Patients on regular haemodialysis will automatically achieve sodium and fluid balance with losses matching dietary intake, provided they are not becoming progressively fluid overloaded or depleted. Excretion of sodium and fluid in healthy subjects is mainly via the kidneys, which is one of many reasons why it is important to preserve residual kidney function (RKF) for as long as possible after initiation of dialysis.
When RKF can no longer prevent the accumulation of sodium and fluid during the interdialytic interval, sodium will be removed, along with the accumulated fluid, by ultrafiltration. During dialysis, the plasma water sodium concentration will equilibrate with the dialysate sodium concentration (DNa) by diffusion through the dialyser membrane. Unlike ultrafiltration, which always results in a loss of sodium from the body, diffusion may lead to sodium loss or gain. Despite reaching equilibrium, the serum sodium concentration (SNa) measured post-dialysis will not usually match the prescribed DNa. Post-dialysis SNa may be higher or lower due to the Gibbs–Donnan effect, reporting of whole serum rather than plasma water concentration [
1], and the variation between delivered and prescribed DNa [
2].
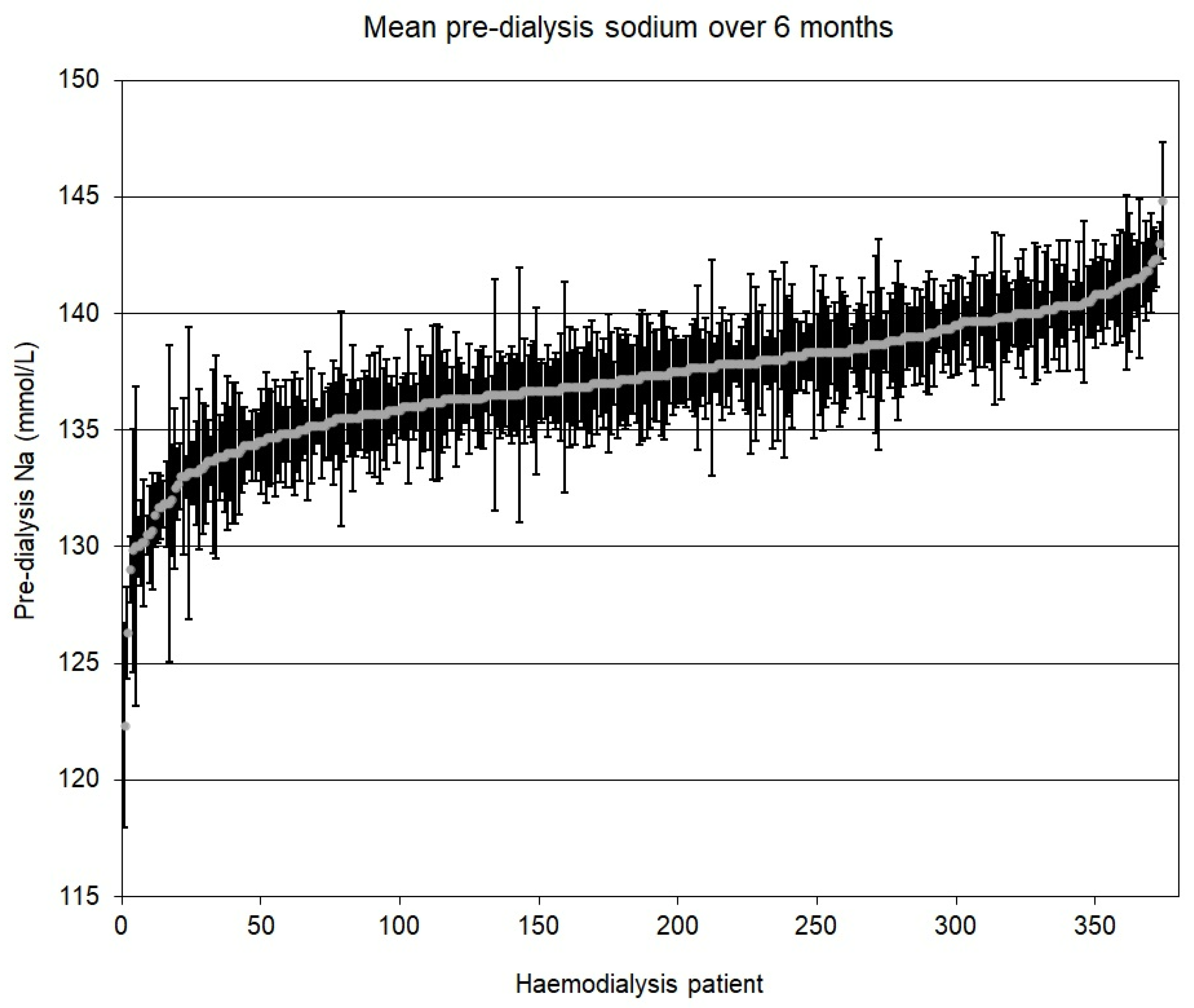
Figure 1 shows the mean pre-dialysis SNa from routine blood measurements for 375 patients treated in our centre over a 6-month period. The variation in mean SNa between patients is due to multiple factors that include RKF, adherence to dietary advice, and difference in the ‘set point’ for SNa (or ‘osmostat’), above which thirst is triggered [
3]. The almost complete absence of SNa above 145 mmol/L in our patients, which was also observed by McCausland et al. in a cohort of 2272 patients [
4], suggests that patients will not tolerate the thirst caused by SNa above the upper limit of the normal range (136–145 mmol/L). While hypernatraemia is very rare, the lack of a feedback mechanism that can correct low SNa means that hyponatraemia is much more common. In our patients, 27% had mean pre-dialysis SNa below the normal range and many more dipped below 136 mmol/L occasionally.
