Engaging in and Sustaining Physical Activity and Exercise: A Descriptive Qualitative Study of Adults 65 Years and Older Using the Self-Determination Theory
Abstract
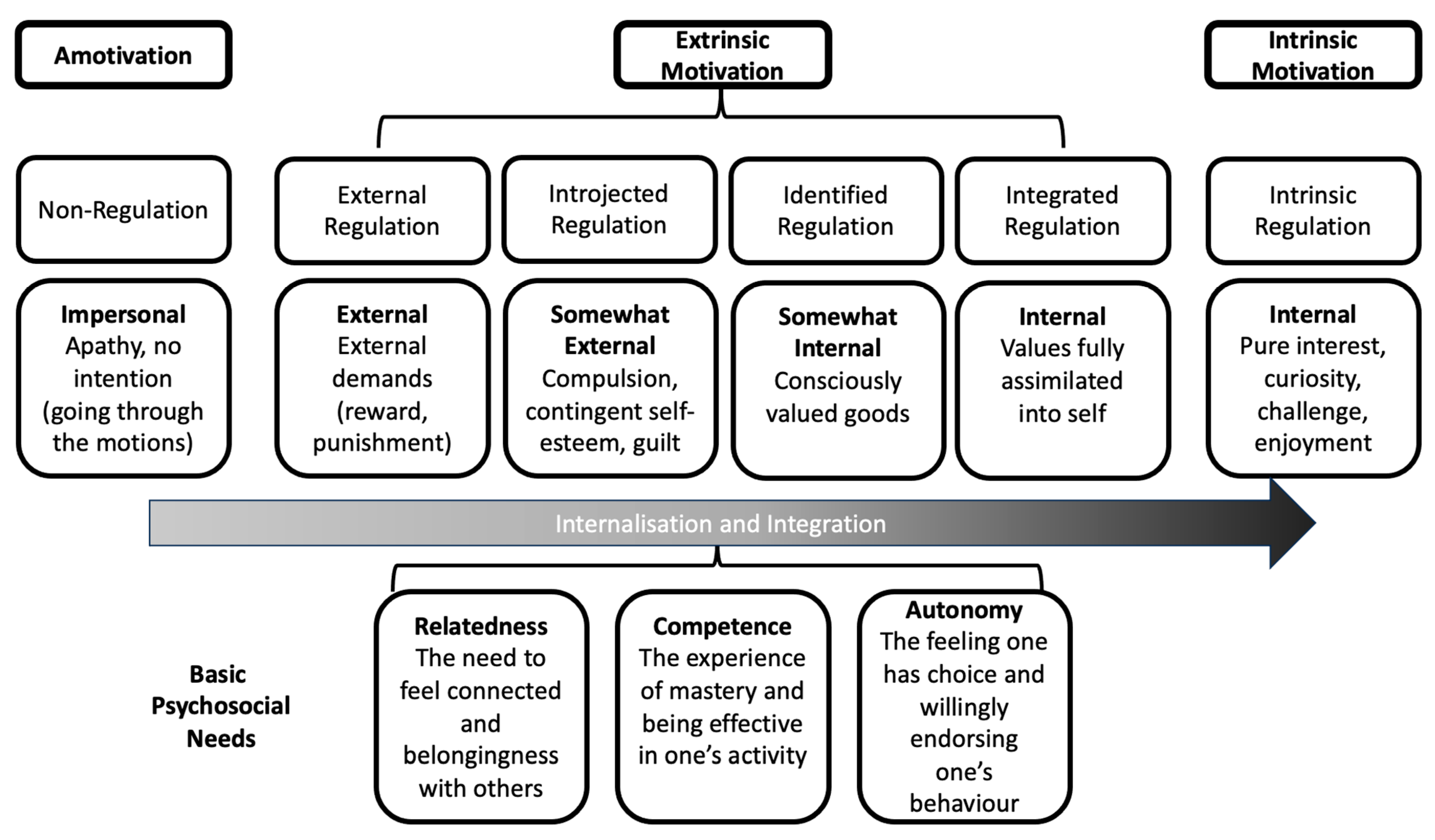
1. Introduction
2. Materials and Methods
2.1. Study and Sampling Context
2.2. Sample Participants and Recruitment
2.3. Data Collection
2.4. Analysis
3. Results
3.1. Themes and Sub-Themes
Theme 1: The Spectrum of Motivating Factors
3.2. Physical Activity and Exercise Bring Me Joy
“I do [enjoy participating in exercise]. I like my swimming.” … “You know just getting there, once you get there you feel I did it, I feel good now… You know…it’s a good feeling when you’ve worked out hard.”(C-FG3-P3)
“When I was younger I was a fairly good athlete and I was very competitive. That never quite goes away. So now I compete with myself.” …it’s a good feeling when you’ve worked out hard.”(C-FG3-P2)
“It feels good after you do-I do it every morning.”(FC-FG2-P4)
3.3. Meaningful Personal Impetuses
“lose weight…I’d like to build up more muscular strength…flexibility is critical as we get older.”(C-FG3-P1)
“And just to minimize the risks. You know and…like because I’m not flexible and not doing anything so I don’t…so you know bending down is much harder now with my knees. So I try to do little things like look at my balance when I’m…you know standing on one leg.”(C-FG3-P4)
“My goal was to walk without a friend here (referring to their walker).”(FC-FG1-P6)
“I already had a problem with balance and walking so for me it was just an automatic thing to try and get help to try and get back on my feet … I wanted to get rid of my walker…”(FC-FG1-P4)
“....arthritis, try to keep it at bay. And avoiding surgery.”(FC-FG1-P5)
“I had a lot of pain and I couldn’t sleep.”(FC-IN2-P1)
“I’m Diabetic. And getting off my duff is kind of important and it’s hard to do.”(C-FG3-P1)
“My doctor suggested that I lose some weight.”(FC-FG1-P6)
“…eah, um, because uh we started off with a reference from a family Doctor…”(C-FG2-P3)
“…when I got my Parkinson’s they recommended boxing or a punching bag, a speed bag, and um just the whole upper body movement, more upper movement, repetitive, sort of things.”(FC-FG1-P3)
3.4. I Get Active with a Little Help from my Spouse and Others
“I think if you have a partner and if the two of you are really interested today I don’t want to do something and my wife says okay let’s do it. Tomorrow she doesn’t want to do it, so we force each other.”(C-FG3-P3)
“I’m very good to giving into social pressures so if I know other people are coming and expecting me I’m more likely to go than if I’m just going on my own. I’m really good at making up excuses.”(C-FG3-P1)
3.5. I See Changes and Improvements
“Yes definitely, there is benefits to going. I know I was away from exercise for 3 years babysitting my grandson and I lost a lot of just my general strength and inabilities. I’ve been here for 5 months and I feel myself getting my strength back. I appreciate it a lot because I have heart issues and it’s very easy to sit and you get very old and you just sit. This is good for me.”(FC-FG2-P5)
“I’ve been using a walker for 12 years I was young when I started and I’m just as active now with the walker in fact more active now than I was back then.”(FC-FG1-P2)
“Well, I think I’m a lot fitter than most of my friends to be quite honest.” … Well, they’ve kept me fairly active. And able to do a lot more things than a lot of people my age.”(FC-IN1-P1)
“I always look at other people who are younger than I am and they can not even walk to the bus stop anymore. And I think that is an incentive for me to keep on moving.”(C-FG3-P5)
