Process Mining Organization (PMO) Modeling and Healthcare Processes
Abstract
1. Introduction
1.1. Main Scenario of Technologies and Tools Upgrading Processes in Healthcare
1.2. Main Research Topic: Process Mining Organization (PMO) Modeling
1.3. Alternative Approaches for Process Modeling
1.4. Importance of Data Interpretations and Data Modeling in Healthcare Processes
1.5. Paper Validation Criteria and Vademecum
- Good process performance deduced using the KPI estimation (decrease in time delays, risk events, patient risk, and in unnecessary care services);
- Workflow matching with priorities and urgencies of the hospitalization units;
- Positive feedback of doctors and of other healthcare personnel regarding the applied operative workflows limiting risks;
- Possibility to formulate an audit form matched with the designed workflows.
- Section 2 provides tools and methods regarding BPMN-PMO design and modeling;
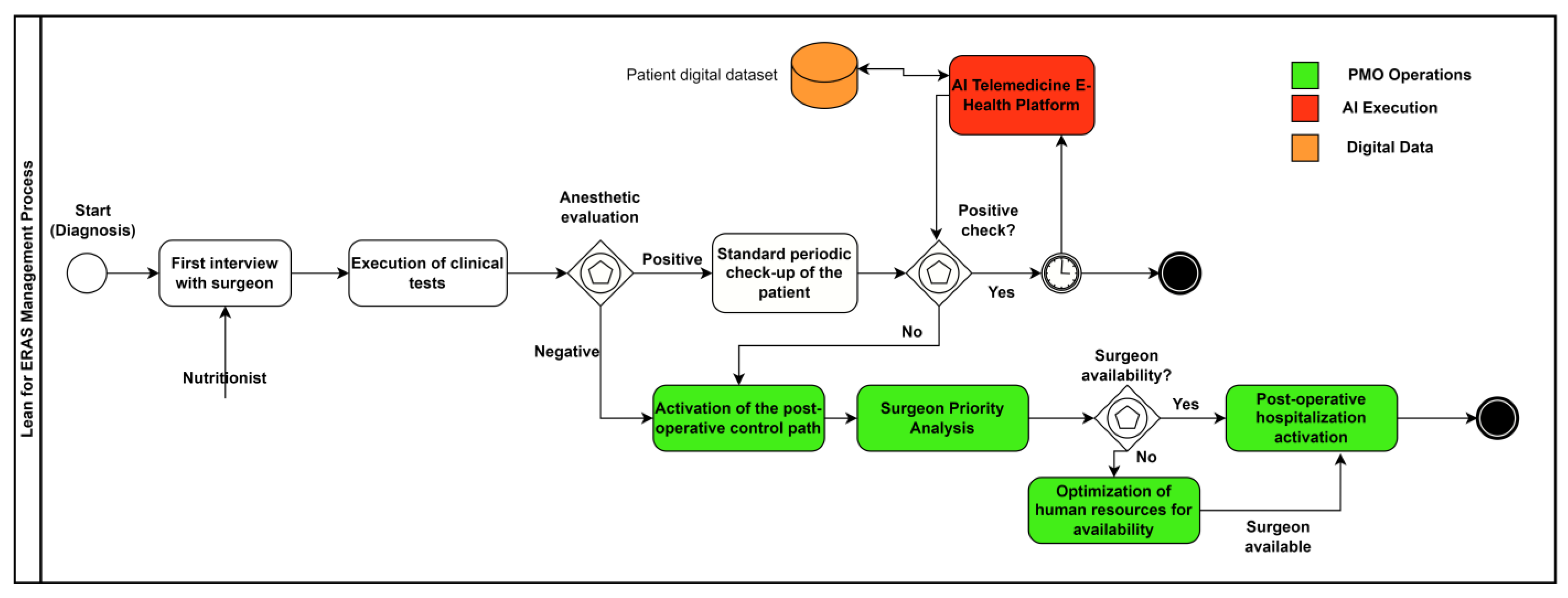
- Section 3.1 develops BPMN-PMO examples regarding HR organizations in healthcare environments;
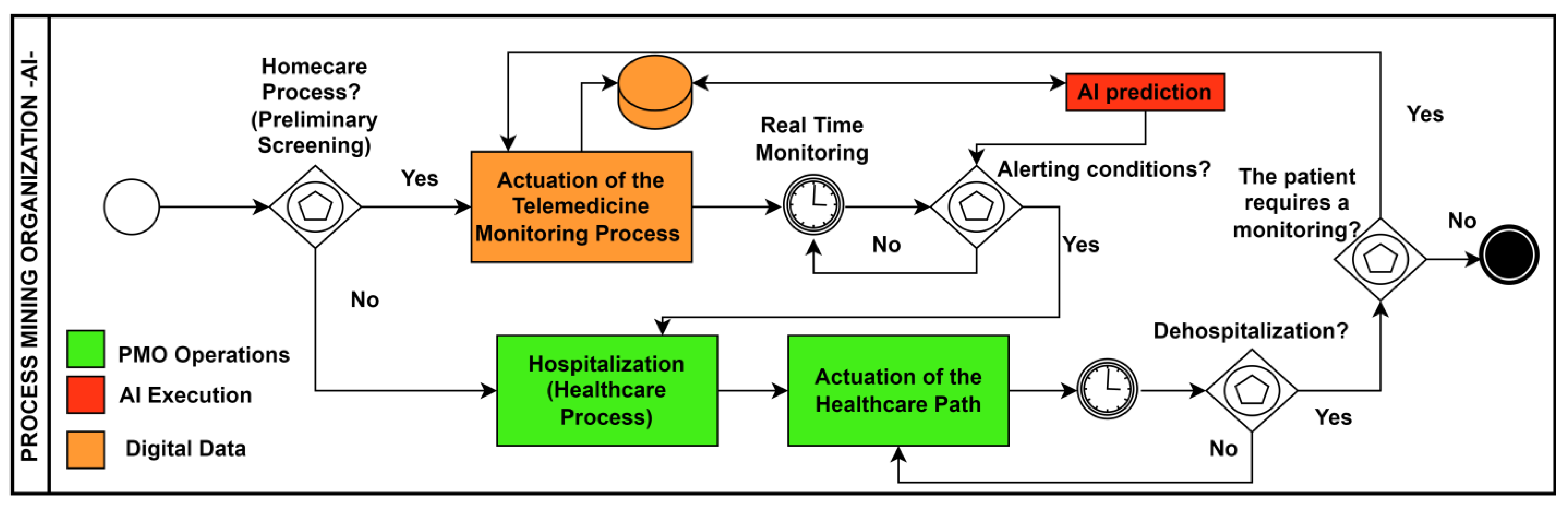
- Section 3.2 provides some examples of BPMN-PMO workflows in HR management to decrease the fall risk of patients and in telemedicine application fields;
- Section 4 provides guidelines for PMO design approach, including process monitoring aspects;
- Section 4 also discusses the advantages, disadvantages, and limits of the proposed theoretical workflows.
