Idiopathic Mandibular Osteosclerosis: A Case of Complex Diagnosis
Abstract
1. Introduction
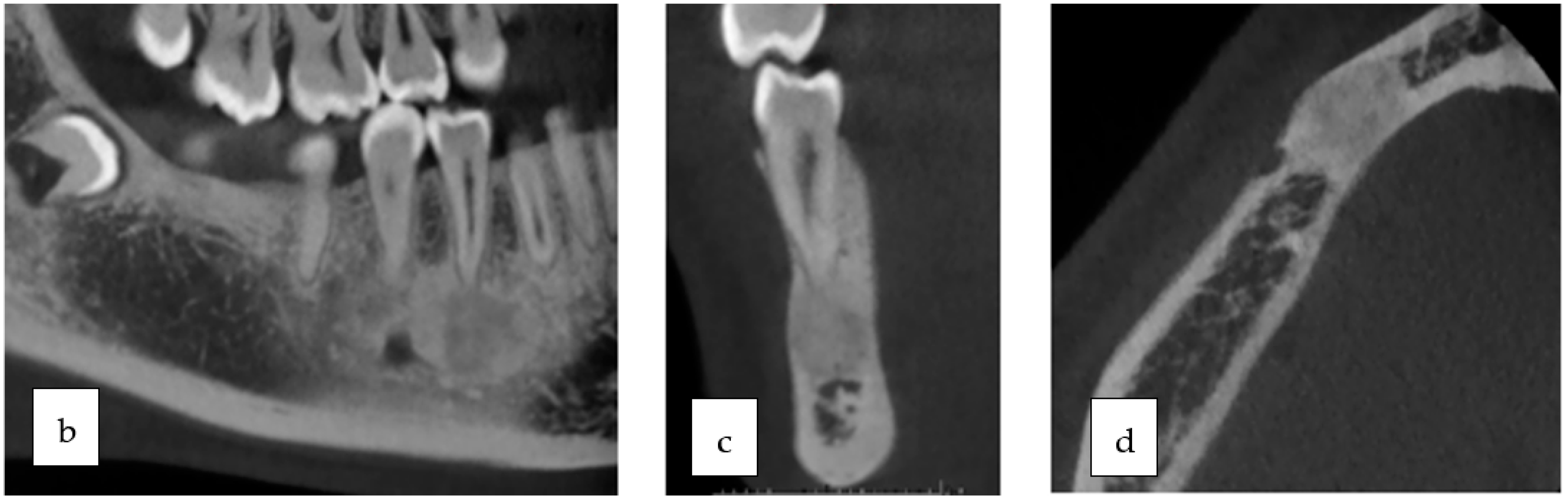
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gamba, T.O.; Maciel, N.A.P.; Rados, P.V.; Da Silveira, H.L.D.; Arús, N.A.; Flores, I.L. The imaging role for diagnosis of idiopathic osteosclerosis: A retrospective approach based on records of 33,550 cases. Clin. Oral Investig. 2021, 25, 1755–1765. [Google Scholar] [CrossRef] [PubMed]
- Hlongwa, P.; Moshaoa, M.A.L.; Musemwa, C.; Khammissa, R.A.G. Incidental Pathologic Findings from Orthodontic Pretreatment Panoramic Radiographs. Int. J. Environ. Res. Public Health 2023, 20, 3479. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, D.; Yu, W. Incidental findings in a consecutive series of digital panoramic radiographs. Imaging Sci. Dent. 2020, 50, 53–64. [Google Scholar] [CrossRef] [PubMed]
- Fuentes, R.; Arias, A.; Astete, N.; Farfán, C.; Garay, I.; Dias, F. Prevalence and morphometric analysis of idiopathic osteosclerosis in a Chilean population. Folia Morphol. 2018, 77, 272–278. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Xu, L.; Cai, C.; Liu, Z.; Zhang, L.; Wang, C.; Xu, J. Longitudinal investigation of idiopathic osteosclerosis lesions of the jaws in a group of Chinese orthodontically-treated patients using digital panoramic radiography. J. Dent. Sci. 2022, 17, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Al-Habib, M.A. Prevalence and Pattern of Idiopathic Osteosclerosis and Condensing Osteitis in a Saudi Subpopulation. Cureus 2022, 14, e22234. [Google Scholar] [CrossRef]
- Geist, J.R.; Katz, J.O. The frequency and distribution of idiopathic osteosclerosis. Oral Surg. Oral Med. Oral Pathol. 1990, 69, 388–393. [Google Scholar] [CrossRef]
- Ledesma-Montes, C.; Jiménez-Farfán, M.D.; Hernández-Guerrero, J.C. Idiopathic osteosclerosis in the maxillomandibular area. Radiol. Medica 2019, 124, 27–33. [Google Scholar] [CrossRef]
- Yesiltepe, S.; Bayrakdar, I.S.; Orhan, K.; Çelik, Ö.; Bilgir, E.; Aslan, A.F.; Odabaş, A.; Costa, A.L.F.; Jagtap, R. A deep learning Model for Idiopathic Osteosclerosis Detection on Panoramic Radiographs. Med. Princ. Pract. 2022, 6, 555–561. [Google Scholar] [CrossRef]
- Schulz, M.; Reichart, P.A.; Dula, K.; Bornstein, M. Focal osteosclerotic lesions of the jaws—A review focusing on diagnostic and therpeutic aspects. Schweiz. Monatsschrift Zahnmed. 2010, 120, 325–339. [Google Scholar]
- Ledesma-Montes, C.; Jiménez-Farfán, M.D.; Hernández-Guerrero, J.C. Maxillomandibular giant osteosclerotic lesions. J. Appl. Oral Sci. 2018, 26, e20170535. [Google Scholar] [CrossRef] [PubMed]
- Marques Silva, L.; Guimaraes, A.L.; Dilascio, M.L.; Castro, W.H.; Gomez, R.S. A rare complication of idiopathic osteosclerosis. Med. Oral Patol. Oral Cir. Bucal 2007, 12, E233–E234. [Google Scholar] [PubMed]
- Green, T.L.; Walton, R.E.; Clark, J.M.; Maixner, D. Histologic examination of condensing osteitis in cadaver specimens. J. Endod. 2013, 39, 977–979. [Google Scholar] [CrossRef] [PubMed]
- Kosti, E.; Lambrianidis, T.; Chatzisavvas, P.; Molyvdas, I. Healing of a radiolucent periradicular lesion with periradicular radiopacity. J. Endod. 2004, 30, 548–550. [Google Scholar] [CrossRef] [PubMed]