“Yes, I’m doing the best I can to improve and I have actually-the settings on resistance machines and that, they’re going up. So I’m doing a little more than maintenance. And it takes a lot time of course to do-to get anywhere with this. But I think over the time I’ve made substantial progress…Well, the only real expectation I had was to get rid of the pain so I could sleep at night. Now, the fact that I’m sorta improving –I really wasn’t expecting that to happen. You could say they more than met expectations.”(FC-IN2-P1)
Theme 2—Facilitators and Barriers
3.6. I Can Do This
“I was pleased with the program that was set up for me. Once it was set up I could administer it myself you know, 3 times a week.”(FC-FG1-P3)
3.7. Connections and Sense of Belonging
“Well I think the social aspect of it … Just getting out and meeting people and so on, you know and uh, I think that’s a big part.”(C-FG2-P1)
“It provides motivation … like you say-walking-I mean I love to walk but it’s better if you do it in a more social situation or where there’s other people … Or even if you can talk with somebody.”(C-FG2-P2)
“I wanted to exercise, plus meeting people. I live by myself with a dog and a cat. Just meeting other people and talking to them. It helps I think.”(FC-FG2-P1)
“Yeah I think being around people you can joke with or talk a little bit, that’s a big part of it.”(C-FG3-P4)
“I’ve made some good friends.”(FC-IN1-P1)
“I met my chess contacts through the Club.”(FC-FG1-P2)
“So… I think the incentive the ability to go and such and do things, meet people, have some continuity in your life is a good thing.”(C-FG1-P1)
3.8. Setting, Environment, and People Supports
“For my needs, it’s been very adequate. I come down 5 days a week, we have a book in which they’ve listed what we should do so that we’re not over doing it or, not doing enough and I found that worked very well, … they sat down and went through it so I knew what I was supposed to be doing, I wasn’t guessing, because some of the them will write in the space what you’re supposed to be doing. You don’t understand what they’re trying to tell you because they have a gym way of talking, so that you might not get it, but I found here it’s very easy just to ask someone and they’ll tell you, until you get on to your own program and then it sort of becomes, it’s memory work.”(FC-FG1-P6)
“I think also when you ask for help, help is provided. They’re not breathing down your neck all the time which is a good thing too. It’s just finding that right balance. They’ve always been helpful.”(FC-FG1-P7)
“I was diagnosed with Parkinson’s disease and they emphasized that exercise is vital to combat, to delay the onset of further Parkinson’s problems.”(FC-FG1-P3)
“I think the choice of equipment is quite good… if you have to do strength or flexibility, it’s just a matter of a hydraulic adjustment as opposed to taking off weights, that people might not have the ability to do and the mobility to move things around…it’s just the matter of pushing a button. I think that is very very good.”(FC-FG1-P9)
“I think there’s some issues about seniors trying to get fit that are quite different than people in their twenties, thirties and forties. I like to think that I’ve been collecting injuries for a very long time and I’m quite frankly nervous about starting a series of exercises or strengthening activities because I don’t want to exasperate my pre-existing injuries. I know where my weaknesses are and I don’t know how to get past them.(C-FG3-P1)
“I think that’s very valid. I’m feeling the same way. Like I want to know that someone is also, has expertise with this age group because of the limitations that we may experience with the aging process … I was more referring to the age specific changes that we might have.”(C-FG3-P4)
