Abstract
Background: The objectives of this pilot study are to compare the oral health status of institutionalised and non-institutionalised elderly people in Xiamen, China, and investigate oral health-related factors among this population. Methods: One elderly residential centre and one community centre in the same district were invited to join this study. Elderly people who were aged 65 years or older and able to participate in the oral health examination and questionnaire survey were recruited. Their demographic information, oral health-related behaviours, and oral health-related quality of life were collected through a questionnaire survey. The Decayed, Missing, and Filled Teeth (DMFT) index and the Community Periodontal Index were adopted to assess caries experience and periodontal status, respectively. A chi-square test, a t-test, and a correlation analysis were conducted for data processing. Results: Forty-nine elderly people participated in this study. There is no significant difference in the demographic background between non-institutionalised and institutionalised people. The mean DMFT index in the institutionalised group is significantly higher than that in the non-institutionalised group (p = 0.004). In contrast, the non-institutionalised group showed a significantly higher prevalence of gingival bleeding (p = 0.013) and a higher prevalence of periodontal pockets (p = 0.006) than the institutionalised group. Monthly income is also associated with the caries experience in this population. Conclusions: Institutionalised elderly people showed a higher severity of dental caries but a lower prevalence of periodontal symptoms than the non-institutionalised group. It is noteworthy that the generalisation of this pilot study is limited. Future research should be conducted to comprehensively investigate the oral health status of this population.
1. Introduction
Improvements in living quality have contributed to an increase in life expectancy and, therefore, an ageing population [1]. According to the seventh national survey in 2020, China had almost 200 million people aged over 65 years, which accounted for 13.5% of the total population [2]. Therefore, it is generally accepted that an ageing society is becoming a significant problem in China. Societal ageing can affect economic growth, the pattern of policymaking, the way of family function, the prevalence of chronic diseases, and the distribution of healthcare resources [3].
Oral health is defined as ‘the state of the mouth, teeth and orofacial structures that enable individuals to perform essential functions such as eating, breathing and speaking, and encompasses psychosocial dimensions such as self-confidence, well-being and the ability to socialise and work without pain, discomfort and embarrassment’ [4]. It is an important component of general health that contributes to the general well-being and quality of life. According to a WHO report released in 2022, untreated dental caries is the most common disease worldwide, affecting an estimated 2.5 billion people. The burden of oral diseases is higher among older people living alone or in nursing homes [5]. The fourth National Oral Health Survey in China showed that the prevalence of dental caries in the 65 to 74 age group was 98%; the mean Decayed, Missing, and Filled Teeth (DMFT) index was 13.3 [6]. A study in Brazil, also a developing country, showed a high prevalence of dental caries and tooth decay in almost all age groups [7]. Caries can cause pain and discomfort in the teeth, resulting in food impaction and bad breath [8]. Untreated caries may develop progressively, leading to pulp infection and periapical inflammation [9]. Periodontal diseases are also prevalent in the Chinese elderly population. The prevalence of bleeding on probing (BoP) and calculus was 83% and 90%, respectively; almost 75% of 65- to 74-year-old people presented the symptom of clinical attachment loss (CAL) equal or larger than 4 mm [10]. Periodontitis can lead to gum swelling and bleeding; severe cases will cause bone loss, tooth loosening, and finally, tooth loss. Both untreated dental caries and periodontal diseases will eventually affect the whole dentition, leading to compromised masticatory function; poor chewing ability and discomfort in eating will affect the absorption of nutrients in elderly people and cause long-term malnutrition [11]. Meanwhile, missing teeth or edentulous will influence the appearance, self-esteem, and interpersonal communication of elderly patients [12]. In addition, periodontitis is a risk factor for some systemic conditions, including Alzheimer’s disease, upper respiratory infections, and pneumonia [13]. Therefore, dental caries and periodontal diseases remain significant oral health issues in elderly people; those conditions will not affect only patients’ oral health but also their general health and quality of life.
Oral health status can be associated with the living and caring situations of elderly people. Although homebound elderly people receive care and support from their family members, it was reported that they typically did not receive medical or dental check-ups for years [14]. In contrast, nursing homes are usually equipped with health consultants who can provide basic healthcare support to the residents. However, studies have reported the oral health status in institutionalised elderly people was significantly worse than that in non-institutionalised elderly people [15,16]. In China, the primary mode of elderly support is their family. Since the family planning policy has been adopted for four decades, the shrinking family size poses special challenges for the young generation in providing care for their parents and grandparents [17]. Therefore, the mode of elderly care is transferring from home care to institutionalised care. There was a total of 38,000 nursing homes for elderly people in China in 2020, which showed an increase of 10% from the previous year; the number of beds was more than three times as five years ago [18]. However, whether staying in nursing homes has an impact on the oral health status of Chinese elderly people is unknown. Therefore, the aim of this pilot study is to preliminarily investigate the oral health status of institutionalised and non-institutionalised elderly people in Xiamen, China, and explore oral health-related factors among this population.
