1. Introduction
In March of 2020 the World Health Organization (WHO) categorized the COVID-19 outbreak as a global health pandemic [
1]. Following this designation, the Federal and Provincial governments of Canada implemented various measures to contain the spread of the disease including border closure, limiting travel, limits on gatherings, lockdowns, mask mandates, and immunization [
2]. Among these measures was closures of gyms and a pause on leisure and recreational programs [
3,
4] that may have limited physical activity (PA) and encouraged sedentary behaviour [
5].
Evidence from Canada and other developed countries has shown that lockdowns throughout the pandemic have had a negative impact on PA participation as well as emotional, psychological, and social well-being [
6,
7]. Data from over 40,000 able-bodied individuals found that low levels of moderate to vigorous intensity PA (MVPA) during the pandemic were associated with higher levels of depression and anxiety [
8]. To make matters worse, low levels of PA have been shown to be associated with a higher risk of severe COVID-19 outcomes [
9].
A 2020 report by the Global Disability Rights Monitor raised the alarm about the impact of the COVID-19 pandemic on people with disabilities worldwide through the testimonies of more than 2100 respondents from 134 countries [
10]. The report concluded that nations have failed to sufficiently meet the needs of people with disabilities throughout the pandemic and made eleven recommendations on how to be more inclusive including improved access to healthcare and the funding of community-based projects. Interestingly, within these recommendations, there was no mention of the need for access to opportunities for participation in PA or recreational programs.
The pandemic, associated lockdowns, and lack of access to gym and recreation programs likely has an even greater negative impact on those with disabilities. First, regular PA is essential to the health of people with disabilities [
11], yet over 200 intraindividual, interindividual, institutional, policy, and community-level factors were linked to PA participation among people with disabilities before the COVID-19 outbreak [
12]. These factors include extensive barriers that contribute to people with disabilities being 16–64% less likely than the general population [
11] to meet the WHO’s PA guidelines of at least 150 min/week of moderate intensity PA, 75 min/week of vigorous intensity PA, or an equivalent combination of moderate and vigorous PA [
13]. Given the extensive barriers to PA participation [
12], individuals with disabilities likely have a greater need for additional support to participate in PA such as safe environments and adaptive equipment. Recreational facilities may provide one of the only settings in which such support is provided. Second, individuals with disabilities experience an almost five-fold greater prevalence of mental distress than able-bodied individuals [
14] and experiencing physical disability is significantly associated with a greater likelihood of experiencing symptoms of depression and anxiety [
15]. Cross-sectional studies conducted during the first-wave of the pandemic generally reported a negative impact of the pandemic on self-reported PA and well-being in people with disabilities [
16]. We are unaware of any longitudinal studies that have examined perceived impact of the pandemic on PA, changes in the PA, physical and mental health of people with disabilities over the course of the pandemic.
Given the association between physical activity, physical health, and mental health in individuals with disabilities pre-pandemic [
11], the purpose of the present study was to describe self-reported PA participation and physical and mental health among Canadian adults who identify as having a disability over two separate timeframes (18 June 2020 to 18 December 2020 and 19 December 2020 to 18 September 2021 (referred to as iterations 1 and 2, respectively) during the pandemic. In addition, we intended to test for changes in PA, physical health, and mental health over these timeframes. A second purpose was to describe the needs of Canadians with disabilities during the pandemic and whether they were being met or unmet.
We hypothesized that in a sample of Canadians with disabilities, (1) the majority of respondents would report that the pandemic had a negative impact on their PA levels as it has among people with disabilities in other countries, (2) physical health would be correlated with mental health at both timeframes as would changes in physical and mental health between timeframes, and (3) more respondents would report access to recreation facilities as an unmet need during, versus before, the pandemic.
2. Materials and Methods
2.1. Overview
The COVID-19 Disability Survey was an initiative to record the experiences, concerns, and needs of Canadians with disabilities during the COVID-19 outbreak and recovery period. The survey was developed in partnership with representatives of Abilities Centre—a not-for-profit organization based in Whitby, ON that provides inclusive programs for people with disabilities—and researchers from the University of British Columbia Okanagan and Canadian Disability Participation Project (F.H., J.Ú.C., K.M.G.)—an alliance of university, public, private and government sector partners working to enhance community participation among people with disabilities [
17].