2. Materials and Methods
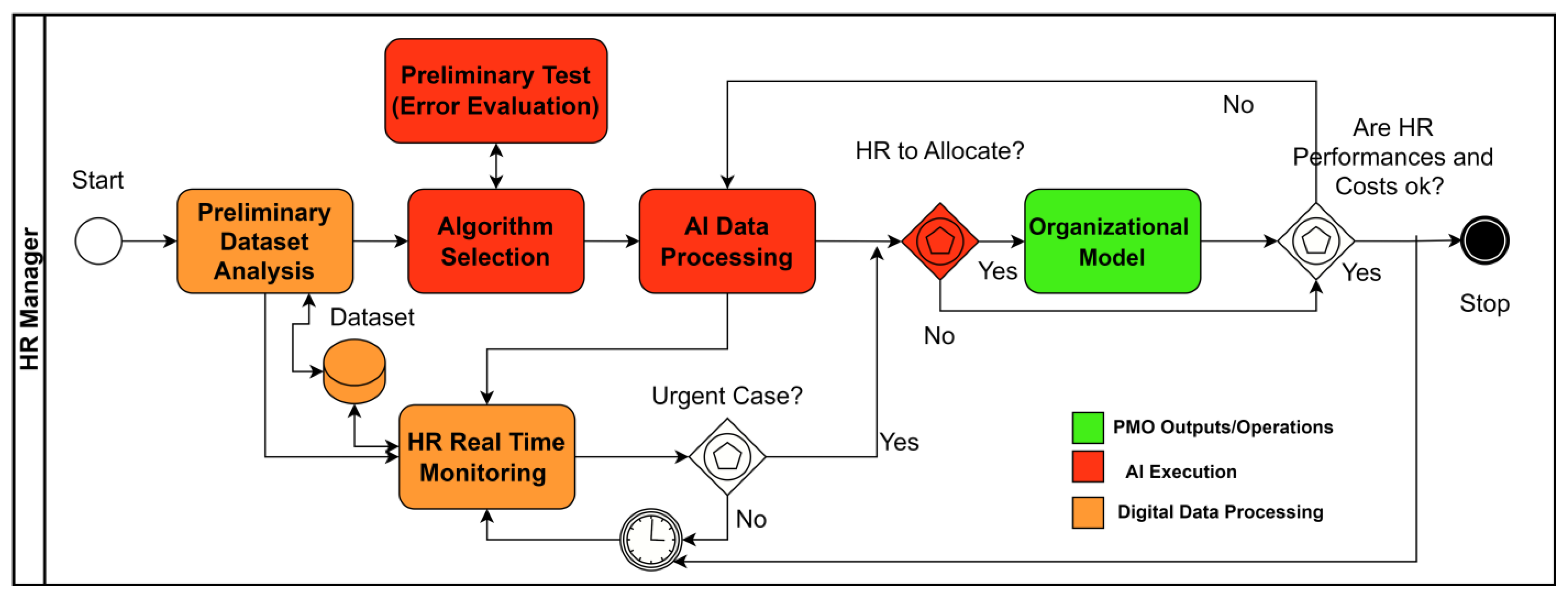
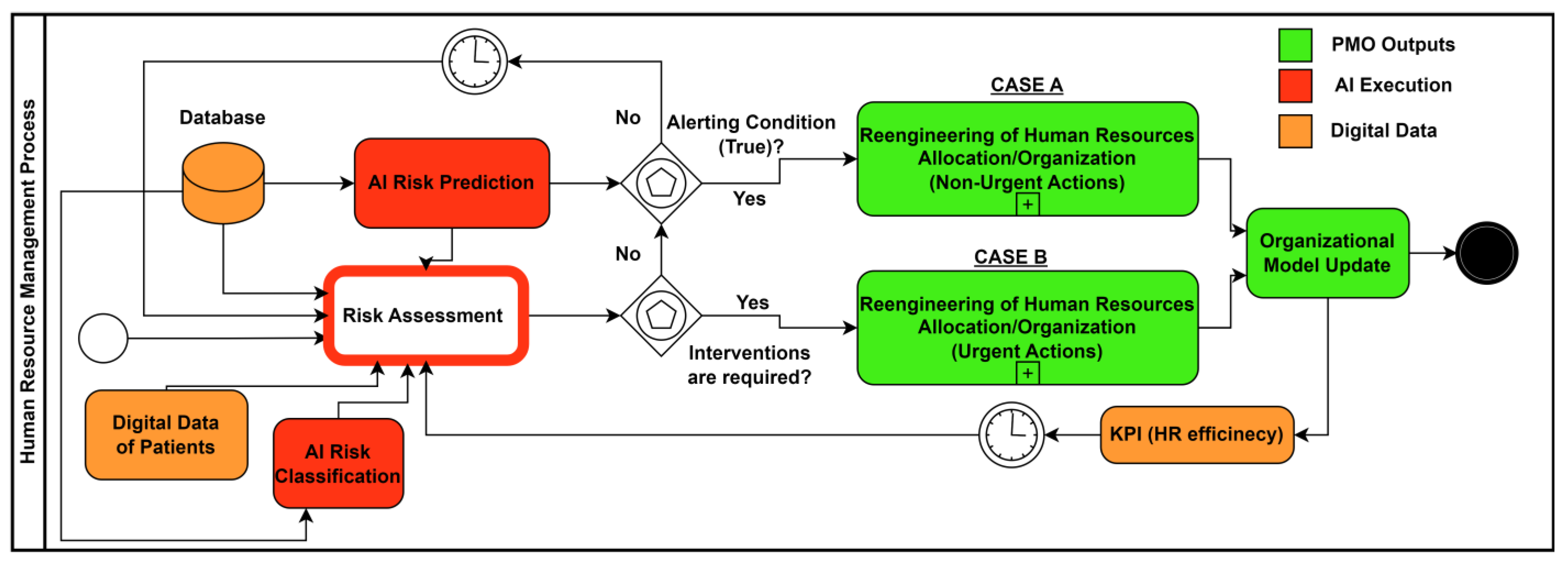
- Orange color, identifying digital sources and digital data (it represents the digital transformation of the healthcare institution);
- Red color, representing the AI decision-making engine (AI data prediction or AI data classification/clustering);
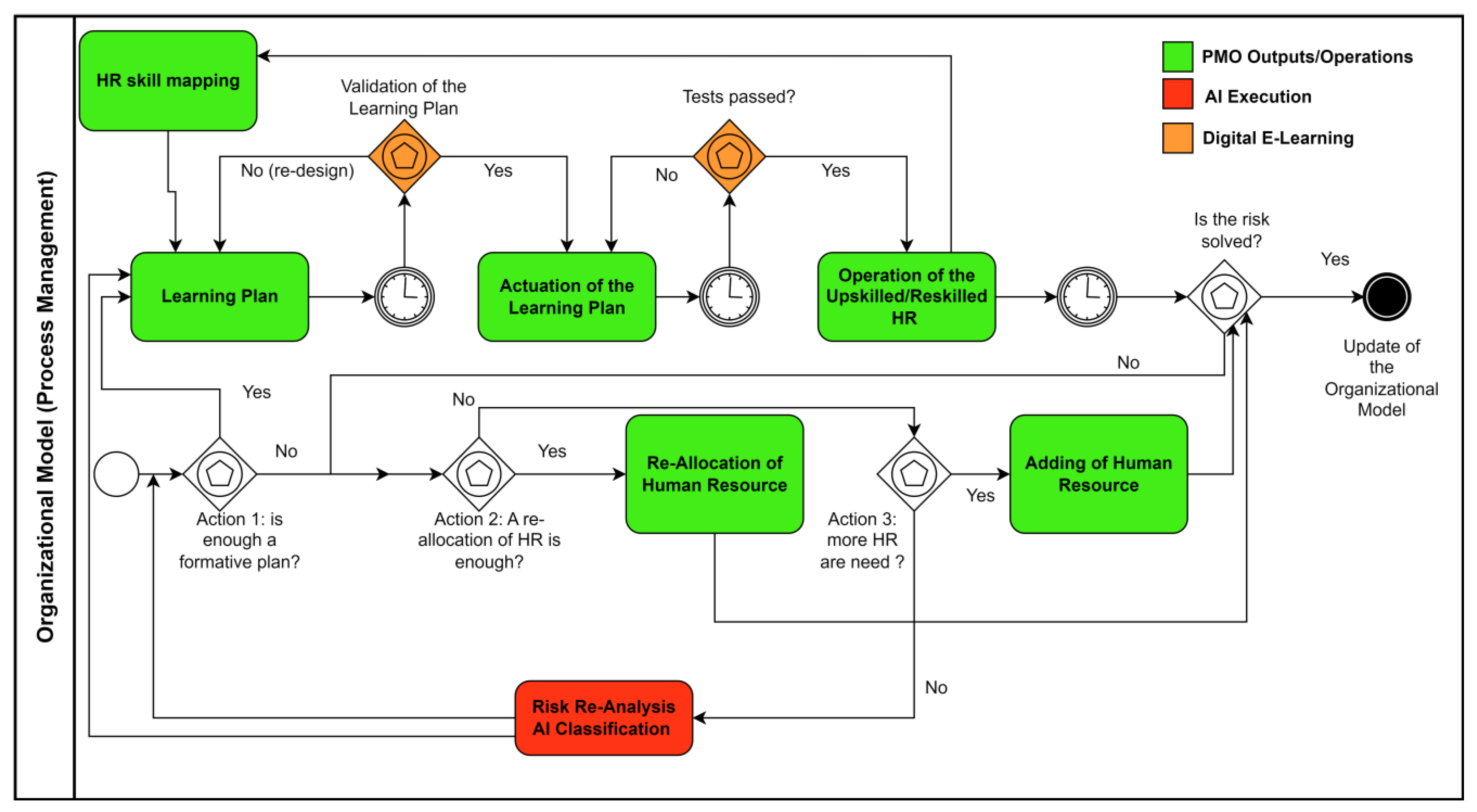
- Green color, indicating the PMO outputs or the HR organizational improved models (this color characterizes the organizational impact);
- White color (transparent), modeling the standards tasks or the graphical elements which are retained but are not so important in the design stage.
- Event symbols: “Start” (begin of a process); “end” (end of a process); “timer” (periodical evaluation of a part of the process’s workflow).
- Gateway symbols: “Exclusive” (logic condition selecting a subprocesses); “exclusive-event-based” (deep checkpoint improving decision-making actions).
3. Workflow Results: Design of PMO Healthcare Processes
3.1. HR Management through Data-Driven Approach
- Preliminary dataset analysis: The attributes of the analyzed dataset are selected based on the analysis to perform (in this phase, data cleaning and/or data filtering, preparing digital data for processing, can be executed).
- Algorithm selection: The selection of the AI algorithm depends on dataset typology (AI unsupervised algorithms are preferred for a dataset with a high number of attributes and that has difficulty finding the key attributes to extract more useful information; additionally, AI supervised algorithms are indicated when an significant attribute is to be supervised as a class to classify or to predict).
- The AI algorithm is executed, and the results are interpreted to find solutions about HR allocation, HR procedures to actuate, and, in general, to update the organizational model.
3.2. Application Field: Fall Risks and HR Management
- Action 1 (learning plan actuation in long periods): If necessary, a formative plan is enabled (training plan, execution of the plan, and test of nurse upskill/reskill) when it is found that the medical staff have no experience in preventing patients’ falls. The formation is important to know and for better application of the security procedures (Conley risk evaluation [24], actions to prevent risks, mechanical tools to add on beds, use of sensors and digital tools for patient monitoring, etc.).
