Abstract
Background: Violence against women or other vulnerable individuals is a serious violation of human rights and a global public health issue representing a significant “problem of enormous global health proportions”. Violence against women is an endemic phenomenon; the numbers are very high, highlighting the severity and urgency of the problem. Methods: We conducted this research by examining the field of violence against women. Our analysis involved reviewing papers published between 2018 and December 2023, which were identified through electronic database searches. Out of a total of 136 papers initially identified, we considered 71 documents. Results: This research highlights the global nature of violence against women, including psychological assessments of harm, as a socio-cultural problem and underlines the more common injuries. Conclusions: We examined how the presence of forensic experts can be beneficial in identifying and evaluating injuries, as well as reconstructing the dynamics of the events, particularly for judicial purposes.
1. Introduction
Violence against women or other vulnerable individuals is a serious violation of human rights and a global public health issue representing a significant “problem of enormous global health proportions”(WHO) [1]. However, stereotypes and prejudices surrounding this issue often lead to the misconception that it only occurs among the most vulnerable segments of the population; in reality, data show otherwise, occurring without distinctions of educational attainment or socioeconomic status. Violence against women is an endemic phenomenon, prevalent across all latitudes, and as early as 1979, the UN established CEDAW, the Convention on the Elimination of All Forms of Discrimination against Women [2]. In the subsequent Declaration on the Elimination of Violence against Women, issued in 1993, the United Nations General Assembly defined violence against women as “any act of gender-based violence that results in, or is likely to result in, physical, sexual, or mental harm or suffering to women, including threats of such acts, coercion, or arbitrary deprivation of liberty, whether occurring in public or private life.” Globally, the numbers are very high, highlighting the severity and urgency of the problem. In most cases, victims of violence are women. Worldwide, it is estimated that about 35% of women have experienced sexual and/or non-sexual violence at least once in their lifetime. In 38% of cases of female homicides, the perpetrator is the partner. Globally, in 30% of cases, women experience violence from their partners within their own homes. Sub-Saharan Africa and Southeast Asia are the regions most affected by the problem [1]. In July 2017, the UN adopted General Recommendation No. 35, which further specifies the obligations of States to intervene and counter gender-based violence, including forms of violence affecting women’s reproductive health rights and violence perpetrated online and through new technologies [3,4]. Despite all prevention measures implemented over the years, the issue of violence against women persists, with significant physical and psychological consequences for the victims. Unfortunately, this violence can also lead to homicide; in Italy, the National Institute of Statistics (ISTAT) reported 106 femicides in 2022, while the number rose to 110 in 2023 [5].
2. Materials and Methods
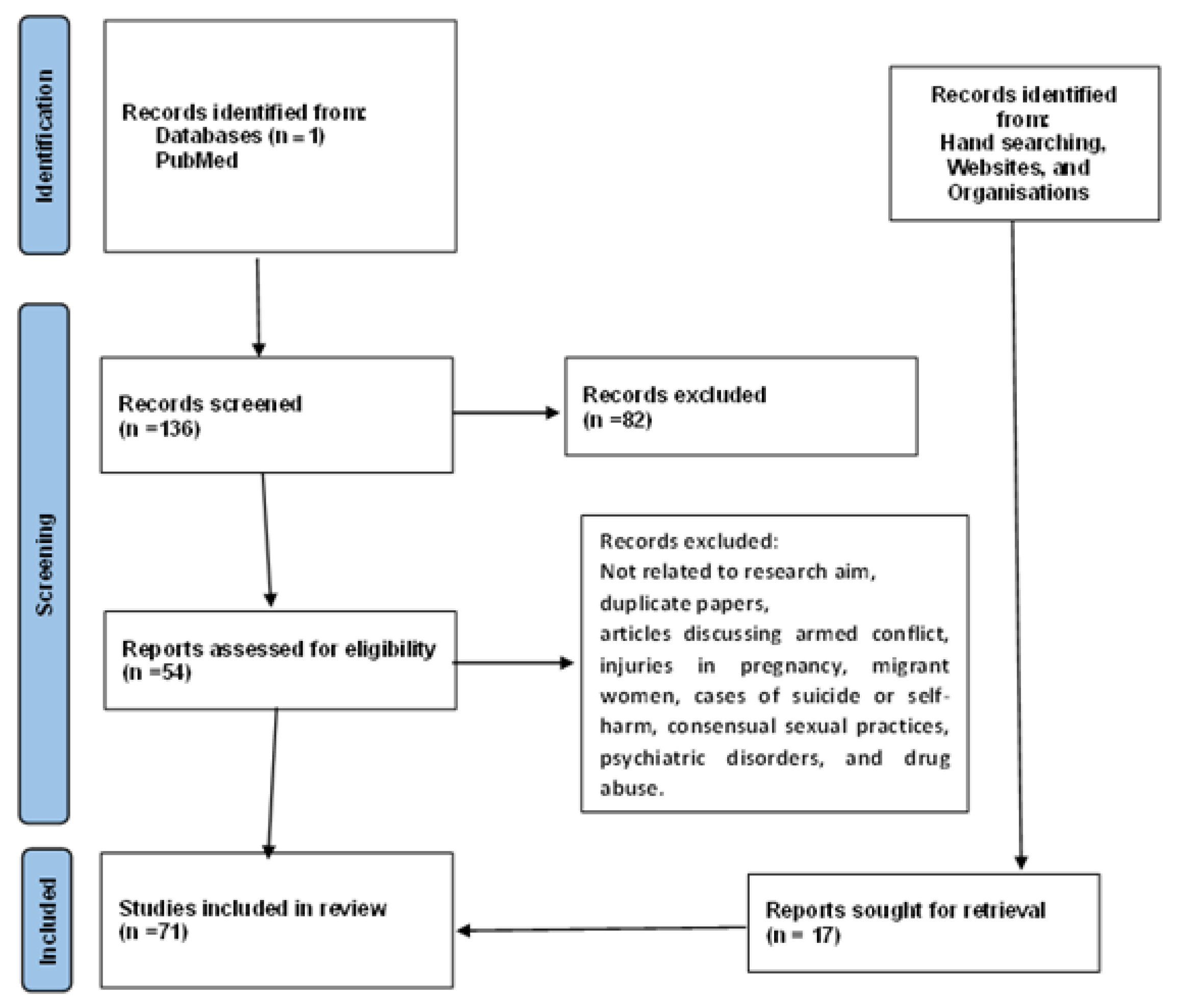
We conducted this research by examining the landscape of violence against women at both the Italian and global levels. Our analysis involved reviewing papers published between 2018 and December 2023, which were identified through electronic database searches. The search terms used were [forensic] and [violence] and [against] and [women], within a single scientific database (PubMed). Out of a total of 136 papers initially identified, after removing duplicates and excluding articles that did not meet the established criteria, we included 54 titles in this review. Only English articles were included. Non-original articles, letters, as well as articles in which violence against women occurred in contexts of conflict, injuries during pregnancy, migrant women, cases of suicide or self-harm, consensual sexual practices, psychiatric disorders, and drug abuse were excluded. Additionally, through a manual search, we identified further literature, data, and additional records, bringing the total to 71 documents considered for our study (Figure 1).
