1. Introduction
Oral sex is a highly intimate and erotic activity which involves the use of the mouth to sensually stimulate the anus or genitalia of a partner [
1,
2]. The practice of oral sex has been in human existence for millennia [
3]. Today, many people feel free to disclose their oral sex experience, and over 30% of the world’s adult population has engaged in oral sex, at least once in their lifetime [
4,
5,
6].
Oral sex has its benefits and risks. Oral sex had been found to improve the sexual satisfaction, intimacy, and relationship quality among sexual partners [
7,
8]; also, it reduces the risk of endometriosis, miscarriage, the sexually transmitted infections of the anus or genitalia, and pre-eclampsia [
7,
9,
10,
11]. However, if carried out unprotected, it is possible to contract sexually transmitted oral infections (STOIs) through oral sex [
12,
13]. Common examples of STOIs are the oral human papillomavirus (HPV) infection, oral herpes simplex virus (HSV) infection, molluscum contagiosum, oral gonorrhoea, oral chlamydia, and oral syphilis [
13]. If STOIs are poorly or not treated, they may progress into notorious complications [
13]. For example, an oral HPV infection can progress into HPV-associated oropharyngeal cancer, and an oral HSV/gonorrhoeal/chlamydial/syphilitic infection can progress into severe pharyngitis [
13].
Protected oral sex is achievable, if carried out with the use of recommended barriers, such as a dental dam, condom, or plastic wrap. These barriers have been widely recommended for the prevention of STOIs [
12].
In Nigeria, issues concerning oral sex currently remain as rarely studied phenomena [
5], probably due to the highly conservative socio-cultural landscape of the Nigerian society, which forbids the open disclosures about personal sexual experiences [
14,
15]. However, some of the few Nigerian multicentre studies available on sexual behaviours have reported oral sex prevalence rates as high as 26.6–49.6% among Nigerian adolescents and adults [
5,
14,
15]. Obviously, these findings demonstrate that oral sex is not an uncommon sexual practice in Nigeria.
Based on scientific reports, the sub-Saharan African countries, including Nigeria, are the countries that have the greatest burdens of sexually transmitted infections (STIs) in the world [
16,
17,
18]. In Nigeria, a recent national report showed that at least one out of every one hundred Nigerians have a human immunodeficiency virus (HIV) infection [
19]; however, there is no known recent report on the national burden of other STIs, including STOIs [
20]. Nonetheless, a small number of reports have shown that STOIs are common among the Nigerian populace [
20,
21].
The need to prevent and control the burden of STOIs in Nigeria is urgent [
18]. However, with the limited socio-economic resources and the current fragility of the health workforce and health systems in Nigeria, the most sustainable approach is through public health education because it is effective, relatively cheaper, and easier than other public health intervention strategies [
18,
22,
23,
24].
The knowledge of STIs, inclusive of STOIs, among the lay public, particularly among those without tertiary school education, is generally low [
25,
26,
27]. Nigerian clinicians are one of the leading and highly influential players in sexual health education [
23,
28,
29]. Based on the credible evidence, Nigerian clinicians have participated in multiple successful school-based and clinical interventions on sexual and reproductive health [
23,
28,
29]; however, research has shown that not all sexual health interventions are favoured by Nigerian clinicians, due to their concerns about the socio-cultural landscape of Nigeria [
30].
Currently, there are no known public health interventions on oral sex in Nigeria. Furthermore, the evidence concerning the disposition of Nigerian clinicians, concerning oral sex-related interventions, is lacking. The acquisition of this evidence forms a basis for the development of appropriate interventions on oral sex. Therefore, this study seeks to investigate the factors determining the willingness of Nigerian clinicians towards the recommendation of protected oral sex, to their patients. The outcomes of this study will provide key information which will pave the future clinical- and community-based education interventions on sexual health and safer oral sex practices.