“But they’re not necessarily totally qualified so it’s like. … It’s you, you don’t have somebody who knows what they’re doing.”(C-FG2-P2)
“You know I-I was fine before I got all this arthritis … You know but then now I-I wanna go but I don’t wanna go and be the only one that can’t go like that … And then the-the girl is so young, you know, and they try to understand but they don’t understand.”(C-FG2-P4)
“if they can’t tell me what I can do to help myself more I’m at a loss.”(C-FG1-P1)
“And the staff here in-invariable say good morning to you. They’re really good at it. It seems like a friendly place.”(FG2-P2)
“… the assistants who accompany those who have disabilities are also excellent and I’ve always been impressed with the quality of the personnel they have in the program.”(FG1-P2)
“Oh, I think that they’re a very friendly bunch and certainly able to help if you help if you have a problem. Anyway, it’s just a great atmosphere.”(IN1-P1)
“Well they work with us individually too um, setting up the program we will follow we have books down in the gym that we keep track of what we do every day and what we accomplished um, it’s a well-thought out program I think. There’s something for everybody, not everybody does the same thing when they get down there, they more or less have their own programs.”(FG1-P1)
“They give you a program and they reassess you every few weeks, and that’s an good, important thing to do to so you don’t get stuck in the one set of exercises. Yup, yes they change [the program] as you get stronger or things in your life change.” … “Oh well, what I like especially, apart from the equipment. The equipment was good. But the people, the personnel, and they’re great... they’re tops. They help you they go around and they supervise. They’re fantastic, that’s it.”(FG2-P4)
“And I think they are very knowledgeable too. I’ve never had a question that they couldn’t answer. I had both hips replaced and they were certainly helpful in my recovery from that.”(FG2-P3)
“…you are still going to need individualized assistance for you. Everybody else has got their own problems. So they have to look at everybody individually.”(C-FG3-P2)
“With the personnel to help with individual needs.” … “And help to get past [health limitations]. I know what the limitations are but i don’t know how to get passed it.”(C-FG3-P1)
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Ageing and Health. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 10 January 2021).
- Beard, J.R.; Officer, A.; de Carvalho, I.A.; Sadana, R.; Pot, A.M.; Michel, J.-P.; Lloyd-Sherlock, P.; Epping-Jordan, J.E.; Peeters, G.M.E.E.G.; Mahanani, W.R.; et al. The World report on ageing and health: A policy framework for healthy ageing. Lancet Lond. Engl. 2016, 387, 2145–2154. [Google Scholar] [CrossRef] [PubMed]
- Government of Canada CI of HR; Canadian Institutes of Health Research. CIHR Institute of Aging Strategic Plan 2019–2021: Living Longer, Living Better—CIHR. 2003. Available online: https://cihr-irsc.gc.ca/e/51447.html (accessed on 10 March 2021).
- World Health Organization. Integrated Care for Older People: Guidelines on Community-Level Interventions to Manage Declines in Intrinsic Capacity; World Health Organization: Geneva, Switzerland, 2017; Available online: https://iris.who.int/handle/10665/258981 (accessed on 23 December 2023)ISBN 978-92-4-155010-9.
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Rep. 1985, 100, 126–131. [Google Scholar] [PubMed]
- WHO Team. WHO Guidelines on Physical Activity and Sedentary Behaviour. 2020, p. 104. Available online: https://iris.who.int/bitstream/handle/10665/336656/9789240015128-eng.pdf?sequence=1 (accessed on 23 December 2023).