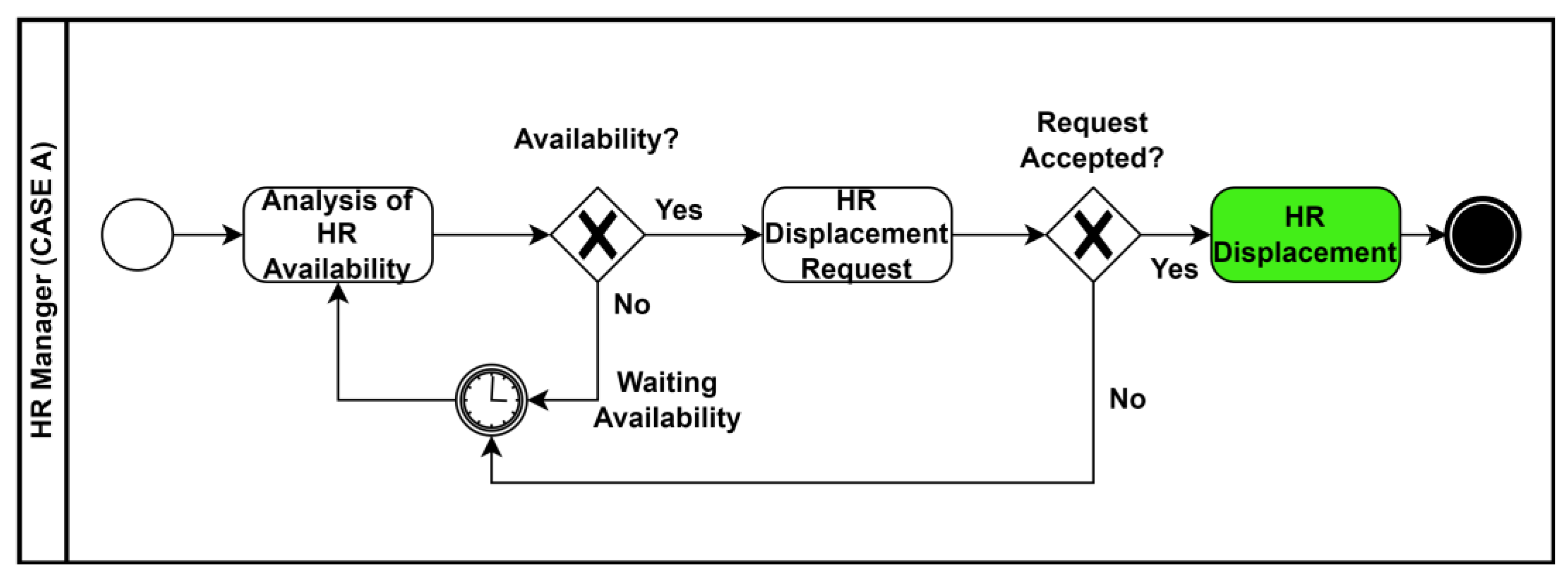
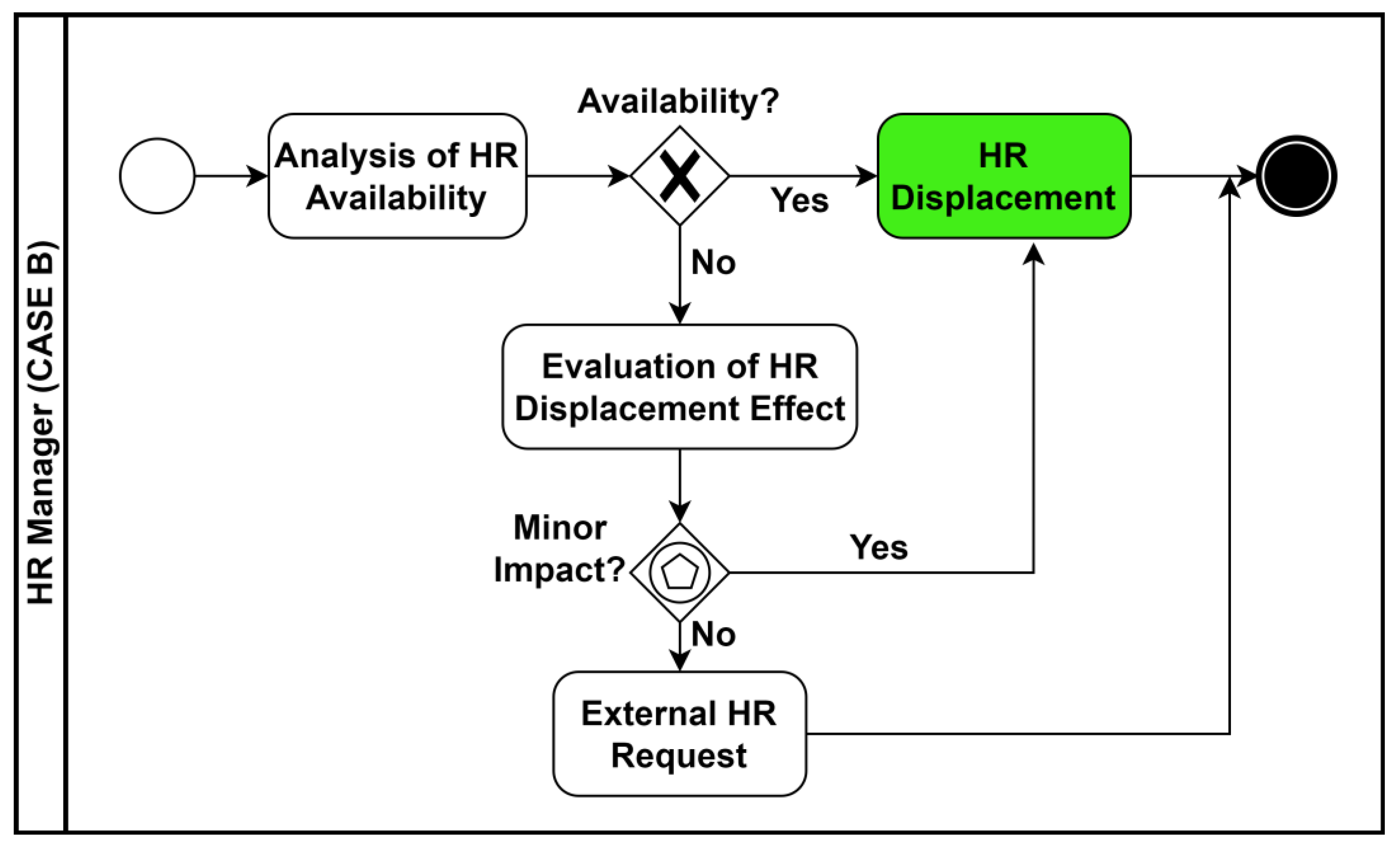
- Action 2 (HR displacement in short/medium period): If a formative plan is not enough, and if necessary, a reallocation of nurses is performed (allocation of nurses in specific rooms with patients with high risk, allocations of nurses in time slots characterized by a high fall probability, movement of nurses from other departments, etc.).
- Action 3 (HR addition in short/medium period): If it is not possible or not necessary to activate Action 1 or Action 2, a last solution is the addition of new skilled nurses but with an increase in costs of the hospitalization unit.
- Case A (nonurgent actions): The nonurgent actions are performed when alerting conditions estimated by the AI algorithm are found;
- Case B (urgent actions): The urgent actions are executed when a high risk is assessed.