2. Materials and Methods
This pilot study used a cross-sectional design conducted in Xiamen from 2022 to 2023. Ethical approval was obtained from the Institutional Review Board of the Medical Ethics Committee at Xiamen University (No. XDYX202206K04).
2.1. Recruitment of Participants
One community health centre and one elderly residential centre in the same district were invited to join this study. Dental examination and oral health education stations were set up in those centres. Participants were recruited on a walk-in basis. Elderly people who (1) were aged 65 years or older, (2) had no serious systemic disease, and (3) were cooperative with the dental examination were eligible for this study. Elderly people with poor general conditions that would impede their ability to undergo the study components were excluded from this study. Research assistants provided a comprehensive explanation of the aim of this study to all participants and/or their guardians. A written informed consent form was obtained from each participant.
2.2. Clinical Examination
Two dentists (NW and HY) from Xiang’an Hospital at Xiamen University performed dental examinations. They were trained by an experienced oral epidemiologist (SSG) and calibrated in the oral assessments, including dental caries and periodontal status. Participants were asked to clean the oral cavity before clinical examination to avoid recording errors. Dentists followed the guidelines of the oral health survey published by the World Health Organization [19] and used hand instruments to conduct oral diagnoses in elderly people by visual and exploratory methods. Caries experience was measured using the Decayed, Missing, and Filled Teeth (DMFT) index. A tooth was classified as decayed when there was an evident cavity on the crown and/or root of the tooth, or the tooth was filled with caries. A tooth was classified as missing when it was absent due to caries. A tooth was classified as filled when it had undergone permanent filling without any signs of caries. Periodontal status was determined using the Community Periodontal Index (CPI). Gingival bleeding and periodontal pockets were assessed for all available teeth. Clinical attachment loss (CAL) was recorded for the representative teeth in six sextants (16/17, 11, 26/27, 36/37, 31, 46/47); the sextant with the highest score was considered the CAL status of the whole mouth.
2.3. Questionnaire Survey
The questionnaire survey consisted of two parts. The first part collected demographic information and oral health-related behaviours of the elderly people, including age, sex, education level, monthly income, toothbrushing habits, smoking history, consumption of tea, and dental visit experience [20]. The second part assessed the oral health-related quality of life (OHRQoL) of the participants. The Chinese version of the Oral Health Impact Profile-14 (OHIP-14) scale was adopted to measure the OHRQoL. The OHIP-14 aimed to assess the impact of oral health on people’s quality of life, including pain, function, emotion, and social interaction with seven dimensions, i.e., functional limitation, physical pain, psychological discomfort, physical disability, psychological disability, social disability, and handicap [21]. The OHIP-14 scores can range from 0 to 56; a higher score indicates a worse OHRQoL. Participants were required to complete the questionnaires on-site. Project assistants (CM and DL) assisted the elderly people in answering the questions at an individual interview base. Another assistant (JL) checked the completeness of the questionnaires when it was returned. If any data were missing or uncertain, project assistants would perform follow-up visits or telephone calls to make sure the questions were appropriately answered.
2.4. Data Analysis
Two investigators entered the data into Excel files independently. The data were proofread by a third investigator before analysis. All the analyses were performed using SPSS 25.0 software (IBM Corporation, Armonk, NY, USA). The grouping variable in this study is whether the elderly people were institutionalised or non-institutionalised. The assumptions checked were whether there were differences between institutionalised or non-institutionalised elderly people regarding their socioeconomic backgrounds, oral health status, and oral health-related behaviours. Independent t-tests were conducted to compare continuous data between institutionalised and non-institutionalised groups, including DMFT scores, OHIP-14 scores, and the age of the participants. Chi-square tests were performed to analyze categorical data, including the CPI, demographic information, and oral health-related behaviours. Independent t-tests and Pearson correlation coefficient analysis were used to explore the associated factors of dental caries in this elderly population. Pearson correlation coefficient analysis was also performed to study the correlation between the OHIP-14 domains and elderly people’s oral health status. The statistical significance level was set at 0.05 for all tests.