2. Methods
2.1. Study Design
This study was an online exploratory study of clinicians in Nigeria, and it forms a part of the research projects undertaken by the International Head and Neck Cancer Working Group [
31]. This design was considered the most appropriate for this study because it conforms with the COVID-19 safety protocols as participant–investigator physical contact is not required [
32]. Secondly, the scope of this study was on a sensitive topic in the Nigerian socio-cultural context; therefore, this research design ensures the greater privacy of participants, due to the non-physical contact between the participants and the investigators [
14,
15].
2.2. Participants
The study participants were clinicians in Nigeria who identified themselves as a dentist, medical doctor, midwife/nurse, or clinical pharmacist.
2.3. Study Instrument
The study instrument was a Google Form-based electronic questionnaire (e-questionnaire) adapted from the existing literature [
12,
33]. The questionnaire was edited by multidisciplinary experts (public health scientists, physicians, surgeons, dentists, and sociologists) to ensure face validity. Upon the approval of the edited version by the experts, the questionnaire was piloted amongst 10 clinicians (three dentists, four medical doctors, one nurse, and one clinical pharmacist). The e-questionnaire was further refined to address all inconsistencies observed from the pilot study, prior to its use on the study participants.
2.4. Measures
The e-questionnaire’s final version was semi-structured, and it consisted of three sections and thirty-five items. The first section consisted of eight items, requesting information about the socio-demographic characteristics (age, gender, marital status, clinical profession, place of practice, number of years in practice, etc.). The second section had 12 items, requesting information about the participants’ knowledge of oral sex, which were: ‘Do you have adequate knowledge about oral sex?’, ‘Have you read a peer reviewed journal on oral sex/STIs in the past 6 months?’, ‘When was the last time you read an article on oral sex?’, etc. The third section, consisting of 15 items, requested information about the attitudes and practices of the participants, on oral sex, ranging from engagement in the act of oral sex, and patient and community counselling on oral sex; the items in this section included ‘Have you ever had oral sex?’, ‘Have you ever used anything to prevent sexually transmitted infections whilst having oral sex?’, ‘Do you ever discuss the risk of oral sex with patients?’, ‘Are you willing to discuss oral sex in community health engagement/advocacy meetings?’, etc. All responses to the e-questionnaire items were close-ended with dichotomous or multichotomous responses except for two items that were open-ended: ‘Age’ and ‘Number of years in practice’.
2.5. Sample Size
The sample size for this study was calculated using the Leslie Kish formula [
34]:
In the formula,
n represents the sample size; “
Z (∝⁄2)”, which is equal to 1.96 and represents the
Z score value obtained from the confidence level; “
p” represents the prevalence rate of oral sex; “
e” represents the margin of error which was 0.05; and “
q” represents the compliment of
p (i.e., 1 −
p). The value of
p was obtained from the lifetime oral sex prevalence of 75.6%, reported in a recent study conducted in the USA, among men and women (aged 15 to 44 years) [
35].
Based on this calculation, the minimum sample size for this study was 285.
2.6. Data Collection
Between 1 March 2022 and 21 June 2022, the hyperlink to the e-questionnaire was circulated, through the aid of gatekeepers, to medical doctors, nurses, midwives, clinical pharmacists, and dentists in Nigeria, through various national, zonal, state, and regional groups on the Telegram and WhatsApp social media. Weekly reminders were sent to the participants to follow-up on those who had not yet participated in the study.
Prior to accessing the questionnaire, the participant was required to read the electronic participant information sheet and give their informed consent electronically. This information sheet was a preamble document attached to the questionnaire and it contained details about the study’s aims and objectives, benefits, potential harm, and data privacy and management. Only those who consented were able to participate in the study. Every participant had a unique visitor identity which was assigned to them, and this prevented the duplicate participation per participant.
2.7. Data Analysis
The data collected were exported to the Statistical Package for Social Sciences (SPSS) version 21 software (IBM Corp, New York, NY, USA) for analysis. The frequency distributions of all variables were determined. Bivariate (using Chi-Square test) and multivariate (using multiple logistic regression model) analyses were carried out for the variables of interest, with the level of statistical significance set at a p-value of <0.05.