3.3. Telemedicine Impacting Organizational Models
4. Discussion
- The actors of the systems and the number of pools were defined;
- The preliminary interviews to define the process were performed;
- The main tasks to highlight in the main process were defined and the whole BPMN workflow was simplified;
- The preliminary BPMN workflows were sketched;
- The workflow was simulated by considering all possible cases;
- The final BPMN workflow was optimized;
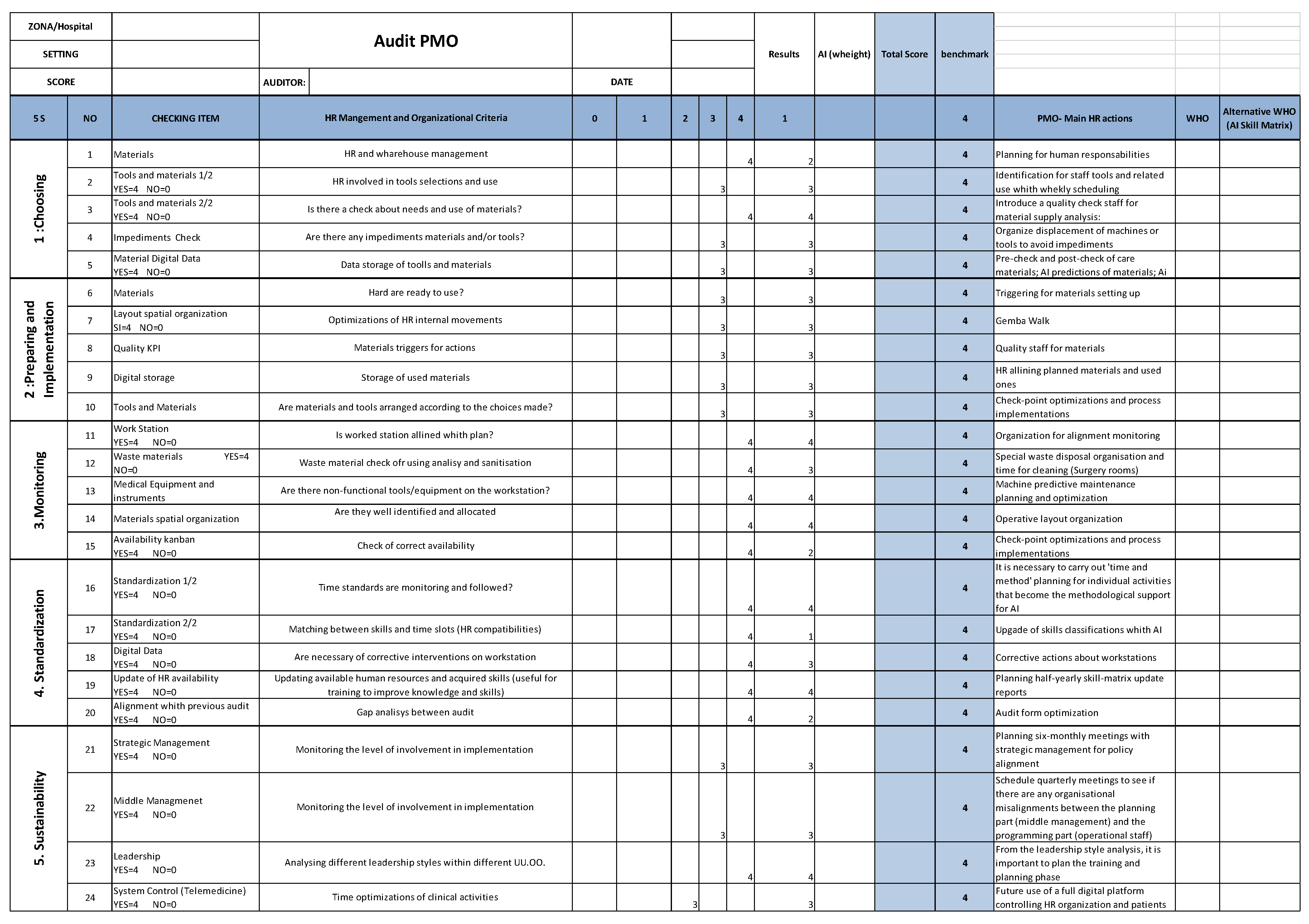
- An audit form was estimated to control the “TO BE” clinical processes (an example of the audit form is given in Appendix B).
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
- A: number of falls;
- B: number of falls that happened between 8 p.m. and 8 a.m.;
- C: number of falls that happened between 8 a.m. and 8 p.m.;
- D: number of performed computerized axial tomography (CAT) analyses;
- E: number of X-ray analyses;
- F: number of ultrasound analyses;
- G: number of external consulting;
- H: checked blunt injuries due to a fall;
- I: events related to major trauma;
- J: low-risk cases (0 < Conley index [20] < 1);
- K: high-risk cases (Conley index > 2).