3. Results
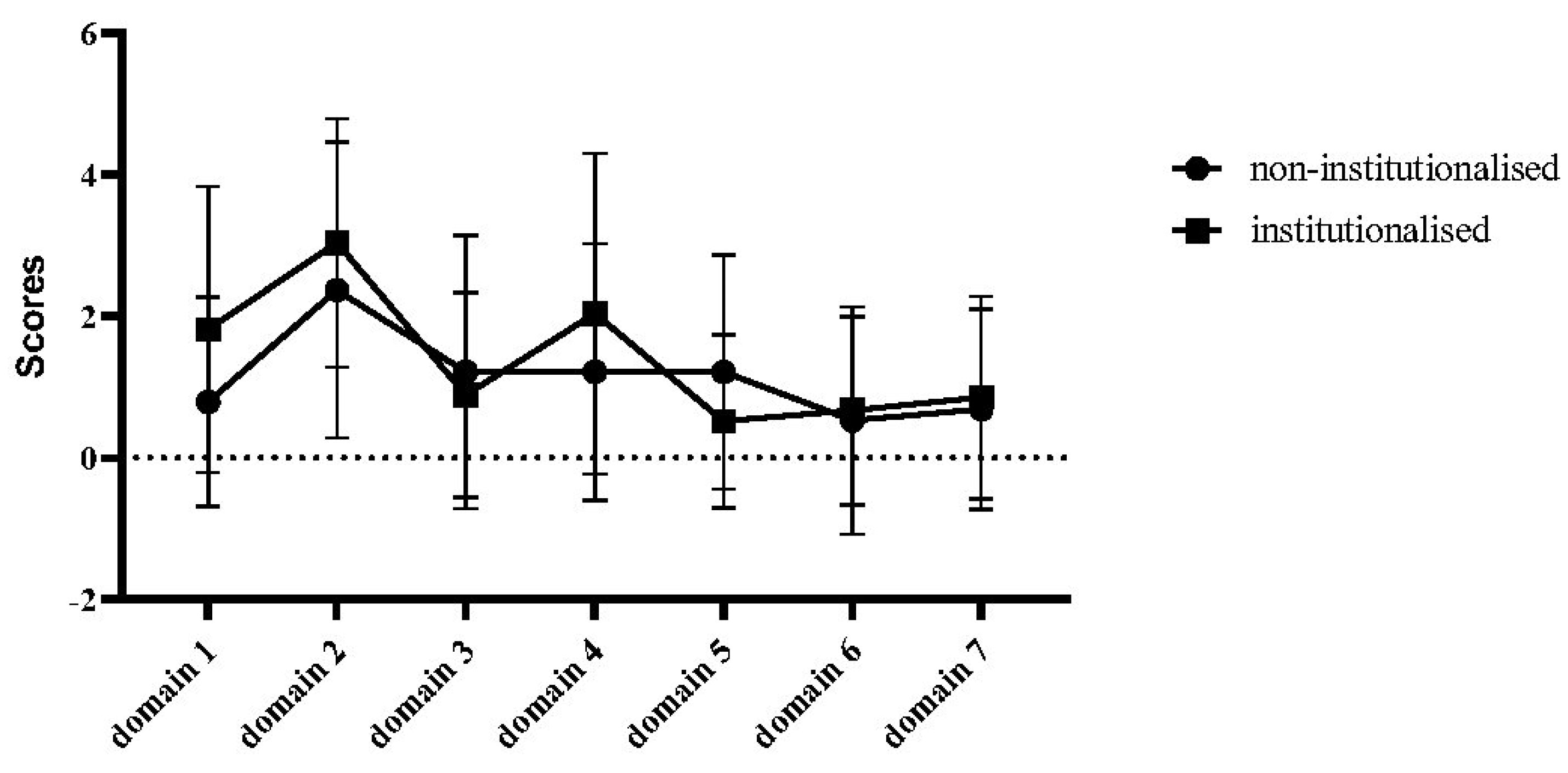
A total of 49 elderly people were recruited in this study, with 22 participants from the community centre and 27 participants from a residential nursing home. The mean age of the participants was 74.0 ± 10.9 years old. Males consisted of the majority of recruited people (67.3%). Table 1 presents the demographic information, oral health-related behaviours, and the OHRQoL between non-institutionalised and institutionalised groups. There is no significant difference between the two groups regarding sex, age, education level, and monthly income. Less than half of the participants had a history of smoking, and more than 70% of the elderly people consumed tea daily. Only a few elderly people had visited a dentist within one year; the prevalence was slightly higher in institutionalised people, and there was no significant difference between the two groups (9.1% for the non-institutionalised group and 18.5% for the institutionalised group, p = 0.436). The prevalence of regulated toothbrushing habits was higher in the institutionalised elderly people, but there was no significant difference between the groups. The OHIP-14 score was 8.0 ± 8.3 for institutionalised elderly individuals and 9.7 ± 9.6 for non-institutionalised individuals (p = 0.534). The responses of seven OHIP-14 domains are presented in Figure 1. There was no significant difference in the scores of all OHIP-14 domains between study groups. Domain 2, namely, physical pain, showed slightly higher scores (2.37 ± 2.09 in non-institutionalised elderly people and 3.04 ± 1.75 in institutionalised people), but there was no statistical significance. For the elderly people living in institutions, the three most affected OHIP-14 domains were ‘physical pain’, ‘physical disability’, and ‘functional limitation’. Meanwhile, ‘physical pain’, ‘psychological discomfort’, and ‘physical disability’ were the most influential domains for elderly people living in the community.