Reports on iteration 1 and iteration 2 are available on the Abilities Centre website at
https://abilitiescentre.org/disabilitysurvey (accessed on 4 October 2021) [
18] and on the Open Science Framework at
https://osf.io/z4gr2 (accessed on 4 October 2021) [
19]. These reports briefly address the impact of the pandemic on PA habits and report on the complete set of data collected including the worries, needs, and well-being of Canadians with disabilities during each survey’s timeframe. The present paper focuses only on self-reported PA, physical and mental health, and perceived needs of adults with disabilities during the pandemic.
2.2. Survey Development
The first draft of the survey was developed by five team members (J.U.C., F.H., K.M.G., P.D.S., T.J.K.) in consultation with representatives from three national organizations (Rick Hansen Foundation, Canadian Labour Congress, and Canadian Autism Spectrum Disorder Alliance) and a coalition of British Columbia provincial disability organizations. The survey was originally written in English, and translated into French, plain language, and American Sign Language.
Three iterations of the survey were developed, administered, and managed online using Qualtrics software (Provo, UT, USA). First, a pilot iteration was developed that collected responses only from ON residents between 5 May 2020 and 22 June 2020. Based on feedback from the pilot iteration, and to adapt to the developing pandemic and the responses of the Federal and Provincial Governments, iteration 1 of the survey collected responses from people with disabilities from across Canada between 18 June 2020 and 18 December 2020. Iteration 2 of the survey collected responses between 19 December 2020 and 18 September 2021. Timeframes were based on events happening across Canada that our partners believed could influence the needs and experiences of Canadians living with disabilities during the pandemic such as the vaccine rollout (end iteration 1) and lifting of the majority of pandemic restrictions (end iteration 2). Further information about the survey methodology can be found on the Open Science Framework website at
https://osf.io/z4gr2 (accessed on 4 October 2021) [
19]. Ethical approval was provided by the University of British Columbia’s Behavioral Research Ethics Board (H20-01203).
2.3. Participants
Participants were recruited through social media posts (i.e., Twitter) from the above-mentioned partner organizations. The survey was open to all Canadian residents who identified as having a disability as well as parents, caregivers, and family members of people with disabilities. For the purpose of this study, only responses from adults who identified as having a disability are included in the analyses.
To be included in the main analyses, participants had to indicate their impairment type/s in response to the question “How would you describe your disability?” Participants were given response options consistent with how impairments are reported by Statistics Canada [
20]. An identification code based on each respondent’s (1) year of birth, (2) first two letters of mother’s maiden name, (3) gender identity, and (4) province of residence, was used to identify individuals who responded to both iterations. These respondents’ data were used in sub-analyses of the longitudinal impact of the pandemic.
2.4. Procedures
All questions were administered online using Qualtrics software (Provo, UT, USA). Time to complete the survey—including sections not presented in the present study—was 20 ± 18 and 20 ± 16 min for iteration 1 and 2, respectively. Among those who responded to both iterations, the average time between completing iterations was 94 ± 36 days.
2.4.1. Perceived Impact of the Pandemic
Respondents were asked to report whether there had been ‘no change’, a ‘negative change’, or a ‘positive change’ in various health habits, including ‘exercise/physical activity’, since the start of the pandemic. Regarding mental health, respondents were asked: ‘has the COVID-19 pandemic negatively impacted your mental health?’ Response options were: ‘not at all’, ‘very little’, ‘to some extent’, ‘to a great extent’, or ‘completely’.
