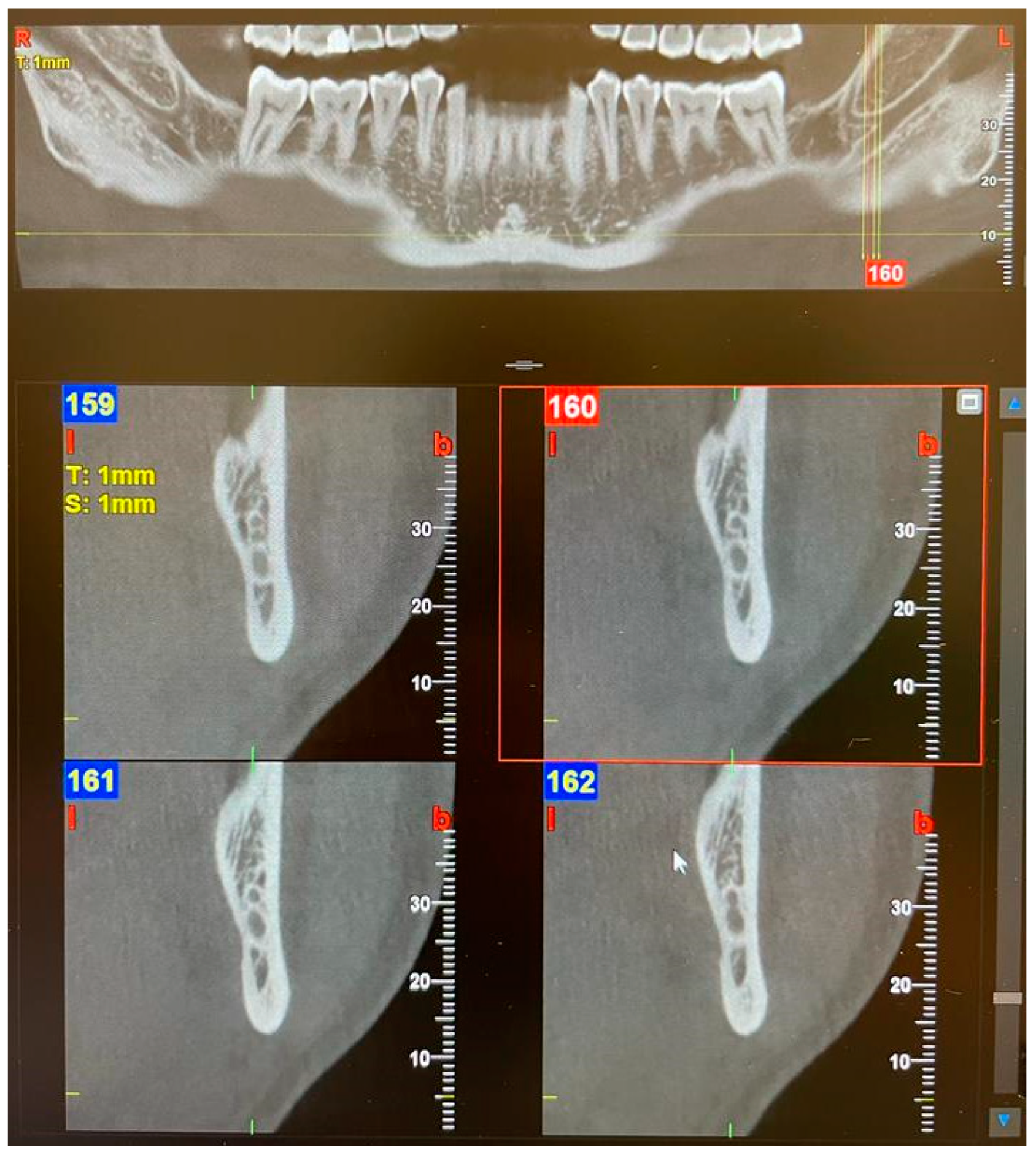
Cone-Beam Computed Tomography Assessment of Bifid and Trifid Mandibular Canals: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Inclusion Criteria
2.2. Exclusion Criteria
2.3. Statistical Analysis
3. Results
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Correction Statement
References
- Rashsuren, O.; Choi, J.W.; Han, W.J.; Kim, E.K. Assessment of bifid and trifid mandibular canals using cone-beam computed tomography. Imaging Sci. Dent. 2014, 44, 229–236. [Google Scholar] [CrossRef]
- Thakur, N.; Kumar, A.; Singh, P.; Gopalakrishnan, D.; Mishra, B.P.; Jha, M.S. Assessment of Anatomical Variations of Mandibular Canal Depicted in Panoramic Radiography. J. Pharm. Bioallied. Sci. 2021, 13 (Suppl. S2), S1394–S1397. [Google Scholar] [CrossRef] [PubMed]
- Miličević, A.; Salarić, I.; Đanić, P.; Miličević, H.; Macan, K.; Orihovac, Ž.; Zajc, I.; Brajdić, D.; Macan, D. Anatomical Variations of the Bifid Mandibular Canal on Panoramic Radiographs in Citizens from Zagreb, Croatia. Acta Stomatol. Croat. 2021, 55, 248–255. [Google Scholar] [CrossRef] [PubMed]
- Sanchis, J.M.; Peñarrocha, M.; Soler, F. Bifid mandibular canal. J. Oral Maxillofac. Surg. 2003, 61, 422–424. [Google Scholar] [CrossRef] [PubMed]
- Claeys, V.; Wackens, G. Bifid mandibular canal: Literature review and case report. Dentomaxillofac. Radiol. 2005, 34, 55–58. [Google Scholar] [CrossRef] [PubMed]
- Naitoh, M.; Hiraiwa, Y.; Aimiya, H.; Gotoh, M.; Ariji, Y.; Izumi, M.; Kurita, K.; Ariji, E. Bifid mandibular canal in Japanese. Implant Dent. 2007, 16, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Rouas, P.; Nancy, J.; Bar, D. Identification of double mandibular canals: Literature review and three case reports with CT scans and cone beam CT. Dentomaxillofac. Radiol. 2007, 36, 34–38. [Google Scholar] [CrossRef]
- Soman, C.; Wahass, T.; Alahmari, H.; Alamri, N.; Albiebi, A.; Alhabashy, M.; Talha, A.; Alqhtani, N. Prevalence and Characterization of bifid mandibular Canal Using Cone Beam Computed Tomography: A Retrospective Cross-Sectional Study in Saudi Arabia. Clin. Cosmet. Investig. Dent. 2022, 14, 297–306. [Google Scholar] [CrossRef] [PubMed]
- De Castro, M.A.A.; Barra, S.G.; Vich, M.O.L.; Abreu, M.H.G.; Mesquita, R.A. Mandibular canal branching assessed with cone beam computed tomography. Radiol. Med. 2018, 123, 601–608. [Google Scholar] [CrossRef]