2.8. Ethical Considerations
The study was conducted under full compliance with the 1964 Helsinki Declaration on health research involving human participants and its protocol was ethically approved by the Sokoto State Ministry of Health (Ref.: SMH/1580.V.IV). All participants gave their informed consent, prior to their participation, and their participation was completely voluntary and strictly confidential.
4. Discussion
Oral sex is a known risk factor of STI transmission [
12,
13]. Worrisomely, the burdens of oral sex practice and STIs are very high in Nigeria [
15,
16,
17,
18]. Despite this huge public health burden, there is only little evidence on the disposition of clinicians in Nigeria towards the prescription of oral sex barriers to their patients. Pertinently, the lack of credible evidence on the clinicians’ dispositions on the prescription of safer oral sex techniques compounds the problem further. However, the provision of research evidence on these areas provides deep insights that will be instrumental for the development of effective and tailored interventions on sexual health and STI preventions, especially among those who are sexually active. The need to provide this evidence birthed this study.
The findings obtained in this study are insightful and noteworthy. To start with, majority of the study respondents were male, and within their third to fourth decade of life (
Table 1). This finding is in-keeping with the general demographic outlook of clinicians in Nigeria, which is predominantly made up of young- to middle-aged men [
36]. Furthermore, the majority of them were working in tertiary healthcare settings (
Table 1). In Nigeria, an overwhelming majority of tertiary healthcare centres are situated in urban/semi-urban areas, and research evidence has shown that many Nigerian healthcare workers prefer to work in urban/semi-urban areas because such places have better social amenities, compared to the rural areas [
37,
38]. Therefore, this may justify why the majority of respondents are working in tertiary healthcare settings.
From the investigation of the background knowledge of the respondents on oral sex (
Figure 1 and
Table 2), it was observed that the majority obtained their information concerning oral sex from more credible sources (such as peer-reviewed and textbooks), while just a few relied on less credible sources, such as social media, print media, and blogs [
39,
40]. Additionally, research has shown that peer discussion is a widely utilized and a credible source of information among clinicians; however, only very few respondents in this study had utilized such route [
41,
42]. Overall, this suggests that peer discussions on oral sex is a very rare opportunity among clinicians in Nigeria.
Although peer-reviewed journals were one of the top two most utilized sources of information on oral sex among respondents, an overwhelming majority of them did not use it to obtain information on oral sex/STIs within six months prior to their participation in this study (
Table 2). This may suggest that most of them might not have considered the need to regularly update their knowledge on the current updates on oral sex/STIs. However, with the heavy burden of STIs and the rising prevalence of oral sex in Nigeria, it is worthwhile for clinicians to keep abreast of current issues in these areas [
16,
17,
18,
19,
20,
21,
43].
The knowledge of the risks of unprotected oral sex, as well as the safety precautions to follow when having oral sex, was high among the respondents (
Table 2). For example, the majority (~70%) disagreed that oral sex is a low-risk sexual activity [
12,
33]. However, this is not the case among the lay public, as many people perceive it as a low-risk practice, thus engaging in the act without adequate protection [
44,
45,
46,
47]. Overall, this shows that public knowledge/perception of oral sex is an important issue of public health concern.
