Abstract
The burden of morbidity and mortality caused by sexually transmitted infections (STIs) has serious consequences on the quality of life of populations. Nowadays, despite numerous prevention campaigns, sexually transmitted infections have been on the rise in France for several years. It remains important to transmit the right information in order to better educate and support patients. Where then remains the problem, and how can we improve the involvement and awareness of the general population regarding the risks of these STIs? It is imperative to work upstream on the training of health professionals and students because they are the first interlocutors and the only ones to transmit the knowledge acquired during their initial training to the individuals concerned. The objective of this work is to identify the areas where health professionals and students do not yet have all the notions acquired via a multiple-choice questionnaire on the different STIs and their major characteristics. These results will contribute to the implementation of additional training at the Health Centers in France.
1. Introduction
Every day, more than 1 million people contract an STI worldwide, according to the WHO [1]. Despite the means of screening, early diagnosis, and available treatments, STIs remain a public health problem. There are more than 30 different bacteria, viruses, and parasites that can be transmitted through sexual contact. The most common sexually transmitted infections (STIs) include chlamydia, gonorrhea, and syphilis [1]. Other common STIs include human papillomavirus (HPV), herpes simplex virus (HSV), hepatitis A, hepatitis B, hepatitis C, and HIV, all having serious health consequences and complications, including cancer and infertility (Table 1). In France, diagnoses of bacterial sexually transmitted infections (STIs) have been on the rise since their resurgence in the late 1990s. Between 2014 and 2016, the number of early syphilis, gonorrhea, and lymphogranuloma venereum diagnoses increased significantly, especially among men who have sex with men. Heterosexuals also experienced an increase in syphilis and gonorrhea cases. Regular screening of patients and partners, followed by prompt treatment, remains crucial to interrupt STI transmission, especially in the context of expanded human immunodeficiency virus (HIV) prevention through biomedical prophylaxis [2]. Recent reports from the European Centre for Disease Prevention and Control (ECDC) also highlight a significant surge in reported cases of chlamydia, gonorrhea, and lymphogranuloma venereum (LGV) across 27 European Union/European Economic Area (EU/EEA) countries. This collective increase underscores the dynamic and challenging landscape of sexually transmitted infections (STIs). The rising numbers mirror the previously reported trend of increasing syphilis cases by the ECDC, indicating a decade-long escalation in STI rates across Europe, with the overall trajectory remaining upward. Specifically, gonorrhea cases continue to rise, surpassing pre-pandemic levels. Notably, men who have sex with men (MSM) constitute more than half of the reported cases [3].

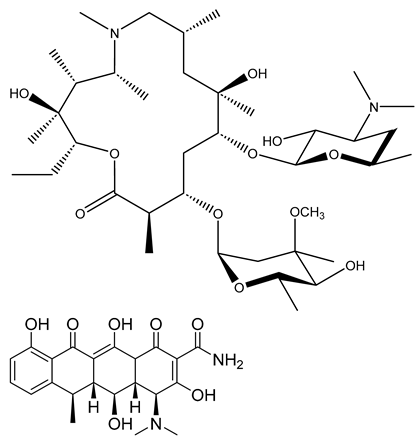
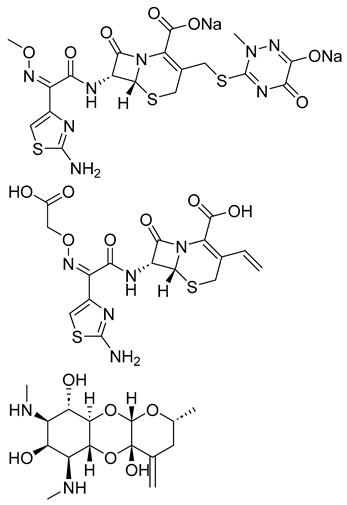
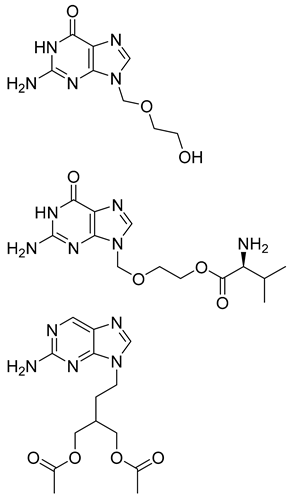
Table 1.
Major pathogens involved in STIs.