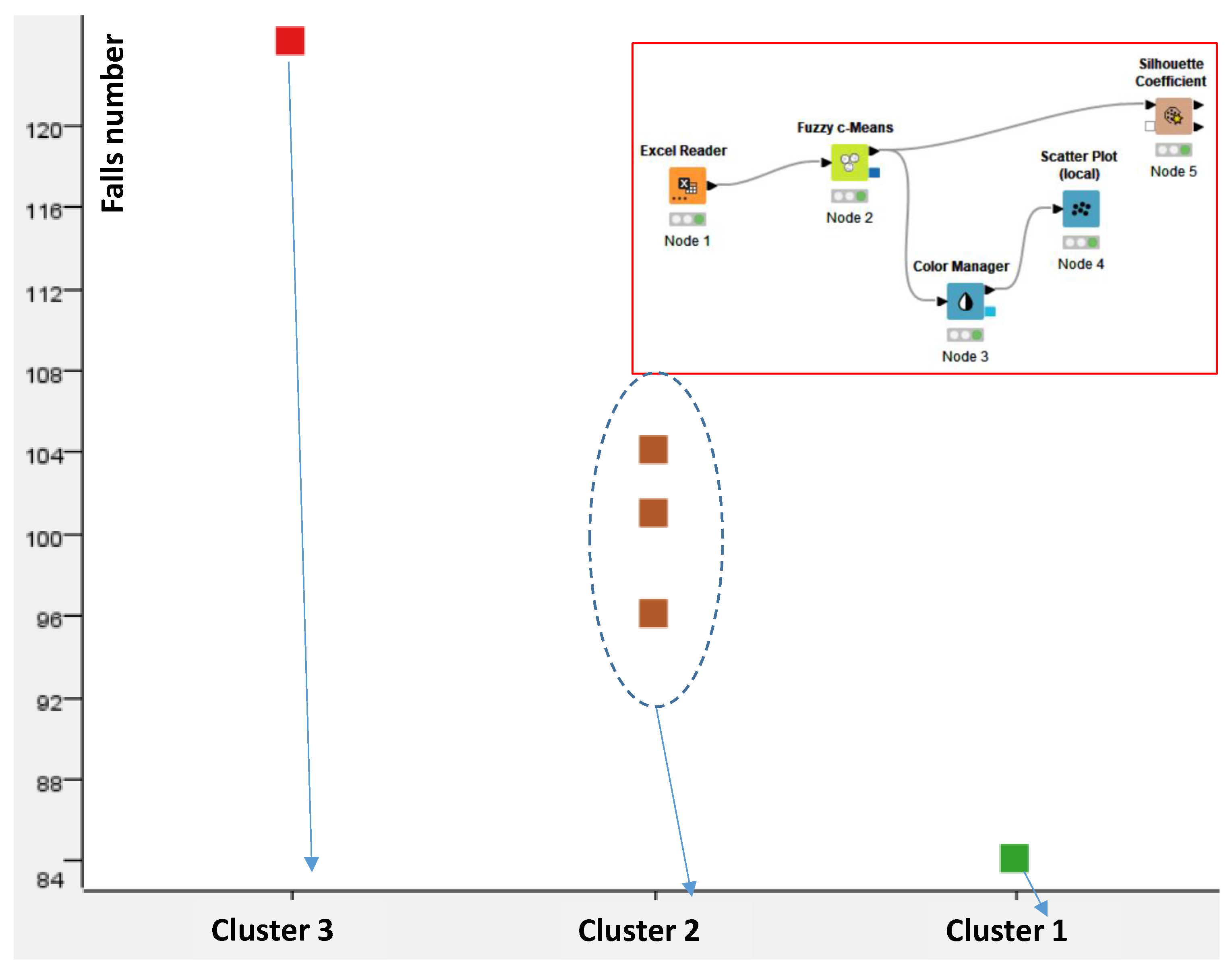
| Cluster | Cluster Features | PMO Outputs |
|---|---|---|
| Cluster 1 |
| Best cluster indicating the year 2020. No particular corrective actions are required. The medical stuff is more present in the time slot when the patient falls occur (low risk). |
| Cluster 2 |
| The years 2019, 2021, and 2022 appertain to this cluster (moderate risk).
|
| Cluster 3 |
| Worse cluster related to the year 2018. A specific action concerns the management of the clinical machines and their HR operators. |
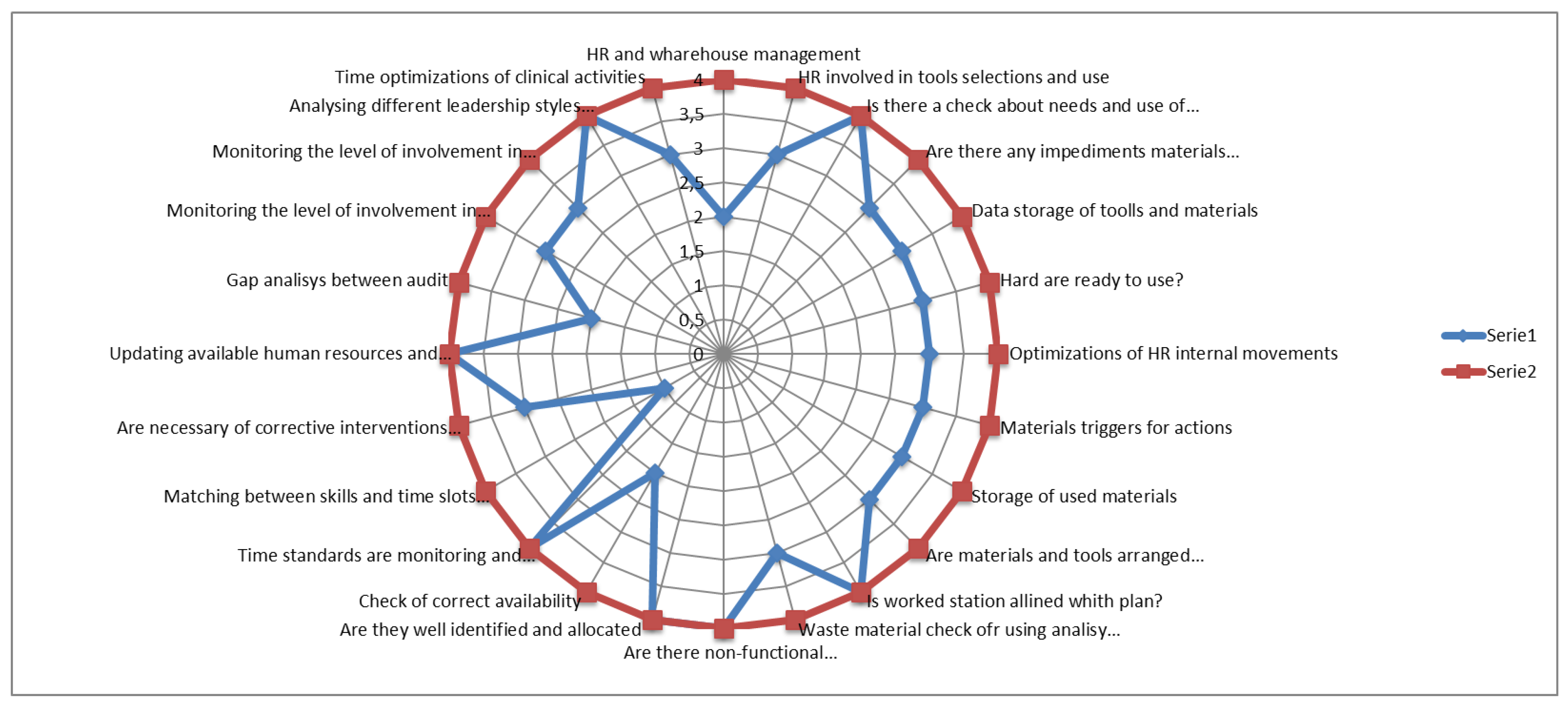
Appendix B. AI-Based Consulting Audit Framework
- Materials choosing;
- Preparing and implementation;
- Monitoring;
- Standardization;
- Sustainability.