- Gomes, M.; Figueiredo, D.; Teixeira, L.; Poveda, V.; Paúl, C.; Santos-Silva, A.; Costa, E. Physical inactivity among older adults across Europe based on the SHARE database. Age Ageing 2017, 46, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.S.; Vos, T.; Flaxman, A.D.; Danaei, G.; Shibuya, K.; Adair-Rohani, H.; AlMazroa, M.A.; Amann, M.; Anderson, H.R.; Andrews, K.G.; et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2224–2260. [Google Scholar] [CrossRef] [PubMed]
- Bauman, A.; Merom, D.; Bull, F.C.; Buchner, D.M.; Fiatarone Singh, M.A. Updating the Evidence for Physical Activity: Summative Reviews of the Epidemiological Evidence, Prevalence, and Interventions to Promote “Active Aging”. Gerontologist 2016, 56 (Suppl. 2), S268–S280. [Google Scholar] [CrossRef] [PubMed]
- Cassilhas, R.C.; Tufik, S.; Mello, M.T. Physical exercise, neuroplasticity, spatial learning and memory. Cell. Mol. Life Sci. 2016, 73, 975–983. [Google Scholar] [CrossRef]
- Peluso, M.A.M.; Andrade, L.H.S.G. de Physical Activity and Mental Health: The Association Between Exercise and Mood. Clinics 2005, 60, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Swift, D.L.; Johannsen, N.M.; Lavie, C.J.; Earnest, C.P.; Church, T.S. The Role of Exercise and Physical Activity in Weight Loss and Maintenance—ClinicalKey. Prog. Cardiovasc. Dis. 2019, 56, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Warburton, D.E.R.; Nicol, C.W.; Bredin, S.S.D. Health benefits of physical activity: The evidence. CMAJ Can. Med. Assoc. J. 2006, 174, 801–810. [Google Scholar] [CrossRef]
- McPhee, J.S.; French, D.P.; Jackson, D.; Nazroo, J.; Pendleton, N.; Degens, H. Physical activity in older age: Perspectives for healthy ageing and frailty. Biogerontology 2016, 17, 567–580. [Google Scholar] [CrossRef]
- Pedersen, B.K.; Saltin, B. Evidence for prescribing exercise as therapy in chronic disease. Scand. J. Med. Sci. Sports 2006, 16, 3–63. [Google Scholar] [CrossRef]
- Chodzko-Zajko, W.J.; Proctor, D.N.; Fiatarone Singh, M.A.; Minson, C.T.; Nigg, C.R.; Salem, G.J.; Skinner, J.S. Exercise and Physical Activity for Older Adults. Med. Sci. Sports Exerc. 2009, 41, 1510–1530. [Google Scholar] [CrossRef] [PubMed]
- Liu-Ambrose, T.; Davis, J.C.; Best, J.R.; Dian, L.; Madden, K.; Cook, W.; Hsu, C.L.; Khan, K.M. Effect of a Home-Based Exercise Program on Subsequent Falls Among Community-Dwelling High-Risk Older Adults After a Fall: A Randomized Clinical Trial. JAMA 2019, 321, 2092–2100. [Google Scholar] [CrossRef] [PubMed]
- Vogel, T.; Brechat, P.-H.; Leprêtre, P.-M.; Kaltenbach, G.; Berthel, M.; Lonsdorfer, J. Health benefits of physical activity in older patients: A review. Int. J. Clin. Pract. 2009, 63, 303–320. [Google Scholar] [CrossRef] [PubMed]
- Pereira, C.; Baptista, F.; Cruz-Ferreira, A. Role of physical activity, physical fitness, and chronic health conditions on the physical independence of community-dwelling older adults over a 5-year period—ClinicalKey. Arch. Gerontol. Geriatr. 2016, 65, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Dal Bello-Haas, V.P.M.; O’Connell, M.E.; Morgan, D.G. Maintaining health and wellness in the face of dementia: An exploratory analysis of individuals attending a rural and remote memory clinic. Rural Remote Health 2014, 14, 2722. [Google Scholar] [CrossRef]
- O’Connell, M.E.; Dal Bello-Haas, V.; Crossley, M.; Morgan, D.G. Attitudes toward physical activity and exercise: Comparison of memory clinic patients and their caregivers and prediction of activity levels. J. Aging Phys. Act. 2015, 23, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Stiggelbout, M.; Hopman-Rock, M.; Mechelen, W. van Entry Correlates and Motivations of Older Adults Participating in Organized Exercise Programs. J. Aging Phys. Act. 2008, 16, 342–354. [Google Scholar] [CrossRef] [PubMed]
- Maula, A.; LaFond, N.; Orton, E.; Iliffe, S.; Audsley, S.; Vedhara, K.; Kendrick, D. Use it or lose it: A qualitative study of the maintenance of physical activity in older adults. BMC Geriatr. 2019, 19, 349. Available online: https://go-gale-com.libaccess.lib.mcmaster.ca/ps/i.do?p=AONE&sw=w&issn=14712318&v=2.1&it=r&id=GALE%7CA610303468&sid=googleScholar&linkaccess=abs (accessed on 2 September 2023). [CrossRef]