Today, HIV screening and treatment are experiencing much progress, but we must not forget all the other STIs, which are therefore constantly increasing in the number of cases each year. In view of the resurgence of these STIs, more and more resistance to antibiotics is being declared for bacterial STIs, and the therapeutic arsenal is therefore becoming less and less important, a very worrying fact for the years to come. For several of them, vaccines are not available, and for those for which there is a vaccine (HPV, hepatitis B, hepatitis A), vaccination coverage in France is insufficient (Table 2). It should also be noted that beyond the direct health risks, these pathologies have serious consequences on reproduction, such as the appearance of sterility and maternal–fetal transmissions, which can lead to malformations or death in utero. There is an increase in risky sexual behavior and a lack of knowledge of these pathologies, a phenomenon against which health professionals must act by providing the necessary information and by communicating more often and more easily on these subjects with their patients. International institutions seek to advance progress and reduce the figures that are still catastrophic nowadays compared to the means deployed [31]. It is important to identify the problem and improve the awareness of the general population regarding the risks of these STIs. The objective of this work was to evaluate the level of knowledge on this subject among health professionals and students in France. The evaluation was based on a multiple-choice questionnaire, aiming to identify the gaps in the knowledge on STIs for each health sector. The results of this survey highlighted the lack of knowledge in certain areas among health professionals and students. The results of this study will allow the state sexual health services to develop additional, comprehensive, and targeted training for each health profession on STIs as part of continuing personal development (CPD).

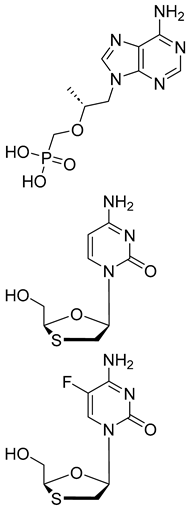
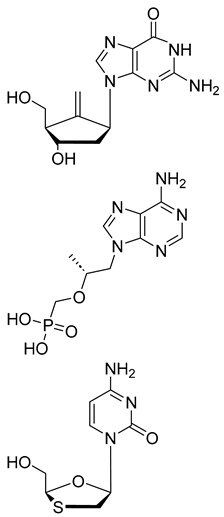
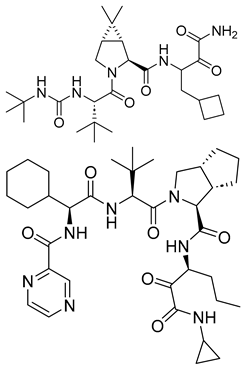
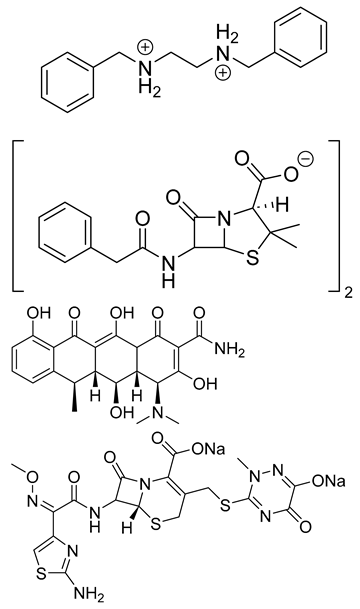
Table 2.
Available treatments for major STIs.
2. Materials and Methods
2.1. Choice of the Population Studied
This study focuses on knowledge of sexually transmitted infections among students and health professionals. We therefore distinguished two very distinct groups in this study: on the one hand, students from different schools or faculties of medical sciences and, on the other, active health professionals with more or fewer years of experience.
We chose the following areas to carry out this study: medicine, pharmacy, dentistry, midwifery, nursing, and physiotherapy. These fields of activity were chosen because these professions require knowledge of STIs to interact with their patients, and these professionals or future professionals received teaching on the subject during their initial training. Indeed, doctors, pharmacists, and midwives may be directly confronted with these pathologies during consultations or interviews with their patients, raising questions, making clinical observations, and making diagnostic or treatment choices. On the other hand, less concerned with monitoring these pathologies with the patient, surgeons and dentists are constantly confronted with a risk of AEB (Accidental Exposure to Biological Liquids) and must be up to date on the latest recommendations. The same goes for physiotherapists who have close contact with patients. We also chose to include pharmacy technicians in this questionnaire because they are at the counter like community pharmacists and are confronted with certain questions on the subject from a large number of patients.
2.2. Creation of the Questionnaire for Health Professionals and Students
The development of this survey questionnaire began in December 2018 and was completed in May 2019. It underwent multiple corrections so that it could be as exhaustive and as fair as possible, and it was designed in a way that prevented the interpretation of the questions in different ways. The free Google Forms platform was selected to carry out this online questionnaire.
We chose to treat several aspects of the nine main sexually transmitted infections.
The questionnaire was divided into several parts (Supplementary Table S1). The first focused on the professional profile of the individual but allowed anonymity to be respected. The second concerned generalities such as mandatory reporting and the origin of infections. Then, the third theme, the longest, directly questioned the different STIs: HIV, hepatitis (A, B, C), syphilis, papillomavirus, chlamydia infection, gonococcal infection, and herpes. Each STI was approached from different points: mode of transmission, clinic, diagnosis, treatment, and prevention.