McCausland et al. showed that there was no difference in the mean pre-dialysis SNa for patients treated with DNa < 140, 140 or >140 mmol/L [
4], and after analysing the observational (DOPPS) data for 11,555 patients, Hecking et al. also found no association between pre-dialysis SNa and DNa [
5]. To maintain the same pre-dialysis SNa when DNa is reduced, patients must either increase their dietary sodium intake or decrease their fluid intake. If fluid intake does decrease, a reduction in DNa should be associated with a decrease in interdialytic fluid gain (IDFG). A systematic review of 23 studies comparing high and low DNa found that in almost all cases patients dialysing against low DNa did have significantly lower IDFG [
6]. Lower IDFG should lead to a reduction in intradialytic complications related to fluid removal. However, the review found that low DNa was frequently associated with an increased risk of morbidity, including intradialytic hypotension (IDH), cramps, and longer recovery times. During a recent RCT from New Zealand, patients who converted to DNa 135 mmol/L from 140 mmol/L had more than three times as many episodes of IDH and 10% of them withdrew before completing the 12-month follow-up due to IDH, headache, or cramps [
7]. This suggests the benefit of a lower ultrafiltration rate can be outweighed by osmotic disequilibrium (due to the fall in SNa during dialysis), which causes fluid to shift from extracellular to intracellular compartments, decreasing blood volume. Ultimately, the sodium gained between sessions has to be removed, and decreasing DNa simply changes the proportions lost by convection and diffusion.
Evidence relating to mortality is limited. In the DOPPS analysis, the use of higher DNa was associated with better survival in patients treated at facilities using a standard DNa but with higher mortality rates where DNa was individualised [
8]. This was due to the prescription of higher DNa in older and sicker patients, suggesting that comparisons of mortality rates should be restricted to patients whose DNa is not individualised [
9].
It is clear from the literature that there is no ideal DNa. This is not surprising as the problems related to DNa are caused by the accumulation of too much sodium and/or fluid between sessions. The best way to minimise accumulation (after the preservation of RKF) is to restrict salt intake. Lowering DNa will tend to increase the loss of accumulated sodium by diffusion with the risk of osmotic disequilibrium, while higher DNa will tend to increase the required ultrafiltration rates.
The standard DNa selected by dialysis units should minimise the interventions required for complications associated with low or high DNa. Assuming that there has been some degree of optimisation over the years, the best compromise is likely to be 138 to 140 mmol/L. Approximately 90% of the DOPPS units that had a standard DNa chose a concentration in this range [
10]. The optimum standard DNa for any unit will depend on practice patterns (interventions to preserve kidney function, availability of dietary advice, dialysis time and frequency, use of bioimpedance to assess fluid status, early assessment for transplant in healthier patients, etc.) and so may change over time.
Before adjusting the standard DNa, an audit should be carried out of IDFG, the frequency of intradialytic complications and/or interventions, and the change in SNa during dialysis. Measurements of pre- and post-dialysis SNa are required as the latter cannot be assumed to be equal to DNa. After excluding patients who rarely experience problems during dialysis, the proportion of symptomatic patients whose SNa increases or decreases during dialysis can be compared.
If SNa increases, the patient may benefit from a lower DNa. However, if the patient has low SNa due to fluid intake that is not sodium related (e.g., poor control of blood sugar or social drinking), the increase in SNa may be helping the patient tolerate fluid removal. Patients whose SNa decreases during dialysis may benefit from a higher DNa provided any additional fluid gained can be removed without complications.
If an adjustment to the standard DNa is indicated, the audit should be repeated once patients are established on the new DNa to check that a reduction in intradialytic morbidity across the unit has been achieved. The change may not always have the desired effect in symptomatic patients and may adversely affect those who were comfortable with the DNa to which they were accustomed.
As with adjustment of the standard DNa, individualisation of DNa has the potential to do more harm than good. Changes in prescription should not be made unless the unit has the resources to monitor the patient and ensure that they have benefitted. For patients with high IDFG and low pre-dialysis SNa, the cause of excessive fluid gain should be addressed before considering a decrease in DNa. A higher DNa may help patients who suffer with IDH and cramps but, again, other causes (such as excessive fluid depletion during dialysis and post-dialysis hypokalaemia) should be ruled out first.
We were asked to end this statement with our approach to selecting a standard DNa in a new unit with no historical data to audit. Our starting point would be 138 mmol/L, based on the opinion that inappropriately low target weight is a significant factor in intradialytic complications. If the setting of patients’ target weight is guided by objective measurements of fluid status rather than blood pressure, post-dialysis dehydration and loss of RKF should be avoided, meaning that patients are less likely to benefit from higher DNa. In our ideal practice, all staff in the new unit, not just the dietitians, would be able to provide appropriate and individualised dietary advice for patients with high IDFG.