Table 1.
Demographic information, oral health-related behaviours, and the OHRQoL of institutionalised and non-institutionalised elderly people.
Figure 1.
Scores of seven OHIP-14 domains (domain 1—functional limitation, domain 2—physical pain, domain 3—psychological discomfort, domain 4—physical disability, domain 5—psychological disability, domain 6—social disability, and domain 7—handicap).
The dental caries and periodontal status of the participants are presented in Table 2. The mean DMFT scores were significantly higher for elderly people who were living in the residential nursing home than non-institutionalised people (20.4 ± 9.3 vs. 12.4 ± 7.7, p = 0.004). In addition, elderly people living in institutions had a significantly higher mean MT score compared to those not living in institutions (13.5 ± 10.3 vs. 7.4 ± 5.6, p = 0.024). No statistical difference was observed for the DT and FT components. Non-institutionalised elderly people showed worse periodontal conditions than those living in the nursing home. There was a significant difference in gingival bleeding between the two groups (p = 0.013). Gingival bleeding was present in almost all non-institutionalised elderly participants (94.7%), while 60% of the institutionalised elderly participants showed gingival bleeding. A significant difference regarding the prevalence of periodontal pockets was observed between the two groups (p = 0.006). Around one-third (34.8%) of the institutionalised elderly people had periodontal pockets, whereas the majority (78.9%) of the non-institutionalised elderly people had periodontal pockets. However, no significant difference was found in CAL between the two groups.

Table 2.
Caries experience and periodontal status of institutionalised and non-institutionalised elderly people.
The associated factors of dental caries are presented in Table 3. In general, the OHRQoL was not related to the caries experience. Age, sex, education level, smoking history, daily consumption of tea, dental visit experience, and toothbrushing frequency were not associated factors for dental caries in this population. Nevertheless, this study found monthly income was associated with DMFT score (p = 0.022). The results revealed that elderly individuals with a lower monthly income had a significantly higher DMFT score than those with a higher monthly income. Moreover, all OHIP-14 domains showed positive correlations with the severity of dental caries and CAL. Among the seven domains of the OHIP-14, ‘functional limitation’ (r = 0.295) and ‘physical disability’ (r = 0.247) had the strongest correlation with dental caries; ‘psychological discomfort’ (r = 0.283) and ‘physical disability’ (r = 0.272) had the strongest correlation with CAL. However, no statistical significance was identified between the OHIP-14 domains and elderly people’s dental caries and CAL status (Table 4).

Table 3.
Associated factors of dental caries in the elderly population.

Table 4.
Correlation between the OHIP-14 domains and oral health status.
4. Discussion
This pilot study aims to investigate the oral health status of institutionalised and non-institutionalised elderly people in Xiamen, China, and explore oral health-related factors among these people. Since no similar study has been conducted in this population, this study presents novel insights into the oral health status, behaviours, and oral health-related factors of elderly individuals with different living conditions. The findings would help oral health professionals understand the oral health conditions of this population and make specific designs of oral health promotion programmes for them. This study recruited one community centre and one residential nursing home in the same district. There were no significant differences in demographic backgrounds, including age, sex, education level, and monthly income, between elderly people living in different environments. We considered that they were comparable populations, which could minimise the number of irrelevant factors in this study. Due to the limitation of the field setting and limitation cooperative behaviours of the elderly participants, we did not perform duplicate examinations in the study population.
