Biomechanical Risk Factors of Injury-Related Single-Leg Movements in Male Elite Youth Soccer Players
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Participants and Injury Data Collection
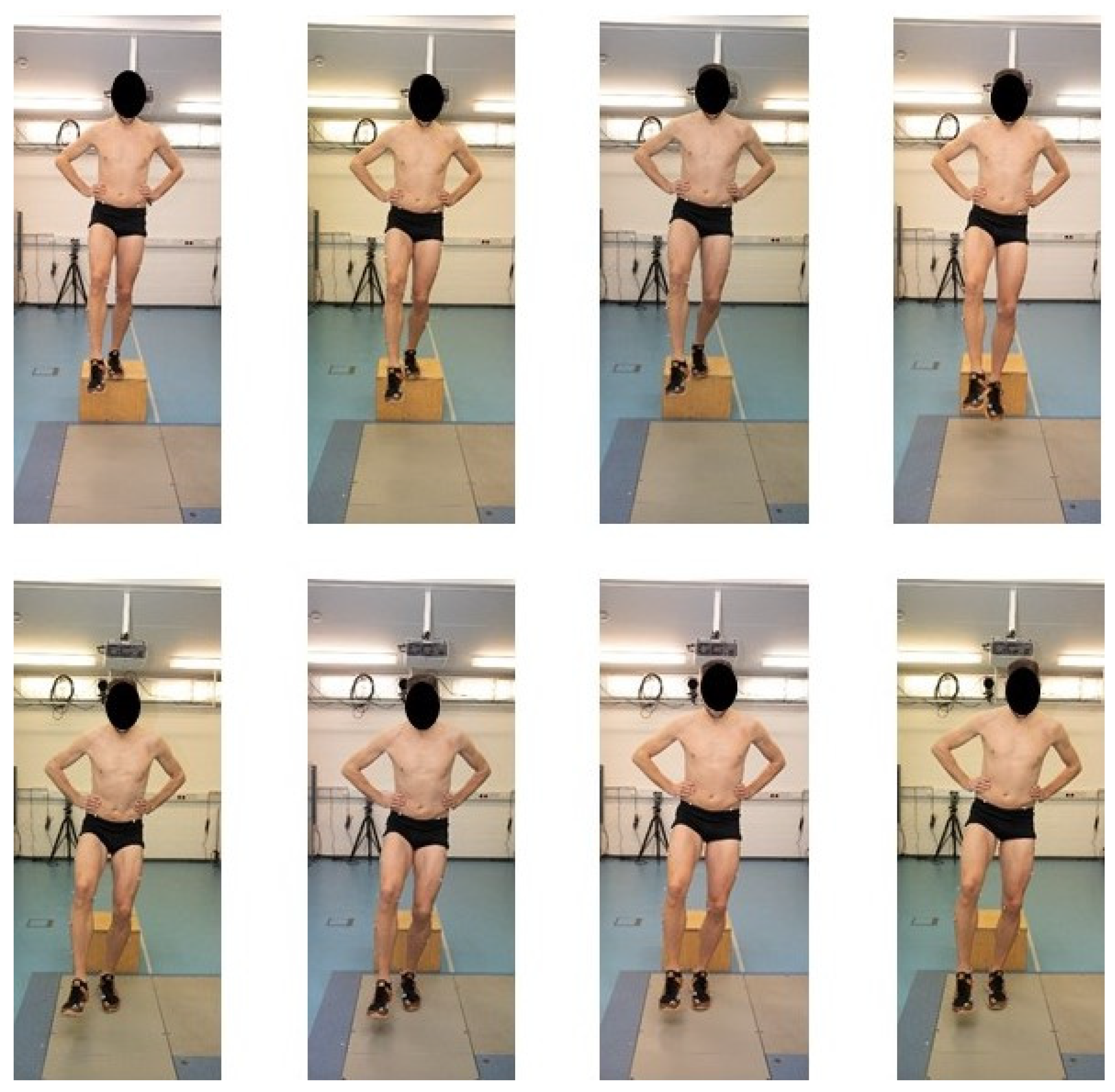
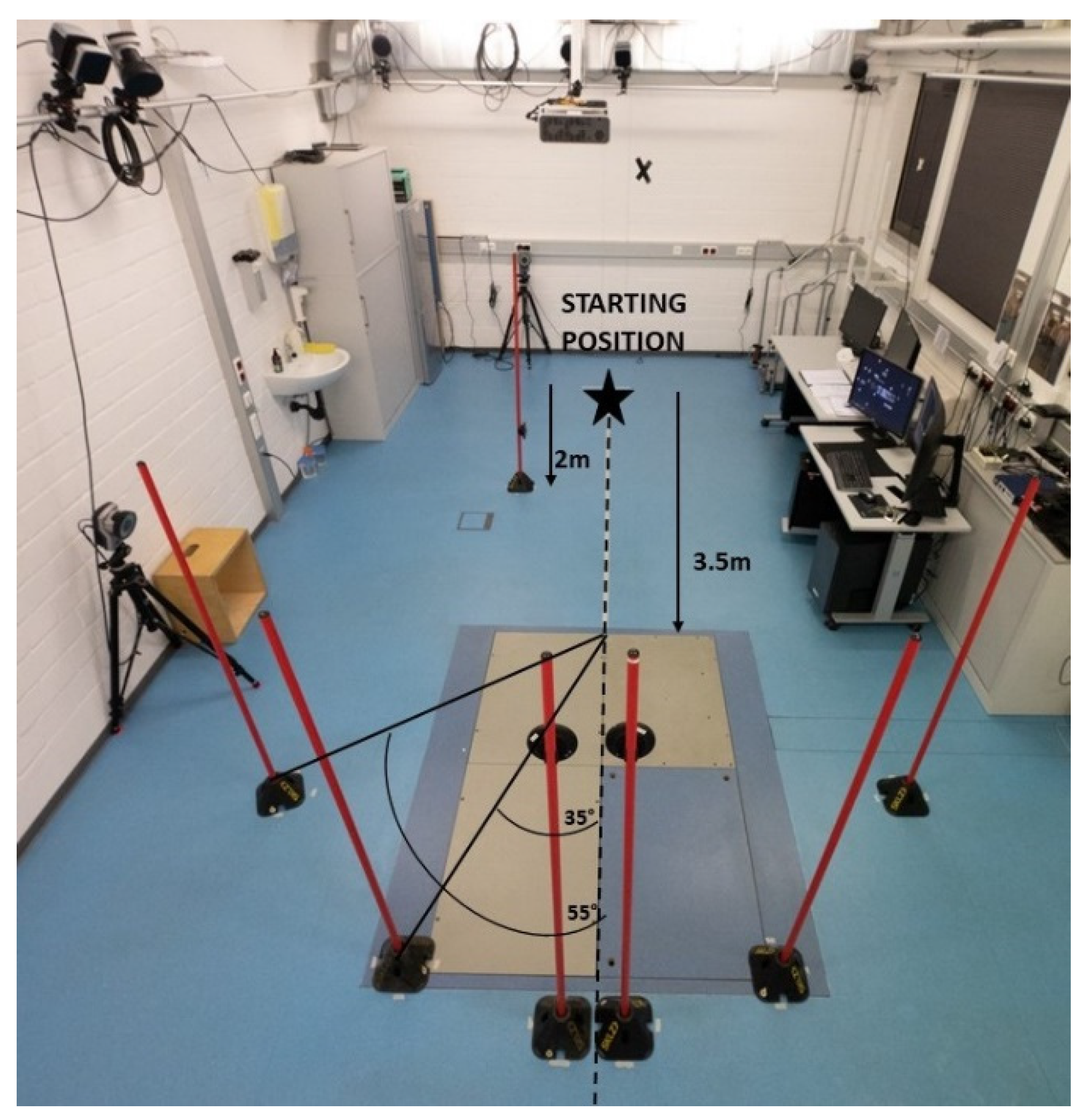
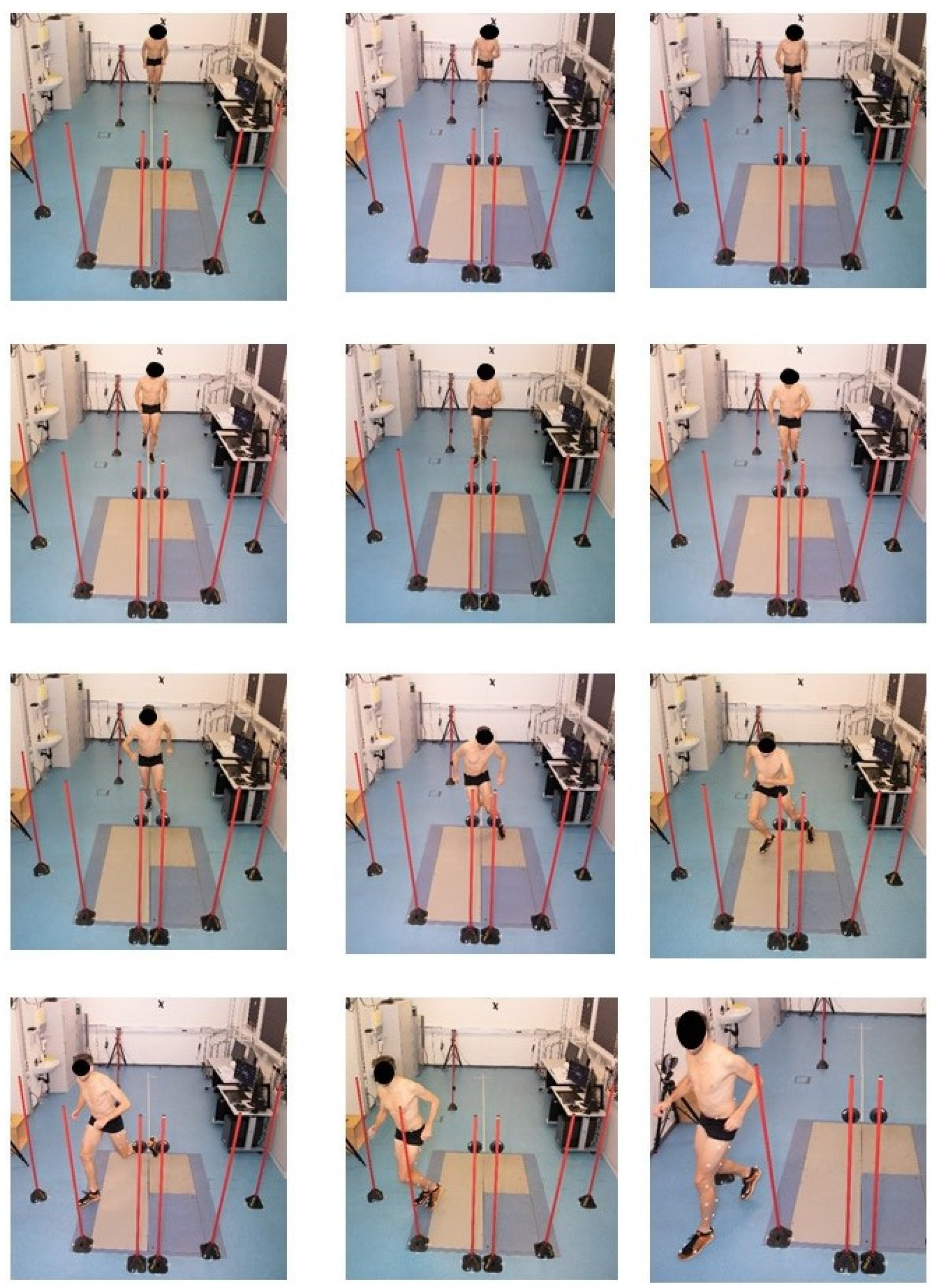
2.2. Experimental Protocol
2.3. Kinematic and Kinetic Analysis
2.4. Statistical Analyses
3. Results
3.1. Injury Epidemiology
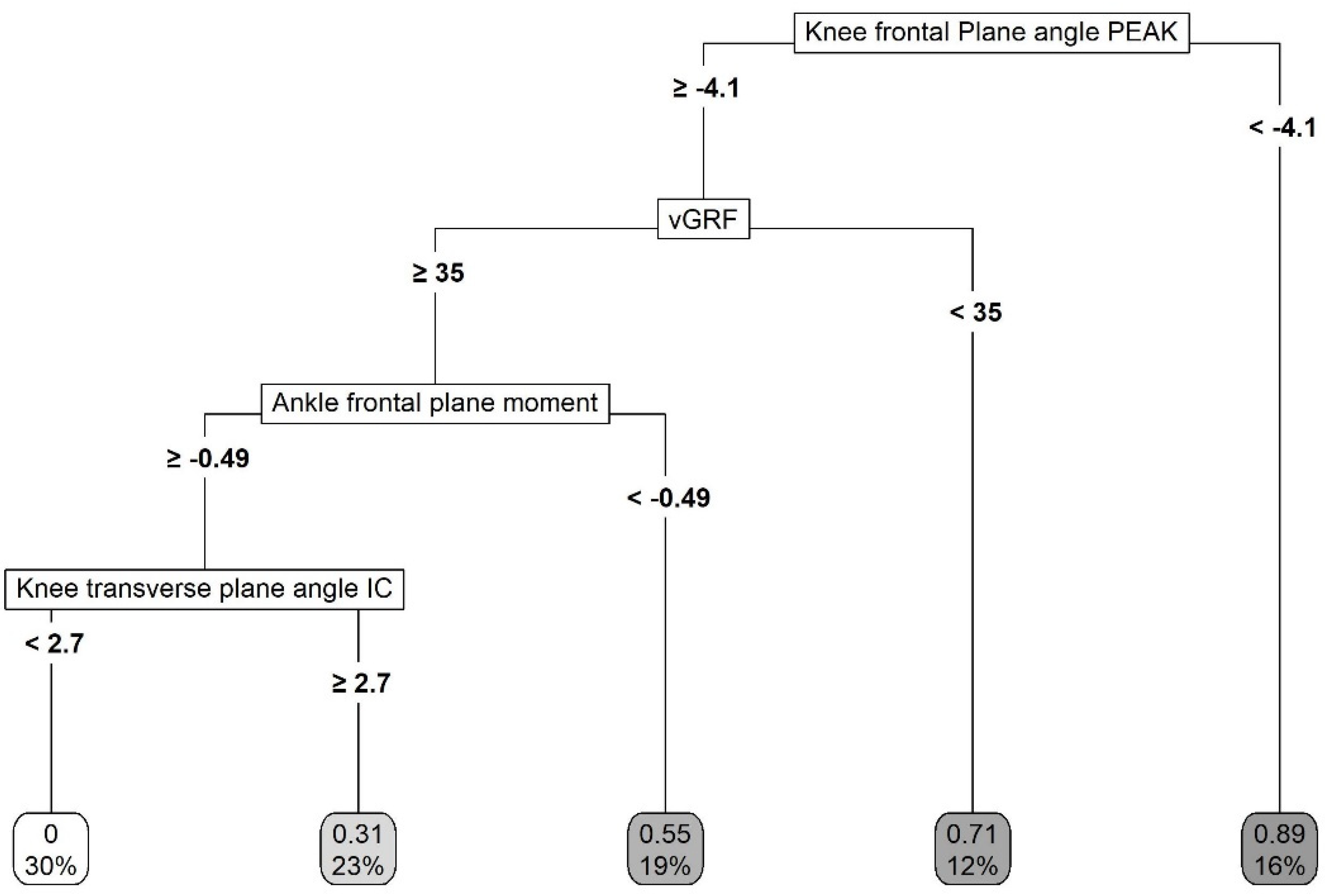
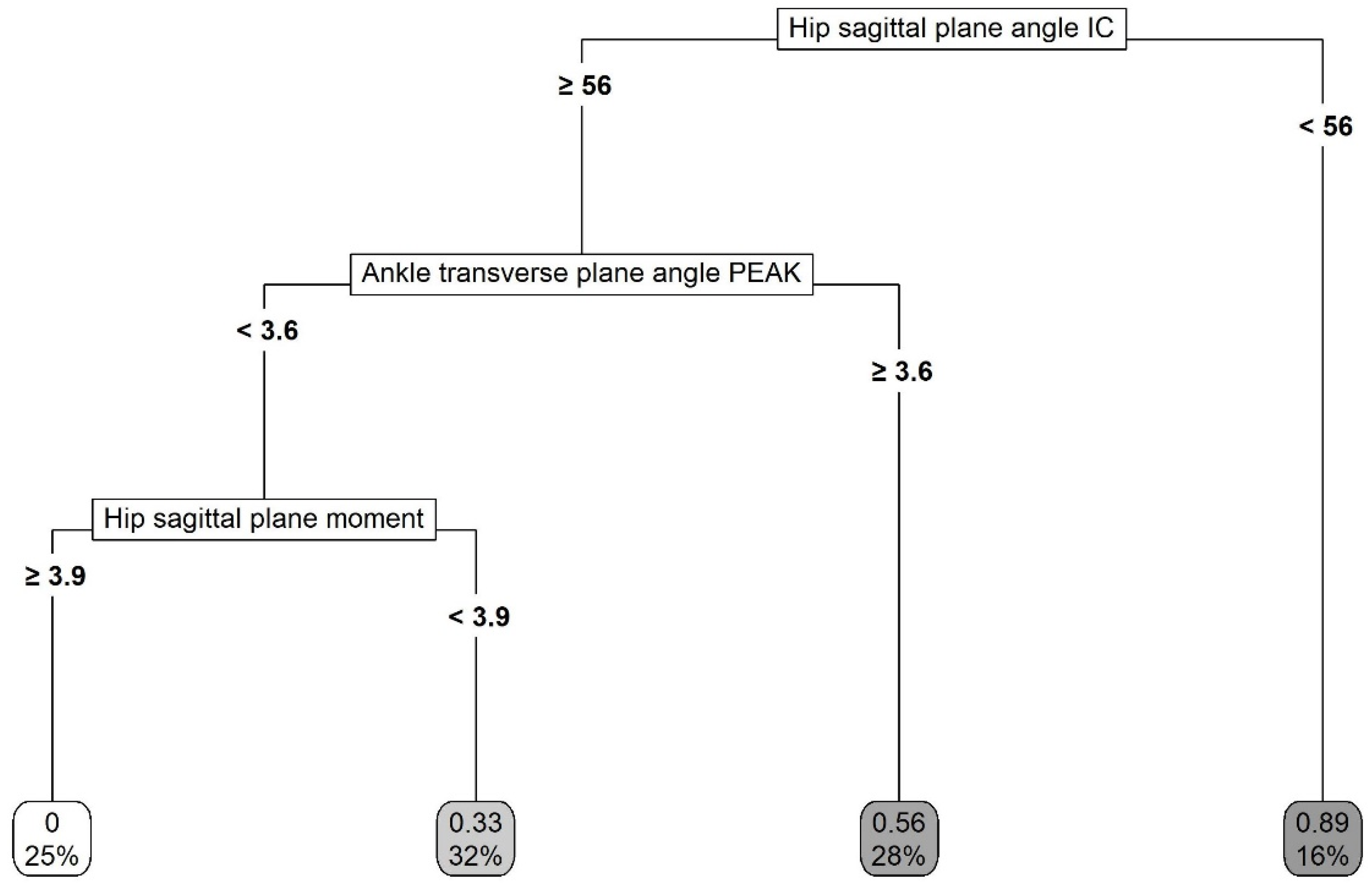
3.2. Multivariate Analysis
4. Discussion
4.1. Single-Leg Landing Task
4.2. Unanticipated Cutting Task
4.3. Practical Applications
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pfirrmann, D.; Herbst, M.; Ingelfinger, P.; Simon, P.; Tug, S. Analysis of injury incidences in male professional adult and elite youth soccer players: A systematic review. J. Athlet. Train. 2016, 51, 410–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Price, R.; Hawkins, R.; Hulse, M.; Hodson, A. The football association medical research programme: An audit of injuries in academy youth football. Br. J. Sports Med. 2004, 38, 466–471. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Renshaw, A.; Goodwin, P.C. Injury incidence in a premier league youth soccer academy using the consensus statement: A prospective cohort study. BMJ Open Sport Exerc. Med. 2016, 2, e000132. [Google Scholar] [CrossRef] [Green Version]
- Read, P.J.; Oliver, J.L.; De Ste Croix, M.B.; Myer, G.D.; Lloyd, R.S. Neuromuscular risk factors for knee and ankle ligament injuries in male youth soccer players. Sports Med. 2016, 46, 1059–1066. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zazulak, B.T.; Ponce, P.L.; Straub, S.J.; Medvecky, M.J.; Avedisian, L.; Hewett, T.E. Gender comparison of hip muscle activity during single-leg landing. J. Orthop. Sports Phys. Ther. 2005, 35, 292–299. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lehnert, M.; De Ste Croix, M.; Zaatar, A.; Hughes, J.; Varekova, R.; Lastovicka, O. Muscular and neuromuscular control following soccer-specific exercise in male youth: Changes in injury risk mechanisms. Scand. J. Med. Sci. Sports 2017, 27, 975–982. [Google Scholar] [CrossRef]
- Boden, B.P.; Sheehan, F.T.; Torg, J.S.; Hewett, T.E. Noncontact anterior cruciate ligament injuries: Mechanisms and risk factors. J. Am. Acad. Orthop. Surg. 2010, 18, 520–527. [Google Scholar] [CrossRef] [Green Version]
- Murphy, D.; Connolly, D.; Beynnon, B. Risk factors for lower extremity injury: A review of the literature. Br. J. Sports Med. 2003, 37, 13–29. [Google Scholar] [CrossRef] [Green Version]
- Whiting, W.C.; Zernicke, R.F. Biomechanics of Musculoskeletal Injury; Human Kinetics: Champaign, IL, USA, 2008. [Google Scholar]
- Ross, S.E.; Guskiewicz, K.M.; Yu, B. Single-leg jump-landing stabilization times in subjects with functionally unstable ankles. J. Athlet. Train. 2005, 40, 298–304. [Google Scholar]
- Hughes, G.; Watkins, J. A risk-factor model for anterior cruciate ligament injury. Sports Med. 2006, 36, 411–428. [Google Scholar] [CrossRef]
- Hewett, T.E.; Myer, G.D.; Ford, K.R.; Heidt, R.S., Jr.; Colosimo, A.J.; McLean, S.G.; van den Bogert, A.J.; Paterno, M.V.; Succop, P. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study. Am. J. Sports Med. 2005, 33, 492–501. [Google Scholar] [CrossRef] [Green Version]
- Dingenen, B.; Malfait, B.; Nijs, S.; Peers, K.H.; Vereecken, S.; Verschueren, S.M.; Staes, F.F. Can two-dimensional video analysis during single-leg drop vertical jumps help identify non-contact knee injury risk? A one-year prospective study. Clin. Biomech. 2015, 30, 781–787. [Google Scholar] [CrossRef] [PubMed]
- Alentorn-Geli, E.; Mendiguchia, J.; Samuelsson, K.; Musahl, V.; Karlsson, J.; Cugat, R.; Myer, G.D. Prevention of anterior cruciate ligament injuries in sports. Part I: Systematic review of risk factors in male athletes. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 3–15. [Google Scholar] [CrossRef]
- Fagenbaum, R.; Darling, W.G. Jump landing strategies in male and female college athletes and the implications of such strategies for anterior cruciate ligament injury. Am. J. Sports Med. 2003, 31, 233–240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Mechelen, W.; Hlobil, H.; Kemper, H.C. Incidence, severity, aetiology and prevention of sports injuries. A review of concepts. Sports Med. 1992, 14, 82–99. [Google Scholar] [CrossRef] [PubMed]