- Silva, B.S.F.; Bueno, M.R.; Yamamoto-Silva, F.P.; Gomez, R.S.; Peters, O.A.; Estrela, C. Differential diagnosis and clinical management of periapical radiopaque/hyperdense jaw lesions. Braz. Oral Res. 2017, 31, e52. [Google Scholar] [CrossRef]
- Alfahad, S.; Alostad, M.; Dunkley, S.; Anand, P.; Harvey, S.; Monteiro, J. Dense bone islands in pediatric patients: A case series study. Eur. Arch. Paediatr. Dent. 2021, 22, 751–757. [Google Scholar] [CrossRef]
- Takata, T.; Slootweg, P.J. Odontogenic and maxillofacial bone tumours. In WHO Classification of Head and Neck Tumours, 4th ed.; El-Naggar, A.K., Chan, J.K., Grandis, J.R., Takata, T., Slootweg, P.J., Eds.; IARC: Lyon, France, 2017. [Google Scholar]
- Barnes, L.; Everson, J.W.; Reichart, P.; Sidransky, D. (Eds.) Pathology and Genetics of Head and Neck Tumours; World Ahealth Organization Classification of Tumours; IARC: Lyon, France, 2005. [Google Scholar]
- Xu, L.; Liu, Y.; Luo, J.; Jiang, M.; Guo, W.; Zheng, G. Analysis of clinical and imaging findings in cementoblastoma. Hua Xi Kou Qiang Yi Xue Za Zhi 2015, 33, 419–422. (In Chinese) [Google Scholar] [CrossRef]
- Pathak, J.; Hosalkar, R.M.; Sidana, S.; Swain, N.; Patel, S. Benign cementoblastoma involving left deciduous first molar: A case report and review of literature. J. Oral Maxillofac. Pathol. 2019, 23, 422–428. [Google Scholar] [CrossRef]
- Brannon, R.B.; Fowler, C.B.; Carpenter, W.M.; Corio, R.L. Cementoblastoma: An innocuous neoplasm? A clinicopathologic study of 44 cases and review of the literature with special emphasis on recurrence. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2002, 93, 311–320. [Google Scholar] [CrossRef]
- Brad, W.N.; Douglas, D.D.; Carl, M.A. Chir-Oral and Maxillofacial Pathology-Saunders, 4th ed.; Saunders: London, UK, 2015. [Google Scholar]
- Kawai, T.; Hiranuma, H.; Kishino, M.; Jikko, A.; Sakuda, M. Cemento-osseous dysplasia of the jaws in 54 Japanese patients: A radiographic study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1999, 87, 107–114. [Google Scholar] [CrossRef]
- Hentati, H.; Njim, L. Fibrome ossifiant mandibulaire associé à une canine incluse. Médecine Buccale Chir. Buccale 2013, 19, 127–130. [Google Scholar] [CrossRef][Green Version]
- Pérez-García, S.; Berini-Aytés, L.; Gay-Escoda, C. Ossifying fibroma of the upper jaw: Report of a case and review of the literature. Med. Oral. 2004, 9, 333–339, (In English, Spanish). [Google Scholar] [PubMed]
- Kaplan, I.; Nicolaou, Z.; Hatuel, D.; Calderon, S. Solitary central osteoma of the jaws: A diagnostic dilemma. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2008, 106, e22–e29. [Google Scholar] [CrossRef] [PubMed]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perez, A.; Mamane, A.; Lombardi, T. Idiopathic Mandibular Osteosclerosis: A Case of Complex Diagnosis. Oral 2023, 3, 572-579. https://doi.org/10.3390/oral3040046
Perez A, Mamane A, Lombardi T. Idiopathic Mandibular Osteosclerosis: A Case of Complex Diagnosis. Oral. 2023; 3(4):572-579. https://doi.org/10.3390/oral3040046
Chicago/Turabian StylePerez, Alexandre, Avigaïl Mamane, and Tommaso Lombardi. 2023. "Idiopathic Mandibular Osteosclerosis: A Case of Complex Diagnosis" Oral 3, no. 4: 572-579. https://doi.org/10.3390/oral3040046
APA StylePerez, A., Mamane, A., & Lombardi, T. (2023). Idiopathic Mandibular Osteosclerosis: A Case of Complex Diagnosis. Oral, 3(4), 572-579. https://doi.org/10.3390/oral3040046






