1. Introduction
Asthma has a prevalence of 10% and is therefore the most frequent chronic disease in childhood, commonly inciting at the age of 3 to 5 years [
1]. Hospital admissions for acute asthma are responsible for up to 10–15% of all childhood admissions, especially in peak seasons [
2,
3,
4,
5,
6]. In asthmatic children, severe airflow limitation caused by airway narrowing can rapidly develop as the airways are relatively small and easily obstructed by mucus and bronchospasms [
2]. Acute standard therapy is mostly supportive with oxygen and inhaled bronchodilators, the efficacy of which is compromised by the severe airflow limitation [
2].
During strenous exercise in cold, dry air hyperpnoea will transiently dehydrate a large number of airways. In asthmatic children the osmotisch stimulus created will shrink the inflammatory cells residing in the airways leading to the release of inflammatory mediators [
7,
8]. These mediators induce bronchoconstriction, airway wall edema and excessive mucus production resulting in airway narrowing and the classic asthmatic symptoms of wheezing, cough and dyspnea. Exercise-induced asthma (EIA) symptoms are usually short-lived, resolving in 15–30 min, as the provoking stimulus is transient. During an asthma attack, the same inflammatory mediators are released as in EIA, and the airway narrowing is similarly reversible to bronchodilators. Imaging studies in EIA showed ventilation defects as is known from asthma attacks, probably also due to mucus plugged in constricted airways. An exercise challenge test is therefore a suitable method to investigate mechanisms of asthma [
9].
High flow nasal cannula (HFNC) therapy is a non-invasive oxygen delivery mode which is safe and well tolerated by adults and children with respiratory distress [
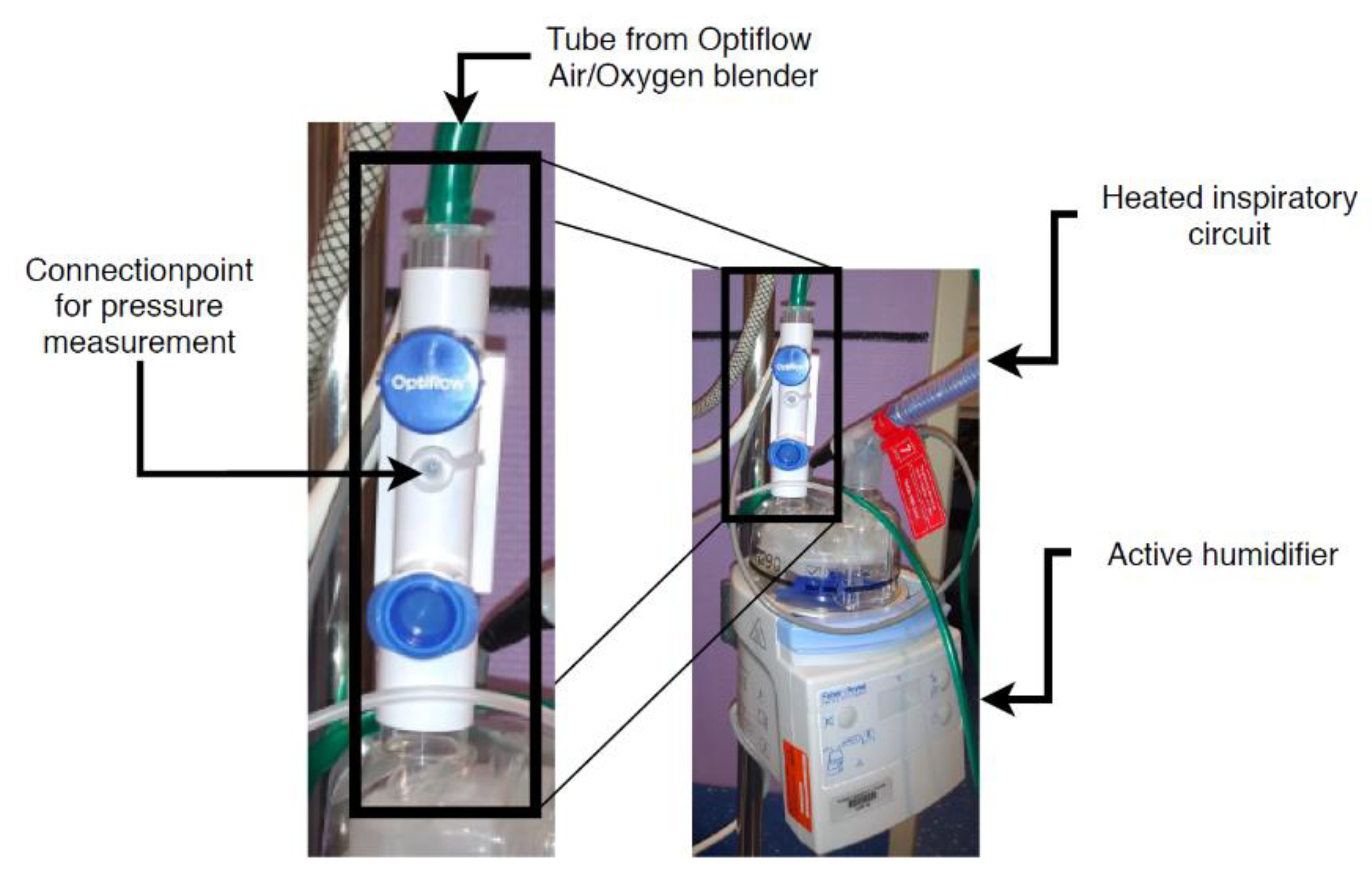
3]. HFNC therapy delivers pressurized warmed and moisturized air (see
Figure 1). It is possible to enrich the warmed moisturized air with oxygen.
Although some recent retrospective reports suggest HFNC therapy is effective for acute asthma in a pediatric intensive care unit (PICU) [
4,
5,