2.4.2. Self-Reported Physical Activity Participation
The International Physical Activity Questionnaire—Short Form (IPAQ) [
21] was administered to measure the frequency, intensity, and time spent on PA over the seven days prior to completing the survey. The questionnaire was adapted by removing questions regarding time spent sitting, as these questions may be confusing/irrelevant to people who use wheelchairs. The IPAQ is a valid and reliable questionnaire for assessing self-reported PA participation in able-bodied individuals [
21] and has been used previously to assess PA among people with mobility impairments [
22]. The adapted 6-item IPAQ asked respondents to indicate on how many days they engaged in vigorous PA, moderate PA, and walking (or ‘wheeling’ for wheelchair users) and, if they indicated their participation in one or more of these activities, how many hours and minutes they spent engaged each day on average. To assist respondents with appropriately reporting/classifying the intensity of their activity, descriptions of feelings associated with vigorous intensity PA (‘make you feel like you are working really hard, almost at your maximum’) and moderate intensity PA (‘make you feel like you are working somewhat hard, but you can keep doing them for a while without getting tired’) were provided as well as examples of each. Weekly minutes of each PA category was calculated as the number of days engaged in each PA category multiplied by the average time spent on each of those days.
As the WHO guidelines for PA in people with disability indicate a minimum of 150 min PA/week of at least moderate intensity we calculated the sum of moderate and vigorous PA and report the total as MVPA. Respondents were categorized as those who engaged in no weekly MVPA (i.e., 0 min/week), those who completed 1–149 min/week, and those who achieved the WHO’s recommendations for people with disabilities of 150 min/week MVPA [
23,
24]. Weekly time engaged in walking/wheeling is reported using these same categories (i.e., none, 1–149 min/week, >150 min/week). To be consistent with both the IPAQ and the WHO guidelines, which define slow walking as light intensity (i.e., not of adequate intensity to meet guidelines), we did not include minutes spent walking in our calculation of MVPA [
23].
2.4.3. Physical and Mental Health
The Patient-Reported Outcomes Measurement Information System (PROMIS) Global-10 questionnaire assessed respondents’ perceptions of their own physical and mental health [
25]. The PROMIS Global-10 is not disease or disability specific as it intends to reflect an individual’s general assessment of their own health and has demonstrated construct validity in the able-bodied population [
25]. Four items are used to assess physical health—three 5-point items and an 11-point pain rating scale that is then converted to a 5-point scale. Four 5-point items are used to assess mental health. Raw scores for both physical and mental health range from 4–20. The raw scores were converted to a T-score where a score of 50 represents the mean value for the general population and the standard deviation around that mean is equal to 10 [
26]. These values were based on norms for the general population of the United States as there are no norms for the PROMIS scale based on the Canadian population. At iteration 1, Cronbach’s alpha for the physical and mental health components of the test were 0.70 and 0.86, respectively. At iteration 2, these values were 0.74 and 0.85 for physical and mental health.
2.5. Needs Assessment
Respondents were asked to indicate whether or not they had 12 specified ‘needs’, including access to leisure and recreation programs. Needs were pre-identified based on a list adapted from a needs survey of Canadians with spinal cord injury [
27] and included additional needs following discussions with community organizations. Respondents who identified that they had a specific need were then asked to rate the degree to which these needs were being met at the time of survey completion as well as before the pandemic (iteration 1 only). Meeting of needs were rated on a 5-point scale with the response options of ‘not at all’, ‘very little’, ‘somewhat, ‘very much’, and ‘completely’. Respondents were then asked to identify whether they had received support for this need during the pandemic.
2.6. Statistical Analyses
Comparisons between the percentages of participants giving each response for the demographics, physical and mental health, self-report PA participation, and needs measures during iteration 1 and 2 were performed using Pearson’s chi-square tests, except age which was assessed by independent samples t-tests.
Changes in PA and health over time were tested using paired samples t-tests if the data were normally distributed or Wilcoxon matched-pairs signed rank test if not normally distributed (determined by Shapiro–Wilk test). To assess correlations between changes in physical and mental health, residualized change scores were computed to measure changes from iteration 1 to 2 (controlling for baseline scores) and then Pearson’s correlation coefficients were computed using the residualized change scores. Analyses were conducted using SPSS, version 27 (IBM Corp., Armonk, NY, USA) and GraphPad Prism, version 9.1.0 (GraphPad Software, Inc., LaJolla, CA, USA). Data are presented as the mean ± SD; p < 0.05 was considered statistically significant.