Figure 1.
Prisma flowchart.
The objective of this research is to highlight the global nature of violence against women. Furthermore, to elucidate the regulations governing this field, we specifically focused on the types of injuries sustained by victims of violence following assaults. We examined how the presence of forensic experts can be beneficial in identifying and evaluating these injuries, as well as in reconstructing the dynamics of the events, particularly for judicial purposes.
3. Results
According to UNIFEM data, one in three women has been raped, beaten, coerced into sexual activity, or otherwise abused at least once in their lifetime [6]. Various forms of violence exist [7,8,9], but according to the WHO, domestic violence is the leading cause of death or serious injury for women aged 16 to 44; domestic violence is the world’s leading cause of death, more than cancer, malaria, or road accidents. According to the UN, 30% of British women experience abuse from their spouses or ex-spouses. In the West Bank, the percentage reaches 52%; in Nicaragua, 28%; in Bangladesh, 47%; in Canada, 29%; in Turkey, 58%; in Australia, 23%; and in Cambodia, 16%. There is also another type of direct violence against women known as cultural violence. This is based on so-called cultural or religious practices but remains a significant violation of human rights, which is unfortunately still widespread. In Bangladesh, many women are disfigured or killed with acid. In 2002 alone, 315 such attacks on women and girls were recorded, almost one per day. To this, the practice of selective abortions must be added, which is especially prevalent in China; it has been observed that more than 60 million women are “missing” from the Earth due to the practice of selective abortions [10]. In the USA, within the scope of an investigation conducted in 2003, 23% of young lesbians reported being subjected to attempted rape by their schoolmates, and 50% of them experienced sexual harassment.
3.1. Victims of Violence: The Numbers in Italy
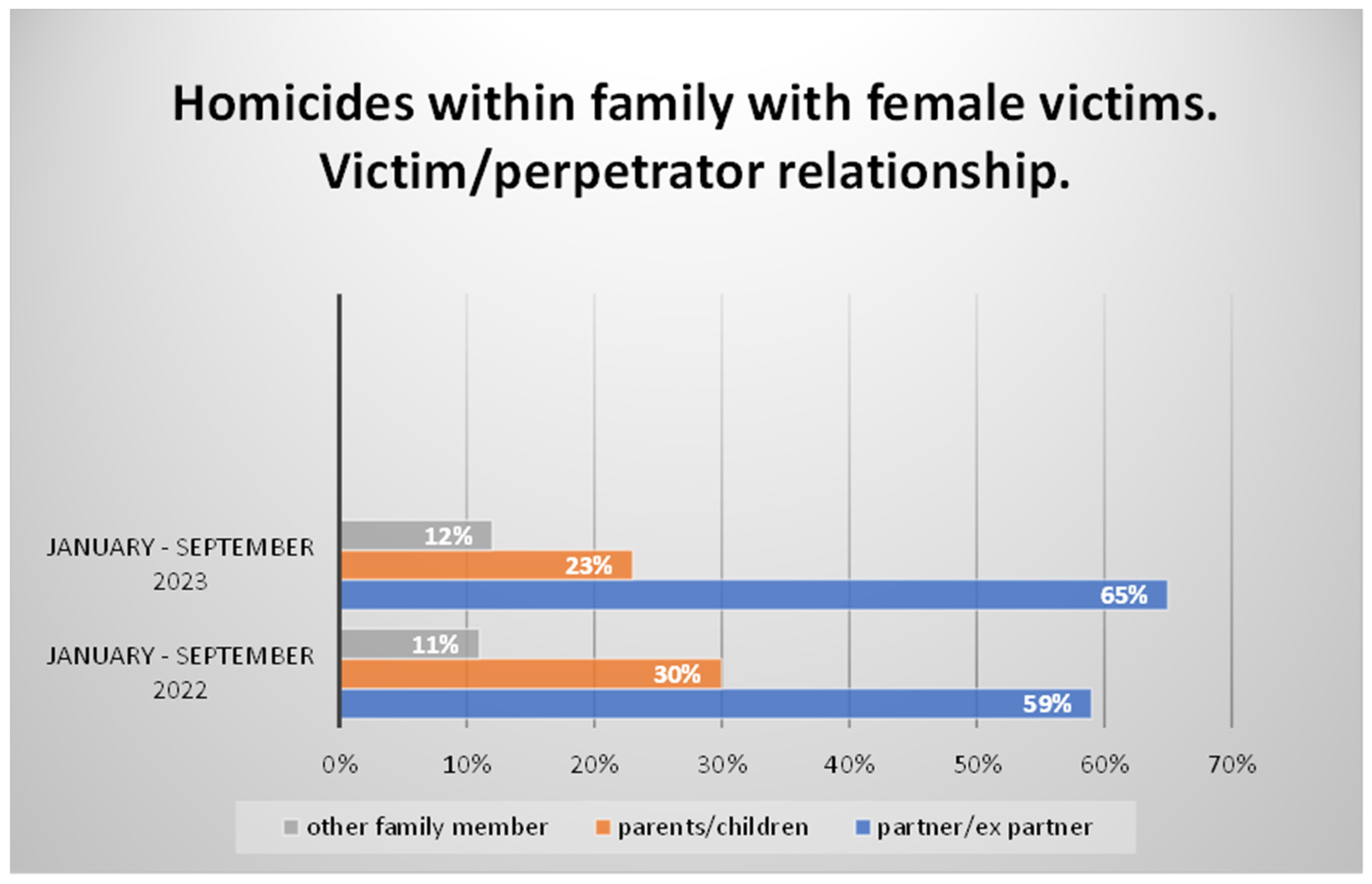
In Italy, Istat data also show that 31.5% of women have experienced some form of physical or sexual violence in their lifetime. The most severe forms of violence are perpetrated by partners or ex-partners, relatives, or friends. In 62.7% of cases, rapes are committed by partners. According to the Report of the Criminal Analysis Service of the Central Directorate of Criminal Police updated to 20 November 2022, there were 273 homicides recorded from 1 January to 20 November 2022 (+2% compared to the same period in 2021), with 104 female victims (−5% compared to the same period in 2021, when there were 109 women killed). Women killed in a family/relationship context were 88 (−6% compared to the same period in 2021, when there were 94 victims); of these, 52 died at the hands of their partner/ex-partner (−16% compared to the 62 victims in the same period in 2021) [11]. In the first nine months of 2023, according to the report, women victims of homicide committed by their partner or ex-partner accounted for 65% of those killed in a family/relationship context, compared to 59% recorded in the corresponding timeframe in 2022 [12] (Figure 2).