- Bahr, R. Why screening tests to predict injury do not work—And probably never will…: A critical review. Br. J. Sports Med. 2016, 50, 776–780. [Google Scholar] [CrossRef] [Green Version]
- Raisanen, A.M.; Arkkila, H.; Vasankari, T.; Steffen, K.; Parkkari, J.; Kannus, P.; Forsman, H.; Pasanen, K. Investigation of knee control as a lower extremity injury risk factor: A prospective study in youth football. Scand. J. Med. Sci. Sports 2018, 28, 2084–2092. [Google Scholar] [CrossRef] [Green Version]
- Aerts, I.; Cumps, E.; Verhagen, E.; Verschueren, J.; Meeusen, R. A systematic review of different jump-landing variables in relation to injuries. J. Sports Med. Phys. Fit. 2013, 53, 509–519. [Google Scholar]
- Myer, G.D.; Ford, K.R.; Khoury, J.; Succop, P.; Hewett, T.E. Development and validation of a clinic-based prediction tool to identify female athletes at high risk for anterior cruciate ligament injury. Am. J. Sports Med. 2010, 38, 2025–2033. [Google Scholar] [CrossRef] [Green Version]
- Myer, G.D.; Ford, K.R.; Khoury, J.; Succop, P.; Hewett, T.E. Biomechanics laboratory-based prediction algorithm to identify female athletes with high knee loads that increase risk of acl injury. Br. J. Sports Med. 2011, 45, 245–252. [Google Scholar] [CrossRef] [Green Version]
- Boden, B.P.; Torg, J.S.; Knowles, S.B.; Hewett, T.E. Video analysis of anterior cruciate ligament injury abnormalities in hip and ankle kinematics. Am. J. Sports Med. 2009, 37, 252–259. [Google Scholar] [CrossRef] [PubMed]
- Stolen, T.; Chamari, K.; Castagna, C.; Wisloff, U. Physiology of soccer: An update. Sports Med. 2005, 35, 501–536. [Google Scholar] [CrossRef]
- Strudwick, A. Soccer Science; Human Kinetics: Champaign, IL, USA, 2016. [Google Scholar]
- Taylor, J.B.; Ford, K.R.; Nguyen, A.-D.; Shultz, S.J. Biomechanical comparison of single-and double-leg jump landings in the sagittal and frontal plane. Orthop. J. Sports Med. 2016, 4, 2325967116655158. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dingenen, B.; Staes, F.F.; Janssens, L. A new method to analyze postural stability during a transition task from double-leg stance to single-leg stance. J. Biomech. 2013, 46, 2213–2219. [Google Scholar] [CrossRef] [PubMed]
- Yu, B.; Lin, C.-F.; Garrett, W.E. Lower extremity biomechanics during the landing of a stop-jump task. Clin. Biomech. 2006, 21, 297–305. [Google Scholar] [CrossRef]
- Bloomfield, J.; Polman, R.; O’Donoghue, P. Physical demands of different positions in fa premier league soccer. J. Sports Sci. Med. 2007, 6, 63. [Google Scholar]
- Almonroeder, T.G.; Garcia, E.; Kurt, M. The effects of anticipation on the mechanics of the knee during single-leg cutting tasks: A systematic review. Int. J. Sports Phys. Ther. 2015, 10, 918–928. [Google Scholar]
- Besier, T.F.; Lloyd, D.G.; Ackland, T.R.; Cochrane, J.L. Anticipatory effects on knee joint loading during running and cutting maneuvers. Med. Sci. Sports. Exerc. 2001, 33, 1176–1181. [Google Scholar] [CrossRef]
- Dempsey, A.R.; Lloyd, D.G.; Elliott, B.C.; Steele, J.R.; Munro, B.J. Changing sidestep cutting technique reduces knee valgus loading. Am. J. Sports Med. 2009, 37, 2194–2200. [Google Scholar] [CrossRef] [Green Version]
- Dempsey, A.R.; Lloyd, D.G.; Elliott, B.C.; Steele, J.R.; Munro, B.J.; Russo, K.A. The effect of technique change on knee loads during sidestep cutting. Med. Sci. Sports Exerc. 2007, 39, 1765–1773. [Google Scholar] [CrossRef] [Green Version]
- Chinnasee, C.; Weir, G.; Sasimontonkul, S.; Alderson, J.; Donnelly, C. A biomechanical comparison of single-leg landing and unplanned sidestepping. Int. J. Sports Med. 2018, 39, 636–645. [Google Scholar] [CrossRef] [PubMed]
- Arendt, E.; Dick, R. Knee injury patterns among men and women in collegiate basketball and soccer. Ncaa data and review of literature. Am. J. Sports Med. 1995, 23, 694–701. [Google Scholar] [CrossRef] [PubMed]