3. Results
3.1. Participants
A total of 1241 responses to iteration 1 and 1140 responses to iteration 2 were received. Following removal of incomplete responses, responses from caregivers of children with disabilities, and duplicate responses, 599 (iteration 1) and 528 (iteration 2) unique complete responses were included in analyses. Demographic information for respondents to each iteration and for those who responded to both iterations regarding respondents’ age, gender identity, impairment/s, ethnicity and household income is provided in
Table 1. Regarding respondents to both iterations, these respondents were older (50 ± 13) than those who responded only to iteration 1 (48 ± 14,
p = 0.023) or iteration 2 (45 ± 15,
p < 0.001). Additionally, a greater percentage of respondents to both iterations identified as Caucasian and fewer identified as Hispanic, South Asian, or Black (all
p < 0.05). Given the variability in sample sizes across impairment groups, demographics are reported for the entire sample rather than as a function of impairment group.
3.2. Perceived Impact of the Pandemic
At iteration 1, 64% indicated that the pandemic negatively impacted their PA habits, compared to 59% at iteration 2. When asked whether the pandemic had negatively impacted their mental health, 83% of iteration 1 respondents and 78% of iteration 2 respondents indicated ‘to some extent’, ‘to a great extent’, or ‘completely’.
3.3. Self-Reported Physical Activity Participation during the Pandemic
The distribution of participants who reported 0, 1–149, or 150+ min/week MVPA in the previous seven days was significantly different for iteration 1 and 2 (x2[2, 882] = 25.08, p < 0.001). For iteration 1 and 2, respectively, 59% and 44% of respondents reported no MVPA in the week prior to completing the survey. Only 19% of iteration 1 respondents compared to 32% of iteration 2 respondents reported meeting the WHO’s PA recommendations. While most respondents indicated that they engaged in some walking/wheeling each week, 30% of iteration 1 and 29% of iteration 2 respondents did not.
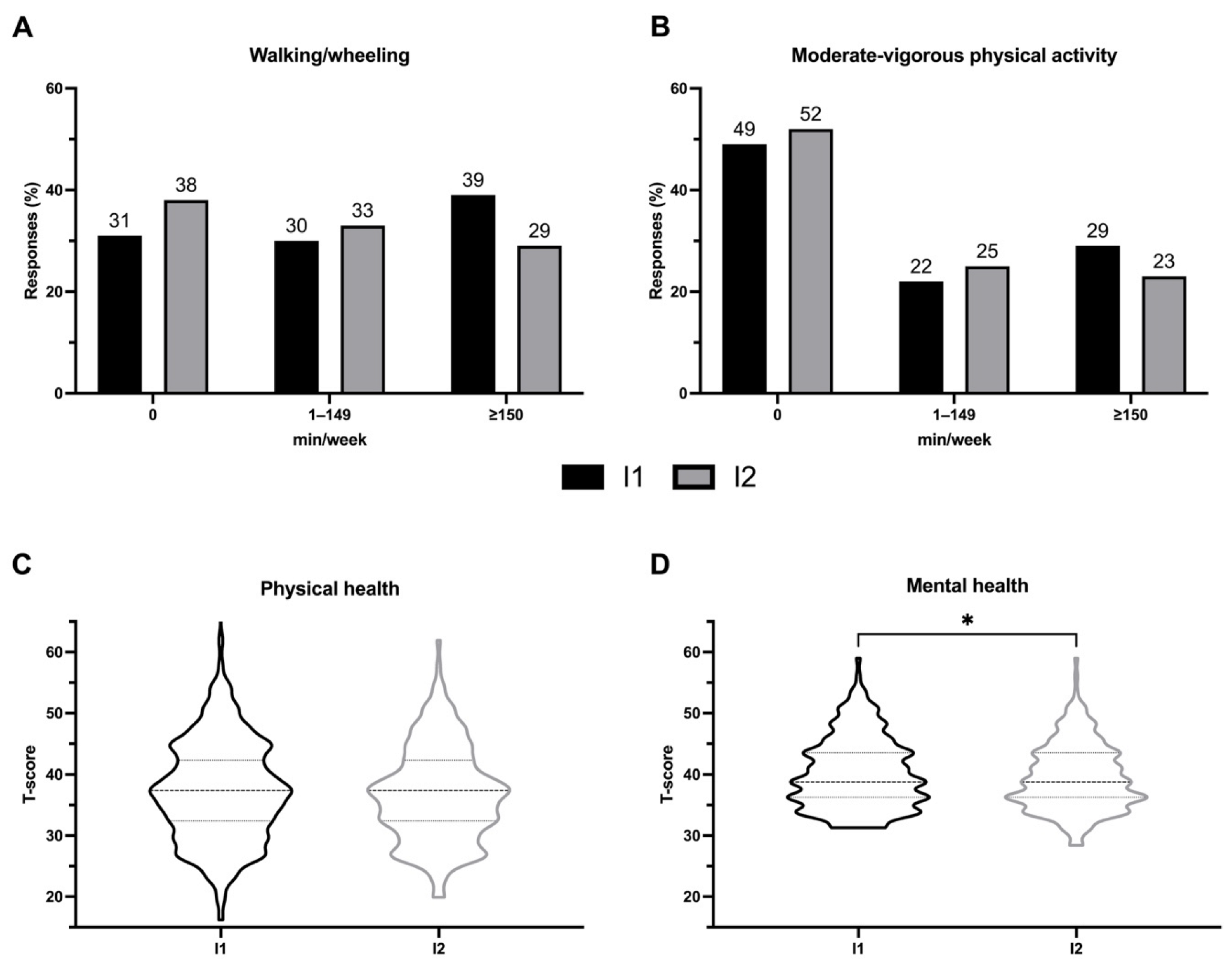
Among the cohort of respondents who completed both iterations there was no significant difference in self-reported walking/wheeling (246 ± 478 vs. 211 ± 428 min/week,
p > 0.05) or self-reported MVPA (194 ± 453 vs. 172 ± 464 min/week,
p > 0.05) between iterations. There was no change over time in the proportion of respondents who reported no weekly walking/wheeling, some walking/wheeling, or who achieved ≥150 min/week walking/wheeling (see
