Association of Foot Sole Sensibility with Quiet and Dynamic Body Balance in Morbidly Obese Women
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Evaluations, Equipment and Procedures
2.3. Data Collection and Analysis
3. Results
3.1. Plantar Sensibility
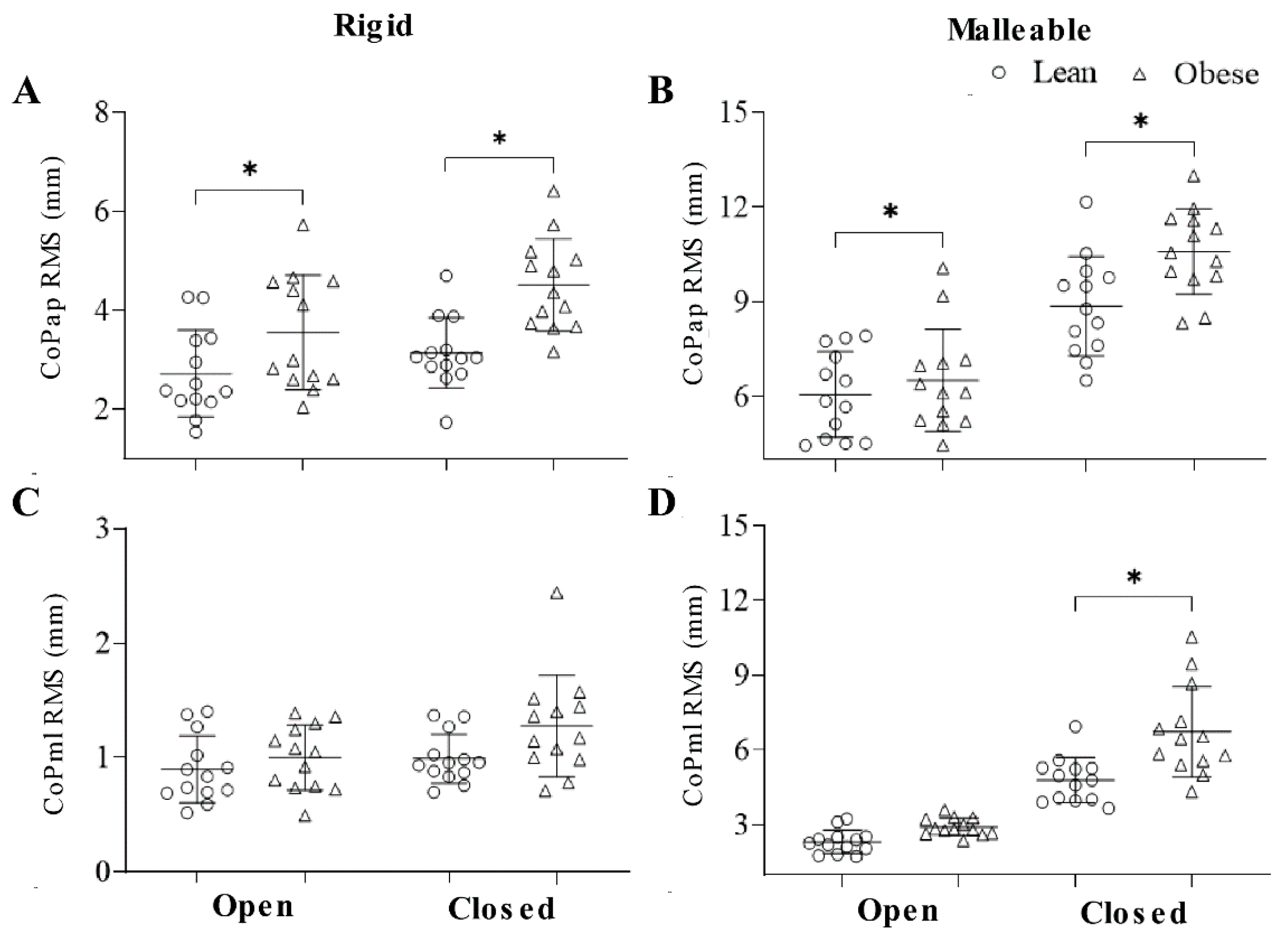
3.2. Quiet Stance
3.3. Dynamic Balance
4. Discussion
4.1. Quiet Balance
4.2. Dynamic Balance
4.3. Plantar Sensibility and Balance
5. Conclusions, Applications and Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hue, O.; Simoneau, M.; Marcotte, J.; Berrigan, F.; Doré, J.; Marceau, P.; Marceau, S.; Tremblay, A.; Teasdale, N. Body weight is a strong predictor of postural stability. Gait Posture 2007, 26, 32–38. [Google Scholar] [CrossRef]
- Dutil, M.; Handrigan, G.A.; Corbeil, P.; Cantin, V.; Simoneau, M.; Teasdale, N.; Hue, O. The impact of obesity on balance control in community-dwelling older women. Age 2013, 35, 883–890. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ku, P.X.; Osman, N.A.; Yusof, A.; Abas, W.W. Biomechanical evaluation of the relationship between postural control and body mass index. J. Biomech. 2012, 45, 1638–1642. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maktouf, W.; Boyas, S.; Beaune, B.; Durand, S. Differences in lower extremity muscular coactivation during postural control between healthy and obese adults. Gait Posture 2020, 81, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Menegoni, F.; Galli, M.; Tacchini, E.; Vismara, L.; Cavigioli, M.; Capodaglio, P. Gender-specific effect of obesity on balance. Obesity 2009, 17, 1951–1956. [Google Scholar] [CrossRef] [PubMed]
- Meng, H.; Gorniak, S.L. Effects of adiposity on postural control and cognition in older adults. Gait Posture 2020, 82, 147–152. [Google Scholar] [CrossRef]
- Meng, H.; O’Connor, D.P.; Lee, B.-C.; Layne, C.S.; Gorniak, S.L. Effects of adiposity on postural control and cognition. Gait Posture 2016, 43, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Corbeil, P.; Simoneau, M.; Rancourt, D.; Tremblay, A.; Teasdale, N. Increased risk for falling associated with obesity: Mathematical modeling of postural control. IEEE Trans. Neural Syst. Rehabil. Eng. 2001, 9, 126–136. [Google Scholar] [CrossRef]
- Neri, S.G.; Harvey, L.A.; Tiedemann, A.; Gadelha, A.B.; Lima, R.M. Obesity and falls in older women: Mediating effects of muscle quality, foot loads and postural control. Gait Posture 2020, 77, 138–143. [Google Scholar] [CrossRef] [PubMed]