Finally, the last part made it possible to assess the expectations and needs of professionals or students. It allowed them to determine if the training they have received so far seems sufficient to them and if they would be interested in additional training on the subject.
The last question, “did you seriously answer this questionnaire?” allowed us to understand the level of sincerity of the responses to the survey questionnaire.
We also chose to establish a scale to allow respondents to obtain a score as well as a detailed correction at the end of the questionnaire.
We chose multiple-choice questions in order to reduce the response time and make it more pleasant and less redundant for the respondents. On Google Forms, it was only possible to award a scale of 1 point per right or wrong answer. If the person only answered half of the question, then they would receive 0 points. This scale was put in place to motivate people to respond but also to allow them to obtain a detailed correction.
2.3. Validation
The survey questionnaire was scientifically validated during three multidisciplinary meetings by a group of sexology experts. This group of experts was made up of a sexologist pharmacist, a doctor specializing in infectious diseases, a sexologist nurse, and a sexologist midwife.
2.4. Distribution of the Survey Questionnaire
The estimated time to complete the online questionnaire was 20 min. The survey questionnaire was accessible online from 1 June to 20 September 2019, using the Google Forms tool.
Students were contacted via the social networks of groups of faculties or schools, as well as via the institutional student email box of their university. We estimate a large portion of student responses are due to social media.
Initially, an email was sent to each dean or director of the chosen areas of activity in order to diffuse the questionnaire to the students. Some structures responded favorably, sometimes depending on the schools of the given university, as in the case of the University of Lorraine (Nancy, France), where the faculties of medicine, the school of midwifery, and the school of nursing replied positively, contrary to the faculty of pharmacy.
Secondly, for professionals, an email was sent to each departmental and regional council of the orders of medicine, pharmacy, midwives, and dentistry in France. Few responded favorably, but some still distributed it, which made it possible to considerably increase the responses from professionals. We also contacted the regional unions of health professionals (URPS), representing self-employed health professionals according to their sector of activity, and some responded favorably to our request.
In addition, the questionnaire was also distributed via social networks to groups of health professionals.
Finally, the survey was distributed by email to several hospitals (CHRU Lille, CH Tourcoing, CHRU Nancy Brabois), health professionals’ groups (Totum pharmacy), or health structures and their associated groups (medical interns, pharmacy interns, etc.) on social networks.
Many structures did not respond or responded unfavorably for different reasons: replying to questionnaires was not in their missions, the structure was not concerned by the topic of this study, for respect to the private email boxes of health professionals, etc. Finally, 1211 responses were collected.
3. Results
3.1. Description of the Study Population
One thousand two hundred and eleven people responded to the survey. The gender distribution is 932 women (77%) and 277 men (22.8%). Two people did not answer the gender question (0.2%). This questionnaire was scored out of 50 points with a mean of 21.92, a median of 22, and a range from 0 to 41 points.
Excluded from this study were 82 people:
- -
- Forty responders were neither health professionals nor students.
- -
- Five responders were excluded because they did not answer this questionnaire seriously.
- -
- Twenty-five professionals not exercising a profession concerned by this study.
- -
- Ten students not completing a course concerned by this study.
- -
- One physiotherapy student who is the only one in his specialty to have responded to the survey questionnaire.
- -
- One pharmacy technician student who is the only one in his specialty to have responded to the survey questionnaire.
The results of this study, presented in this work, relate to 1129 responses. The most represented age group is 20–29 years old, with 548 responses. Student responders numbered 314 (27.8%), and health professionals numbered 815 (72.2%) (Supplementary Table S1).
3.2. Health Students
Among the 314 health students, the majority of responses came from students between the 3rd and 6th years of the university curriculum, with a majority of 15.6% of responding students from the 3rd to 5th year.
The majority of students responding were pharmacy students, with 118 responses (37.6%), 71 medical students (22.6%), 62 dental students (19.7%), 37 nursing students (11.8%), and 26 midwifery students (8.3%) (Table 3).

Table 3.
Percentage of correct answers among health students according to their socioprofessional category.
3.3. Health Professionals
Among the 815 professionals, the majority of responses came from professionals with less than 10 years of experience, with 454 (55.7%) responses.
Within these professionals, there are different health professions. Out of 815 professionals, 224 (27.5%) are medical doctors, 240 (29.4%) are pharmacists, 229 (28.1%) are midwives, 48 (5.9%) are nurses, 42 (5.2%) are pharmacy technicians, 22 (2.7%) are physiotherapists, and 10 (1.2%) are dentists (Table 4).

Table 4.