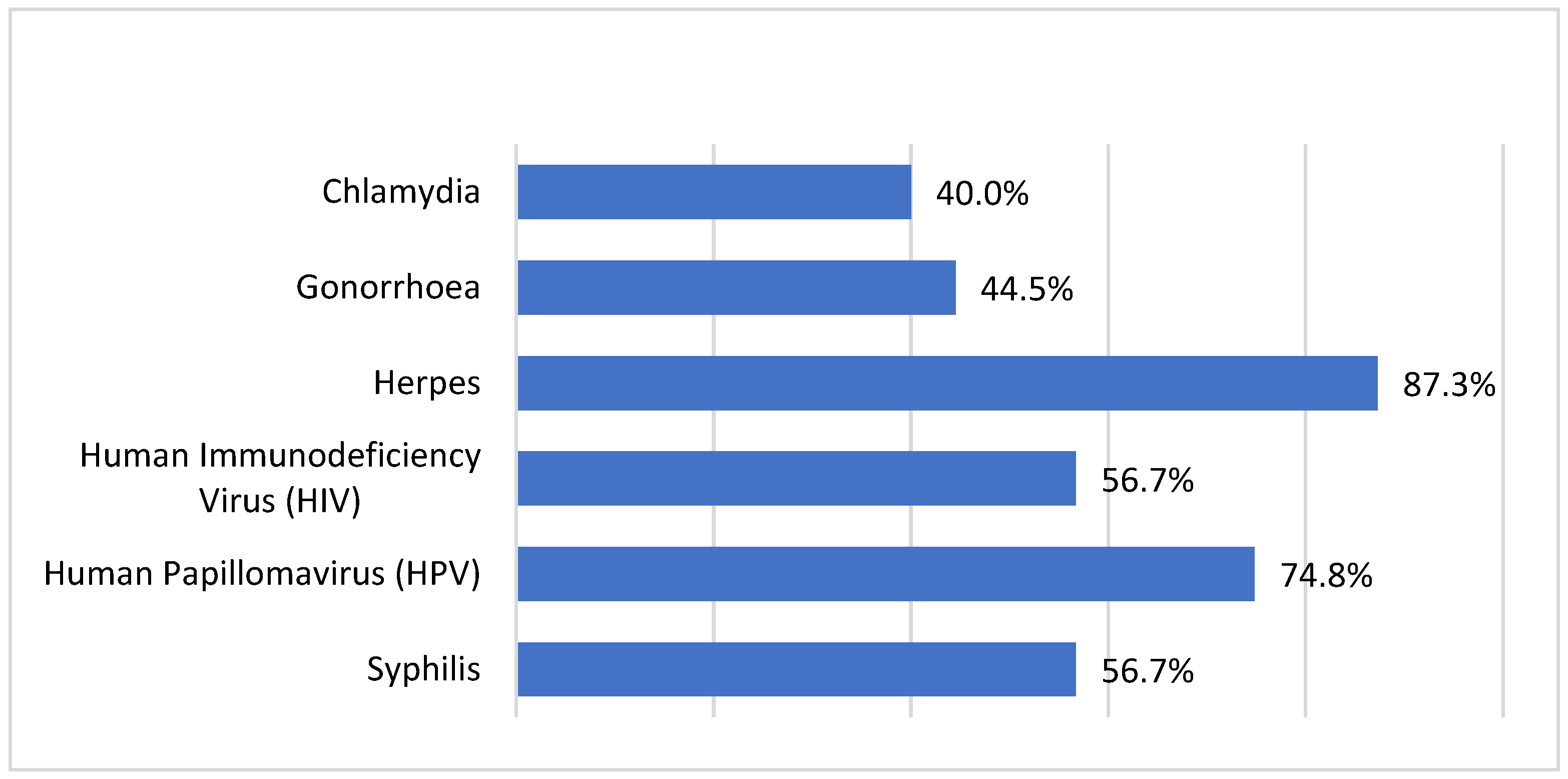
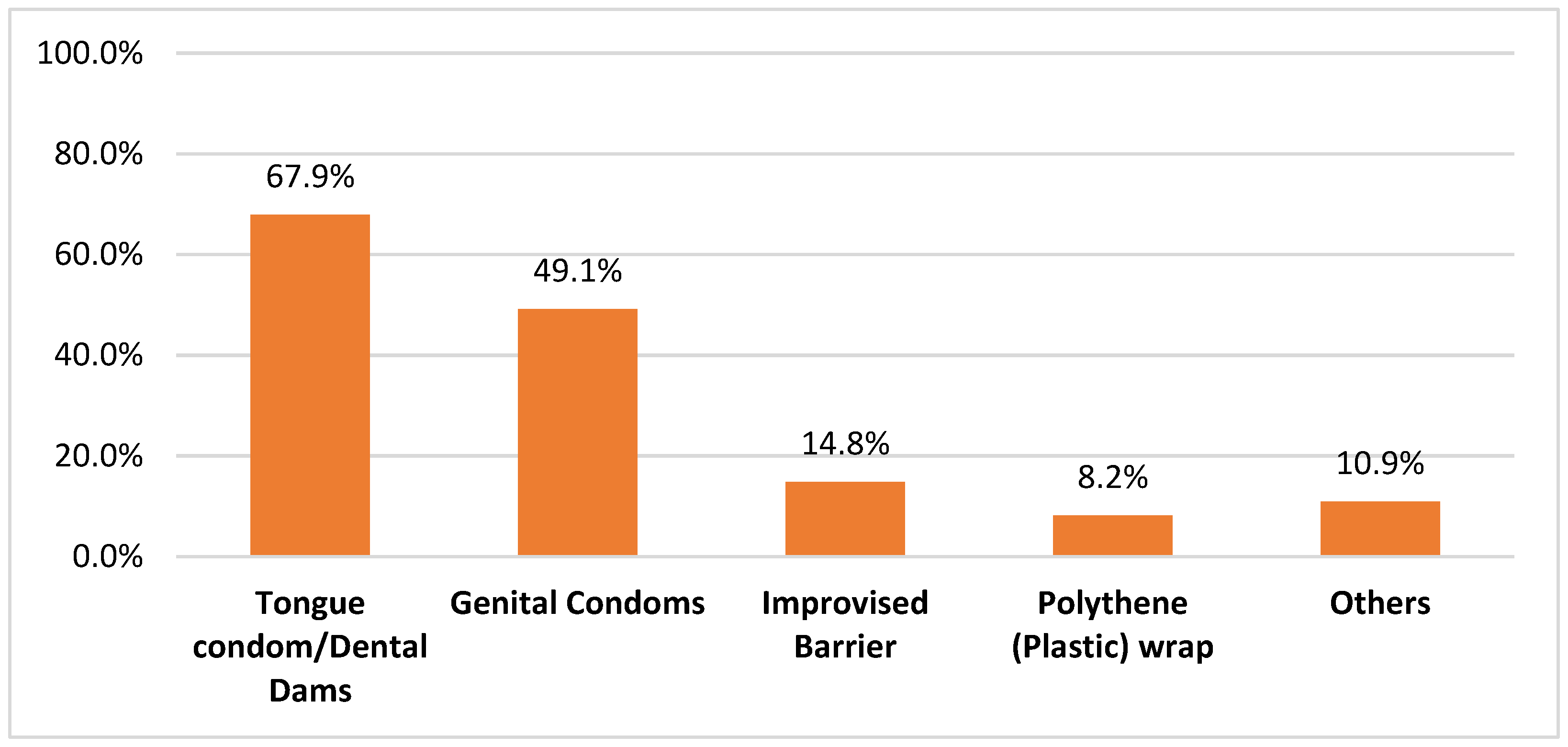
Despite the acceptably high level of knowledge of oral sex among the respondents, an overwhelming majority were not knowledgeable about pre-formed protective barriers (dental dam, tongue condom) or the procedure for the fabrication of improvised barriers used for oral sex (
Table 2). Poor knowledge of these barriers has also been reported among different population groups [
48,
49]. This implies that the knowledge of protective oral sex barriers is generally very low. This, therefore, demonstrates the need for massive public health education programmes on safer oral sex practices.
Pertinently, the lifetime prevalence rate of oral sex among the respondents was high (55.5%) (
Table 3). This rate was found to be higher than that reported in some studies conducted among a sample of nurses (49.6%), nursing students (0.63%), and secondary school students (9.1%) in Nigeria [
14,
50,
51]. Based on the recency the data in this present study, it can be inferred that the lifetime prevalence of oral sex keeps increasing [
5]. This further confirms that oral sex is a very common practice in the 21st century Nigerian society [
2].