Figure 1A). Likewise, there was no change over time in the percentage of respondents doing no MVPA, some MVPA, or the recommended ≥150 min/week MVPA (see
Figure 1B).
3.4. Physical and Mental Health and Correlations with Self-Reported Physical Activity
At iteration 1 and iteration 2, over 90% of respondents reported their PROMIS physical health score to be worse than the average able-bodied adult (i.e., T-score < 50). More iteration 2 than iteration 1 respondents reported a physical health T-score of <40 (64% vs. 44%, (x2[3, 1037] = 8.132, p < 0.001). Fifty-two percent of iteration 1 and 91% of iteration 2 respondents reported their mental health to be worse than the average able-bodied adult.
Among those who responded to both surveys, physical health did not change between iteration 1 and 2 (37.4 ± 8.4 vs. 36.7 ± 7.8,
p > 0.05, see
Figure 1C), however mental health was significantly worse during iteration 2 (40.2 ± 5.8 vs. 39.5 ± 5.5,
p = 0.028, see
Figure 1D).
PROMIS scores for physical and mental health had a significant, large positive correlation [
28] during each timeframe (iteration 1: r = 0.51,
p < 0.001; iteration 2: r = 0.56,
p < 0.001). Among those who completed both iterations, changes in physical and mental health from the first to second iteration shared a small positive, but significant, correlation (r = 0.17,
p = 0.014).
Among respondents to iteration 1, MVPA had a small, negative correlation with both physical (r = −0.19, p < 0.001) and mental health (r = −0.12, p = 0.011). Among respondents to iteration 2, MVPA had small-to-medium sized positive correlations with both physical (r = 0.27, p < 0.001) and mental health (r = 0.24, p < 0.001).
3.5. Unmet Needs before and during the Pandemic
Of all needs assessed, access to leisure and recreation programs was the most frequently identified unmet need during the pandemic and had the greatest increase in the number of respondents with this unmet need from before the pandemic to iteration 1 (see
Table 2). Thirty percent of respondents to iteration 1 indicated that, before the pandemic, access to leisure and recreation programs was an unmet need. More respondents reported this to be an unmet need during the timeframes covered by iteration 1 (76%;
x2 = [1, 769]160.4,
p < 0.001), and iteration 2 (69%;
x2 = [1, 882]110.1,
p < 0.001). Only 27% of respondents reported receiving support for this need during the timeframe covered by iteration 1, and 24% at iteration 2—fewer than the percentage of respondents receiving support for any other need at each timeframe.