Percentage of correct answers among healthcare professionals according to their socioprofessional category (PH, physiotherapists; PT, pharmacy technicians).
4. Discussion
4.1. Reliability of Responses to the Survey Questionnaire
In this survey questionnaire, no random drawing was carried out to select the respondents. The respondents were random people wishing to participate in this study and evaluate themselves based on this multiple-choice questionnaire. The risk of duplicates could not be ruled out; it was impossible to check whether a person had responded several times. The questionnaire was distributed via many social networks and health communications channels and included as many health professionals and students as possible.
4.2. Age Group Distribution in the Responded Population
Among all respondents, there was a higher rate of women, with 77% (934), and only 23% (279) of men. Part of this imbalance can be explained by a greater number of women in medical, pharmaceutical, and paramedical studies.
More professionals responded, with 72.2% (815), compared to students 27.8% (314). This difference is perhaps explained by the distribution of questionnaires from June to September, during the term break period when student and institutional mailboxes are less consulted.
The most represented age groups are 20–29, with 48.5% (548), and 30–39, with 25.5% (288). In addition, the largest share of professionals is those with a rate of years of experience < 10 years. This could be explained by the fact that younger populations (students and health professionals) have more frequent access to social networks.
Among health professionals, medical doctors, pharmacists, and midwives are in the majority, with 224, 240, and 229 respondents, respectively. These are the professional groups that were the most responsive across France. These are also the professions most concerned by all the items covered in this questionnaire. Dentists and physiotherapists are fewer in number, with 10 and 22 respondents, respectively, but we chose to keep them so as not to completely exclude these professions from this study.
Among students, pharmacy students, medical students, and dentistry students are in the majority, with 118, 71, and 62 respondents, respectively. In the majority of the cases, the faculties of medicine and dentistry sent the questionnaire to student emails, and pharmacy students were contacted mostly via social networks. Physiotherapy students were excluded because there were too few of them.
4.3. Level of General Knowledge
When professionals and students were questioned about the notion of mandatory reporting of STIs, we obtained a very low overall success rate, with 10.1% (114) correct answers. Indeed, as many as 58.8% (668) believe that syphilis must be reported, even though it has not been subjected to mandatory reporting since 2000 in France. Hepatitis C is not a mandatory reporting STI, and yet, 44.3% (503) of health professionals or students consider it as such. For HIV, the results are reassuring because 84.3% (958) consider it to be a mandatory reporting disease. On the other hand, for hepatitis A and hepatitis B, which are also mandatory to report, the correct answers are close to 37% (420) for hepatitis A and 51.8% (588) for hepatitis B. More than 50% of all health professionals believe that syphilis is a mandatory reporting disease; they are therefore not outdated on this point. Only 12.9% of the medical doctors answered correctly concerning hepatitis A, hepatitis B, and HIV.
The students are not completely informed on the topic either because more than 30% of them believe syphilis to be a mandatory reporting STI.
In most European countries, there are established national guidelines for managing sexually transmitted infections (STIs), covering both diagnosis and treatment. These guidelines are more commonly followed at specialized STI care sites, such as STI clinics, dermatovenereology clinics, and dermatology clinics, compared to other healthcare settings where STIs are encountered. Interestingly, each country has its unique reporting requirements and guidelines. Despite the existing diversity in STI surveillance systems across Europe, similar priorities exist in different nations [61,62]. To enhance our understanding of STI epidemiology and the factors driving transmission across Europe, it is crucial to define standardized minimum datasets. Additionally, the use of sentinel and enhanced surveillance systems, alongside universal case and laboratory reporting data, would significantly contribute to effective public health responses. However, the current heterogeneity of surveillance systems complicates direct comparisons of STI incidence rates across the continent. The same issue is observed worldwide, including in Latin American countries, where HIV reporting is similar across the countries, but STI reporting is highly variable [63]. Urgently implementing standardized mandatory reporting and systems for detecting and monitoring localized outbreaks of acute bacterial STIs is essential.
The results concerning the identification of pathologies due to bacteria are 62.7%, which is an average among students and health professionals, with a clear identification of gonococcal infection (95.5%) and chlamydia infection (88.9%), but a lower rate for syphilis (72.7%). On these first two questions, it is clear that syphilis is a pathology that is not completely known in all its aspects by health professionals and students. This is surprising given its reemergence in the world today. Overall, on all questions, we noticed a better success rate among medical doctors, pharmacists, and midwives compared to other professions. This figure is still reassuring because these are the health professions that receive the most information on sexually transmitted infections in all their aspects.