- Han, T.; Tijhuis, M.; Lean, M.; Seidell, J. Quality of life in relation to overweight and body fat distribution. Am. J. Public Health 1998, 88, 1814–1820. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berrigan, F.; Simoneau, M.; Tremblay, A.; Hue, O.; Teasdale, N. Influence of obesity on accurate and rapid arm movement performed from a standing posture. Int. J. Obes. 2006, 30, 1750–1757. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Do Nascimento, J.; Silva, C.; Dos Santos, H.; de Almeida Ferreira, J.; De Andrade, P. A preliminary study of static and dynamic balance in sedentary obese young adults: The relationship between BMI, posture and postural balance. Clin. Obes. 2017, 7, 377–383. [Google Scholar] [CrossRef] [PubMed]
- Błaszczyk, J.W.; Cieślinska-Świder, J.; Plewa, M.; Zahorska-Markiewicz, B.; Markiewicz, A. Effects of excessive body weight on postural control. J. Biomech. 2009, 42, 1295–1300. [Google Scholar] [CrossRef] [PubMed]
- Teasdale, N.; Simoneau, M.; Corbeil, P.; Handrigan, G.; Tremblay, A.; Hue, O. Obesity alters balance and movement control. Curr. Obes. Rep. 2013, 2, 235–240. [Google Scholar] [CrossRef] [Green Version]
- Birtane, M.; Tuna, H. The evaluation of plantar pressure distribution in obese and non-obese adults. Clin. Biomech. 2004, 19, 1055–1059. [Google Scholar] [CrossRef] [PubMed]
- Hills, A.; Hennig, E.; McDonald, M.; Bar-Or, O. Plantar pressure differences between obese and non-obese adults: A biomechanical analysis. Int. J. Obes. 2001, 25, 1674–1679. [Google Scholar] [CrossRef] [Green Version]
- Dowling, A.; Steele, J.; Baur, L. What are the effects of obesity in children on plantar pressure distributions? Int. J. Obes. 2004, 28, 1514–1519. [Google Scholar] [CrossRef] [Green Version]
- Song, J.; Kane, R.; Tango, D.N.; Vander Veur, S.S.; Furmato, J.; Komaroff, E.; Foster, G.D. Effects of weight loss on foot structure and function in obese adults: A pilot randomized controlled trial. Gait Posture 2015, 41, 86–92. [Google Scholar] [CrossRef] [Green Version]
- Ajisafe, T.; Gilson, A.; Garcia, T.; DeAnda, N. Obesity, but not overweight, is associated with plantar light touch sensation in children aged 8 to 16 years: A cross-sectional study. Obes. Sci. Pract. 2020, 6, 107–116. [Google Scholar] [CrossRef] [Green Version]
- Yümin, E.T.; Şimşek, T.T.; Sertel, M.; Ankaralı, H. The effect of age and body mass index on plantar cutaneous sensation in healthy women. J. Phys. Ther. Sci. 2016, 28, 2587–2595. [Google Scholar] [CrossRef] [Green Version]
- Bueno, J.W.F.; Coelho, D.B.; de Souza, C.R.; Teixeira, L.A. Associations between women’s obesity status and diminished cutaneous sensibility across foot sole regions. Percept. Mot. Skills 2021, 128, 243–257. [Google Scholar] [CrossRef]
- Wu, X.; Madigan, M.L. Impaired plantar sensitivity among the obese is associated with increased postural sway. Neurosci. Lett. 2014, 583, 49–54. [Google Scholar] [CrossRef]
- Matsudo, S.; Araújo, T.; Matsudo, V.; Andrade, D.; Andrade, E.; Oliveira, L.; Braggion, G. International physical activity questionnaire (IPAQ): Study of validity and reliability in Brazil. Rev. Bras. Ativ. Fis. Saúde 2001, 6, 5–18. [Google Scholar]
