 3.1 (1.8–4.2) | 0.07 |
| Clinical Features b | Control Group (Af) (n = 125) | Treatment Group (Af + SeR + SL + Ly + Br) (n = 125) | p-Value |
| N° of daytime micturition (median, IQR) | 8 (6–11) | 6 (5–9) | 0.04 |
| N° of nighttime micturition (median, IQR) | 2 (1–4) | 1 (1–2) | 0.03 |
| Prostate volume (cc) (median, IQR) | 52 (40–62) | 51 (39–62) | 0.41 |
| Qmax (mL/s) (median, IQR) | 13.8 (12–16) | 16.7 (13–19) | 0.001 |
| Qave (mL/s) (median, IQR) | 12 (10–14) | 14.2 (10–16) | 0.05 |
| PVR (cc) (median, IQR) | 109 (99–123) | 102 (91–116) | 0.02 |
| PSA (ng/mL) (median, IQR) | 3.6 (2.5–4.6) | 2.9 (1.9–3.8) | 0.04 |
| Adverse Events | Treatment Group (Af + SeR + SL + Ly + Br) * (n = 125) | Control Group (Af) (n = 125) | p Value |
|---|---|---|---|
| Total, n (%) | 16 (13%) | 15 (12%) | 0.84 |
| Ejaculatory disorders | 6 (4.9%) | 6 (4.8%) | 0.92 |
| Postural hypotension | 3 (2.4%) | 4 (3.2%) | 0.78 |
| Headache | 4 (3.3%) | 2 (1.6%) | 0.59 |
| Stomach upset | 3 (2.4%) | 1 (0.8%) | 0.31 |
| Dry mouth | 1 (0.8%) | 2 (1.6%) | 0.42 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lambertini, L.; Di Maida, F.; Tellini, R.; Bisegna, C.; Valastro, F.; Grosso, A.A.; Scelzi, S.; Del Giudice, F.; Ferro, M.; Pirola, G.M.; et al. Impact of the Treatment of Serenoa repens, Solanum lycopersicum, Lycopene and Bromelain in Combination with Alfuzosin for Benign Prostatic Hyperplasia. Results from a Match-Paired Comparison Analysis. Uro 2021, 1, 228-237. https://doi.org/10.3390/uro1040025
Lambertini L, Di Maida F, Tellini R, Bisegna C, Valastro F, Grosso AA, Scelzi S, Del Giudice F, Ferro M, Pirola GM, et al. Impact of the Treatment of Serenoa repens, Solanum lycopersicum, Lycopene and Bromelain in Combination with Alfuzosin for Benign Prostatic Hyperplasia. Results from a Match-Paired Comparison Analysis. Uro. 2021; 1(4):228-237. https://doi.org/10.3390/uro1040025
Chicago/Turabian StyleLambertini, Luca, Fabrizio Di Maida, Riccardo Tellini, Claudio Bisegna, Francesca Valastro, Antonio Andrea Grosso, Sabino Scelzi, Francesco Del Giudice, Matteo Ferro, Giacomo Maria Pirola, and et al. 2021. "Impact of the Treatment of Serenoa repens, Solanum lycopersicum, Lycopene and Bromelain in Combination with Alfuzosin for Benign Prostatic Hyperplasia. Results from a Match-Paired Comparison Analysis" Uro 1, no. 4: 228-237. https://doi.org/10.3390/uro1040025
APA StyleLambertini, L., Di Maida, F., Tellini, R., Bisegna, C., Valastro, F., Grosso, A. A., Scelzi, S., Del Giudice, F., Ferro, M., Pirola, G. M., Gubbiotti, M., Masieri, L., Busetto, G. M., de Cobelli, O., Minervini, A., & Mari, A. (2021). Impact of the Treatment of Serenoa repens, Solanum lycopersicum, Lycopene and Bromelain in Combination with Alfuzosin for Benign Prostatic Hyperplasia. Results from a Match-Paired Comparison Analysis. Uro, 1(4), 228-237. https://doi.org/10.3390/uro1040025