Clinicians in Nigeria are highly influential in persuading the public on issues pertaining to health and wellbeing [
52]. Although it has been established that not all public health or clinical interventions on sexual health are welcomed by Nigerian clinicians, it is very interesting to know that an overwhelming majority of the respondents in this study were willing to recommend/discuss safer oral sex measures to/with patients, as well as discuss the issues pertaining to this in academic-, clinic- and community-based settings (
Figure 3;
Table 4 and
Table 5) [
30]. The high level of willingness demonstrated by the respondents further demonstrates that the introduction of clinic-based interventions on safer oral sex promotion is highly likely to succeed in the Nigerian healthcare settings.
From further probing of the respondents, it was also noted that only a minority of the respondents have ever engaged their patients or academic/professional colleagues, in discussions on oral sex safety (
Table 4 and
Table 5). This is a missed opportunity, and there is a need for a change in thinking of this situation, going on the current epidemiological status of oral sex and STIs in Nigeria [
5,
14,
19,
20,
21,
30,
50]. It also plausible that the general lack of access to protective oral sex barriers in Nigeria might have contributed to why the respondents did not engage in such.
Many factors were found to determine if the respondents were willing to recommend, in clinical settings, protective measures for patients engaging in oral sex; these factors ranged from socio-demographic factors to knowledge factors (
Table 6 and
Table 7). As shown in
Table 6, only a few factors, which were associated with knowledge on oral sex and willingness to discuss oral sex, were found to be significantly associated with the respondents’ willingness to recommend protection for oral sex. Although the other factors were not statistically significant, they are noteworthy. For example, a higher proportion of the younger age groups were generally willing to recommend protection for oral sex, compared to the older age groups. Social conservatism, which is oftentimes more pronounced among older people, might be a possible reason for this observation [
53]. It was also observed that a higher proportion of clinical pharmacists, nurses/midwives, primary, and secondary healthcare clinicians were more likely to recommend protection for oral sex, compared to other groups (physicians, dentists, and tertiary healthcare clinicians). Pertinently, among the category of clinicians surveyed, dentists can be regarded as the major experts in STOI prevention and control, as their specialism is in oral care; however, they were not as positively disposed to recommending protected oral sex practices, compared to all of the other clinician categories. Unfortunately, the reasons for these disparities are not known, as they were not investigated in this study. Therefore, further investigation is needed to deeply understand the cause of this observation among dentists.
However, this study has its limitations. First, the representation of the professional groups in this study was uneven, owing to the nonrandomized nature of the data collection process. Consequently, the generalizability of these results should be observed with caution. Secondly, the online mode of data collection was likely to have excluded a certain population of clinicians who were not as digitally savvy as those who responded to our questionnaire [
54]. Thirdly, this study had a low response rate. Due to selective nonresponse, studies with low response rates may generate biased prevalence rates [
55]. This is probably due to the sensitivity of the topic under investigation; however, the response rates might have increased if the authors had provided monetary incentives as a reward for participation [
56]. Unfortunately, due to the lack of funding, monetary incentives could not be provided in this study.
Regardless of these limitations, this study has its strengths. First, this study is believed to be the first study to investigate issues concerning knowledge, attitudes, and practices concerning oral sex, amongst a diverse group of clinicians in Nigeria. Second, the findings obtained in this study are very interesting, crucial, insightful, and basic for the future development and implementation of clinic- and community-based interventions on sexual health, oral sex education, and safe sex promotion.
In conclusion, engagement in discussions on safer oral sex practices, in clinic- and community-based settings, was found to be an uncommon practice among the surveyed clinicians; however, it is laudable that most of them were willing to discuss oral sex in future in clinic- and community-based settings and were willing to discuss/recommend safer oral sex practices to people. This is an opportunity that can be exploited for the development and implementation of effective clinic- and community-based interventions on safe oral sex behaviours in Nigeria.