The major finding of this study demonstrated a higher DMFT index among older adults living in institutional settings compared to those living in non-institutional environments, which aligns with existing reports summarised by a systematic review [22]. Several factors may be related to this situation. First, inadequate strategies for caries prevention and treatment are prevalent in the elderly population. People living in institutions encounter additional oral health challenges, such as insufficient oral healthcare provision [23], ineffective oral hygiene practices, and limited resources allocated toward the prevention and treatment of oral diseases [24]. Second, systemic health plays a significant role in oral health-related practices. Older adults living in institutions often exhibit a greater burden of systemic health issues, including chronic diseases [25] and cognitive decline [20,26], which impede their ability and inclination to undertake appropriate self-care oral practices, consequently elevating the risk of dental caries. Third, mobility restrictions and financial constraints commonly encountered by institutionalised elderly people usually hinder their ability to obtain timely and suitable oral healthcare interventions, thereby leaving dental caries untreated or unaddressed. We observed a significantly higher MT index among older adults living in nursing homes, which indicated that tooth extraction was the primary treatment option for dental diseases in this population. This preference for the extraction of unsalvageable teeth over conservative treatments may be attributed to limited dental knowledge and poor attitudes toward oral healthcare in elderly people. Oral healthcare is often not considered a priority or routine, leading to delays in oral assessment and treatment [27]. Accordingly, only when faced with severe pain do these individuals tend to seek dental care, which may result in tooth extraction as the sole solution for caries has progressed to a terminal stage [28]. Over the past decade, there has been a shift from MT to FT in the DMFT component of older adults living in Europe [29]. This suggests that the treatment of dental caries has shifted from extraction to restorative interventions as a result of improvements in dental health services. Dental professionals in China should consider promoting regular dental examinations of elderly people and treating dental caries through restoration in the early stage of their disease.
However, in this study, we found that the periodontal status of institutionalised elderly people was better than that of the non-institutionalised elderly, which was different from the previous reports [15,16]. The reason for this result may be because, in recent years, the staff in nursing homes have paid more attention to the oral health problems of elderly people [18]. In this study, we found that the majority of the residents in nursing homes performed toothbrushing twice or more times a day. However, more than half of the elderly people living in the community only brushed their teeth once a day or they did not brush regularly. By talking with the staff in this nursing home, we noticed that the nursing home provided free toothbrushes and toothpaste to their residents regularly. In addition, the nursing home was equipped with professional nursing staff; they reminded, supervised, or helped the elderly people clean their teeth at least once a day. Although institutionalised elderly people showed worse caries status, it can be related to long-term effects, including poorer oral health-related behaviours in the past, lower monthly income, and systematic health issues. In contrast, since they had good toothbrushing behaviours recently, their gingival conditions were better than non-institutionalised elderly people. The prevalence of gum bleeding and periodontal pockets was much higher in non-institutionalised elderly people in our findings, which may be associated with their unsatisfactory toothbrushing habits. Research has reported that intergenerational support can promote oral health-seeking behaviours among elderly family members [30]. Intergenerational support refers to the assistance that adult children provide for their parents, including financial help, daily caregiving, and emotional comfort. Therefore, dental professionals should enhance oral health promotion, including improving oral hygiene habits, knowledge, and attitudes toward oral health, particularly in non-institutionalised settings and toward not only the elderly people themselves but also their younger family members.
Studies have reported that poor dentition may lead to a worse OHRQoL [31,32]. This study found a trend of a positive correlation between the OHIP-14 score and the DMFT index in elderly people, but there was statistical significance. There may be two reasons for the insignificant result. This pilot study aimed for an initial investigation, so it recruited a limited number of participants. Increasing the sample size can be an option in future studies to understand the correlation between dental caries and the OHRQoL more comprehensively. In addition, elderly people are more likely to dismiss minor or even severe oral health problems that are essential to general well-being [32]. They were satisfied with their oral health at a lower level of oral health expectation. Elderly people are more likely to perceive oral health problems as insignificant because their physical functioning declines when getting older and they are more likely to suffer from a variety of diseases, making them less likely to report oral health problems. Therefore, oral health sometimes has less impact on quality of life than general health [33].
In our study, we demonstrated that monthly income was associated with the dental caries status in this population, which was consistent with previous studies [34]. Low-income older adults need to meet their basic needs before addressing oral health issues. Therefore, oral health may be a relatively low priority in their perception [34]. In addition, they usually choose tooth extraction rather than conservative treatments at higher costs, which might be one of the reasons for their high MT index [35]. There is a strong association between people’s monthly income and educational level [30]. Other studies have reported that education level was also associated with caries status [36]. In this study, we found that elderly people who received compulsory education or below had a higher DMFT score than those who received advanced education. Although there is no statistical difference, based on this trend, oral health professionals should design targeted services for elderly people with low income and low education, and their caregivers in the community and institutions should provide better help for their oral health.