- Prodromos, C.C.; Han, Y.; Rogowski, J.; Joyce, B.; Shi, K. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury–reduction regimen. Arthrosc. J. Arthrosc. Relat. Surg. 2007, 23, 1320–1325.e1326. [Google Scholar] [CrossRef] [PubMed]
- Waldén, M.; Hägglund, M.; Werner, J.; Ekstrand, J. The epidemiology of anterior cruciate ligament injury in football (soccer): A review of the literature from a gender-related perspective. Knee Surg. Sports Traumat. Arthrosc. 2011, 19, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Shultz, S.J.; Schmitz, R.J.; Benjaminse, A.; Collins, M.; Ford, K.; Kulas, A.S. Acl research retreat vii: An update on anterior cruciate ligament injury risk factor identification, screening, and prevention. J. Athlet. Train. 2015, 50, 1076–1093. [Google Scholar] [CrossRef] [Green Version]
- Hrysomallis, C. Hip adductors’ strength, flexibility, and injury risk. J. Strength Cond. Res. 2009, 23, 1514–1517. [Google Scholar] [CrossRef]
- Wing, C.; Bishop, C. Hamstring strain injuries: Incidence, mechanisms, risk factors, and training recommendations. Strength Cond. J. 2020, 42, 40–57. [Google Scholar] [CrossRef]
- Fong, D.T.-P.; Hong, Y.; Chan, L.-K.; Yung, P.S.-H.; Chan, K.-M. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007, 37, 73–94. [Google Scholar] [CrossRef] [Green Version]
- De Bleecker, C.; Vermeulen, S.; De Blaiser, C.; Willems, T.; De Ridder, R.; Roosen, P. Relationship between jump-landing kinematics and lower extremity overuse injuries in physically active populations: A systematic review and meta-analysis. Sports Med. 2020, 50, 1515–1532. [Google Scholar] [CrossRef]
- Fuller, C.W.; Ekstrand, J.; Junge, A.; Andersen, T.E.; Bahr, R.; Dvorak, J.; Hagglund, M.; McCrory, P.; Meeuwisse, W.H. Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. Br. J. Sports Med. 2006, 40, 193–201. [Google Scholar] [CrossRef]
- Kolodziej, M.; Nolte, K.; Schmidt, M.; Alt, T.; Jaitner, T. Identification of neuromuscular performance parameters as risk factors of non-contact injuries in male elite youth soccer players: A preliminary study on 62 players with 25 non-contact injuries. Front. Sports Act. Living 2021, 3, 615330. [Google Scholar] [CrossRef] [PubMed]
- Russell, K.A.; Palmieri, R.M.; Zinder, S.M.; Ingersoll, C.D. Sex differences in valgus knee angle during a single-leg drop jump. J. Athl. Train. 2006, 41, 166–171. [Google Scholar]
- Pollard, C.D.; Sigward, S.M.; Powers, C.M. Gender differences in hip joint kinematics and kinetics during side-step cutting maneuver. Clin. J. Sport Med. 2007, 17, 38–42. [Google Scholar] [CrossRef] [Green Version]
- Jeong, J.; Choi, D.-H.; Shin, C.S. Core strength training can alter neuromuscular and biomechanical risk factors for anterior cruciate ligament injury. Am. J. Sports Med. 2021, 49, 183–192. [Google Scholar] [CrossRef] [PubMed]
- Dix, C.; Arundale, A.; Silvers-Granelli, H.; Marmon, A.; Zarzycki, R.; Snyder-Mackler, L. Biomechanical measures during two sport-specific tasks differentiate between soccer players who go on to anterior cruciate ligament injury and those who do not: A prospective cohort analysis. Int. Sports Phys. Ther. 2020, 15, 928. [Google Scholar] [CrossRef]
- Thomas, C.; Dos’ Santos, T.; Comfort, P.; Jones, P.A. Male and female soccer players exhibit different knee joint mechanics during pre-planned change of direction. Sports Biomech. 2020, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Kristianslund, E.; Krosshaug, T. Comparison of drop jumps and sport-specific sidestep cutting: Implications for anterior cruciate ligament injury risk screening. Am. J. Sports Med. 2013, 41, 684–688. [Google Scholar] [CrossRef]
- Kristianslund, E.; Faul, O.; Bahr, R.; Myklebust, G.; Krosshaug, T. Sidestep cutting technique and knee abduction loading: Implications for acl prevention exercises. Br. J. Sports Med. 2014, 48, 779–783. [Google Scholar] [CrossRef] [Green Version]
- Schmidt, M.; Nolte, K.; Terschluse, B.; Jaitner, T. Fatigue impairs kinematics but not kinetics of landing and cutting movements in elite youth female handball. ISBS Proc. Arch. 2020, 38, 696. [Google Scholar]
- Kristianslund, E.; Krosshaug, T.; Van den Bogert, A. Effect of low pass filtering on joint moments from inverse dynamics: Implications for injury prevention. J. Biomech. 2012, 45, 666–671. [Google Scholar] [CrossRef] [Green Version]