Figure 2.
Data January—22 September.
At this point, there was a recognized need for support for victims who found themselves in situations of distress and urgency from both medical and legal and social perspectives. Several anti-violence and anti-stalking hotlines (e.g., 1522), the YouPol app by the State Police, anti-violence centers, and the Health and Women’s Protection Service of the INMP (National Institute for the Promotion of Migrant Population Health) were established. In severe cases—or those perceived as such—victims can directly seek help at the emergency room, especially when immediate and unavoidable medical care is needed. Emergency room socio-healthcare workers, in addition to providing necessary care, are adequately trained to clinically address and then guide the victim towards an appropriate and healthy path. In 2021, there were 11,771 women who accessed emergency departments with a diagnosis of violence, totaling 12,780 accesses. The incidence of these accesses is 18.4 per 10,000 total emergency department accesses (in men, it is 15.1), steadily increasing since 2017 (14.1) despite the overall decrease in emergency department visits due to the COVID-19 pandemic. Emergency department accesses by women with a diagnosis of violence between 2019 and 2020 (the year of the pandemic) decreased less compared to total accesses: from 15,791 to 11,818 (−25.2% compared to −39.8% of total accesses). However, in 2022, there were 4.9 emergency department accesses by women with a diagnosis of violence per 10,000 residents compared to the 4.4 accesses recorded in the previous year [5,13].
Young women aged 18 to 34 were the most affected (8.8 per 10,000 in the years 2020–2021), followed by adult women aged 35–49 (7.2 per 10,000 in 2020–2021). In the biennium 2020–2021, emergency department accesses with a diagnosis of violence for foreign women were more than double compared to Italian women. Accesses mainly occur via personal means; however, since 2017, there has been a decrease in violence-related accesses via this arrival method in favor of emergency department visits via the 118 service. From EMUR data, the concerning trend observed is that the proportion of violence-related accesses with a green triage code (minor urgency) decreased from 76.2% in 2017 to 60.3% in 2021, while those with a yellow code (urgent and non-deferrable urgency) increased from 12.8% to 27.7%. Furthermore, for women, maltreatment and violence within couples and families are more frequent compared to men, while for men, injuries inflicted by others are more common, similar to what happens in cases of homicides. It was also noted that emergency department accesses for violence exhibit high regional variability for both genders. Regarding women, in the period before the pandemic, the incidence of accesses per 10,000 total accesses varies from a value of 3.0 in Molise to a value of 23.3 in Liguria, while in the post-pandemic period, the incidence varies from 2.6 in Molise to 27.6 in Abruzzo. Even the rates show marked territorial variability. What is common, however, is that during emergency department visits, information about the perpetrator of violence is still scarce in the collected data (10.8% of female admissions), and voluntary discharge strongly characterizes admissions for violence (8.3% compared to 1.9% in regular admissions) and is more frequent in foreign women by almost double [14]. In the five years of 2017–2021, both for emergency department accesses and hospitalizations, the most frequently associated diagnoses with violence were related to traumas and poisonings (fractures, wounds, bruises, burns, and poisonings) and mental disorders (predominant emotional disorders, some adjustment disorders and reactions, cannabinoid abuse, drug abuse without dependence [15], anxiety disorders, and dissociative and somatoform disorders [13].
3.2. Legislation in Italy and Europe
The first significant innovation in Italian legislation concerning sexual violence occurred with the approval of Law No. 66 on 15 February 1996. With this law, violence against women began to be considered a crime against personal freedom, reforming the previous legislation, which classified it among crimes against public morality and decency. Since then, increasingly more legal and social measures have been introduced to combat cases of violence. Our country then took a historic step in combating gender-based violence with Law No. 77 on 22 June 2013 by approving the ratification of the Istanbul Convention [16] outlined in May 2011, in which Article 4 establishes the principle that every individual has the right to live free from violence in both public and private spheres. In the Italian context, the legislature has intervened multiple times, primarily to increase penalties or introduce new crimes. However, Law 119/2013 (“Conversion into law, with modifications, of decree-law no. 93 of 14 August 2013, containing urgent provisions on security and the fight against gender-based violence”) also provided greater freedom and security for victims—both Italian and foreign—to more easily seek assistance from local support structures. Additionally, to design adequate policies for the prevention and combat of gender-based violence and to ensure effective monitoring of the phenomenon, Law No. 53 of 5 May 2022, entitled “Provisions on statistics on gender-based violence,” was approved. Article 4 of this law requires all public healthcare facilities, particularly emergency departments, to provide data and information regarding violence against women. These recent regulations highlight the significant attention given to victims of all types of violence but also emphasize the significant social issue, as evident from the previously mentioned statistics: the prevalence of female victims of violence.
The regulatory intervention that undoubtedly demonstrates greater attention to the victim of violence is certainly the “Decree of the President of the Council of Ministers of 24 November 2017” [17], which stipulates the presence of personnel trained not only in recognizing and managing the victims of violence but also specialized in forensic expertise specifically trained for appropriate investigations and collection of evidence useful for judicial purposes. In light of this importance, guidelines for forensic medical assistance to victims of sexual violence have indeed been published, aimed at standardizing forensic examinations, improving healthcare services for all individuals victimized by sexual violence, and increasing awareness of the issue of sexual violence [18]. In Europe, the issue is governed by several directives on judicial cooperation in criminal matters, gender equality, and asylum policies. On 8 March 2022, International Women’s Day, the European Commission proposed a new directive on combating violence against women and domestic violence aimed at ensuring a minimum level of protection from this type of violence throughout the Union. This directive also introduced the offense of online violence, referring to the non-consensual sharing of private images, as well as online stalking, harassment, or hate speech. As a result, in November 2022, the European Commission announced the establishment of a helpline number valid throughout Europe for victims of violence against women to ensure that in each Member State, victims can access free and secure counseling and support. The EU helpline number is 116,016.
In June 2023, the European Council agreed on its position regarding the proposal for a directive on combating violence against women and domestic violence. In this, it is stated that “Violence against women and domestic violence are matters of criminal law, violations of human rights, and forms of discrimination. Their combat falls within the action of the European Commission aimed at protecting the fundamental values of the EU and ensuring respect for the Charter of Fundamental Rights of the European Union.” The directive establishes minimum standards regarding the rights of victims and the protection and assistance of victims, thus configuring as offenses in the EU female genital mutilation, online stalking, online harassment, non-consensual sharing of intimate or manipulated material, incitement to hatred or violence online [19]. For these offenses, the proposal also contains provisions concerning sanctions, aggravating circumstances, jurisdiction, and limitation periods. Female genital mutilation, for example, must become punishable across all Member States with a maximum penalty of at least five years of imprisonment [4,16].