- Bell-Krotoski, J. Advances in sensibility evaluation. Hand Clin. 1991, 7, 527–546. [Google Scholar] [CrossRef]
- Perry, S.D. Evaluation of age-related plantar-surface insensitivity and onset age of advanced insensitivity in older adults using vibratory and touch sensation tests. Neurosci. Lett. 2006, 392, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Collins, S.; Visscher, P.; De Vet, H.C.; Zuurmond, W.W.; Perez, R.S. Reliability of the Semmes Weinstein monofilaments to measure coetaneous sensibility in the feet of healthy subjects. Disabil. Rehabil. 2010, 32, 2019–2027. [Google Scholar] [CrossRef]
- Bell-Krotoski, J. “Pocket filaments” and specifications for the semmes-weinstein monofilaments. J. Hand Ther. 1990, 3, 26–31. [Google Scholar] [CrossRef]
- Snyder, B.A.; Munter, A.D.; Houston, M.N.; Hoch, J.M.; Hoch, M.C. Interrater and intrarater reliability of the semmes-weinstein monofilament 4-2-1 stepping algorithm. Muscle Nerve 2016, 53, 918–924. [Google Scholar] [CrossRef] [PubMed]
- Kutner, M.H.; Nachtsheim, C.J.; Neter, J.; Li, W. Applied Linear Statistical Models; McGraw-Hill Irwin: Boston, MA, USA, 2005; Volume 5. [Google Scholar]
- Oie, K.S.; Kiemel, T.; Jeka, J.J. Multisensory fusion: Simultaneous re-weighting of vision and touch for the control of human posture. Cogn. Brain Res. 2002, 14, 164–176. [Google Scholar] [CrossRef]
- Peterka, R.J. Sensorimotor integration in human postural control. J. Neurophysiol. 2002, 88, 1097–1118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simoneau, M.; Teasdale, N. Balance control impairment in obese individuals is caused by larger balance motor commands variability. Gait Posture 2015, 41, 203–208. [Google Scholar] [CrossRef]
- Mignardot, J.-B.; Olivier, I.; Promayon, E.; Nougier, V. Obesity impact on the attentional cost for controlling posture. PLoS ONE 2010, 5, e14387. [Google Scholar] [CrossRef] [PubMed]
- Kavounoudias, A.; Roll, R.; Roll, J.-P. The plantar sole is a ‘dynamometric map’for human balance control. Neuroreport 1998, 9, 3247–3252. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kennedy, P.M.; Inglis, J.T. Distribution and behaviour of glabrous cutaneous receptors in the human foot sole. J. Physiol. 2002, 538, 995–1002. [Google Scholar] [CrossRef]
- Meyer, P.F.; Oddsson, L.I.; De Luca, C.J. The role of plantar cutaneous sensation in unperturbed stance. Exp. Brain Res. 2004, 156, 505–512. [Google Scholar] [CrossRef] [PubMed]
- Peters, R.M.; McKeown, M.D.; Carpenter, M.G.; Inglis, J.T. Losing touch: Age-related changes in plantar skin sensitivity, lower limb cutaneous reflex strength, and postural stability in older adults. J. Neurophysiol. 2016, 116, 1848–1858. [Google Scholar] [CrossRef] [Green Version]