6], the effectiveness and working mechanism of this therapy in acute childhood asthma is not yet established. Ballestero et al. [
10] found a faster pulmonary recovery in children with acute asthma treated with HFNC compared to standard therapy, but this is the only prospective pilot study to date.
The proposed mechanism of HFNC with no additional oxygen on asthma is twofold:
To attain the preset airflow, the HFNC device adjusts the pressure that is delivered to the patient. We anticipate that the required pressure to deliver the preset airflow will increase if the airways narrow due to an asthmatic response. This will result in a negative relationship between the effectiveness of the therapy and the delivered pressure.
Objective of this study
The study has two objectives:
To investigate whether HFNC therapy in asthmatic children quickens the recovery of lung function in children undergoing a drop in lung function during an exercise challenge test;
To relate the recovery of lung function to a change of pressure used by HFNC device after an exercise induced drop in lung function.
2. Materials and Methods
In this study, the effect of HFNC therapy compared to spontaneous recovery is assessed during an ECT. The Optiflow® of Fisher and Paykel® is used to provide HFNC therapy. The air is humidified with the MR850 Respiratory Humidifier and delivered through nasal interfaces, both products are also from Fisher and Paykel®.
The Optiflow has a standard connection point for pressure measurements (see
Figure 2).
The pressure sensor in this study is the Omega, model: PXM409–070HCGUSBH. The sensor connects to the Optiflow with a perfusion line. The perfusion line is a dead arm connected to the Optiflow system and does not affect the therapy. Omega Digital Transducer Appliction Software logs measurements from the pressure sensor with 160 samples per second. The lung function of the children is monitored with FEV1 measurements with the Vyaire Spiro meter. For the exercise challenge test, we use a climate controlled chamber dedicated for this purpose. The air in this chamber is dry and has a temperature of 10 °C. As exercise, the children can choose between running on a treadmill or jumping in an inflatable bouncing castle.