As already mentioned, Europe does not have specific laws on gender-based violence, but based on the general orientation achieved with the Council directive, the Council initiated dialog with the European Parliament, and as a result, the Istanbul Convention entered into force throughout the EU on 1 October 2023 [20,21].
In Northern Europe, despite being at the forefront globally regarding gender equality, the so-called “Nordic paradox” manifests itself as the dark side of gender equality. These countries exhibit rates of intimate partner violence (IPV) against women higher than the EU average: 32% in Denmark, 30% in Finland, 28% in Sweden, and 22.4% in Iceland, compared to the EU average of 22%. This inconsistency highlights how deeply rooted this issue is in society and underscores the need for further measures to prevent and combat it [22,23,24].
In France—Central Europe—the increase in cases of domestic violence is concerning, with over 244,000 reported victims in 2022, marking a 15% increase and a staggering 95% surge since 2017. Women constitute 87% of these victims, primarily experiencing physical violence (66%), followed by verbal or psychological violence (30%) and sexual violence (4%). The French government has strengthened its commitment with a substantial increase in the budget to EUR 2.4 billion for 2023, representing an increase of EUR 921.1 million compared to the previous year [22]. Additionally, a French study has highlighted that the issue also affects the male population, although further research is needed to better understand the extent of this phenomenon. This study revealed that forensic expertise plays a central role in the identification and management of violence [25].
In Portugal—Southern Europe—data indicate that in 2022, there were over 30,000 reports of domestic violence, resulting in 28 deaths, including 24 women and four children [22]. Additionally, a study has highlighted that those legal sanctions aimed at discouraging violence may not be sufficient for certain offenders. This study advocates for the need for a predictive model to quantify the risk of repeated cases of intimate partner violence (IPV) in the Portuguese population [26]. Similarly, in Spain, the situation does not appear to be better than in the rest of Southern Europe [27,28].
3.3. Italian National Health Service on the Topic of Violence
The Italian National Health Service provides a network of services, both territorial and hospital-based, as well as socio-healthcare and socio-assistance services, available to all victims of violence, both Italian and foreign, aiming to ensure an integrated intervention model. As previously mentioned, one of the most common places to intercept victims is the emergency room. It is here that victims of violence, sometimes unaware of their real condition, turn to for initial healthcare intervention. Specifically, for the timely and adequate management of victims presenting at the emergency room, national guidelines for healthcare facilities were adopted in 2017 regarding emergency and socio-healthcare assistance for women victims of violence. Unless it is necessary to assign an emergency code (red or emergency) to the victim, an urgency code (orange or urgent) should be assigned to ensure prompt medical examination and minimize the risk of reconsideration or voluntary departure. It is also stipulated that the victim should be accompanied to a separate area from the general waiting room, ensuring protection, safety, and privacy. However, since violence often remains hidden, it is important to strengthen the skills of socio-healthcare operators who encounter these victims through specific training programs. Hence, arises the need for a dedicated pathway and the creation of a new severity code: the pink code [17].
3.4. What Is the Pink Code
The “pink code” is a specific triage code in the emergency department, alongside other codes of clinical priority already present in emergency departments, which identifies an access pathway reserved for all victims of violence, whether they are women, men, children, or individuals discriminated against based on ethnicity, religious belief, or social class, with a gender-sensitive approach [29,30].
The purpose of this “privileged” and targeted pathway is to ensure more effective coordination among various institutions and consequently provide a response that is as adequate as possible to the needs presented by the victim of violence upon arrival at the emergency department. The pink code has several objectives, including enabling early recognition of cases of violence, ensuring adequate and timely diagnostic and treatment pathways; coordinating various competent institutions in the field of violence to provide an effective response as quickly as possible; allowing an uninterrupted continuum of actions from the treatment of injuries or conditions resulting from violence to discharge and follow-up of the individual in the community network, always based on the specific needs of the victim in question; and finally, this dedicated pathway aims to ensure equitable treatment across the entire national territory. When initiating a pink code, complex healthcare machinery is activated that is composed of multiple professional figures. This includes doctors—often with multiple specialists’ present—nurses, social workers, psychologists, professionals from anti-violence services, and law enforcement. The cohesive intervention of this task force firstly enables the provision of initial medical care to the case at hand, followed by psychological and social support. Subsequently, it facilitates mediating communication with the relevant authorities (law enforcement, courts, local social services, and protected facilities), always respecting confidentiality and safeguarding the privacy and “silent times” of the victims, especially regarding their choice of the pathway to follow after treatment. The main task of the group is, therefore, to provide socio-healthcare and judicial assistance to victims of violence, with particular attention to bringing to light those episodes of violence in which victims often find it difficult to disclose being subjected to violence by others: a reluctance often due to fear of further violence or retaliation. Among the various tasks of the task force activated with the pink code, perhaps the most concrete and decisive element is the close collaboration with law enforcement, which speeds up the investigation process and any subsequent criminal proceedings and allows for a real picture of the various—and unfortunately numerous—situations of distress and violence present in the territory. The dedicated pathway of the pink code is activated regardless of the mode of access to the national health service: whether it occurs in the emergency department (ED), outpatient area, or regular hospitalization area; it always involves the implementation of precise procedures and the activation of dedicated pathways both within the facility and subsequently in the community, with the aim of providing comprehensive care to the victim. The pathway involves an initial phase of welcoming and identifying the “fragile patient” by the triage nurse, followed by the involvement of emergency department physicians and nurses, the victim protection phase managed by law enforcement, and finally, the handover of the victim to local social assistance services, with the cooperation of social services [31].
3.5. Figures Involved in the Pink Code and the Forensic Physician
As previously mentioned, the pink code relies on various professional figures who work together in harmony, each in their respective fields of expertise, for the ultimate goal of ensuring the victim’s well-being. The team includes the physician who takes care of the victim presenting at the emergency department (ED), a psychologist, a psychiatrist, an infectious disease specialist, a social worker, a gynecologist, a professional from anti-violence centers, and a forensic physician. Specialists of various kinds are involved, and their skills are called upon to provide appropriate healthcare assistance and the right support in terms of health, psychosocial, and territorial aspects. The pink code provides highly qualified and multidisciplinary assistance. The professionals made available, besides addressing the ongoing emergency, can provide information, advice, and clarification or deepen the care pathway in order to provide the right tools to combat violence. The operators involved have specific training and preparation; the victim’s care must be initiated within 30 min of their arrival at the hospital facility; not only the patient’s clinical status but also their psychological and social state must be evaluated. The violence suffered is assessed according to a classification and an evaluation of the risk of violence escalation (Brief Risk Assessment for the Emergency Department: DA-5). Furthermore, law enforcement is alerted to initiate the legal process that may result from the violence. Based on the injuries reported by the victim, additional specialized figures may be activated. Naturally, in cases of physical injuries and/or issues of a medicolegal nature, forensic medical consultation may also be activated.