- Mai, P.; Willwacher, S. Effects of low-pass filter combinations on lower extremity joint moments in distance running. J. Biomech. 2019, 95, 109311. [Google Scholar] [CrossRef]
- Willwacher, S.; Kurz, M.; Menne, C.; Schrödter, E.; Brüggemann, G.-P. Biomechanical response to altered footwear longitudinal bending stiffness in the early acceleration phase of sprinting. Footwear Sci. 2016, 8, 99–108. [Google Scholar] [CrossRef]
- Willwacher, S.; Konig, M.; Braunstein, B.; Goldmann, J.P.; Bruggemann, G.P. The gearing function of running shoe longitudinal bending stiffness. Gait Posture 2014, 40, 386–390. [Google Scholar] [CrossRef] [PubMed]
- Koga, H.; Nakamae, A.; Shima, Y.; Iwasa, J.; Myklebust, G.; Engebretsen, L.; Bahr, R.; Krosshaug, T. Mechanisms for noncontact anterior cruciate ligament injuries: Knee joint kinematics in 10 injury situations from female team handball and basketball. Am. J. Sports Med. 2010, 38, 2218–2225. [Google Scholar] [CrossRef] [PubMed]
- Breiman, L.; Friedman, J.H.; Olshen, R.A.; Stone, C.J. Classification and regression trees. Belmont, ca: Wadsworth. Int. Group 1984, 432, 151–166. [Google Scholar]
- Ruddy, J.D.; Cormack, S.J.; Whiteley, R.; Williams, M.D.; Timmins, R.G.; Opar, D.A. Modeling the risk of team sport injuries: A narrative review of different statistical approaches. Front. Physiol. 2019, 10, 829. [Google Scholar] [CrossRef]
- Akobeng, A.K. Understanding diagnostic tests 1: Sensitivity, specificity and predictive values. Acta Paediatr. 2007, 96, 338–341. [Google Scholar] [CrossRef]
- Schmidt, C.O.; Kohlmann, T. When to use the odds ratio or the relative risk? Int. J. Public Health 2008, 53, 165. [Google Scholar] [CrossRef]
- Hewett, T.E.; Myer, G.D.; Ford, K.R.; Paterno, M.V.; Quatman, C.E. Mechanisms, prediction, and prevention of acl injuries: Cut risk with three sharpened and validated tools. J. Orthop. Res. 2016, 34, 1843–1855. [Google Scholar] [CrossRef] [Green Version]
- Nessler, T.; Denney, L.; Sampley, J. Acl injury prevention: What does research tell us? Curr. Rev. Musculoskelet. Med. 2017, 10, 281–288. [Google Scholar] [CrossRef] [Green Version]
- Silvers-Granelli, H.J.; Bizzini, M.; Arundale, A.; Mandelbaum, B.R.; Snyder-Mackler, L. Does the fifa 11+ injury prevention program reduce the incidence of acl injury in male soccer players? Clin. Orthop. Relat. Res. 2017, 475, 2447–2455. [Google Scholar] [CrossRef] [PubMed]
- Romero-Franco, N.; Ortego-Mate, M.d.C.; Molina-Mula, J. Knee kinematics during landing: Is it really a predictor of acute noncontact knee injuries in athletes? A systematic review and meta-analysis. Orthop. J. Sports Med. 2020, 8, 2325967120966952. [Google Scholar] [CrossRef] [PubMed]
- Krosshaug, T.; Steffen, K.; Kristianslund, E.; Nilstad, A.; Mok, K.M.; Myklebust, G.; Andersen, T.E.; Holme, I.; Engebretsen, L.; Bahr, R. The vertical drop jump is a poor screening test for acl injuries in female elite soccer and handball players: A prospective cohort study of 710 athletes. Am. J. Sports Med. 2016, 44, 874–883. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cronström, A.; Creaby, M.W.; Ageberg, E. Do knee abduction kinematics and kinetics predict future anterior cruciate ligament injury risk? A systematic review and meta-analysis of prospective studies. BMC Musculoskelet. Disord. 2020, 21, 563. [Google Scholar] [CrossRef]
- Wong, P.; Hong, Y. Soccer injury in the lower extremities. Br. J. Sports Med. 2005, 39, 473–482. [Google Scholar] [CrossRef]
- Powers, C.M.; Ghoddosi, N.; Straub, R.K.; Khayambashi, K. Hip strength as a predictor of ankle sprains in male soccer players: A prospective study. J. Athlet. Train. 2017, 52, 1048–1055. [Google Scholar] [CrossRef] [Green Version]
- Claiborne, T.L.; Armstrong, C.W.; Gandhi, V.; Pincivero, D.M. Relationship between hip and knee strength and knee valgus during a single leg squat. J. Appl. Biomech. 2006, 22, 41–50. [Google Scholar] [CrossRef] [Green Version]
- De Marche Baldon, R.; Lobato, D.F.M.; Carvalho, L.P.; Santiago, P.R.P.; Benze, B.G.; Serrão, F.V. Relationship between eccentric hip torque and lower-limb kinematics: Gender differences. J. Appl. Biomech. 2011, 27, 223–232. [Google Scholar] [CrossRef] [Green Version]