- Samra, P.K.; Rebar, A.L.; Parkinson, L.; van Uffelen, J.G.Z.; Schoeppe, S.; Power, D.; Schneiders, A.; Vandelanotte, C.; Alley, S. Physical Activity Attitudes, Preferences, and Experiences of Regionally-Based Australia Adults Aged 65 Years and Older. J. Aging Phys. Act. 2019, 27, 446–451. [Google Scholar] [CrossRef]
- Beauchamp, M.R.; Ruissen, G.R.; Dunlop, W.L.; Estabrooks, P.A.; Harden, S.M.; Wolf, S.A.; Liu, Y.; Schmader, T.; Puterman, E.; Sheel, A.W.; et al. Group-based physical activity for older adults (GOAL) randomized controlled trial: Exercise adherence outcomes. Health Psychol. 2018, 37, 451–461. [Google Scholar] [CrossRef]
- Teixeira, P.J.; Carraça, E.V.; Markland, D.; Silva, M.N.; Ryan, R.M. Exercise, physical activity, and self-determination theory: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 78. [Google Scholar] [CrossRef]
- Haynes, A.; Sherrington, C.; Wallbank, G.; Wickham, J.; Tong, A.; Kirkham, C.; Manning, S.; Ramsay, E.; Tiedemann, A. Using self-determination theory to understand and improve recruitment for the Coaching for Healthy Ageing (CHAnGE) trial. PLoS ONE 2021, 16, e0259873. [Google Scholar] [CrossRef]
- Dattilo, J.; Mogle, J.; Lorek, A.E.; Freed, S.; Frysinger, M. Using Self-determination Theory to Understand Challenges to Aging, Adaptation, and Leisure among Community-dwelling Older Adults. Act. Adapt. Aging 2018, 42, 85–103. [Google Scholar] [CrossRef]
- Ntoumanis, N.; Ng, J.Y.Y.; Prestwich, A.; Quested, E.; Hancox, J.E.; Thøgersen-Ntoumani, C.; Deci, E.L.; Ryan, R.M.; Lonsdale, C.; Williams, G.C. A meta-analysis of self-determination theory-informed intervention studies in the health domain: Effects on motivation, health behavior, physical, and psychological health. Health Psychol. Rev. 2021, 15, 214–244. [Google Scholar] [CrossRef]
- Ryan, R.M.; Deci, E.L. Self-Determination Theory: Basic Psychological Needs in Motivation, Development, and Wellness; The Guilford Press: New York, NY, USA, 2017; p. 756. ISBN 978-1-4625-2876-9. [Google Scholar]
- Deci, E.L.; Ryan, R.M. The “what” and “why” of goal pursuits: Human needs and the self-determination of behavior. Psychol. Inq. 2000, 11, 227–268. [Google Scholar] [CrossRef]
- Deci, E.L.; Ryan, R.M. Self-Determination Theory: A Macrotheory of Human Motivation, Development, and Health. Can. Psychol. 2008, 49, 182–185. [Google Scholar] [CrossRef]
- Sandelowski, M. Whatever happened to qualitative description? Res. Nurs. Health 2000, 23, 334–340. [Google Scholar] [CrossRef] [PubMed]
- Sandelowski, M. What’s in a name? Qualitative description revisited. Res. Nurs. Health 2010, 33, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Creswell, J.W.; Creswell, J.D. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches, 5th ed.; SAGE: Thousand Oaks, CA, USAu, 2018; p. 275. ISBN 978-1-5063-8670-6. [Google Scholar]
- Kim, H.; Sefcik, J.S.; Bradway, C. Characteristics of Qualitative Descriptive Studies: A Systematic Review. Res. Nurs. Health 2017, 40, 23–42. [Google Scholar] [CrossRef]
- Bradshaw, C.; Atkinson, S.; Doody, O. Employing a Qualitative Description Approach in Health Care Research. Glob. Qual. Nurs. Res. 2017, 4, 2333393617742282. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, B.C.; Harris, I.B.; Beckman, T.J.; Reed, D.A.; Cook, D.A. Standards for Reporting Qualitative Research: A Synthesis of Recommendations. Acad. Med. 2014, 89, 1245–1251. [Google Scholar] [CrossRef] [PubMed]
- Government of Canada, S.C. Census Profile, 2016 Census. 2017. Available online: https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/index.cfm?Lang=E (accessed on 23 December 2023).
- Patton, M.Q. Qualitative Research & Evaluation Methods, 4th ed.; Sage Publications: Thousand Oaks, CA, USA, 2023; Available online: https://us.sagepub.com/en-us/nam/qualitative-research-evaluation-methods/book232962 (accessed on 23 December 2023).