References
- Alnamrouti, A.; Rjoub, H.; Ozgit, H. Do Strategic Human Resources and Artificial Intelligence Help to Make Organisations More Sustainable? Evidence from Non-Governmental Organisations. Sustainability 2022, 14, 7327. [Google Scholar] [CrossRef]
- Aydın, E.; Turan, M. An AI-Based Shortlisting Model for Sustainability of Human Resource Management. Sustainability 2023, 15, 2737. [Google Scholar] [CrossRef]
- Massaro, A. Advanced Control Systems in Industry 5.0 Enabling Process Mining. Sensors 2022, 22, 8677. [Google Scholar] [CrossRef]
- Tambotoh, J.; Prabowo, H.; Isa, S.M.; Pudjianto, B.W. Process mining in governance, risk management, compliance (grc), and auditing: A systematic literature review. J. Theor. Appl. Inf. Technol. 2021, 99, 4334–4344. [Google Scholar]
- Becker, M.; Buchkremer, R. A Practical Process Mining Approach for Compliance Management. J. Fin. Regul. Compliance 2019, 27, 464–478. [Google Scholar] [CrossRef]
- ISO/IEC 19150:2013. Available online: https://www.iso.org/standard/62652.html (accessed on 19 June 2023).
- Object Management Group Business Process Model and Notation. Available online: https://www.bpmn.org/ (accessed on 19 June 2023).
- Pufahl, L.; Zerbato, F.; Weber, B.; Weber, I. BPMN in Healthcare: Challenges and Best Practices. Inf. Syst. 2022, 107, 102013. [Google Scholar] [CrossRef]
- Ongoo, B.S.S.; Proudlove, N.C.; D’ Ambrogio, S.A.; Calabrese, A.; Bisogno, S.; Levialdi Ghiron, N. A BPMN Extension to Support Discrete-Event Simulation for Healthcare Applications: An Explicit Representation of Queues, Attributes and Data-Driven Decision Points. J. Oper. Res. Soc. 2018, 69, 788–802. [Google Scholar] [CrossRef]
- Russo, V.; Ciampi, M.; Esposito, M. A Business Process Model for Integrated Home Care. Procedia Comput. Sci. 2015, 63, 300–307. [Google Scholar] [CrossRef][Green Version]
- Singh, A.; Ravi, P. Lean Six-Sigma (LSS) Applications in Hospitals: A Decade (2011–2020) Bibliometric Analysis. Int. J. Product. Perform. Manag. 2022, 72, 2270–2291. [Google Scholar] [CrossRef]
- Rosa, A.; Massaro, A.; McDermott, O. Process Mining Applied to Lean Management Model Improving Decision Making in Healthcare Organizations. In Proceedings of the 18th International Forum on Knowledge Asset Dynamics, Matera, Italy, 7–9 June 2023; pp. 222–231, ISBN 978-88-96687-16-1. Available online: https://aran.library.nuigalway.ie/handle/10379/17801 (accessed on 19 June 2023).
- Massaro, A.; Maritati, V.; Savino, N.; Galiano, A.; Convertini, D.; De Fonte, E.; Di Muro, M. A Study of a Health Resources Management Platform Integrating Neural Networks and DSS Telemedicine for Homecare Assistance. Information 2018, 9, 176. [Google Scholar] [CrossRef]
- van Hee, K.M.; Sidorova, N.; van der Werf, J.M. Business Process Modeling Using Petri Nets. In Transactions on Petri Nets and Other Models of Concurrency VII; Springer: Berlin/Heidelberg, Germany, 2013; pp. 116–161. [Google Scholar]
- Bouafia, K.; Molnár, B. Hypergraph Application on Business Process Performance. Information 2021, 12, 370. [Google Scholar] [CrossRef]
- Stefanova-Pavlova, M.; Andonov, V.; Tasseva, V.; Gateva, A.; Stefanova, E. Generalized Nets in Medicine: An Example of Telemedicine for People with Diabetes. In Imprecision and Uncertainty in Information Representation and Processing; Springer International Publishing: Cham, Switzerland, 2016; pp. 327–357. [Google Scholar]
- Cazzato, G.; Massaro, A.; Colagrande, A.; Trilli, I.; Ingravallo, G.; Casatta, N.; Lupo, C.; Ronchi, A.; Franco, R.; Maiorano, E.; et al. Artificial Intelligence Applied to a First Screening of Naevoid Melanoma: A New Use of Fast Random Forest Algorithm in Dermatopathology. Curr. Oncol. 2023, 30, 6066–6078. [Google Scholar] [CrossRef]
- Hassan, M.M.; Tahir, M.H.; Ameeq, M.; Jamal, F.; Mendy, J.T.; Chesneau, C. Risk factors identification of COVID-19 patients with chronic obstructive pulmonary disease: A retrospective study in Punjab-Pakistan. Immun. Inflamm. Dis. 2023, 11, e981. [Google Scholar] [CrossRef] [PubMed]
- Ameeq, M.; Tahir, M.H.; Hassan, M.M.; Jamal, F.; Shafiq, S.; Mendy, J.T. A group acceptance sampling plan truncated life test for alpha power transformation inverted perks distribution based on quality control reliability. Cogent Eng. 2023, 10, 2224137. [Google Scholar] [CrossRef]
- Bantan, R.A.R.; Chesneau, C.; Jamal, F.; Elgarhy, M. On the Analysis of New COVID-19 Cases in Pakistan Using an Exponentiated Version of the M Family of Distributions. Mathematics 2020, 8, 953. [Google Scholar] [CrossRef]
- Muneeb Hassan, M.; Ameeq, M.; Jamal, F.; Tahir, M.H.; Mendy, J.T. Prevalence of covid-19 among patients with chronic obstructive pulmonary disease and tuberculosis. Ann. Med. 2023, 55, 285–291. [Google Scholar] [CrossRef]
- Hassan, M.M.; Ameeq, M.; Fatima, L.; Naz, S.; Sikandar, S.M.; Kargbo, A.; Abbas, S. Assessing socio-ecological factors on caesarean section and vaginal delivery: An extended perspective among women of South-Punjab, Pakistan. J. Psychosom. Obstet. Gynaecol. 2023, 44, 2252983. [Google Scholar] [CrossRef]
- Naeem, S.; Ali, A.; Qadri, S.; Khan Mashwani, W.; Tairan, N.; Shah, H.; Fayaz, M.; Jamal, F.; Chesneau, C.; Anam, S. Machine-Learning Based Hybrid-Feature Analysis for Liver Cancer Classification Using Fused (MR and CT) Images. Appl. Sci. 2020, 10, 3134. [Google Scholar] [CrossRef]
- Ali, A.; Qadri, S.; Khan Mashwani, W.; Kumam, W.; Kumam, P.; Naeem, S.; Goktas, A.; Jamal, F.; Chesneau, C.; Anam, S.; et al. Machine Learning Based Automated Segmentation and Hybrid Feature Analysis for Diabetic Retinopathy Classification Using Fundus Image. Entropy 2020, 22, 567. [Google Scholar] [CrossRef]
- Cazzato, G.; Massaro, A.; Colagrande, A.; Lettini, T.; Cicco, S.; Parente, P.; Nacchiero, E.; Lospalluti, L.; Cascardi, E.; Giudice, G.; et al. Dermatopathology of Malignant Melanoma in the Era of Artificial Intelligence: A Single Institutional Experience. Diagnostics 2022, 12, 1972. [Google Scholar] [CrossRef]
- Draw.io. Available online: https://www.drawio.com/ (accessed on 19 June 2023).