There are several limitations of this study. First, we performed convenient sampling in this study, and the sample size was relatively small; selection bias may exist. Second, we did not conduct sample size calculation because the aim of this study is to explore the differences regarding oral health between institutionalised and non-institutionalised elderly people; hypotheses were not pre-established. Third, this study was conducted in only one city in southern China. Therefore, the generalisability of this study was limited. However, this study has provided some preliminary findings, which can be directions for future studies. In addition, given the limitations of the present study, we propose potential improvements for future research. First, we selected two centres situated in the suburban region of Xiamen for this pilot study. The sample size should be increased, and a representative sampling method should be used to recruit a more diverse range of community and nursing home settings to comprehensively investigate this topic and enhance its generalisability. Second, due to the challenges posed by extended clinical examinations among elderly individuals, the current study only recorded the dentition and periodontal condition of the two elderly groups. It is recommended to incorporate supplementary information, such as mucosal health and salivary flow rates, to enhance the understanding of oral health. Third, this study used a simple questionnaire to collect basic information on oral health-related behaviours in elderly people. The preliminary results identified monthly income as the only factor correlated with dental caries status. Other information, such as diet habits and oral health knowledge and attitudes, should be investigated in future studies. Fourth, this study found that there may be potential correlations between the OHIP-14 domain ‘functional limitation’ and dental caries status (p = 0.052), as well as ‘psychological discomfort’, ‘physical disability’, and CAL (p = 0.066 and 0.078, respectively). These findings provide insights for future research that can focus on the correlations between the OHIP-14 domains and oral health status.
5. Conclusions
This pilot study demonstrated that institutionalised elderly people showed a higher severity of dental caries but a lower prevalence of periodontal symptoms than the non-institutionalised group in Xiamen, China. Monthly income was significantly associated with dental caries status in this population. Although the generalisability of this pilot study is limited, the preliminary findings provide insights into the design and implementation of future research. Larger and more representative samples should be included in future studies. In addition, researchers can include more confounding factors and focus on specific OHIP-14 domains to comprehensively investigate the pattern of oral health between institutionalised and non-institutionalised elderly people.
Author Contributions
Conceptualisation, J.L. (Jian Li) and S.G.; methodology, J.L. (Jinghan Lei), C.M., D.L., N.W., H.Y., D.N., J.L. (Jian Li) and S.G.; software, S.G.; validation, N.W., H.Y. and D.N.; formal analysis, S.G.; investigation, J.L. (Jinghan Lei), C.M., D.L., N.W., H.Y., D.N. and J.L. (Jian Li); resources, J.L. (Jian Li); data curation, J.L. (Jinghan Lei), C.M., D.L. and S.G.; writing—original draft preparation, J.L. (Jinghan Lei), C.M., D.L. and S.G.; writing—review and editing, J.L. (Jinghan Lei), J.L. (Jian Li) and S.G.; visualisation, J.L. (Jian Li); supervision, J.L. (Jian Li) and S.G.; project administration, S.G.; funding acquisition, S.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the State Key Laboratory of Vaccines for Infectious Diseases, Xiang’an Biomedicine Laboratory, Xiamen, Fujian, China (No. 2023XAKJ0103067).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Institutional Review Board of the Medical Ethics Committee at Xiamen University (protocol code XDYX202206K04 and date of approval 20 June 2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author due to ethical reasons.
Acknowledgments
The authors would like to express our gratitude to the residential nursing home, the community center, and all the staff and participants who have joined this study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Niu, H.; Álvarez-Álvarez, I.; Guillén-Grima, F.; Aguinaga-Ontoso, I. Prevalence and incidence of Alzheimer’s disease in Europe: A meta-analysis. Neurologia 2017, 32, 523–532. [Google Scholar] [CrossRef] [PubMed]
- Tu, W.-J.; Zeng, X.; Liu, Q. Aging tsunami coming: The main finding from China’s seventh national population census. Aging Clin. Exp. Res. 2021, 34, 1159–1163. [Google Scholar] [CrossRef] [PubMed]
- Henderson, D.A.G.; Donaghy, E.; Dozier, M.; Guthrie, B.; Huang, H.; Pickersgill, M.; Stewart, E.; Thompson, A.; Wang, H.H.X.; Mercer, S.W. Understanding primary care transformation and implications for ageing populations and health inequalities: A systematic scoping review of new models of primary health care in OECD countries and China. BMC Med. 2023, 21, 319. [Google Scholar] [CrossRef] [PubMed]
- Oral Health. Available online: https://www.who.int/zh/health-topics/oral-health#tab=tab_1 (accessed on 30 December 2023).
- WHO Highlights Oral Health Neglect Affecting nearly Half of the World’s Population. Available online: https://www.who.int/news/item/18-11-2022-who-highlights-oral-health-neglect-affecting-nearly-half-of-the-world-s-population (accessed on 30 December 2023).