4. Discussion
The COVID-19 Disability Survey was undertaken to assess the experiences, concerns and needs of Canadians with disabilities during the pandemic. The survey incorporated a validated measure of self-reported PA and has generated the largest sample of PA data collected from Canadian adults with disabilities since 2001 [
29]. This survey, conducted in research partnership, is an important examination of the pandemic experiences of this population as it is (a) the first to report on PA participation among Canadians with disabilities using a validated self-report measure, and (b) the first, worldwide, to report longitudinal PA data in people with disabilities during the pandemic.
As hypothesised, the majority of respondents perceived that the pandemic had a negative impact on their PA habits. Similarly, approximately four in five respondents perceived the pandemic to have had a negative impact on their mental health—for context, this is higher than the proportion of Canadians with disabilities reporting a negative impact on mental health in a cross-sectional survey conducted by Statistics Canada earlier in the pandemic [
30]. When we assessed physical and mental health we found that, in agreement with our hypothesis, physical and mental health had a large-sized correlation among respondents during both iteration timeframes. Changes in physical and mental health from iteration 1 to 2 also correlated, albeit this was a small positive correlation. While these data do not imply causality, we suggest that improving physical health among people with disabilities—both during and following the pandemic—may also facilitate improvements in mental health. Alternatively, improvements in mental health may make it easier for people to take steps toward improving their physical health.
4.1. Self-Reported Physical Activity Participation
The most recent population-level data on PA participation among Canadians with disabilities were collected in 2001 [
29]. As such, we have no recent non-pandemic baseline with which we can compare data from the present survey. The 2001 data, from the Participation and Activity Limitations Survey, suggested reasonable PA participation among Canadians with disabilities. However, the survey did not use a valid measure of PA participation and the survey questions make it impossible to determine whether respondents achieved the PA intensities recommended by the WHO [
23]. These pandemic data are now the best available data on self-reported PA in Canadians with disabilities.
Our data highlight the low PA participation by Canadians with disabilities wherein as few as 19% of respondents reported achieving the WHO’s recommendations for MVPA. Equally as striking is that as many as 59% did no MVPA whatsoever. Given that PA participation was unchanged among respondents from the first iteration to the second, barriers to PA that were present in June–December 2020 may still have been in place December 2020–July 2021.
It is undeniable that Canadians with disabilities face multifarious barriers to PA participation [
12]. While creating additional barriers (e.g., increase in the number of respondents indicating needs for recreation programs not being met), the pandemic has highlighted pre- existing PA barriers and inequities. For instance, there are examples of successful interventions that were used to support PA participation among able-bodied Canadians during lockdown phases of the pandemic, such as the delivery of app-based home workouts [
31]. However, for Canadians with disabilities, pre-existing barriers to PA participation—such as a lack of accessible equipment or the need for another person to provide physical support during a workout [
12]—may have been exacerbated by pandemic restrictions that could not be overcome through shifts to online programming. Efforts must be devoted to developing strategies and policies to remove PA barriers for all Canadians with disabilities to support PA participation regardless of pandemic restrictions. Similarly, efforts should be made to educate individuals with disabilities and healthcare providers on opportunities for PA in the face of pandemic restrictions. Such efforts would align with the United Nations’ Sustainable Development Goal to ensure health and well-being for all [
32].
4.2. Needs Assessment
Assessment of the needs of Canadians with disabilities supports our hypothesis that access to recreation facilities would be a greater unmet need during versus before the pandemic. In fact, the need for access to recreation had the greatest absolute increase from before to during the pandemic of all needs that were assessed. When considered together with the low PA participation rates, these data underscore the long-standing PA barriers experienced by Canadians with disabilities that have been highlighted by the pandemic.