- Hennink, M.M.; Kaiser, B.N.; Marconi, V.C. Code Saturation Versus Meaning Saturation: How Many Interviews Are Enough? Qual. Health Res. 2017, 27, 591–608. [Google Scholar] [CrossRef] [PubMed]
- Hennink, M.M.; Kaiser, B.N.; Weber, M.B. What Influences Saturation? Estimating Sample Sizes in Focus Group Research. Qual. Health Res. 2019, 29, 1483–1496. [Google Scholar] [CrossRef] [PubMed]
- Rikli, R.E.; Jones, C.J. Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical independence in later years. Gerontologist 2013, 53, 255–267. [Google Scholar] [CrossRef]
- Rikli, R.E.; Jones, C.J. Functional Fitness Normative Scores for Community-Residing Older Adults, Ages 60–94. J. Aging Phys. Act. 1999, 7, 162–181. [Google Scholar] [CrossRef]
- Fereday, J.; Muir-Cochrane, E. Demonstrating Rigor Using Thematic Analysis: A Hybrid Approach of Inductive and Deductive Coding and Theme Development—Jennifer Fereday, Eimear Muir-Cochrane. Int. J. Qual. Methods 2006, 5, 80–92. [Google Scholar] [CrossRef]
- Bingham, A.J. From Data Management to Actionable Findings: A Five-Phase Process of Qualitative Data Analysis. Int. J. Qual. Methods 2023, 22, 16094069231183620. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Nowell, L.S.; Norris, J.M.; White, D.E.; Moules, N.J. Thematic Analysis: Striving to Meet the Trustworthiness Criteria. Int. J. Qual. Methods 2017, 16, 1609406917733847. Available online: https://journals.sagepub.com/doi/10.1177/1609406917733847 (accessed on 25 December 2023). [CrossRef]
- Proudfoot, K. Inductive/Deductive Hybrid Thematic Analysis in Mixed Methods Research. J. Mix. Methods Res. 2023, 17, 308–326. [Google Scholar] [CrossRef]
- Bingham, A.J.; Witkowsky, P. Deductive and inductive approaches to qualitative data analysis. In Analyzing and Interpreting Qualitative Data: After the Interview; Vanover, C., Mihas, P., Saldaña, J., Eds.; Sage Publications: Thousand Oaks, CA, USA, 2022; pp. 133–146. ISBN 978-1-5443-9590-6. [Google Scholar]
- Rhodes, R.E.; McEwan, D.; Rebar, A.L. Theories of physical activity behaviour change: A history and synthesis of approaches. Psychol. Sport Exerc. 2019, 42, 100–109. [Google Scholar] [CrossRef]
- Jones, S.A.; Alicea, S.K.; Ortega, J.D. A Self-Determination Theory Approach for Exercise Motivation in Rural Dwelling Older Adults. Act. Adapt. Aging 2020, 44, 24–41. [Google Scholar] [CrossRef]
- Rasinaho, M.; Hirvensalo, M.; Leinonen, R.; Lintunen, T.; Rantanen, T. Motives for and Barriers to Physical Activity among Older Adults with Mobility Limitations. J. Aging Phys. Act. 2007, 15, 90–102. [Google Scholar] [CrossRef] [PubMed]
- Newson, R.S.; Kemps, E.B. Factors That Promote and Prevent Exercise Engagement in Older Adults. J. Aging Health 2007, 19, 470–481. [Google Scholar] [CrossRef] [PubMed]
- Franco, M.R.; Tong, A.; Howard, K.; Sherrington, C.; Ferreira, P.H.; Pinto, R.Z.; Ferreira, M.L. Older people’s perspectives on participation in physical activity: A systematic review and thematic synthesis of qualitative literature. Br. J. Sports Med. 2015, 49, 1268–1276. [Google Scholar] [CrossRef] [PubMed]
- Bethancourt, H.J.; Rosenberg, D.E.; Beatty, T.; Arterburn, D.E. Barriers to and Facilitators of Physical Activity Program Use Among Older Adults. Clin. Med. Res. 2014, 12, 10–20. [Google Scholar] [CrossRef]
- Cohen-Mansfield, J.; Marx, M.S.; Biddison, J.R.; Guralnik, J.M. Socio-environmental exercise preferences among older adults. Prev. Med. 2004, 38, 804–811. [Google Scholar] [CrossRef] [PubMed]
- Schneider, J.K.; Eveker, A.; Bronder, D.R.; Meiner, S.E.; Binder, E.F. Exercise training program for older adults: Incentives and disincentives for participation. J. Gerontol. Nurs. 2003, 29, 21–31. [Google Scholar] [CrossRef]
- Cunningham, C.; O’Sullivan, R. Healthcare Professionals Promotion of Physical Activity with Older Adults: A Survey of Knowledge and Routine Practice. Int. J. Environ. Res. Public Health 2021, 18, 6064. [Google Scholar] [CrossRef]
- Lindsay Smith, G.; Banting, L.; Eime, R.; O’Sullivan, G.; van Uffelen, J.G.Z. The association between social support and physical activity in older adults: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 56. [Google Scholar] [CrossRef]
- Holt-Lunstad, J.; Smith, T.B.; Baker, M.; Harris, T.; Stephenson, D. Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspect. Psychol. Sci. J. Assoc. Psychol. Sci. 2015, 10, 227–237. [Google Scholar] [CrossRef]
- Pickering, J.; Wister, A.V.; O’Dea, E.; Chaudhury, H. Social isolation and loneliness among older adults living in rural areas during the COVID-19 pandemic: A scoping review. BMC Geriatr. 2023, 23, 511. [Google Scholar] [CrossRef]