- Shan, S.; Zhong, S.; Li, J.; Wang, T. Systematic review and meta-analysis of mandibular canal variations on cone beam computed tomography. Oral Radiol. 2022, 38, 445–451. [Google Scholar] [CrossRef]
- Naitoh, M.; Hiraiwa, Y.; Aimiya, H.; Ariji, E. Observation of bifid mandibular canal using cone-beam computerized tomography. Int. J. Oral Maxillofac. Implants 2009, 24, 155–159. [Google Scholar]
- Reia, V.C.B.; de Toledo Telles-Araujo, G.; Peralta-Mamani, M.; Biancardi, M.R.; Rubira, C.M.F.; Rubira-Bullen, I.R.F. Diagnostic accuracy of CBCT compared to panoramic radiography in predicting IAN exposure: A systematic review and meta-analysis. Clin. Oral Investig. 2021, 25, 4721–4733. [Google Scholar] [CrossRef]
- Valenzuela-Fuenzalida, J.J.; Cariseo, C.; Gold, M.; Díaz, D.; Orellana, M.; Iwanaga, J. Anatomical variations of the mandibular canal and their clinical implications in dental practice: A literature review. Surg. Radiol. Anat. 2021, 43, 1259–1272. [Google Scholar] [CrossRef]
- Haas, L.F.; Dutra, K.; Porporatti, A.L.; Mezzomo, L.A.; De Luca Canto, G.; Flores-Mir, C.; Corrêa, M. Anatomical variations of mandibular canal detected by panoramic radiography and CT: A systematic review and meta-analysis. Dentomaxillofac. Radiol. 2016, 45, 20150310. [Google Scholar] [CrossRef] [PubMed]
- Ngeow, W.C.; Chai, W.L. The clinical anatomy of accessory mandibular canal in dentistry. Clin. Anat. 2020, 33, 1214–1227. [Google Scholar] [CrossRef] [PubMed]
- Nithya, J.; Aswath, N. Assessing the Prevalence and Morphological Characteristics of Bifid Mandibular Canal Using Cone-Beam Computed Tomography—A Retrospective Cross-Sectional Study. J. Clin. Imaging Sci. 2020, 10, 30. [Google Scholar] [CrossRef] [PubMed]
- Sîrbu, V.D.; Perlea, P.; Nimigean, V.R.; Bădiţă, D.G.; Şerban, A.; Nimigean, V. Morphological assessment of the mandibular canal trajectory in dentate subjects. Rom. J. Morphol. Embryol. 2017, 58, 1401–1408. [Google Scholar]
- Fuentes, R.; Farfán, C.; Astete, N.; Garay, I.; Dias, F.; Arias, A. Bilateral bifid mandibular canal: A case report using cone beam computed tomography. Folia Morphol. 2018, 77, 780–784. [Google Scholar] [CrossRef]
- Kageyama, I.; Maeda, S.; Takezawa, K. Importance of anatomy in dental implant surgery. J. Oral Biosci. 2021, 63, 142–152. [Google Scholar] [CrossRef]