- Draw.io Releases Notes. Available online: https://github.com/jgraph/drawio-desktop/releases (accessed on 19 June 2023).
- Bhatti, D.M.S.; Saeed, N.; Nam, H. Fuzzy C-Means Clustering and Energy Efficient Cluster Head Selection for Cooperative Sensor Network. Sensors 2016, 16, 1459. [Google Scholar] [CrossRef]
- Oleka, C.J.; Aikhuele, D.O.; Omorogiuwa, E. Data-Driven Intelligent Model for the Classification, Identification, and Determination of Data Clusters and Defect Location in a Welded Joint. Processes 2022, 10, 1923. [Google Scholar] [CrossRef]
- KNIME. Available online: https://www.knime.com/ (accessed on 20 June 2023).
- Shutaywi, M.; Kachouie, N.N. Silhouette Analysis for Performance Evaluation in Machine Learning with Applications to Clustering. Entropy 2021, 23, 759. [Google Scholar] [CrossRef] [PubMed]
- Guzzo, A.S.; Meggiolaro, A.; Mannocci, A.; Tecca, M.; Salomone, I.; La Torre, G. Conley Scale: Assessment of a Fall Risk Prevention Tool in a General Hospital. J. Prev. Med. Hyg. 2015, 56, E77–E87. [Google Scholar]
- Elia, G.; Margherita, A.; Massaro, A.; Vacca, A. Adoption of Open Innovation in the COVID-19 Emergency: Developing a Process Based Information Coordination System. Bus. Process Manag. J. 2022, 28, 419–441. [Google Scholar] [CrossRef]
- Alauthman, M.; Al-qerem, A.; Sowan, B.; Alsarhan, A.; Eshtay, M.; Aldweesh, A.; Aslam, N. Enhancing Small Medical Dataset Classification Performance Using GAN. Informatics 2023, 10, 28. [Google Scholar] [CrossRef]
- Sinha, R.S.; Lee, S.-M.; Rim, M.; Hwang, S.-H. Data Augmentation Schemes for Deep Learning in an Indoor Positioning Application. Electronics 2019, 8, 554. [Google Scholar] [CrossRef]

| HR Intervention Typology | Goal | Possible Correlated Negative Impact | Action Guidelines |
|---|---|---|---|
| Training | Decrease in the health risk of the patient in hospitals. | Legal impact (compensation of patients in cases of inadequately trained personnel). | Reskill and upskill of the medical staff according to the specific risk to control. |
| HR allocation and displacement |
| Imbalances due to the movement of staff between different departments or different healthcare units. | Controlling of the staff displacement according to priorities and to real needs (use of the telemedicine supporting the medical staff management). |
| HR recruitment | Recruitment of new skilled medical staff, improving care services and clinical processes. | Increase in HR costs. | Recruitment is executed according to a preliminary analysis of needs and possible improvement in the care service quality. |
| Definition of new responsibilities and roles | Definition of new procedures and protocols by designating new staff roles or assigning new responsibilities. |
| Preliminary discussion with the whole staff about the new roles; design of the new protocols, comparing all HR opinions. |
| HR for control room (telemedicine applied to homecare assistance) | Designation of some of the medical staff to remotely monitor patients at home. | Adhesion of patients to wear medical sensors at home. | Implementation of the telemedicine platform according to privacy laws and linking electronic health records. |
| PMO Corrective Action | PMO Advantages | PMO Disadvantages |
|---|---|---|
| Training |
| Improvement in organizational process about training plan and execution (an initial mapping of the HR skills is required to optimize the training plan). |
| HR allocation and displacement |
| Possible increase in the management impact decreasing the efficiency of other departments/sections moving their staff (decrease in the care service quality). |
| Monitoring of task execution of HR | The HR traceability allows the estimation of KPIs regarding HR efficiency. | A major control of HR activities could generate fear in the staff, thus decreasing the care service efficiency. |
| PMO Limits | Description | PMO Perspectives |
|---|---|---|
| Implementation of the AI data-driven processes | The adoption of supervised and unsupervised AI algorithms for the execution of processes requires a high level of expertise in the field of AI and process engineering (a strong HR upskill is required and only few professional figures could work for an AI-based audit). | A future use of digital processes could enable specified automatisms, thus optimizing time delays and HR allocation responses of the hospitals. |
| Digital solution integration |
| Future use of a full digital platform controlling HR organization and patients (including telemedicine care services). |
| Digital dataset available | AI-supervised algorithms require a large number of digital data (optimization of learning model). Digital transformation processes of healthcare units are typically slow. | Advanced solutions such as big data tools (data collection and data fusion) and augmented data (creation of artificial dataset to increase the initial performance of the training models) are useful to improve the AI performance. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rosa, A.; Massaro, A. Process Mining Organization (PMO) Modeling and Healthcare Processes. Knowledge 2023, 3, 662-678. https://doi.org/10.3390/knowledge3040041
Rosa A, Massaro A. Process Mining Organization (PMO) Modeling and Healthcare Processes. Knowledge. 2023; 3(4):662-678. https://doi.org/10.3390/knowledge3040041
Chicago/Turabian StyleRosa, Angelo, and Alessandro Massaro. 2023. "Process Mining Organization (PMO) Modeling and Healthcare Processes" Knowledge 3, no. 4: 662-678. https://doi.org/10.3390/knowledge3040041
APA StyleRosa, A., & Massaro, A. (2023). Process Mining Organization (PMO) Modeling and Healthcare Processes. Knowledge, 3(4), 662-678. https://doi.org/10.3390/knowledge3040041