- Buchanan, J.J.; Horak, F.B. Voluntary control of postural equilibrium patterns. Behav. Brain Res. 2003, 143, 121–140. [Google Scholar] [CrossRef]
- Teixeira, L.A.; Coutinho, J.d.F.S.; Coelho, D.B. Regulation of dynamic postural control to attend manual steadiness constraints. J. Neurophysiol. 2018, 120, 693–702. [Google Scholar] [CrossRef]
- Kennedy, P.M.; Carlsen, A.N.; Inglis, J.T.; Chow, R.; Franks, I.M.; Chua, R. Relative contributions of visual and vestibular information on the trajectory of human gait. Exp. Brain Res. 2003, 153, 113–117. [Google Scholar] [CrossRef]
- Noohi, F.; Kinnaird, C.; DeDios, Y.; Kofman, I.S.; Wood, S.; Bloomberg, J.; Mulavara, A.; Seidler, R. Functional brain activation in response to a clinical vestibular test correlates with balance. Front. Syst. Neurosci. 2017, 11, 11. [Google Scholar] [CrossRef] [Green Version]
- Dietz, V.; Trippel, M.; Ibrahim, I.; Berger, W. Human stance on a sinusoidally translating platform: Balance control by feedforward and feedback mechanisms. Exp. Brain Res. 1993, 93, 352–362. [Google Scholar] [CrossRef] [PubMed]
- Jilk, D.J.; Safavynia, S.A.; Ting, L.H. Contribution of vision to postural behaviors during continuous support-surface translations. Exp. Brain Res. 2014, 232, 169–180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Teixeira, L.A.; Maia Azzi, N.; de Oliveira, J.Á.; Ribeiro de Souza, C.; da Silva Rezende, L.; Boari Coelho, D. Automatic postural responses are scaled from the association between online feedback and feedforward control. Eur. J. Neurosci. 2020, 51, 2023–2032. [Google Scholar] [CrossRef] [PubMed]
- Kennefick, M.; McNeil, C.J.; Burma, J.S.; Copeland, P.V.; van Donkelaar, P.; Dalton, B.H. Modulation of vestibular-evoked responses prior to simple and complex arm movements. Exp. Brain Res. 2020, 238, 869–881. [Google Scholar] [CrossRef]
- Miscio, G.; Guastamacchia, G.; Brunani, A.; Priano, L.; Baudo, S.; Mauro, A. Obesity and peripheral neuropathy risk: A dangerous liaison. J. Peripher. Nerv. Syst. 2005, 10, 354–358. [Google Scholar] [CrossRef] [PubMed]
- Lhomond, O.; Teasdale, N.; Simoneau, M.; Mouchnino, L. Neural consequences of increasing body weight: Evidence from somatosensory evoked potentials and the frequency-specificity of brain oscillations. Front. Hum. Neurosci. 2016, 10, 318. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Lean | Obese | |
|---|---|---|
| Weight (Kg) | 56.02 (5.22) [51–68] | 124.72 (16.59) [100–157] |
| Height (cm) | 159.0 (5.52) [148–171] | 160.38 (8,92) [143–177] |
| BMI (Kg/m2) | 22.17 (1.79) [20.14–24.84] | 48.39 (4.01) [43.09–57.30] |
| Waist circumference (cm) | 79.08 (6.65) [69–89] | 135.54 (10.63) [121–150] |