- Zhou, X.; Gao, X.; Zhang, J. Bifid mandibular canals: CBCT assessment and macroscopic observation. Surg. Radiol. Anat. 2020, 42, 1073–1079. [Google Scholar] [CrossRef]
- Orhan, K.; Aksoy, S.; Bilecenoglu, B.; Sakul, B.U.; Paksoy, C.S. Evaluation of bifid mandibular canals with cone-beam computed tomography in a Turkish adult population: A retrospective study. Surg. Radiol. Anat. 2011, 33, 501–507. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.H.; Lee, K.S.; Oh, M.G.; Choi, H.Y.; Lee, S.R.; Oh, S.H.; Choi, Y.J.; Kim, G.T.; Choi, Y.S.; Hwang, E.H. The incidence and configuration of the bifid mandibular canal in Koreans by using cone-beam computed tomography. Imaging Sci. Dent. 2014, 44, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Auluck, A.; Pai, K.M.; Mupparapu, M. Multiple mandibular nerve canals: Radiographic observations and clinical relevance. Report of 6 cases. Quintessence Int. 2007, 38, 781–787. [Google Scholar]
- Shen, E.C.; Fu, E.; Fu, M.M.; Peng, M. Configuration and corticalization of the mandibular bifid canal in a Taiwanese adult population: A computed tomography study. Int. J. Oral Maxillofac. Implants 2014, 29, 893–897. [Google Scholar] [CrossRef] [PubMed]
- Okumuş, Ö.; Dumlu, A. Prevalence of bifid mandibular canal according to gender, type and side. J. Dent. Sci. 2019, 14, 126–133. [Google Scholar] [CrossRef]
- Fu, E.; Peng, M.; Chiang, C.Y.; Tu, H.P.; Lin, Y.S.; Shen, E.C. Bifid mandibular canals and the factors associated with their presence: A medical computed tomography evaluation in a Taiwanese population. Clin. Oral Implants Res. 2014, 25, e64–e67. [Google Scholar] [CrossRef]
- Chávez-Lomeli, M.E.; Mansilla Lory, J.; Pompa, J.A.; Kjaer, I. The human mandibular canal arises from three separate canals innervating different tooth groups. J. Dent. Res. 1996, 75, 1540–1544. [Google Scholar] [CrossRef]






| Canal Type | Features |
|---|---|
| 1—Retromolar | The retromolar canal, which bifurcates from the mandibular canal in the mandibular ramus region, courses forward, reaching the retromolar region. |
| 2—Dental | The dental canal, which bifurcates from the mandibular canal in the mandibular ramus region, courses forward, reaching the roots of the molars. |
| 3—Forward | Without confluence: The forward canal, which bifurcates from the mandibular canal in the mandibular ramus region, courses forward to the second molar region. With confluence: The forward canal, which bifurcates from the mandibular canal in the mandibular ramus, courses anteriorly and then rejoins the main mandibular canal. |