A forensic physician is a specialized professional in the field of medicine that deals with the relationship between medicine and law. Their main task is to ascertain and evaluate the health status, both physical and psychological, of a victim and any legal consequences. The role of this professional is crucial in disputes related to civil liability, criminal responsibility, or medical–legal liability. Another important aspect of the forensic physician’s work is the medical history of the injurious event and the objective examination of the resulting injury. A deep understanding of forensic pathology and injuries forms the basis of the forensic physician’s work and the examination of the victim of violence. The intervention of this specialized figure also serves to establish the presence of the so-called material causal nexus between two events, a preceding one and a subsequent one, which have a cause-and-effect relationship; establishing such a relationship naturally requires a thorough understanding of the characteristics of the subsequent event, namely the injuries that have affected the physical and psychological integrity of the individual, resulting in biological damage. An expert in forensic medicine, preferably specialized, also with psychiatric/psychological expertise, is skilled in distinguishing various injuries, describing them, and associating them with an event and a causative agent, thereby offering greater guarantees of objective rigor in a context where clinical data are or will be used for judicial purposes [32]. Traumatic injuries are closely related to the injuring agent that caused them, which can be represented by any means capable of causing harm, whether intentional or accidental. The forensic physician can better distinguish whether the trauma is single or multiple, simultaneous, or repeated over time, than any other specialist. Furthermore, the effects of trauma can be local (if they develop at the site of action of the injuring agent) or distant; regarding timing, the effects of trauma can also be immediate or delayed, triggering a sequence of events connected to each other. Finally, the forensic physician, with their expertise, enables a swifter initiation of a legal process that may result from the violence, supported by the findings highlighted during the examination. This professional figure, therefore, serves as the privileged and often necessary consultant to formulate a diagnosis regarding the hypothesis of abuse or violence against the victim and to carry out investigations and fulfill obligations useful for forensic purposes [32].
Knowing how to recognize and accurately collect evidence for analysis in order to ensure proper custody is a requirement for which there is not always the necessary sensitivity on the part of the clinical specialists who intervene in the victim’s initial care. This is because, through training, they are mentally oriented towards providing assistance. As stated by the Italian Geneticists Group (GeFI) [33], it is crucial to follow certain procedures very precisely. In light of this, the “Guidelines for the collection of biological samples for forensic genetics analysis in the care pathway of victims of sexual violence and/or abuse” have been proposed [34], which were then included in the decree referring to national guidelines for health and hospital companies regarding emergency assistance and socio-healthcare assistance for women victims of violence [17]. Adherence to these guidelines and the accuracy of evidence collection is therefore essential to produce evidence in any potential legal proceedings [35,36,37].
3.6. Victims of Violence and Psychological Damage
Psychological damage is understood as an alteration of the psychological integrity and personality balance of an individual who is a victim of a traumatic event, resulting in a significant limitation of personality and daily life functioning. Since the psyche is not directly observable, the assessment of damage can only be made based on its functioning and the ability to objectively describe the alteration of certain mental processes compared to the condition prior to the unlawful act [38,39]. Although recent studies agree on the need for a radical reassessment of the importance of the effects of violence on women’s mental health, the greatest difficulty lies in conceptualization and defining psychological damage related to violence of various natures [40,41,42]. This issue is evidenced by the wide range of terminology used in the literature to refer to psychological violence and the effects of violence on the human psyche, often referred to as emotional abuse, coercion, psychological aggression, and so forth [43]. It is known that the effects on victims of violence can be diverse and can manifest both physically and psychologically. Among the psychological effects are post-traumatic stress disorder (PTSD), depression, and anxiety. If symptoms appear within two days to four weeks after the trauma, it is referred to as acute stress disorder, while if symptoms persist over time, it will be called post-traumatic stress disorder. It is of fundamental importance to remember that symptoms can also have a delayed onset, meaning they may not manifest in a period immediately following exposure to the traumatic event [44,45,46,47]. In addition to PTSD symptoms, victims may develop symptoms of trauma re-experiencing, including intrusive thoughts related to the trauma, recurring nightmares, or flashbacks; symptoms of avoidance; reduced interest or participation in activities previously considered significant; diminished affectivity; and a sense of foreshortened future. Some studies have shown that some women victims of violence have a higher risk compared to the general population in terms of substance abuse, alcohol abuse, or binge eating. Recently, a particular disorder has been highlighted in individuals who have experienced violence: Aggression-Related Obsessive–Compulsive Disorder. This is a subtype of Obsessive–Compulsive Disorder, where intrusive thoughts (obsessions) are related to intense fear of thinking, saying, or committing intentional or unintentional harmful or aggressive actions towards oneself or others [48]. According to 2014 Istat data in Italy, more than half of the victims of violence experience psychological effects, including loss of trust and self-esteem (52.75%), anxiety, phobia, and panic attacks (46.8%), despair and feelings of helplessness (46.4%), sleep and eating disorders (46.3%), depression (40.3%), difficulty concentrating and memory loss (24.9%), recurring body pains (21.8%), difficulties in managing children (14.8%), and finally, self-harm or suicidal thoughts (12.1%). Compared to the general population, a woman who is a victim of violence is at a 5/6 times higher risk of depression than a woman who has not experienced violence [48].
It is crucial to provide immediate psychological support to victims of violence in order to protect and manage their psychological damage, starting with support from family members or those close to them, without causing secondary traumatization. In the latter case, there is a risk that the victim may not feel understood or listened to and may even feel blamed. Secondary traumatization is extremely dangerous because it undermines the victim’s future expectations of receiving help. Victims often feel a sense of guilt and shame for what they have endured, feeling that they somehow provoked or deserved the aggression. After family support, a crucial place for protecting both physical and psychological damage is the hospital emergency department. It is essential for medical and nursing staff to be sensitive and empathetic towards the victim in order to avoid further secondary traumatization [49,50].
4. Discussion
Worldwide data are alarming, and human rights violations are sadly commonplace in every latitude. The pink code appears to be a theoretically effective tool for providing victims of violence with comprehensive and personalized assistance not only on the clinical but also on the social level. Although it is not identified throughout Europe as the pink code, the Italian National Health Service pathway is dedicated to victims of violence, and as we have seen, the pervasiveness of the issue is recognized in every European country.
However, from the analysis of the literature and our experience in Roman hospitals regarding violence and the pink code, we have found that, unfortunately, the role of the forensic physician in the hospital setting is mostly perceived only as a reference figure for risk management and for the hospital’s medical–legal disputes. From our assessment, however, scientific evidence leads us to other considerations; we have noticed that although the forensic physician is among the specialists to consult in cases of violence victims, this consultation only occurs in extreme cases or those recognized as such by the first aid healthcare professionals; the forensic physician is therefore not routinely alerted and is absent during most initial visits; this is to the detriment of the victim and the subsequent collection and validity of the evidence that can be used in criminal proceedings.