- Si, Y.; Tai, B.; Hu, D.; Lin, H.; Wang, B.; Wang, C.; Zheng, S.; Liu, X.; Rong, W.; Wang, W.; et al. Oral health status of Chinese residents and suggestions for prevention and treatment strategies. Glob. Health J. 2019, 3, 50–54. [Google Scholar] [CrossRef]
- de Albuquerque, L.S.; de Queiroz, R.G.; Abanto, J.; Bönecker, M.J.S.; Forte, F.D.S.; Sampaio, F.C. Dental Caries, Tooth Loss and Quality of Life of Individuals Exposed to Social Risk Factors in Northeast Brazil. Int. J. Environ. Res. Public Health 2023, 20, 6661. [Google Scholar] [CrossRef]
- Niesten, D.; Witter, D.J.; Bronkhorst, E.M.; Creugers, N.H. Oral health care behavior and frailty-related factors in a care-dependent older population. J. Dent. 2017, 61, 39–47. [Google Scholar] [CrossRef]
- Chai, H.H.; Chen, K.J.; Duangthip, D.; Lo, E.C.M.; Chu, C.H.; Gao, S.S. Parental perspectives on the use of silver diamine fluoride therapy to arrest early childhood caries in kindergarten outreach dental services: A qualitative study. J. Dent. 2022, 125, 104250. [Google Scholar] [CrossRef]
- Jiao, J.; Jing, W.; Si, Y.; Feng, X.; Tai, B.; Hu, D.; Lin, H.; Wang, B.; Wang, C.; Zheng, S.; et al. The prevalence and severity of periodontal disease in Mainland China: Data from the Fourth National Oral Health Survey (2015–2016). J. Clin. Periodontol. 2020, 48, 168–179. [Google Scholar] [CrossRef] [PubMed]
- Yoshihara, A.; Watanabe, R.; Hanada, N.; Miyazaki, H. A longitudinal study of the relationship between diet intake and dental caries and periodontal disease in elderly Japanese subjects. Gerodontology 2009, 26, 130–136. [Google Scholar] [CrossRef]
- Slade, G.; Akinkugbe, A.; Sanders, A. Projections of U.S. Edentulism Prevalence Following 5 Decades of Decline. J. Dent. Res. 2014, 93, 959–965. [Google Scholar] [CrossRef]
- Gil-Montoya, J.A.; Ferreira de Mello, A.L.; Barrios, R.; Gonzalez-Moles, M.A.; Bravo, M. Oral health in the elderly patient and its impact on general well-being: A nonsystematic review. Clin. Interv. Aging 2015, 10, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Sanders, A.E.; Slade, G.D.; Lim, S.; Reisine, S.T. Impact of oral disease on quality of life in the US and Australian populations. Community Dent. Oral Epidemiol. 2009, 37, 171–181. [Google Scholar] [CrossRef]
- Niesten, D.; Witter, D.; Bronkhorst, E.; Creugers, N. Oral health-related quality of life and associated factors in a care-dependent and a care-independent older population. J. Dent. 2016, 55, 33–39. [Google Scholar] [CrossRef]
- e Farias, I.P.S.; de Sousa, S.A.; Almeida, L.d.F.D.d.; Santiago, B.M.; Pereira, A.C.; Cavalcanti, Y.W. Does non-institutionalized elders have a better oral health status compared to institutionalized ones? A systematic review and meta-analysis. Cienc. Saude Coletiva 2020, 25, 2177–2192. [Google Scholar] [CrossRef]
- Chen, X.; Zhuoga, C.; Deng, Z. Adaptations to the One-Child Policy: Chinese Young Adults’ Attitudes Toward Elder Care and Living Arrangement after Marriage. Front. Psychol. 2021, 12, 608111. [Google Scholar] [CrossRef]
- Fang, E.F.; Xie, C.; Schenkel, J.A.; Wu, C.; Long, Q.; Cui, H.; Aman, Y.; Frank, J.; Liao, J.; Zou, H.; et al. A research agenda for ageing in China in the 21st century (2nd edition): Focusing on basic and translational research, long-term care, policy and social networks. Ageing Res. Rev. 2020, 64, 101174. [Google Scholar] [CrossRef]
- Oral Health Surveys: Basic Methods—5th Edition. Available online: https://apps.who.int/iris/bitstream/handle/10665/97035/9789241548649_eng.pdf;jsessionid=4FD3AB5AB3DDDCA31A027DD31E57306C?sequence=1 (accessed on 30 December 2023).