Interestingly, access to recreation facilities remained the greatest unmet need during iteration 2 when restrictions around access to such facilities were less. We believe that this demonstrates that, simply because facilities were opening, this did not necessarily mean that facilities are accessible to all Canadians with disabilities who have been clear in expressing their unmet need for PA and recreation programs during the pandemic. Greater effort is needed to ensure the protection of the rights of people with disabilities to participate in PA on an equal basis with others now and beyond the pandemic [
33].
4.3. Impact
Our research highlights a unique research partnership wherein real-time data was collected and disseminated in an inclusive and accessible manner to help ensure that the COVID-19 response strategies of communities and governments met the needs of people of all abilities. Findings from each iteration have been disseminated via press releases, government presentations, four open-access reports, and social media posts.
Most notably, findings from iteration 1 were presented to the Ontario Government’s Ministry of Seniors and Accessibility and used to support policy change regarding access to PA for Ontarians with disabilities [
34]. This change, an amendment to the Reopening Ontario Act, 2020 [
35], allowed for recreation facilities to re-open that supported physical therapy for people with disabilities. People with disabilities were able to visit these facilities in order to exercise, with a written prescription from a qualified regulated health professional and if access to physical therapy was not available elsewhere.
4.4. Strengths and Limitations
Strengths of the present study include the use of a valid measure of self-reported PA participation—albeit for able-bodied and select disability populations, the use of a longitudinal study design, the ability to compare two jurisdictions with differing policy-level responses to the pandemic, and the availability of the survey in English, French, plain language and American Sign Language. The research partnership between University-based researchers and Abilities Centre was a particular strength as it helped with recruitment and dissemination of interim findings as well as with access to government organizations that ultimately allowed these findings to influence policy change.
The heterogeneity of impairments reported by respondents can be seen as both a strength—as it provides a more representative sample of the disability population that is relevant to policy makers—and a limitation—in that we are unable to make conclusions regarding the impact of the pandemic on specific disability populations. By including participants with a diverse range of impairments in our analyses we note that caution should be taken not to equate the experience of each individual’s impairments. Similarly, it should not be assumed that PA participation among all people with disabilities, regardless of impairment, have been equally affected by the lockdown. Given differences in impairments and ethnicity of respondents to the two iterations, data from respondents who completed both iterations should be prioritized for any comparison of findings across iteration timeframes.
We also acknowledge that the survey sample may not be a representative sample of all Canadians with disabilities as recruitment was largely done through social media and word of mouth. However, this sampling method is not different than previous ‘crowd-sourced’ surveys of people with disabilities performed by Statistics Canada early in the pandemic [
30,
36]. Further, the respondents who completed the surveys and were included in the sub-analysis comparing both iterations may not have been representative of the survey respondents as a whole. For example, during both timeframes, these respondents were more likely to achieve WHO PA guidelines and less likely to do no MVPA whatsoever. Compared to the Statistics Canada surveys, strengths of the present survey are that it was repeated, measured PA participation, and was available in American Sign Language and plain language such that responses could be collected from individuals with more diverse impairment types.
We used the IPAQ to determine whether respondents achieved the WHO guidelines of 150+ min/week of PA [
24]. However, an inherent limitation of the IPAQ is that it categorizes all walking/wheeling as being of a lesser intensity than MVPA. Given that 45–55% of respondents reported impaired ability to walk, and energy expenditure during walking/wheeling is typically greater for those with impairments (e.g., who use canes, crutches, manual wheelchairs) than those without, some respondents may have undertaken walking/wheeling of adequate intensity to be considered MVPA. As such, we acknowledge that the IPAQ may miss some instances of moderate intensity walking/wheeling but, given the well-documented issues of over-reporting on the IPAQ and other self-report measures of PA participation [
37,
38], we believe that our data is an accurate representation of PA levels among Canadians with disabilities. This underscores the need for the development of valid and reliable self-report measures of PA that can be used to assess MVPA among people with diverse abilities.
Finally, the lack of pre-pandemic data on PA among Canadians with disabilities limits our ability to draw conclusions as to the impact of the pandemic on self-reported PA beyond that presented under ‘perceived impact of the pandemic’. However, it is a limitation that perceived impact was assessed by a single item that did not capture the magnitude of change.