2.1. Study Population and Size
Children, aged 6–18 years, that previously performed a standard ECT with a FEV1 lability of ≥30% are included in this study. It is expected that HFNC therapy will speed up the recovery of an exercise-induced decline in lung function. We hypothesize that the recovery time to normal lung function will be halved using HFNC, which is considered to be clinically relevant. Pulmonary function recovers within 15–20 min in most 3–7 years old children and spontaneous recovery is most often nearly completed within 30 min [
11,
12]. Sample size analysis is performed with t-test of SPSS version 3.1.6. with a paired design [
13]. The power is set to 80% and the significance level (α) 5%. It is estimated that the effect size is 50%, based on a mean recovery rate of 10 min when using HFNC therapy and 20 min for spontaneous recovery. The within group standard deviation is 12.5 min. Therefore, a minimum of 14 patients are necessary to obtain significant results.
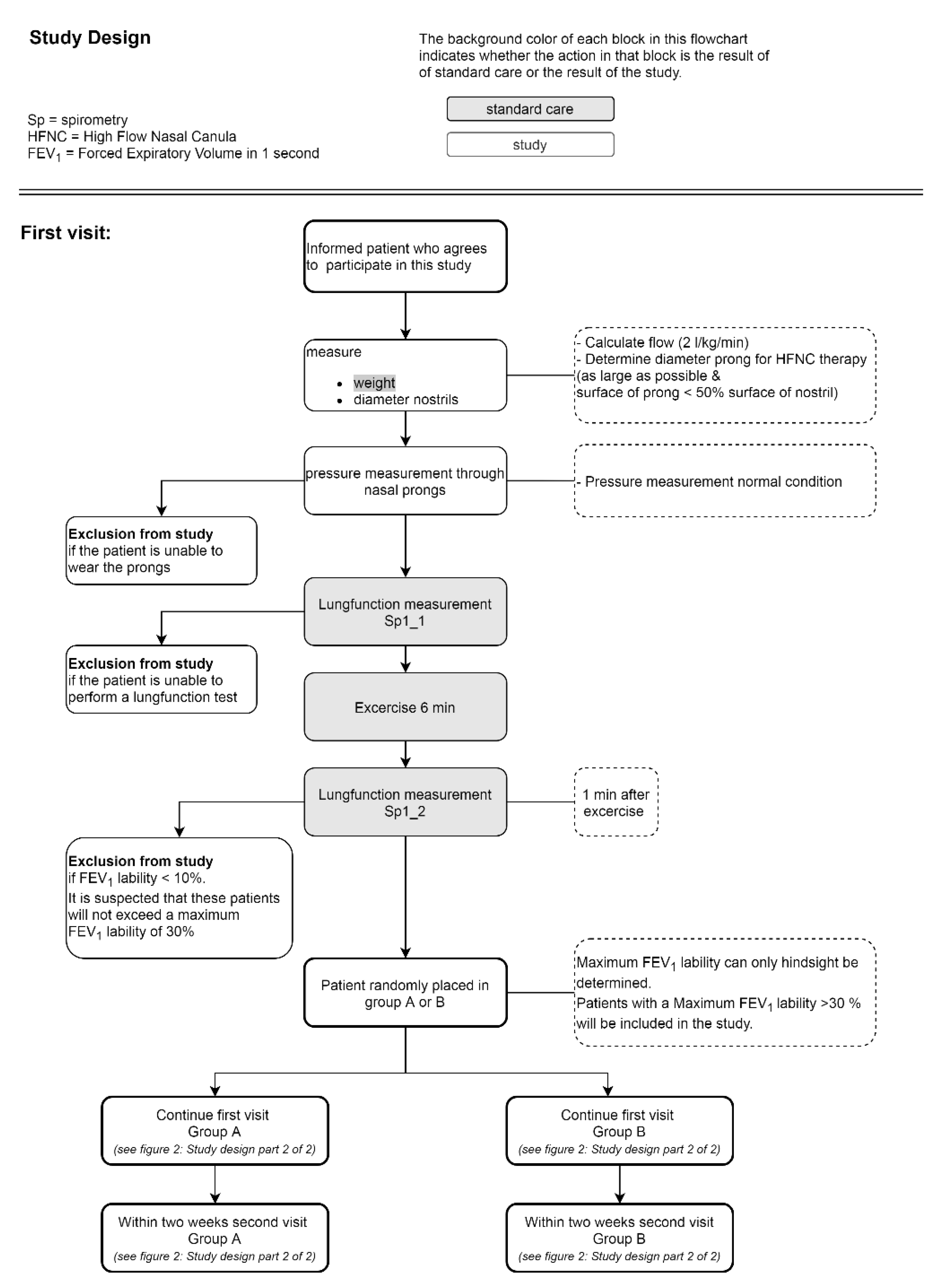
2.2. Study Design
This study is a prospective crossover study, implying that each child has to perform the ECT twice during two separate hospital visits. One ECT with spontaneous recovery and one ECT with HFNC therapy. To minimize the burden on the children who are participating in this study, we use the hospital visit that is part of the standard care the obtain the spontaneous recovery measurements. During this visit, the fall of FEV
1 and its reversibility during the ECT with spontaneous recovery is used to diagnose the severity of the asthma. In addition, a pressure measurement in the nasal airways is performed, using the prongs of the HFNC device. At set times, lung function tests are performed (see
Figure 3). Lung function is measured using spirometry. For each lung function measurement spirometry is performed twice in a row. The ECTs are performed on different days within two weeks from each other at approximately the same time of the day. The order in which the tests are performed is randomly distributed over the different days. The study design is graphically represented in
Figure 3 and
Figure 4.
3. Results
The primary endpoints of this study are the recovery of lung function assessed with spirometry measurements and the duration to fully recovered lung function after ECT within 10% of baseline FEV1. These are numerical parameters and will be compared between the unpaired groups using an unpaired T-test. To allow for comparison between patients, the lung function measurement is expressed as a change in percentage compared to baseline.