| 4—Buccolingual | The buccal canal, which bifurcates from the mandibular canal in the mandibular ramus, courses bucco-inferiorly. Lingual canal: The lingual canal, which bifurcates from the mandibular canal in the mandibular ramus, courses lingually and then penetrates through the lingual cortical bone. |
| 5—Trifid | Two accessory canals of the previous canal types. |
| Canal Type | Right (R) | Left (L) | Tot (R + L) | % on Tot Hemi-Mandibles | |
|---|---|---|---|---|---|
| 1—Retromolar | M | 3 | 1 | 4 | 3.57% |
| F | 8 | 5 | 13 | ||
| TOT | 11 | 6 | 17 | ||
| 2—Dental III molar | M | 0 | 0 | 0 | 0.21% |
| F | 1 | 0 | 1 | ||
| TOT | 1 | 0 | 1 | ||
| 2—Dental II molar | M | 1 | 1 | 2 | 0.42% |
| F | 0 | 0 | 0 | ||
| TOT | 1 | 1 | 2 | ||
| 2—Dental I molar | M | 0 | 0 | 0 | 0.63% |
| F | 3 | 0 | 3 | ||
| TOT | 3 | 0 | 3 | ||
| 3—Forward with confluence | M | 2 | 3 | 5 | 2.10% |
| F | 2 | 3 | 5 | ||
| TOT | 4 | 6 | 10 | ||
| 3—Forward without confluence | M | 3 | 2 | 5 | 1.68% |
| F | 1 | 2 | 3 | ||
| TOT | 4 | 4 | 8 | ||
| 4—Buccolingual | M | 3 | 1 | 4 | 1.26% |
| F | 1 | 1 | 2 | ||
| TOT | 4 | 2 | 6 | ||
| 5—Trifid | M | 0 | 1 | 1 | 0.42% |
| F | 0 | 1 | 1 | ||
| TOT | 0 | 2 | 2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
D’Agostino, S.; Valentini, G.; Baldini, A.; Ferrara, E.; Dolci, M. Cone-Beam Computed Tomography Assessment of Bifid and Trifid Mandibular Canals: A Cross-Sectional Study. Oral 2023, 3, 266-275. https://doi.org/10.3390/oral3020022
D’Agostino S, Valentini G, Baldini A, Ferrara E, Dolci M. Cone-Beam Computed Tomography Assessment of Bifid and Trifid Mandibular Canals: A Cross-Sectional Study. Oral. 2023; 3(2):266-275. https://doi.org/10.3390/oral3020022
Chicago/Turabian StyleD’Agostino, Silvia, Giulia Valentini, Alessandro Baldini, Elisabetta Ferrara, and Marco Dolci. 2023. "Cone-Beam Computed Tomography Assessment of Bifid and Trifid Mandibular Canals: A Cross-Sectional Study" Oral 3, no. 2: 266-275. https://doi.org/10.3390/oral3020022
APA StyleD’Agostino, S., Valentini, G., Baldini, A., Ferrara, E., & Dolci, M. (2023). Cone-Beam Computed Tomography Assessment of Bifid and Trifid Mandibular Canals: A Cross-Sectional Study. Oral, 3(2), 266-275. https://doi.org/10.3390/oral3020022