On a global scale, this study reflects a general tendency in terms of STI knowledge. A study conducted among medical students in Bangladesh by Mahboob, N et al. [64] indicates a clear gap in the knowledge about STIs. Another study, targeting the evaluation of knowledge on STIs among healthcare providers in Laos also indicated misperceptions of STI causes, transmission, and symptoms [65]. A study by Folasayo et al. assessing the knowledge and preventive practices related to sexually transmitted infections among health university students in Malaysia equally indicates that knowledge on STIs is still lacking, and the risky behavior in sexual practice by students is alarming [66].
A particular category of individuals at risk of developing STIs are men who have sex with men. Indeed, although anyone who engages in sexual activity is susceptible to contracting sexually transmitted infections (STIs), sexually active gay, bisexual, and other men who have sex with men (MSM) face a heightened risk. MSM not only experience elevated rates of syphilis but also account for over half of all new HIV infections. Several factors contribute to the increased prevalence of STIs among MSM. These include higher rates of HIV and other STIs, which raise the likelihood of encountering an infected partner and acquiring an infection themselves. Additionally, specific behaviors—such as inconsistent condom use and engaging in anal sex—further amplify the risk of STI transmission. Unfortunately, stigma and discrimination can adversely impact the overall health of gay and bisexual men. Several studies align with existing evidence that sexually transmitted infections (STIs) are more prevalent among men who have sex with men (MSM). Additionally, the studies reveal that the bacterial STI burden is greater in MSM compared to non-MSM males, emphasizing the need for tailored healthcare services for MSM. STI prevalence among MSM also seem to remain relatively stable over time [67]. Men who have sex with men (MSM) and participate in unprotected anal intercourse with casual partners face a significant risk of contracting sexually transmitted infections (STIs). However, reliable epidemiological data on this topic are limited. The overall findings indicate that the incidence rates of various STIs are notably high among MSM engaging in high-risk sexual behavior. Of particular concern are the elevated rates of gonorrhea, chlamydia, and hepatitis C infections observed. This specific subgroup of MSM would benefit from frequent access to STI testing, treatment, and follow-up [68].
4.4. Level of Knowledge on HIV
Several questions were asked about HIV infections. Health professionals and students were assessed on their knowledge regarding transmission, clinic, diagnosis, treatment, and prevention. It appears that, overall, knowledge about HIV is quite solid. Indeed, both health professionals and students agree on transmission through unprotected sexual intercourse and through blood for HIV, with 99.6% and 99.5% positive replies, respectively. The rate of correct answers for maternal–fetal transmission is a little lower at 84.3%. There is no significant difference between the different trades. The enzyme-linked immunosorbent assay (ELISA) blood screening test, coupled with the Western blot confirmation test, are analytical assays well known to French health professionals and students (84.5%), according to the survey results. It seems certain that HIV is a non-curable viral infection, with only 1.8% of responses to the item “can cure the infected person”. We note lower success rates among pharmacy technicians (52%) and physiotherapists (50%), as well as among nursing students on this item. The current guidelines for HIV diagnosis mandate a follow-up Western blot (WB) after a positive ELISA test. Detecting anti-HIV antibodies during acute infection usually takes three to six weeks due to the window [69]. The CDC diagnostic algorithm suggests using the HIV-EIA test, capable of detecting both antibodies and p24 antigen [70], thereby shortening the window period to two weeks after infection [71].
However, certain points still need to be improved. Indeed, the possible clinical manifestations remain uncertain for professionals and students. Among the correct answers, flu-like syndrome with fever (75.7%) and skin rash (60.1%) are the best known. Diarrhea (44.9%), shingles (43.5%), and tuberculosis (42.4%) are less well-known harbingers of HIV infection. The asymptomatic nature of the disease, although very common, was selected by 59.9% of the participants.
Among professionals, only 17.4% of respondents correctly selected all the clinical signs, and among students, only 15.6% replied accurately. Less than half of the medical doctors and medical students, the two groups most concerned by the clinical practice, answered this question correctly, with 42.4% and 45.1% correct responses, respectively. Prevention also seems to be a point to be explored further during training: the use of condoms (99.8%) and the use of sterile equipment when injecting drugs (93.7%) seem to be well-acquired knowledge. However, when it comes to post-exposure prophylaxis (PEP) within 48 h after recent possible exposure to HIV, or pre-exposure prophylaxis (PrEP), knowledge is frailer, with, respectively, 67.9% and only 44.7% success rates on these question items.
Among professionals, 33.1% answered this question correctly, and among students, 26.4%. Only half of the medical, pharmacy, and midwifery students selected PrEP as HIV prevention. Among professionals, only 31% of the midwives selected PrEP as a correct answer. It is noteworthy that PrEP is now a treatment that exists and affects all professions because it is prescribed, delivered in pharmacies, used by a large number of the population, and has allowed real progress in reducing the transmission of the virus. Nowadays, it seems surprising that only half of health professionals and students define this treatment as prevention.