- Gao, S.S.; Chen, K.J.; Duangthip, D.; Lo, E.C.M.; Chu, C.H. The Oral Health Status of Chinese Elderly People with and without Dementia: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 1913. [Google Scholar] [CrossRef]
- Hongxing, L.; List, T.; Nilsson, I.-M.; Johansson, A.; Astrøm, A.N. Validity and reliability of OIDP and OHIP-14: A survey of Chinese high school students. BMC Oral Health 2014, 14, 158. [Google Scholar] [CrossRef]
- Chan, A.K.Y.; Tamrakar, M.; Jiang, C.M.; Lo, E.C.M.; Leung, K.C.M.; Chu, C.H. A Systematic Review on Caries Status of Older Adults. Int. J. Environ. Res. Public Health 2021, 18, 10662. [Google Scholar] [CrossRef]
- Stancic, I.; Petrovic, M.; Popovac, A.; Vasovic, M.; Despotovic, N. Caregivers’ attitudes, knowledge and practices of oral care at nursing homes in Serbia. Vojn. Pregl. 2016, 73, 668–673. [Google Scholar] [CrossRef]
- Saarela, R.K.T.; Hiltunen, K.; Kautiainen, H.; Roitto, H.-M.; Mäntylä, P.; Pitkälä, K.H. Oral hygiene and health-related quality of life in institutionalized older people. Eur. Geriatr. Med. 2021, 13, 213–220. [Google Scholar] [CrossRef] [PubMed]
- De Deco, C.P.; Santos, J.F.F.D.; Cunha, V.d.P.P.d.; Marchini, L. General health of elderly institutionalised and community-dwelling Brazilians. Gerodontology 2007, 24, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Lee, E.; Lee, S.-W. Association between oral health and frailty: Results from the Korea National Health and Nutrition Examination Survey. BMC Geriatr. 2022, 22, 369. [Google Scholar] [CrossRef] [PubMed]
- Hoben, M.; Kent, A.; Kobagi, N.; Huynh, K.T.; Clarke, A.; Yoon, M.N. Effective strategies to motivate nursing home residents in oral care and to prevent or reduce responsive behaviors to oral care: A systematic review. PLoS ONE 2017, 12, e0178913. [Google Scholar] [CrossRef]
- Kamberi, B.; Koçani, F.; Begzati, A.; Kelmendi, J.; Ilijazi, D.; Berisha, N.; Kqiku, L. Prevalence of Dental Caries in Kosovar Adult Population. Int. J. Dent. 2016, 2016, 4290291. [Google Scholar] [CrossRef]
- Carvalho, J.C.; Schiffner, U. Dental Caries in European Adults and Senior Citizens 1996–2016: ORCA Saturday Afternoon Symposium in Greifswald, Germany—Part II. Caries Res. 2018, 53, 242–252. [Google Scholar] [CrossRef]
- Wen, C.; Zhang, Q. The role of intergenerational support in shaping oral healthcare-seeking behavior among older adults in China. Front. Public Health 2023, 11, 1234539. [Google Scholar] [CrossRef]
- Baniasadi, K.; Armoon, B.; Higgs, P.; Bayat, A.; Gharehghani, M.A.M.; Hemmat, M.; Fakhri, Y.; Mohammadi, R.; Moghaddam, L.F.; Schroth, R.J. The Association of Oral Health Status and socio-economic determinants with Oral Health-Related Quality of Life among the elderly: A systematic review and meta-analysis. Int. J. Dent. Hyg. 2021, 19, 153–165. [Google Scholar] [CrossRef]
- Kotzer, R.D.; Lawrence, H.P.; Clovis, J.B.; Matthews, D.C. Oral health-related quality of life in an aging Canadian population. Health Qual. Life Outcomes 2012, 10, 50. [Google Scholar] [CrossRef]
- Östberg, A.; Hall-Lord, M. Oral health-related quality of life in older Swedish people with pain problems. Scand. J. Caring Sci. 2011, 25, 510–516. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Palacios, R.D.; Ramírez-Amador, V.; Jarillo-Soto, E.C.; Irigoyen-Camacho, M.E.; Mendoza-Núñez, V.M. Relationship between gender, income and education and self-perceived oral health among elderly Mexicans. An exploratory study. Cienc. Saude Coletiva 2015, 20, 997–1004. [Google Scholar] [CrossRef] [PubMed]
- Msyamboza, K.P.; Phale, E.; Namalika, J.M.; Mwase, Y.; Samonte, G.C.; Kajirime, D.; Sumani, S.; Chalila, P.D.; Potani, R.; Mwale, G.C.; et al. Magnitude of dental caries, missing and filled teeth in Malawi: National Oral Health Survey. BMC Oral Health 2016, 16, 29. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-García, S.; Heredia-Ponce, E.; Juárez-Cedillo, T.; Gallegos-Carrillo, K.; Espinel-Bermúdez, C.; De La Fuente-Hernández, J.; García-Peña, C. Psychometric properties of the General Oral Health Assessment Index (GOHAI) and dental status of an elderly Mexican population. J. Public Health Dent. 2010, 70, 300–307. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).