Considering that ethics, professional ethics, and medical duty primarily require the treatment of morbidity, it is clear that every access to healthcare facilities in cases of violence must be adequately identified and promptly treated without any exclusion. However, once the treatment pathway has been initiated, it is convenient and useful, both for the victim and for the healthcare professional conducting the initial assessment, to seek the assistance of the forensic physician. The expertise of the forensic physician combines the purely healthcare–curative training of the clinician with the legal–forensic perspective, which cannot be overlooked in this context. The need to identify the injuries caused by violence from the first medical assessment is evidently of great help in subsequent legal proceedings, as it inevitably conditions the collection of samples that could be incomplete or invalid if not carried out according to appropriate methodology. In these cases, the presence of an expert medical forensic specialist provides greater assurance of not losing those elements that, while perhaps of little use for healthcare purposes, can be of great importance in the context of a judicial investigation. Many operators in the field of forensic investigations, not only the group of Italian forensic geneticists, emphasize that medical-legal expertise must be physically present in emergency departments: the forensic physician must be enabled to operate and do so to the best of their ability for the ultimate goal of the victim’s well-being, in every facet it may present [33,34,51,52,53] In essence, the forensic physician represents the meeting point between all specialized figures that encounter the victim of violence within an emergency department and must always be considered in the patient’s assessment, allowing all information collected by experts to converge in one direction: that of achieving the patient’s health and respecting the rights of the citizen.
During the initial examination of a victim of violence, it is crucial to perform a detailed description of the injuries caused by the trauma, not only aimed at their subsequent treatment but also capable of going beyond the medical limit and, in fact, surpassing it with objective forensic rigor, considering potential legal–forensic implications. It is important to meticulously describe the anatomical site, with reference to topographical relationships and the morphological characteristics of individual injuries. Notably, the “simple” description of the injury is not always so precise, and often the first healthcare professionals who intervene following an assault describe the signs present on the victim incorrectly. So, for instance, what may initially be described as strangulation (mechanical asphyxia perpetrated by compressing the upper respiratory pathways forcefully using only the hands) becomes choking (compression exerted on the upper respiratory pathways using any mechanical means). Similarly, a stab wound (a continuous incision deepening into tissues caused by instruments with sharp edges and pointed ends) is categorized as a cutting injury (superficial wounds caused by the use of a blade with a sharp edge) or, even worse, as a laceration/contusion injury from a blunt object (continuous solutions of the skin and underlying soft tissues, produced by a blunt object, with a tearing mechanism and bruising of the edges).
As can be well understood, distinguishing between different injuries may not have significant value in the immediate medical treatment of the injuries themselves. However, it represents a significant advantage from a legal standpoint in the event of subsequent criminal proceedings. Defining and describing an injury for what it truly is could even be the basis for initiating the legal process itself or ensuring the successful outcome of criminal proceedings. That is why, during the pink code pathway, the forensic physician, preferably and especially during the initial examination of a victim of violence, must also proceed with the documentation of photographs, refining the etiopathogenetic and circumstantial assessment, as well as the collection and preservation of all items (clothing and personal belongings of the victim), and biological samples useful for forensic and legal–technical purposes (chain of custody). This is carried out in order to highlight and avoid the loss of evidence, often transient and fleeting, of the violence itself, thereby also avoiding further stress on the victim, who is already burdened with physical and psychological distress.
A forensic physician can provide a significant contribution to the field of violence medicine by assessing the nature of the injury, the modality, and dynamics that can have multiple variations, starting primarily from the importance of detecting the right elements in a scientific and appropriate manner. Some scientific studies demonstrate that conducting a clinical forensic assessment in these situations correlates with a higher diagnostic probability of abuse cases compared to assessments performed by other specialists [51]. Conducting an initial medical examination not only by a clinician for the treatment of injuries but also by a forensic physician, performed according to a methodology based on forensic objective rigor, can have a significant impact on the subsequent legal course of the case under examination [52]. Additionally, knowledge in the field of toxicology and forensic genetics [53], which are areas of expertise in forensic medicine, can provide decisive elements for correctly reconstructing the dynamics of violence.
5. Limitations
This study is not without limitations. The first limitation is the use of a single search engine, but the data extracted are nonetheless representative of the pervasive global phenomenon. Another limitation is the study of only English-language documents; we are confident that a study based on documents written in other languages would have yielded broader and more usable results, but our research has nevertheless proven satisfactory in terms of the multicultural assessment of the issue.
Author Contributions
Conceptualization, L.D.P., D.T. and G.N.; methodology, L.D.P.; software, D.T.; validation. E.M., G.M.V. and S.Z.; formal analysis, G.N.; investigation, L.D.P., D.T. and G.N.; resources, E.M., G.M.V. and S.Z.; data curation, L.D.P., D.T. and G.N.; writing—original draft preparation, L.D.P., D.T. and G.N.; writing—review and editing, E.M., G.M.V. and S.Z.; visualization, L.D.P., D.T., G.N., E.M., G.M.V. and S.Z.; supervision, E.M., G.M.V. and S.Z.; project administration, L.D.P. and D.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Violence against Women. Available online: https://www.who.int/news-room/fact-sheets/detail/violence-against-women (accessed on 15 December 2023).
- Convention on the Elimination of All Forms of Discrimination against Women New York, 18 December 1979. Available online: https://www.ohchr.org/en/instruments-mechanisms/instruments/convention-elimination-all-forms-discrimination-against-women (accessed on 15 December 2023).
- OHCHR. General Recommendation No. 35 (2017) on Gender-Based Violence against Women, Updating General Recommendation No. 19 (1992). CEDAW_GR_35.Pdf. Available online: https://www.ohchr.org/en/documents/general-comments-and-recommendations/general-recommendation-no-35-2017-gender-based (accessed on 15 December 2023).
- Zagloul, N.M.; Farghaly, R.M.; ELKhatib, H.; Issa, S.Y.; El-Zoghby, S.M. Technology Facilitated Sexual Violence: A Comparative Study between Working and Non-Working Females in Egypt before and during the COVID-19 Pandemic. Egypt. J. Forensic Sci. 2022, 12, 21. [Google Scholar] [CrossRef] [PubMed]
- Le Vittime di Omicidio—Anno 2022. Available online: https://www.istat.it/it/archivio/291266 (accessed on 18 December 2023).
- UNIFEM Resources on Women, Peace and Security. Available online: https://www.unwomen.org/en/digital-library/publications/2010/1/unifem-resources-on-women-peace-and-security (accessed on 18 December 2023).