- Zadpoor, A.A.; Nikooyan, A.A. The effects of lower-extremity muscle fatigue on the vertical ground reaction force: A meta-analysis. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2012, 226, 579–588. [Google Scholar] [CrossRef]
- Bates, N.A.; Ford, K.R.; Myer, G.D.; Hewett, T.E. Impact differences in ground reaction force and center of mass between the first and second landing phases of a drop vertical jump and their implications for injury risk assessment. J. Biomech. 2013, 46, 1237–1241. [Google Scholar] [CrossRef] [Green Version]
- Sell, T.C.; Ferris, C.M.; Abt, J.P.; Tsai, Y.S.; Myers, J.B.; Fu, F.H.; Lephart, S.M. Predictors of proximal tibia anterior shear force during a vertical stop-jump. J. Orthop. Res. 2007, 25, 1589–1597. [Google Scholar] [CrossRef] [PubMed]
- Devita, P.; Skelly, W.A. Effect of landing stiffness on joint kinetics and energetics in the lower extremity. Med. Sci. Sports Exerc. 1992, 24, 108–115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zadpoor, A.A.; Nikooyan, A.A. The relationship between lower-extremity stress fractures and the ground reaction force: A systematic review. Clin. Biomech. 2011, 26, 23–28. [Google Scholar] [CrossRef]
- Koshino, Y.; Ishida, T.; Yamanaka, M.; Samukawa, M.; Kobayashi, T.; Tohyama, H. Toe-in landing increases the ankle inversion angle and moment during single-leg landing: Implications in the prevention of lateral ankle sprains. J. Sport Rehab. 2017, 26, 530–535. [Google Scholar] [CrossRef] [PubMed]
- Wright, I.C.; Neptune, R.R.; van den Bogert, A.J.; Nigg, B.M. The influence of foot positioning on ankle sprains. J. Biomech. 2000, 33, 513–519. [Google Scholar] [CrossRef] [Green Version]
- Robbins, S.; Waked, E.; Rappel, R. Ankle taping improves proprioception before and after exercise in young men. Br. J. Sports Med. 1995, 29, 242–247. [Google Scholar] [CrossRef] [Green Version]
- Herb, C.C.; Grossman, K.; Feger, M.A.; Donovan, L.; Hertel, J. Lower extremity biomechanics during a drop-vertical jump in participants with or without chronic ankle instability. J. Athlet. Train. 2018, 53, 364–371. [Google Scholar] [CrossRef]
- Ireland, M.L. Anterior cruciate ligament injury in female athletes: Epidemiology. J. Athlet. Train. 1999, 34, 150. [Google Scholar]
- Ireland, M.L. The female acl: Why is it more prone to injury? Orthop. Clin. 2002, 33, 637–651. [Google Scholar] [CrossRef] [Green Version]
- Shultz, S.J.; Schmitz, R.J. Effects of transverse and frontal plane knee laxity on hip and knee neuromechanics during drop landings. Am. J. Sports Med. 2009, 37, 1821–1830. [Google Scholar] [CrossRef] [Green Version]
- Everard, E.; Lyons, M.; Harrison, A.J. An examination of the relationship between the functional movement screen, landing error scoring system, and 3d kinematic data during a drop jump task. J. Strength Cond. Res. 2019, 35, 3012–3020. [Google Scholar] [CrossRef] [PubMed]
- Dai, B.; Herman, D.; Liu, H.; Garrett, W.E.; Yu, B. Prevention of acl injury, part I: Injury characteristics, risk factors, and loading mechanism. Res. Sports Med. 2012, 20, 180–197. [Google Scholar] [CrossRef]
- Self, B.P.; Paine, D. Ankle biomechanics during four landing techniques. Med. Sci. Sports Exerc. 2001, 33, 1338–1344. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.-N.; Bates, B.T.; Dufek, J.S. Contributions of lower extremity joints to energy dissipation during landings. Med. Sci. Sports Exerc. 2000, 32, 812–819. [Google Scholar] [CrossRef]
- Donelon, T.A.; Dos’Santos, T.; Pitchers, G.; Brown, M.; Jones, P.A. Biomechanical determinants of knee joint loads associated with increased anterior cruciate ligament loading during cutting: A systematic review and technical framework. Sports Med.-Open 2020, 6, 53. [Google Scholar] [CrossRef] [PubMed]
- Kipp, K.; McLean, S.G.; Palmieri-Smith, R.M. Patterns of hip flexion motion predict frontal and transverse plane knee torques during a single-leg land-and-cut maneuver. Clin. Biomech. 2011, 26, 504–508. [Google Scholar] [CrossRef] [Green Version]
- Norcross, M.F.; Lewek, M.D.; Padua, D.A.; Shultz, S.J.; Weinhold, P.S.; Blackburn, J.T. Lower extremity energy absorption and biomechanics during landing, part i: Sagittal-plane energy absorption analyses. J. Athlet. Train. 2013, 48, 748–756. [Google Scholar] [CrossRef] [Green Version]