4.5. Level of Knowledge on Hepatitis A
Several questions were asked about hepatitis A. Health professionals and students were assessed on their knowledge regarding transmission, clinic, diagnosis, treatment, and progression of the pathology. Globally, there is a gap in the knowledge of hepatitis A in the case of health professionals and health sciences students. Indeed, 82% of respondents replied that hepatitis A is transmitted through feces. Only 56% of them make the connection between feces and oral–anal sexual practices, which makes hepatitis A a sexually transmitted infection. In addition, 29% believe that hepatitis A is transmitted through blood, and 21.1% connected the transmission to injection drug use, which is not the case. Among professionals, the success rate for the question does not exceed 30%, and nurses, physiotherapists, and midwives do not exceed 20%. Among students, the success rate is around 30%, except for medical students, who obtain a rate of 50%. Nowadays, it is essential to consider hepatitis A as a sexually transmitted infection in view of increasingly widespread anal sex practices, and the mode of transmission should be known to all health professionals. The clinical manifestations are poorly known (15%), at least not in their entirety, as is the asymptomatic nature of the disease (22.9%). The screening technique is known by 96%, as far as the blood test is concerned. Conversely, for the possible developments of hepatitis A, knowledge is meager (24%). Close to 72% replied that a spontaneous recovery is possible in hepatitis A, whereas for 60.5%, fulminant hepatitis is an option, which are the correct answers for the outcomes of hepatitis A infection. However, a third of the respondents consider that hepatitis A infection can progress towards chronic hepatitis, liver cancer, and cirrhosis and that it can be cured with antiviral treatment, which is false. There is a significant difference among health professionals, notably between medical doctors, showing a success rate of 52.7%, and other health professions which do not exceed 20% of correct answers. Of note, among the nursing students, none gave the correct answer. Finally, for vaccination, we observe good success rates, indicating that professionals and students are aware of existing vaccines. On the other hand, for hepatitis A, only 40% of nursing and dental students know that the hepatitis A vaccine is available. In total, 74.3% of health professionals and students are aware of the existence of the vaccine, which is surprisingly low. Therefore, hepatitis A remains a pathology that seems very little developed in terms of teaching, given the overall results of the questionnaire. The hepatitis A infection seems a little clearer for medical students, but nevertheless, it is not completely acquired. All professions concerned by this study seem to need additional training on the subject.
4.6. Level of Knowledge on Hepatitis B
Overall, and as for all hepatitis infections in this survey, knowledge remains meager for hepatitis B. Regarding transmission, it seems very clear for all the participants that hepatitis B is transmitted through unprotected sexual intercourse (90.8%), through blood (97.1%), and consequently, through injection drug use (79.6%). However, only 25.1% of health professionals and students believe that hepatitis B can be transmitted through saliva, even though it is a means of transmission (e.g., bites) because even at a low concentration, it allows the transmission of the virus, particularly during the acute infection. Less than a third of each health profession knows that the virus can be transmitted by saliva, except dentists (50%), perhaps more informed given the constant contact with saliva in their professional practice. Among students, less than 20% consider saliva as a transmission way, except dental students, with a 48.7% success rate for the question. The clinical manifestations are known, but not entirely. Respondents correctly selected some, but not all symptoms. The asymptomatic nature of the disease is known to 34.9% only. No dentist or pharmacy technician gave a correct answer. Medical doctors had a success rate of 47.3%, even though they should be able to cite all the symptoms. Pharmacists present 7.5% of correct answers, a score far too low for a health professional supposedly familiar with the clinical aspects of the disease.
Concerning hepatitis B screening, the blood test seems to be practically unanimously well known, with 95.3% correct responses. When questioned about the evolution of hepatitis B, health professionals and students show diversity in knowledge. Close to 94% agree that chronic hepatitis is an outcome of hepatitis B. This is followed by cirrhosis and cancer, with 73.1 and 75.9%, respectively. Knowledge is much scarcer regarding spontaneous healing, with only 43.2% of the correct answers. In addition, 52.6% believe that hepatitis B can be cured with antivirals, whereas there is no curative treatment for this disease. The scores are low among students, with only an 11.3% success rate among medical students, 11% among pharmacy students, and 11.5% among midwifery students. Among professionals, no dentist, nurse, or physiotherapist gave a correct answer on the evolution of hepatitis B. Medical doctors had a success rate of only 17% concerning the evolution of the pathology, and pharmacists obtained only 5% of correct answers. Notwithstanding, these professions are supposed to be familiar with the evolution of hepatitis B. Finally, concerning vaccination, almost all the participants (97.7%) replied correctly to the question on the existence of a vaccine against hepatitis B. Additional training might then be necessary for health professionals, notably on the mode of transmission, particularly for saliva, as well as on the clinic, and on the evolution of hepatitis B.