| Hip circumference (cm) | 94.15 (3.85) [90–102] | 144.08 (9.07) [128–165] |
| IPAQ (min) | 197.31 (144.03) [0–525] | 315.77 (231.63) [0–780] |
| Lean | Obese | All | |||||
|---|---|---|---|---|---|---|---|
| rs | p | rs | p | rs | p | ||
| Rigid | |||||||
| CoPap RMS (mm) | open | 0.27 | 0.37 | −0.44 | 0.13 | 0.27 | 0.19 |
| closed | 0.12 | 0.69 | −0.33 | 0.27 | 0.48 | 0.01 | |
| CoPml RMS (mm) | open | 0.72 | <0.01 | −0.37 | 0.21 | 0.31 | 0.13 |
| closed | 0.68 | 0.01 | 0.22 | 0.48 | 0.61 | <0.01 | |
| Malleable | |||||||
| CoPap RMS (mm) | open | −0.37 | 0.21 | −0.41 | 0.17 | −0.17 | 0.40 |
| closed | 0.09 | 0.76 | 0.04 | 0.90 | 0.44 | 0.03 | |
| CoPml RMS (mm) | open | 0.52 | 0.07 | 0.63 | 0.02 | 0.72 | <0.01 |
| closed | 0.57 | 0.04 | 0.69 | <0.01 | 0.75 | <0.01 | |
| Lean | Obese | |||||
|---|---|---|---|---|---|---|
| Open | Closed | Open | Closed | Factor | p | |
| Trunk frequency (Hz) | 0.50 | 0.50 | 0.49 | 0.50 | group | 0.09 |
| (0.01) | (0.01) | (0.02) | (0.02) | vision | 0.40 | |
| Trunk amplitude (mm) | 73.73 | 69.07 | 82.16 | 74.53 | group | 0.31 |
| (14.10) | (13.95) | (26.73) | (15.92) | vision | 0.03 | |
| CoPap RMS (mm) | 20.39 | 20.24 | 18.73 | 18.07 | group | 0.52 |
| (3.97) | (4.47) | (12.44) | (7.75) | vision | 0.70 | |
| CoPml RMS (mm) | 7.62 | 8.69 | 11.03 | 11.47 | group | 0.18 |
| (1.90) | (2.99) | (8.26) | (7.16) | vision | 0.08 | |
| Lean | Obese | All | |||||
|---|---|---|---|---|---|---|---|
| rs | p | rs | p | rs | p | ||
| CoPap (mm) | open | 0.44 | 0.13 | 0.11 | 0.73 | −0.18 | 0.37 |
| closed | 0.22 | 0.47 | 0.24 | 0.42 | −0.17 | 0.42 | |
| CoPml (mm) | open | 0.30 | 0.32 | 0.35 | 0.24 | 0.43 | 0.03 |
| closed | 0.31 | 0.30 | 0.54 | 0.06 | 0.39 | 0.05 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bueno, J.W.F.; Coelho, D.B.; de Souza, C.R.; Teixeira, L.A. Association of Foot Sole Sensibility with Quiet and Dynamic Body Balance in Morbidly Obese Women. Biomechanics 2021, 1, 334-345. https://doi.org/10.3390/biomechanics1030028
Bueno JWF, Coelho DB, de Souza CR, Teixeira LA. Association of Foot Sole Sensibility with Quiet and Dynamic Body Balance in Morbidly Obese Women. Biomechanics. 2021; 1(3):334-345. https://doi.org/10.3390/biomechanics1030028
Chicago/Turabian StyleBueno, Jair Wesley Ferreira, Daniel Boari Coelho, Caroline Ribeiro de Souza, and Luis Augusto Teixeira. 2021. "Association of Foot Sole Sensibility with Quiet and Dynamic Body Balance in Morbidly Obese Women" Biomechanics 1, no. 3: 334-345. https://doi.org/10.3390/biomechanics1030028
APA StyleBueno, J. W. F., Coelho, D. B., de Souza, C. R., & Teixeira, L. A. (2021). Association of Foot Sole Sensibility with Quiet and Dynamic Body Balance in Morbidly Obese Women. Biomechanics, 1(3), 334-345. https://doi.org/10.3390/biomechanics1030028