- Leppänen, M.; Pasanen, K.; Krosshaug, T.; Kannus, P.; Vasankari, T.; Kujala, U.M.; Bahr, R.; Perttunen, J.; Parkkari, J. Sagittal plane hip, knee, and ankle biomechanics and the risk of anterior cruciate ligament injury: A prospective study. Orthop. J. Sports Med. 2017, 5, 2325967117745487. [Google Scholar] [CrossRef] [Green Version]
- Leppänen, M.; Pasanen, K.; Kujala, U.M.; Vasankari, T.; Kannus, P.; Äyrämö, S.; Krosshaug, T.; Bahr, R.; Avela, J.; Perttunen, J. Stiff landings are associated with increased acl injury risk in young female basketball and floorball players. Am. J. Sports Med. 2017, 45, 386–393. [Google Scholar] [CrossRef]
- Simpson, J.D.; Stewart, E.M.; Turner, A.J.; Macias, D.M.; Chander, H.; Knight, A.C. Lower limb joint kinetics during a side-cutting task in participants with or without chronic ankle instability. J. Athlet. Train. 2020, 55, 169–175. [Google Scholar] [CrossRef] [Green Version]
- Bisseling, R.W.; Hof, A.L.; Bredeweg, S.W.; Zwerver, J.; Mulder, T. Are the take-off and landing phase dynamics of the volleyball spike jump related to patellar tendinopathy? Br. J. Sports Med. 2008, 42, 483–489. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hadzic, V.; Sattler, T.; Topole, E.; Jarnovic, Z.; Burger, H.; Dervisevic, E. Risk factors for ankle sprain in volleyball players: A preliminary analysis. Isokinet. Exerc. Sci. 2009, 17, 155–160. [Google Scholar] [CrossRef]
- Bittencourt, N.F.N.; Meeuwisse, W.H.; Mendonça, L.D.; Nettel-Aguirre, A.; Ocarino, J.M.; Fonseca, S.T. Complex systems approach for sports injuries: Moving from risk factor identification to injury pattern recognition-narrative review and new concept. Br. J. Sports Med. 2016, 50, 1309–1314. [Google Scholar] [CrossRef] [Green Version]
- Edouard, P.; Ford, K.R. Great challenges toward sports injury prevention and rehabilitation. Front. Sports Act. Living 2020, 2, 80. [Google Scholar] [CrossRef]
- Pappas, E.; Nightingale, E.J.; Simic, M.; Ford, K.R.; Hewett, T.E.; Myer, G.D. Do exercises used in injury prevention programmes modify cutting task biomechanics? A systematic review with meta-analysis. Br. J. Sports Med. 2015, 49, 673–680. [Google Scholar] [CrossRef] [PubMed]
- Pollard, C.D.; Sigward, S.M.; Ota, S.; Langford, K.; Powers, C.M. The influence of in-season injury prevention training on lower-extremity kinematics during landing in female soccer players. Clin. J. Sport Med. 2006, 16, 223–227. [Google Scholar] [CrossRef]
- Myer, G.D.; Ford, K.R.; McLean, S.G.; Hewett, T.E. The effects of plyometric versus dynamic stabilization and balance training on lower extremity biomechanics. Am. J. Sports Med. 2006, 34, 445–455. [Google Scholar] [CrossRef]
- Mandelbaum, B.R.; Silvers, H.J.; Watanabe, D.S.; Knarr, J.F.; Thomas, S.D.; Griffin, L.Y.; Kirkendall, D.T.; Garrett, W., Jr. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am. J. Sports Med. 2005, 33, 1003–1010. [Google Scholar] [CrossRef]
- Hewett, T.E.; Lindenfeld, T.N.; Riccobene, J.V.; Noyes, F.R. The effect of neuromuscular training on the incidence of knee injury in female athletes. Am. J. Sports Med. 1999, 27, 699–706. [Google Scholar] [CrossRef]
- Webster, K.E.; Hewett, T.E. Meta-analysis of meta-analyses of anterior cruciate ligament injury reduction training programs. J. Orthop. Res. 2018, 36, 2696–2708. [Google Scholar] [CrossRef] [PubMed]
- Al Attar, W.S.A.; Alshehri, M.A. A meta-analysis of meta-analyses of the effectiveness of fifa injury prevention programs in soccer. Scand. J. Med. Sci. Sports 2019, 29, 1846–1855. [Google Scholar] [CrossRef] [PubMed]
- Lopes, T.J.A.; Simic, M.; Myer, G.D.; Ford, K.R.; Hewett, T.E.; Pappas, E. The effects of injury prevention programs on the biomechanics of landing tasks: A systematic review with meta-analysis. Am. J. Sports Med. 2018, 46, 1492–1499. [Google Scholar] [CrossRef] [PubMed]
- Faude, O.; Rössler, R.; Petushek, E.J.; Roth, R.; Zahner, L.; Donath, L. Neuromuscular adaptations to multimodal injury prevention programs in youth sports: A systematic review with meta-analysis of randomized controlled trials. Front. Physiol. 2017, 8, 791. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Owoeye, O.B.; VanderWey, M.J.; Pike, I. Reducing injuries in soccer (football): An umbrella review of best evidence across the epidemiological framework for prevention. Sports Med.-Open 2020, 6, 46. [Google Scholar] [CrossRef]