- Morena, D.; De Paola, L.; Ottaviani, M.; Spadazzi, F.; Zamponi, M.V.; Delogu, G.; Di Fazio, N. Obstetric Violence in Italy: From Theoretical Premises to Court Judgments. Clin. Ter. 2024, 175, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Volonnino, G.; Spadazzi, F.; De Paola, L.; Arcangeli, M.; Pascale, N.; Frati, P.; La Russa, R. Healthcare Workers: Heroes or Victims? Context of the Western World and Proposals to Prevent Violence. Healthcare 2024, 12, 708. [Google Scholar] [CrossRef]
- Kaur, N.; Byard, R.W. Dowry Deaths and Honor Killings. In Forensic and Legal Medicine; CRC Press: Boca Raton, FL, USA, 2023; ISBN 978-1-00-313875-4. [Google Scholar]
- 8 Marzo—Stop alla Violenza Sulle Donne. Available online: https://www.amnesty.ch/it/news/2007/8-marzo-giornata-mondiale-della-donna (accessed on 8 April 2024).
- Omicidi Volontari e Violenza di Genere. Available online: http://www.interno.gov.it/it/stampa-e-comunicazione/dati-e-statistiche/omicidi-volontari-e-violenza-genere (accessed on 15 December 2023).
- Il Punto—Il Pregiudizio e la Violenza Contro le Donne. (interno.gov.it). Available online: https://www.interno.gov.it/sites/default/files/2023-12/il_punto_-_il_pregiudizio_e_la_violenza_contro_le_donne.pdf (accessed on 15 December 2023).
- Salute, M. Della 25 Novembre, Giornata Internazionale per L’eliminazione Della Violenza Contro le Donne. Available online: https://www.salute.gov.it/portale/donna/dettaglioNotizieDonna.jsp?lingua=italiano&menu=notizie&p=dalministero&id=6071 (accessed on 17 May 2024).
- Available online: https://www.istat.it/it/files/2023/05/Accessi-pronto-soccorso-donne-5mag2023.pdf (accessed on 15 December 2023).
- Pichini, S.; Mannocchi, G.; Berretta, P.; Zaami, S.; Pirani, F.; Pacifici, R.; Busardò, F.P. Δ9-Tetrahydrocannabinol and Cannabidiol Time Courses in the Sera of “Light Cannabis” Smokers: Discriminating Light Cannabis Use from Illegal and Medical Cannabis Use. Ther. Drug Monit. 2020, 42, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Zupi, d.M. La Convenzione del Consiglio d’Europa sulla Prevenzione e la Lotta Contro la Violenza nei Confronti Delle Donne e la Violenza Domestica (Convenzione di Istanbul). (parlamento.it). Available online: https://www.parlamento.it/application/xmanager/projects/parlamento/file/repository/affariinternazionali/osservatorio/approfondimenti/85_CeSPI_Convenzione_Istanbul.pdf (accessed on 15 December 2023).
- Gazzetta Ufficiale. Available online: https://www.gazzettaufficiale.it/eli/id/2018/01/30/18A00520/SG (accessed on 18 December 2023).
- Guidelines for Medico-Legal Care for Victims of Sexual Violence. (who.int). Available online: https://iris.who.int/bitstream/handle/10665/42788/924154628X.pdf (accessed on 18 December 2023).
- Zaami, S.; Stark, M.; Beck, R.; Malvasi, A.; Marinelli, E. Does Episiotomy Always Equate Violence in Obstetrics? Routine and Selective Episiotomy in Obstetric Practice and Legal Questions. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 1847–1854. [Google Scholar] [CrossRef] [PubMed]
- EU Measures to End Violence against Women. Available online: https://www.consilium.europa.eu/en/policies/eu-measures-end-violence-against-women/ (accessed on 18 December 2023).
- Lotta Contro la Violenza nei Confronti Delle Donne: La Convenzione di Istanbul Entra in Vigore per l’UE—Commissione Europea. Available online: https://italy.representation.ec.europa.eu/notizie-ed-eventi/notizie/lotta-contro-la-violenza-nei-confronti-delle-donne-la-convenzione-di-istanbul-entra-vigore-lue-2023-09-29_it (accessed on 18 December 2023).
- ONU Italia. La Lotta alla Violenza di Genere si Intensifica in Tutta Europa. Available online: https://unric.org/it/la-lotta-alla-violenza-di-genere-si-intensifica-in-tutta-europa/ (accessed on 8 April 2024).
- Jónasdóttir, D.; Thorsteinsdottir, T.; Ásgeirsdóttir, T.L.; Lund, S.H.; Arnarsson, E.Ö.; Ashikali, E.; Líndal, Þ.; Mogensen, B. Women and Intimate Partner Violence: Prevalence of Hospital Visits and Nature of Injuries in the Icelandic Population. Scand. J. Public Health 2021, 49, 260–267. [Google Scholar] [CrossRef] [PubMed]
- Gracia, E.; Martín-Fernández, M.; Lila, M.; Merlo, J.; Ivert, A.-K. Prevalence of Intimate Partner Violence against Women in Sweden and Spain: A Psychometric Study of the “Nordic Paradox”. PLoS ONE 2019, 14, e0217015. [Google Scholar] [CrossRef] [PubMed]
- Savall, F.; Lechevalier, A.; Hérin, F.; Vergnault, M.; Telmon, N.; Bartoli, C. A Ten-Year Experience of Physical Intimate Partner Violence (IPV) in a French Forensic Unit. J. Forensic Leg. Med. 2017, 46, 12–15. [Google Scholar] [CrossRef] [PubMed]
- Vieira-Pinto, P.; Muñoz-Barús, J.I.; Taveira-Gomes, T.; Vidal-Alves, M.J.; Magalhães, T. Intimate Partner Violence against Women. Does Violence Decrease after the Entry of the Alleged Offender into the Criminal Justice System? Forensic Sci. Res. 2022, 7, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Regueira-Diéguez, A.; Pérez-Rivas, N.; Muñoz-Barús, J.I.; Vázquez-Portomeñe, F.; Rodríguez-Calvo, M.S. Intimate Partner Violence against Women in Spain: A Medico-Legal and Criminological Study. J. Forensic Leg. Med. 2015, 34, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Katsos, K.; Sakelliadis, E.I.; Zorba, E.; Tsitsika, A.; Papadodima, S.; Spiliopoulou, C. Intimate Partner Violence in Greece: A Study of 664 Consecutive Forensic Clinical Examinations. Fam. Pract. 2020, 37, 801–806. [Google Scholar] [CrossRef] [PubMed]
- PERCORSO ROSA DEF. (quotidianosanita.it). Available online: https://www.quotidianosanita.it/allegati/allegato8601915.pdf (accessed on 15 December 2023).
- Dumont, N.; Martrille, L.; Albuisson, E.; Baland-Peltre, K.; Marchand, E. Examining Men as Victims of Intimate Partner Violence in a French Forensic Department. Forensic Sci. Int. 2022, 337, 111368. [Google Scholar] [CrossRef] [PubMed]
- Codice Rosa—Differenzadonna.org. Available online: https://www.differenzadonna.org/ (accessed on 18 December 2023).