4.7. Level of Knowledge on Hepatitis C
As with hepatitis A and B, knowledge remains to be deepened on hepatitis C, particularly on transmission modes. Indeed, contrary to hepatitis B, hepatitis C is transmitted only through blood and not through biological fluids, such as semen and vaginal secretions. However, 77.8% of the health professionals and students answered that the virus can be transmitted by unprotected sexual intercourse. The possibility of traumatic sexual intercourse, associated with bleeding can, of course, be considered, but this option was not specified in the item question. Nevertheless, the majority of the respondents agree on transmission through blood, with 95.1% and 80.8% of correct answers, respectively. Among professionals, less than 20% of all professions answered the question correctly by selecting only blood transmission and injection drug use. Among students, we do not exceed 12% correct answers for all health sectors. The clinical manifestations are known but not entirely, as respondents correctly selected some but not all symptoms. The asymptomatic nature of the disease seems known to only 37.1% of all the participants. Medical doctors and medical students seem more successful in the hepatitis A clinic-related questions, with 56.7% of correct answers. The rest of the health professions did not exceed a 20% success rate. Concerning viral detection, the blood test seems to be well known, with 96.3% of correct answers. When questioned about the outcomes of hepatitis C, there are still uncertainties: for 89.6% of respondents, it is clear that hepatitis C can evolve into chronic hepatitis. On the other hand, only 35.4% know that spontaneous recovery is a possibility, and 58.9% know that hepatitis C currently has a curative treatment [72].
Liver cancers and cirrhosis are selected at 72.7% and 73.9%, respectively, whereas these are still the main complications for hepatitis C which should be well known. In addition, 55.7% believe that hepatitis C can lead to fulminant hepatitis, even though this scenario is highly controversial in the scientific literature [73]. Among professionals, no dentist, nurse, or physiotherapist gave a correct answer. Medical doctors had a score of 15% correct answers, whereas pharmacists and midwives did not exceed 5%. Hepatitis C is a sexually transmitted infection that has existed for years and is common throughout the world. It seems unlikely that among the entire panel of health professionals and students, so few are fully aware of the possible developments of the disease (6.5%).
Finally, concerning vaccination, the global score is 88% of negative answers regarding the existence of a vaccine against hepatitis C.
4.8. Level of Knowledge on Syphilis
Syphilis leaves quite many gaps among French health professionals and students. They almost unanimously agree that transmission occurs through unprotected sexual intercourse (99.6%). However, 80% believe that transmission occurs through penile–oral sexual contact. In addition, 56.2% replied that transmission can occur through skin or mucosal contact. It is noteworthy that transmission during oral practices is a fairly significant possibility, whereas transmission through blood is almost non-existent [16]. In terms of clinical manifestations, some symptoms are known but not entirely, with 4.2% correct answers. Respondents agree on the appearance of a chancre at 90.9%, and the skin rash also stands out at 70.9%. On the other hand, hearing disorders, characteristic as a complication of syphilis, are only known by 27.6%, digestive disorders by 20.4%, and the very common asymptomatic nature of the disease is known by only 20.7% of the respondents. No pharmacy technician student or nursing student gave a correct answer to these questions. Among professionals, only 9.8% of the medical doctors were able to identify the clinical symptoms of syphilis. For syphilis screening, 84% of the health professionals and students selected the blood test as an answer. However, 13.8% selected a urine test as a syphilis detection method, whereas it is a chlamydia and gonococcal screening test. Concerning the questions about the evolution of syphilis, the correct replies are deceivingly low in number (7.2%). The maximum number of positive responses are in favor of possible recontamination after recovery, with 68.3% correct replies, and dementia, with a 60% success rate. However, half of the health professionals and students believe that heart complications occur in the evolution of syphilis. A significant number of respondents (48%) also consider that renal complications are part of the evolution of syphilis, which is in fact a very uncommon and rare feature. The clinic and its complications in syphilis seem to be also relatively unknown points in the health sector despite basic training. Thus, medical doctors do not exceed a 13% success rate for the question, and other professionals do not exceed 5% of correct answers. Among medical students and midwifery students, the results are similar, with only 18.3% and 11.5% of correct answers, respectively. The other respondents did not exceed 10% of correct answers.
Conversely, concerning the existence of a vaccine, the score of 98.2% correct answers goes in favor of its non-existence to date. Overall, syphilis remains a generally known disease, but few health professionals seem to have complete control over all aspects of the disease.