- Schnittger, R.I.B.; Wherton, J.; Prendergast, D.; Lawlor, B.A. Risk factors and mediating pathways of loneliness and social support in community-dwelling older adults. Aging Ment. Health 2012, 16, 335–346. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Social Foundations of Thought and Action: A Social Cognitive Theory; Prentice-Hall, Inc.: Englewood Cliffs, NJ, USA, 1986; p. 617. ISBN 978-0-13-815614-5. [Google Scholar]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Rosenstock, I.M.; Strecher, V.J.; Becker, M.H. Social learning theory and the Health Belief Model. Health Educ. Q. 1988, 15, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Meredith, S.J.; Cox, N.J.; Ibrahim, K.; Higson, J.; McNiff, J.; Mitchell, S.; Rutherford, M.; Wijayendran, A.; Shenkin, S.D.; Kilgour, A.H.M.; et al. Factors that influence older adults’ participation in physical activity: A systematic review of qualitative studies. Age Ageing 2023, 52, afad145. [Google Scholar] [CrossRef] [PubMed]
- Mansell, I.; Bennett, G.; Northway, R.; Mead, D.; Moseley, L. The learning curve: The advantages and disadvantages in the use of focus groups as a method of data collection: Focus groups are not simply a discussion between people, but are focused interviews exploring interactions between participants. In this paper, Ian Mansell, Glynis Bennett, Ruth Northway, Donna Mead and Laurie Moseley explore the complexities and practicalities of using focus groups in research, with reference to a study of palliative care services. Nurse Res. 2004, 11, 79–88. [Google Scholar]
- Focus Groups: A Practical Guide for Applied Research, 5th ed.; SAGE: Los Angeles, CA, USA, 2015; ISBN 978-1-4833-5409-5.
- Feil, K.; Fritsch, J.; Rhodes, R.E. The intention-behaviour gap in physical activity: A systematic review and meta-analysis of the action control framework. Br. J. Sports Med. 2023, 57, 1265–1271. [Google Scholar] [CrossRef] [PubMed]
- Moschny, A.; Platen, P.; Klaaßen-Mielke, R.; Trampisch, U.; Hinrichs, T. Barriers to physical activity in older adults in Germany: A cross-sectional study. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 121. [Google Scholar] [CrossRef]
- Stalling, I.; Albrecht, B.M.; Foettinger, L.; Recke, C.; Bammann, K. Associations between socioeconomic status and physical activity among older adults: Cross-sectional results from the OUTDOOR ACTIVE study. BMC Geriatr. 2022, 22, 396. [Google Scholar] [CrossRef] [PubMed]
| Variable | n (%) OR Mean (SD), Range OR Mode, Range |
|---|---|
| Sex, female | 23 (62.2%) |
| Age, years Older adult fitness club member participants Participants engaged in community-based PA Participants interested, but not engaged in community-based PA | 80.9 (7.4) 77.7 (8.0) 76 (SD 6.3) |
| Ethnic origin Caribbean North American European | 3 (8.1%) 18 (48.6%) 16 (43.2%) |
| Education Level Did not complete high school Completed high school degree Completed a college or university degree Other training | 7 (16.2%) 6 (18.9%) 20 (54.1%) 3 (8.1%) |
| Living Status Lives alone Lives with spouse or partner Lives with family members or friends | 19 (51.4%), 14 (37.8%) 4 (10.8%) |
| Employment status Retired, not working Working part-time Working full-time | 35 (94.6%) 1 (2.7%, participant aged 73 years) 1 (2.7%, participant aged 87 years) |
| Number of health conditions * | 2, 0 to 8 |
| Assistive device use Walker Cane Scooter Wheelchair | 3 (8.1%) 4 (10.8%) 1 (2.7%) 2 (5.4%) |
| Amount participant willing to pay for PA or EX An individual PA or EX session CAD 3 CAD 5 Membership or program fee CAD 25 to CAD 50/month CAD 50 to CAD 75/month As low as possible | 32 (86.5%) 5 (13.5%) 32 (86.5%) 3 (8.1%) 2 (5.4%) |
| Subtheme | Description | Representative Quotes |
|---|---|---|
| I Cannot Do This | This subtheme underscored the barriers identified by participants, specifically related to a lack of discipline as a fundamental hindrance to their engagement in PA. This challenge was particularly pronounced among participants who were not members of the older adult fitness club. The feelings associated with real and perceived lack of skills and abilities on sense of competence and, as a result, not finding PA pleasurable was unmistakeable. | “don’t know where to start” (C-FG1-P1) “Um, so, uh the problem was I think discipline …” (C-FG2-P3) “I’m not disciplined enough.” (C-FG1-P1) “This is kind of a…it’s my issue but I’ve never been engaged in sports. And I think part of it that I was never good at it. You know clumsy … You know you’re…so I’ve never been involved in a positive way. Feeling that I can do those things. And I think in my head that’s sort of been perpetuated so that I have joined gyms for years in the past. Like years and years ago and felt intimidated. You know sat on the equipment on the wrong way and had somebody come by and say oh my dear you’re sitting on that backwards. You know like, you just kind of…reinforces that I’m not…I don’t know if capable is the word but…so I never really enjoyed it.” (C-FG3-P1) |