- Franceschetti, L.; Merelli, V.G.; Margherita, M.; Maggioni, L.; Barbara, G.; Kustermann, A.; Cattaneo, C. Older Adult Abuse in a Service for Sexual and Domestic Violence: Medico-Legal Implications from the Experience of an Italian Center. Forensic Sci. Int. 2022, 338, 111383. [Google Scholar] [CrossRef] [PubMed]
- Gino, S.; Bo, M.; Ricciardelli, R.; Alù, M.; Boschi, I.; Carnevali, E.; Fabbri, M.; Fattorini, P.; Piccinini, A.; Previderè, C.; et al. Evaluation of Critical Aspects in Clinical and Forensic Management of Sexual Violence: A Multicentre Ge.F.I. Project. Forensic Sci. Int. 2020, 314, 110387. [Google Scholar] [CrossRef] [PubMed]
- Blandino, A.; Maggioni, L.; Chiaffarino, F.; Parazzini, F.; Capano, D.; Florio, E.M.; Margherita, M.; Bertelle, G.M.; Franceschetti, L.; Amadasi, A.; et al. Sexual Assault and Abuse Committed against Family Members: An Analysis of 1342 Legal Outcomes and Their Motivations. PLoS ONE 2021, 16, e0253980. [Google Scholar] [CrossRef] [PubMed]
- Gray-Eurom, K.; Seaberg, D.C.; Wears, R.L. The Prosecution of Sexual Assault Cases: Correlation with Forensic Evidence. Ann. Emerg. Med. 2002, 39, 39–46. [Google Scholar] [CrossRef]
- Busardò, F.P.; Vaiano, F.; Mannocchi, G.; Bertol, E.; Zaami, S.; Marinelli, E. Twelve Months Monitoring of Hair GHB Decay Following a Single Dose Administration in a Case of Facilitated Sexual Assault. Drug Test. Anal. 2017, 9, 953–956. [Google Scholar] [CrossRef] [PubMed]
- Linee Guida per la Repertazione di Tracce Biologiche per le Analisi di Genetica Forense nel Percorso Assistenziale Delle Vittime di Violenza Sessuale e/o Maltrattamento. (gefi-isfg.org). Available online: https://www.gefi-isfg.org/temp/2202201374428.pdf (accessed on 15 December 2023).
- Pliske, G.; Heide, S.; Lucas, B.; Brandstädter, K.; Walcher, F.; Kropf, S.; Lessig, R.; Piatek, S. Legal medicine specialists within the framework of acute care: Analysis of legal medicine consultations in relation to the victims’ statistics of the state office of criminal investigation in Saxony-Anhalt. Unfallchirurg 2018, 121, 391–396. [Google Scholar] [CrossRef] [PubMed]
- Soldaini, D.F. Il Danno Psichico, Morale e Esistenziale: Riflessioni Circa un Possibile Risarcimento in casi di Vittime da Rapina. (aipgitalia.org). Available online: https://aipgitalia.org/wp-content/uploads/2008/10/Soldainitesina.pdf (accessed on 15 December 2023).
- Marinelli, S.; Basile, G.; De Paola, L.; Napoletano, G.; Zaami, S. Consequences of COVID-19 Restrictions on Adolescent Mental Health and Drug Abuse Dynamics. Eur. Rev. Med. Pharmacol. Sci. 2024, 28, 836–851. [Google Scholar] [CrossRef] [PubMed]
- Heise, L.; Pallitto, C.; García-Moreno, C.; Clark, C.J. Measuring Psychological Abuse by Intimate Partners: Constructing a Cross-Cultural Indicator for the Sustainable Development Goals. SSM Popul. Health 2019, 9, 100377. [Google Scholar] [CrossRef]
- Jewkes, R. Emotional Abuse: A Neglected Dimension of Partner Violence. Lancet 2010, 376, 851–852. [Google Scholar] [CrossRef] [PubMed]
- Domenech Del Rio, I.; Sirvent Garcia Del Valle, E. The Consequences of Intimate Partner Violence on Health: A Further Disaggregation of Psychological Violence-Evidence From Spain. Violence Against Women 2017, 23, 1771–1789. [Google Scholar] [CrossRef]
- Dokkedahl, S.; Kok, R.N.; Murphy, S.; Kristensen, T.R.; Bech-Hansen, D.; Elklit, A. The Psychological Subtype of Intimate Partner Violence and Its Effect on Mental Health: Protocol for a Systematic Review and Meta-Analysis. Syst. Rev. 2019, 8, 198. [Google Scholar] [CrossRef] [PubMed]
- Sonnenberg, S.M. Victims of Violence and Post-Traumatic Stress Disorder. Psychiatr. Clin. N. Am. 1988, 11, 581–590. [Google Scholar] [CrossRef]
- American Psychiatric Association (Ed.) Diagnostic and Statistical Manual of Mental Disorders: DSM-5, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013; ISBN 978-0-89042-554-1. [Google Scholar]
- Barchielli, B.; Lausi, G.; Pizzo, A.; Messineo, M.; Del Casale, A.; Giannini, A.M.; Ferracuti, S. A Medical-Legal and Psychological Systematic Review on Vitriolage Related to Gender-Based Violence. Trauma Violence Abus. 2023, 24, 2953–2965. [Google Scholar] [CrossRef] [PubMed]
- Istat.it—Violenza Sulle Donne. Available online: https://www.istat.it/it/violenza-sulle-donne/il-fenomeno/violenza-dentro-e-fuori-la-famiglia/gravita-e-conseguenze (accessed on 17 May 2024).
- Aguglia, E.; Botter, V.; Riolo, A. La violenza di genere: Un problema di salute pubblica. Riv. Psichiatr. 2011, 46, 89–96. [Google Scholar] [PubMed]
- Rosenberg, M.L.; Fenley, M.A.; Johnson, D.; Short, L. Bridging Prevention and Practice: Public Health and Family Violence. Acad. Med. 1997, 72, S13–S18. [Google Scholar] [PubMed]
- Vittime Di Violenza. Simla: “Servono Medici Legali in Tutti i Pronto Soccorso”—Quotidiano Sanità. Available online: https://www.quotidianosanita.it/lavoro-e-professioni/articolo.php?articolo_id=115826 (accessed on 18 December 2023).
- Responding to Intimate Partner Violence and Sexual Violence against Women. Available online: https://www.who.int/publications-detail-redirect/9789241548595 (accessed on 18 December 2023).
- Abedr-Rahman, H.; Salameh, H.O.; Salameh, R.J.; Alabdallat, L.I.; Al-Abdallat, I.M. Role of Forensic Medicine in Evaluating Non-Fatal Physical Violence against Women by Their Husbands in Jordan. J. Forensic Leg. Med. 2017, 49, 33–36. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).