The pressure values during HFNC therapy are evaluated using the Pearson correlation if the measured values are normally distributed. Otherwise the Spearman correlation is used.
The patients will be included in the summer of 2021.
4. Discussion
An exercise challenge test is an indirect bronchoprovocation challenge test and thus inducing airway narrowing through the inflammatory pathway. Osmolar and thermal processes in the airways caused by exercise-induced hyperpnoe induce the release of inflammatory mediators [
14] similar to an asthma attack in daily life. This type of provocation is more suitable to simulate an asthma attack than a pharmacologically induced asthma attack (direct challenge with metacholine, histamine) which directly stimulates specific receptors on the airway smooth muscle cells. Another advantage of the exercise challenge test over a direct challenge is the relatively common, not unfamiliar and short-lived burden for the children. The exercise-induced asthma attack occurs within minutes after exercise and a child usually recovers from it within 15 min. Asthmatic children have similar experiences in daily life as they are physically active with frequent, spontaneous bouts of exercise at high intensity. In our experience, this pattern of behavior results in frequent transient episodes of airway narrowing, which usually do not constrain them from being physically active. The exercise challenge test has proven to be a valid model to investigate asthma with good repeatability [
15], especially in moderate to severe asthmatic responses. It is therefore truly suitable to investigate potential mechanisms and treatments for asthma.
Author Contributions
R.D.t.W. initiated the study and compiled the protocol including the approval from the Ethics Committee. B.J.T. supervised the project. Both authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study will be conducted according to the guidelines of the Declaration of Helsinki, and is approved by the Ethics Committee MEC-U (protocol code NL75416.100.20, date of approval: 3 May 2021).
Informed Consent Statement
Informed consent will be obtained from all subjects involved in the study.