| Setting, Environment, and People Supports | Participants who were not members of the older adult fitness club discussed a general lack of community-based PA programs and clubs for older adults, as well as limited aspects of programs and clubs for older adults that were in existence to address their needs and goals. The lack of optimal challenges and opportunities to engage in challenging activities to support the SDT competence need was evident. | “And um, I just find in XXX there’s a lot of card playing people like that. …No but there’s really nothing else that you know you can find.” (C-FG2-P1) “But that -sorry I was gonna say that that’s there seems to be and maybe this is just me this notion that seniors just need the recreational piece of it … And-and I think through research and stuff.” (C-FG2-P2) “So, you’re actually sitting and doing stretching and working with balls and stuff like that… and I’d like to do more than that.” (C-FG1-P1) |
Participants who were not members of the older adult fitness club described their negative experiences and lack of relatedness supports when seeking out PA or EX programs and facilities and centers which adversely affected their desire to join or participate. They were made to feel insignificant and not valued, and that they did not belong. | “I find the fitness club you go in as an old person and you still there looking after these guys over here. So that’s the only thing I haven’t really been in to look really, that’s what I found really. They don’t love old people.” (C-FG3-P3) “Yeah I have to agree with that. I looked into joining a club downtown. I got one of these free try us out passes. Nobody spoke to me, nobody looked at me. Lots of people looking at their own bulging muscles but…(laughter) …not at my flabby ones (laughter) … I would never return.” (C-FG3-P1) | |
| Pragmatics | Practical environment and setting supports were highlighted as important as they may be potential barriers to engaging in and sustaining PA: costs, e.g., need to be reasonable; convenience and location, e.g., not wanting to have to travel long distances, especially for those without a car or during inclement weather; need for small number of participants to allow for tailored attention, feedback, and recommendations for progression; and need for availability of safe and easy-to-use equipment. | “There wasn’t parking in this lot, there wasn’t parking across the street and I ended up having to go down to the school which is not a a huge problem but for someone who has ability issues it may be a problem …” (FC-FG1-P4) “I’d like to see it open on Sunday for a few hours. I really regret that it goes from Friday to Monday.” (FC-FG1-P5) “And things like the um, swimming pool that’s way up on XXX … It’s far too expensive for me… You know? Um, so there are those limitations, it’s either distance, bus, you know?” (C-FG1-P1) “It depends on the fitness center or gym. It depends on the staff that they have. Now if they’ve got good staff you get lots of good training or whatever you need. Whether you’re a senior or…” (C-FG3-P2) “Yes and I don’t want to travel really long distances to get to a place where I’m going to participate in something and I do…I understand all the reasons why it’s beneficial to participate and be active. You know all…intellectually I’ve got it.” (C-FG3-P4) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mappanasingam, A.; Madigan, K.; Kalu, M.E.; Maximos, M.; Dal Bello-Haas, V. Engaging in and Sustaining Physical Activity and Exercise: A Descriptive Qualitative Study of Adults 65 Years and Older Using the Self-Determination Theory. J. Ageing Longev. 2024, 4, 156-176. https://doi.org/10.3390/jal4020011
Mappanasingam A, Madigan K, Kalu ME, Maximos M, Dal Bello-Haas V. Engaging in and Sustaining Physical Activity and Exercise: A Descriptive Qualitative Study of Adults 65 Years and Older Using the Self-Determination Theory. Journal of Ageing and Longevity. 2024; 4(2):156-176. https://doi.org/10.3390/jal4020011
Chicago/Turabian StyleMappanasingam, Anittha, Katelyn Madigan, Michael E. Kalu, Melody Maximos, and Vanina Dal Bello-Haas. 2024. "Engaging in and Sustaining Physical Activity and Exercise: A Descriptive Qualitative Study of Adults 65 Years and Older Using the Self-Determination Theory" Journal of Ageing and Longevity 4, no. 2: 156-176. https://doi.org/10.3390/jal4020011
APA StyleMappanasingam, A., Madigan, K., Kalu, M. E., Maximos, M., & Dal Bello-Haas, V. (2024). Engaging in and Sustaining Physical Activity and Exercise: A Descriptive Qualitative Study of Adults 65 Years and Older Using the Self-Determination Theory. Journal of Ageing and Longevity, 4(2), 156-176. https://doi.org/10.3390/jal4020011