- Besier, T.F.; Lloyd, D.G.; Cochrane, J.L.; Ackland, T.R. External loading of the knee joint during running and cutting maneuvers. Med. Sci. Sports Exerc. 2001, 33, 1168–1175. [Google Scholar] [CrossRef]
- Sigward, S.M.; Cesar, G.M.; Havens, K.L. Predictors of frontal plane knee moments during side-step cutting to 45 and 110 degrees in men and women: Implications for anterior cruciate ligament injury. Clin. J. Sport Med. 2015, 25, 529–534. [Google Scholar] [CrossRef] [Green Version]
- Dai, B.; Garrett, W.E.; Gross, M.T.; Padua, D.A.; Queen, R.M.; Yu, B. The effect of performance demands on lower extremity biomechanics during landing and cutting tasks. J. Sport Health Sci. 2019, 8, 228–234. [Google Scholar] [CrossRef] [Green Version]
- Meeuwisse, W.H.; Tyreman, H.; Hagel, B.; Emery, C. A dynamic model of etiology in sport injury: The recursive nature of risk and causation. Clin. J. Sport Med. 2007, 17, 215–219. [Google Scholar] [CrossRef]
- Emery, C.A.; Meeuwisse, W.H.; Hartmann, S.E. Evaluation of risk factors for injury in adolescent soccer: Implementation and validation of an injury surveillance system. Am. J. Sports Med. 2005, 33, 1882–1891. [Google Scholar] [CrossRef]
- Read, P.J.; Oliver, J.L.; De Ste Croix, M.; Myer, G.D.; Lloyd, R.S. A prospective investigation to evaluate risk factors for lower extremity injury risk in male youth soccer players. Scand. J. Med. Sci. Sports 2018, 28, 1244–1251. [Google Scholar] [CrossRef]
- Söderkvist, I.; Wedin, P.-Å. Determining the movements of the skeleton using well-configured markers. J. Biomech. 1993, 26, 1473–1477. [Google Scholar] [CrossRef]
- Lucke-Wold, B.; Nolan, R.; Nwafor, D.; Nguyen, L.; Cheyuo, C.; Turner, R.; Rosen, C.; Marsh, R. Post-traumatic stress disorder delineating the progression and underlying mechanisms following blast traumatic brain injury. J. Neurosci. Neuropharmacol. 2018, 4, 118. [Google Scholar] [PubMed]

| Joint Kinematics at IC (°) and PEAK (°) | All Players (n = 56) | Injured Players (n = 22) | Non-Injured Players (n = 34) |
|---|---|---|---|
| Ankle | |||
| Plantarflexion(+)/Dorsiflexion(−) IC | 24.2 ± 5.3 | 24.2 ± 5.1 | 24.1 ± 5.5 |
| Plantarflexion(+)/Dorsiflexion(−) PEAK | 26.1 ± 6.1 | 26.9 ± 6.4 | 25.6 ± 6.0 |
| Eversion(+)/Inversion(−) IC | −8.2 ± 3.8 | −8.2 ± 4.2 | −8.3 ± 3.5 |
| Eversion(+)/Inversion(−) PEAK | −9.4 ± 3.9 | −9.6 ± 4.2 | −9.2 ± 3.7 |
| External Rotation(+)/Internal Rotation(−) IC | −1.8 ± 3.9 | −1.5 ± 4.0 | −2.0 ± 3.9 |
| External Rotation(+)/Internal Rotation(−) PEAK | −3.2 ± 4.5 | −2.9 ± 4.6 | −3.4 ± 4.4 |
| Knee | |||
| Flexion(+)/Extension(−) IC | 15.1 ± 5.0 | 15.0 ± 4.8 | 15.1 ± 5.2 |
| Flexion(+)/Extension(−) PEAK | 52.3 ± 4.6 | 53.0 ± 4.3 | 51.8 ± 4.8 |
| Adduction(+)/Abduction(−) IC | 2.0 ± 2.9 | 1.6 ± 3.0 | 2.2 ± 2.9 |
| Adduction(+)/Abduction(− PEAK | −0.9 ± 4.0 | −2.0 ± 4.6 | −0.1 ± 3.4 |
| External Rotation(+)/Internal Rotation(−) IC | 2.0 ± 4.0 | 1.5 ± 4.2 | 2.4 ± 3.8 |
| External Rotation(+)/Internal Rotation(−) PEAK | −10.0 ± 4.4 | −9.4 ± 4.6 | −10.4 ± 4.3 |
| Hip | |||
| Flexion(+)/Extension(−) IC | 30.0 ± 6.9 | 30.1 ± 7.5 | 30.0 ± 6.6 |
| Flexion(+)/Extension(−) PEAK | 44.4 ± 8.6 | 44.4 ± 9.8 | 44.4 ± 7.9 |
| Adduction(+)/Abduction(−) IC | −9.6 ± 2.8 | −10.0 ± 2.7 | −9.4 ± 3.0 |
| Adduction(+)/Abduction(−) PEAK | 0.3 ± 3.3 | 0.4 ± 3.5 | 0.2 ± 3.2 |
| External Rotation(+)/Internal Rotation(−) IC | 4.8 ± 4.5 | 4.8 ± 5.6 | 4.8 ± 3.8 |
| External Rotation(+)/Internal Rotation(−) PEAK | −0.6 ± 4.2 | −1.1 ± 4.9 | −0.2 ± 3.7 |
| Joint Kinematics at IC (°) and PEAK (°) | All Players (n = 56) | Injured Players (n = 22) | Non-Injured Players (n = 34) |
|---|---|---|---|
| Ankle | |||
| Plantarflexion(+)/Dorsiflexion(−) IC | −2.9 ± 9.2 | −1.7 ± 11.1 | −3.8 ± 7.7 |
| Plantarflexion(+)/Dorsiflexion(−) PEAK | 3.3 ± 6.5 | 4.7 ± 6.9 | 2.4 ± 6.1 |
| Eversion(+)/Inversion(−) IC | −12.8 ± 5.8 | −13.0 ± 6.0 | −12.7 ± 5.7 |
| Eversion(+)/Inversion(−) PEAK | −22.0 ± 4.9 | −22.2 ± 5.3 | −21.9 ± 4.7 |