Data Availability Statement
Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Wijga, A.H.; Buul, L.W.; van Blokstra, A.; Wolse, A.P.H. Astma Bij Kinderen Tot 12 Jaar. In RIVM Rapport 260384001/2011; RIVM: Bilthoven, The Nederland, 2011. [Google Scholar]
- Tinitinallis, J.E. Pediatrics. In Tintinalli’s Emergency Medicine, 7th ed.; McGraw Hill: New York, NY, USA, 2011; pp. 731–988. [Google Scholar]
- Nishimura, M. High-Flow Nasal Cannula Oxygen Therapy Devices. Respir. Care 2019, 64, 735–742. [Google Scholar] [CrossRef] [PubMed]
- Martínez, F.G.; Sánchez, M.I.; Del Castillo, B.T.; Moreno, J.P.; Muñoz, M.M.; Jiménez, C.R.; Fernández, R.R. Treatment with high-flow oxygen therapy in asthma exacerbations in a paediatric hospital ward: Experience from 2012 to 2016. An. Pediatra 2019, 90, 72–78. [Google Scholar]
- Alcock, A.; Thompson, C.; Robertson, R.; Ali, T. G500(P) An examination of the safety and efficacy of high flow nasal cannula therapy for acute severe asthma and viral induced wheeze in paediatric critical care. Arch. Dis. Child. 2016, 101, A296–A297. [Google Scholar] [CrossRef]
- Baudin, F.; Buisson, A.; Vanel, B.; Massenavette, B.; Pouyau, R.; Javouhey, E. Nasal high flow in management of children with status asthmaticus: A retrospective observational study. Ann. Intensive Care 2017, 7, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Anderson, S.D.; Daviskas, E. The mechanism of exercise-induced ashtma is. J. Allergy Clin. Immunol. 2000, 106, 453–459. [Google Scholar] [CrossRef] [PubMed]
- Weiler, J.M.; Bonini, S.; Coifman, R.; Craig, T.; Delgado, L.; Capão-Filipe, M.; Passali, D.; Randolph, C.; Storms, W. American Academy of Allergy, Asthma & Immunology Work Group Report: Exercise-induced asthma. J. Allergy Clin. Immunol. 2007, 119, 1349–1358. [Google Scholar] [PubMed]
- Crapo, R.O.; Casaburi, R.; Coates, A.L.; Enright, P.L.; Hankinson, J.L.; Irvin, C.G.; MacIntyre, N.R.; McKay, R.T.; Wanger, J.S.; Anderson, S.D.; et al. Guidelines for methacholine and exercise challenge testing: 1999. Am. J. Respir. Crit. Care Med. 2000, 161, 309–329. [Google Scholar] [PubMed] [Green Version]
- Ballestero, Y.; De Pedro, J.; Portillo, N.; Martinez-Mugica, O.; Arana-Arri, E.; Benito, J. Pilot Clinical Trial of High-Flow Oxygen Therapy in Children with Asthma in the Emergency Service. J. Pediatr. 2018, 194, 204–210.e3. [Google Scholar] [CrossRef] [PubMed]
- van Leeuwen, J. Exercise Induced Bronchoconstriction in Childhood Asthma. Ph.D. Thesis, University of Groningen, Groningen, The Netherlands. February 2015.
- Rundell, K.W.; Slee, J.B. Exercise and other indirect challenges to demonstrate asthma or exercise-induced bronchoconstriction in athletes. J. Allergy Clin. Immunol. 2008, 122, 238–246. [Google Scholar] [CrossRef] [PubMed]
- Dupont, W.D.; Plummer, W.D. Power and Sample Size Calculations for Studies Involving Linear Regression. Control Clin. Trials. 1998, 19, 589–601. [Google Scholar] [CrossRef]
- Del Giacco, S.R.; Firinu, D.; Bjermer, L.; Carlsen, K. Exercise and asthma: An overview. Eur. Clin. Respir. J. 2015, 2, 27984. [Google Scholar] [CrossRef] [PubMed]
- Haby, M.M.; Peat, J.K.; Mellis, C.M.; Anderson, S.D.; Woolcock, A.J. An exercise challenge for epidemiological studies of childhood asthma: Validity and repeatabiliy. Eur. Respir. J. 1995, 8, 729–736. [Google Scholar] [PubMed]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).