| External Rotation(+)/Internal Rotation(−) IC | 3.1 ± 5.1 | 3.1 ± 5.9 | 3.1 ± 4.5 |
| External Rotation(+)/Internal Rotation(−) PEAK | −0.2 ± 5.2 | 0.9 ± 5.4 | −1.0 ± 5.0 |
| Knee | |||
| Flexion(+)/Extension(−) IC | 42.8 ± 12.1 | 38.6 ± 12.3 | 45.6 ± 11.2 |
| Flexion(+)/Extension(−) PEAK | 56.6 ± 5.4 | 55.5 ± 6.0 | 57.4 ± 4.8 |
| Adduction(+)/Abduction(−) IC | −1.1 ± 4.3 | −1.1 ± 4.0 | −1.1 ± 4.6 |
| Adduction(+)/Abduction(−) PEAK | −6.0 ± 4.7 | −6.2 ± 4.7 | −5.9 ± 4.8 |
| External Rotation(+)/Internal Rotation(−) IC | −7.1 ± 5.8 | −6.1 ± 6.4 | −7.8 ± 5.3 |
| External Rotation(+)/Internal Rotation(−) PEAK | −12.6 ± 5.4 | −11.5 ± 5.8 | −13.4 ± 5.0 |
| Hip | |||
| Flexion(+)/Extension(−) IC | 66.7 ± 8.9 | 64.0 ± 10.7 | 68.5 ± 7.0 |
| Flexion(+)/Extension(−) PEAK | 68.2 ± 8.6 | 65.6 ± 10.1 | 70.0 ± 7.0 |
| Adduction(+)/Abduction(−) IC | −7.1 ± 4.4 | −7.1 ± 4.5 | −7.2 ± 4.3 |
| Adduction(+)/Abduction(−) PEAK | −3.6 ± 4.6 | −4.0 ± 4.7 | −3.3 ± 4.5 |
| External Rotation(+)/Internal Rotation(−) IC | −2.6 ± 4.7 | −2.5 ± 5.9 | −2.7 ± 3.7 |
| External Rotation(+)/Internal Rotation(−) PEAK | 6.1 ± 5.4 | 6.3 ± 7.1 | 6.0 ± 4.1 |
| PEAK Joint Moments (Nm/kg) | All Players (n = 56) | Injured Players (n = 22) | Non-Injured Players (n = 34) |
|---|---|---|---|
| Ankle | |||
| Plantarflexion(+)/Dorsiflexion(−) SLDL | −0.1 ± 0.0 | −0.1 ± 0.0 | −0.1 ± 0.0 |
| Plantarflexion(+)/Dorsiflexion(−) USSC | 0.1 ± 0.2 | 0.2 ± 0.2 | 0.1 ± 0.2 |
| Eversion(+)/Inversion(−) SLDL | −0.4 ± 0.1 | −0.4 ± 0.1 | −0.4 ± 0.1 |
| Eversion(+)/Inversion(−) USSC | −0.3 ± 0.1 | −0.3 ± 0.1 | −0.3 ± 0.1 |
| External Rotation(+)/Internal Rotation(−) SLDL | −0.4 ± 0.1 | −0.4 ± 0.1 | −0.4 ± 0.1 |
| External Rotation(+)/Internal Rotation(−) USSC | −0.1 ± 0.1 | −0.1 ± 0.1 | −0.1 ± 0.1 |
| Knee | |||
| Flexion(+)/Extension(−) SLDL | 2.5 ± 0.4 | 2.5 ± 0.4 | 2.5 ± 0.4 |
| Flexion(+)/Extension(−) USSC | 2.2 ± 0.5 | 2.3 ± 0.5 | 2.2 ± 0.5 |
| Adduction(+)/Abduction(−) SLDL | −0.7 ± 0.3 | −0.7 ± 0.3 | −0.7 ± 0.3 |
| Adduction(+)/Abduction(−) USSC | −0.9 ± 0.2 | −0.8 ± 0.2 | −0.9 ± 0.2 |
| External Rotation(+)/Internal Rotation(−) SLDL | −0.1 ± 0.1 | −0.1 ± 0.1 | −0.1 ± 0.0 |
| External Rotation(+)/Internal Rotation(−) USSC | −0.3 ± 0.2 | −0.3 ± 0.3 | −0.3 ± 0.2 |
| Hip | |||
| Flexion(+)/Extension(−) SLDL | 3.6 ± 0.6 | 3.7 ± 0.6 | 3.6 ± 0.5 |
| Flexion(+)/Extension(−) USSC | 3.7 ± 0.7 | 3.6 ± 0.7 | 3.8 ± 0.6 |
| Adduction(+)/Abduction(−) SLDL | 1.0 ± 0.2 | 1.0 ± 0.2 | 1.0 ± 0.2 |
| Adduction(+)/Abduction(−) USSC | 0.6 ± 0.3 | 0.6 ± 0.3 | 0.6 ± 0.3 |
| External Rotation(+)/Internal Rotation(−) SLDL | −0.6 ± 0.2 | −0.7 ± 0.3 | −0.6 ± 0.1 |
| External Rotation(+)/Internal Rotation(−) USSC | −0.6 ± 0.2 | −0.7 ± 0.3 | −0.6 ± 0.1 |
| PEAK vGRF (N/kg) | All Players (n = 56) | Injured Players (n = 22) | Non-Injured Players (n = 34) |
| vGRF SLDL | 38.4 ± 3.9 | 38.1 ± 3.2 | 38.5 ± 4.3 |
| vGRF USSC | 20.9 ± 2.5 | 20.8 ± 1.8 | 20.9 ± 2.8 |
| Decision Tree Classification SLDL | |||
|---|---|---|---|
| Injured | Non-Injured | ||
| Injury Status | Injured | 19 True positive (TP) | 4 False positive (FP) |
| Non-Injured | 8 False negative (FN) | 26 True negative (TN) | |
| Decision Tree Classification USSC | |||
|---|---|---|---|
| Injured | Non-Injured | ||
| Injury Status | Injured | 17 True positive (TP) | 6 False positive (FP) |
| Non-Injured | 8 False negative (FN) | 26 True negative (TN) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kolodziej, M.; Willwacher, S.; Nolte, K.; Schmidt, M.; Jaitner, T. Biomechanical Risk Factors of Injury-Related Single-Leg Movements in Male Elite Youth Soccer Players. Biomechanics 2022, 2, 281-300. https://doi.org/10.3390/biomechanics2020022
Kolodziej M, Willwacher S, Nolte K, Schmidt M, Jaitner T. Biomechanical Risk Factors of Injury-Related Single-Leg Movements in Male Elite Youth Soccer Players. Biomechanics. 2022; 2(2):281-300. https://doi.org/10.3390/biomechanics2020022
Chicago/Turabian StyleKolodziej, Mathias, Steffen Willwacher, Kevin Nolte, Marcus Schmidt, and Thomas Jaitner. 2022. "Biomechanical Risk Factors of Injury-Related Single-Leg Movements in Male Elite Youth Soccer Players" Biomechanics 2, no. 2: 281-300. https://doi.org/10.3390/biomechanics2020022