4.9. Level of Knowledge on Papillomavirus
Concerning the notion of transmission of the human papillomavirus (HPV), respondents agree on transmission through unprotected sexual intercourse at 98.8%; for penile–oral sexual contact, the score is 66.9%, and for skin contact, 58.1% correct answers. However, these last two means of transmission are essential, especially in the case of HPV, which can be transmitted with a certain risk, even when using a condom [17]. Overall, medical students are at 64.8% of correct answers, but for the students of the other health sectors, the correct replies do not exceed 50% success on the HPV questions. The same observation applies to health professionals, where the success rate did not exceed 60%, with more than 60% of the HPV clinical manifestations being known. For diagnosis, we still note that 17.2% of health professionals believe that the HPV diagnostic test is blood, whereas in reality, it is based on a biopsy/smear.
Only 58.1% of the interviewed health professionals know that HPV can lead to cancer, even though it is one of the frequent developments of the pathology. Almost one quarter (23.6%) believe that the papillomavirus can be eradicated thanks to antivirals, which is false.
Only half of the medical doctors are familiar with all the outcomes of HPV infection, compared to 25% of the pharmacists, whereas 73% of the medical students seem to be aware of the complications, and in other sectors, this knowledge does not exceed 24%.
The notion of the existence of the HPV vaccine is well known to health professionals and students.
4.10. Level of Knowledge on Chlamydia Infection
On the questions about chlamydia transmission, 60% of the respondents agree on unprotected sexual intercourse, penile–oral sexual contact, and skin contact. However, 9.5% believe that transmission through urine is possible, so it could be assumed that there is confusion with the urine screening test. More than 20% of nurses think that chlamydia is transmitted through saliva and urine. Penile–oral sexual contact and mucosal contact bear high-risk means of transmission, yet health professionals obtain only 60% of the correct response rate. The overall rate of correct answers is worrying because no health profession exceeds the threshold of 35%. The situation is similar in the case of health students, where the success rate did not exceed 50%. It is noteworthy that only 36% of the overall interviewed population know that chlamydia infection can be asymptomatic. Almost half of the interviewees replied that anal pain and anal pruritus can be observed in chlamydia infection.
The screening approaches are not sufficiently well known to French health professionals and students. Indeed, there are multiple means of screening: a urine test, a swab, or a vaginal sample, with a follow up of the infection by PCR. Among the respondents, 89.2% are in favor of vaginal sampling, whereas only 43.2% selected the urine test, which is in fact the reference test in the diagnosis of chlamydia. Very few students, less than 17%, are familiar with the three screening methods. More than 30% of medical doctors and pharmacists believe that screening for chlamydia is done by blood test, which is an error since chlamydia is not detected with blood tests.
Possible reinfection after treatment and recovery is a complication less well known to respondents, with 69% of this item selected correctly. The non-existence of the chlamydia vaccine is a notion familiar to more than 99% of the interviewed. Consequently, it is clear that the modes of transmission, as well as the means of screening, are still poorly understood by French health professionals and students. At a time of chlamydia infections growing at staggering rates and rapidly transmitting through oral sex, it is imperative that health professionals alert patients to the potential risks.
4.11. Level of Knowledge on Gonococcal Infection
As in the case of chlamydia, respondents agree that more than 60% of unprotected sexual intercourse, penile–oral sexual contact, and skin contact are a means of transmission of gonococcal infection. However, 10.7% believe that transmission is through urine or blood, whereas the bacteria circulate in biological fluids such as semen and vaginal secretions. In the case of gonococcal infection, penile–oral sexual contact and mucosal contact are the transmission means that should be known by all health professionals, as they are associated with high risk. Similar to the results obtained for chlamydia, the rate of correct answers for gonococcal infection among health professionals is problematic because no health profession exceeded the threshold of 30% correct answers, except medical doctors with 45.5%, which remains low. Likewise, health students did not exceed 50% of correct answers. Barely 50% of the midwives responded that gonorrhea could be transmitted through oral sex, compared to 37.5% of nurses. No physiotherapy, dentistry, or nursing student knew how to recognize the clinical manifestations of gonococcus. Of note, only 23.7% of the overall study population knew that gonococcal infection can be asymptomatic.
The screening methods are not sufficiently well known by French health professionals and students either. The means of screening remain the same as for chlamydia—a urine test, a swab, or a vaginal sample. The majority (81.8%) are in favor of vaginal sampling, whereas only 39.6% selected the urine test as the correct answer, despite the fact that it remains the reference test in the diagnosis of gonococcal infection. Very few health students and professionals, 17.4% and 15.6%, respectively, knew the three different screening methods. Only one dentist, one nurse, one pharmacy technician, as well as six midwifery and nursing students, gave the correct answer about the screening methods, a worrying figure when we know that this is part of their initial training.
Possible reinfection with gonococci, after treatment and cure, is also a complication less well known to the respondents, with 68.2% of this question item selected correctly. Of note, barely more than half of the respondents selected sterility as a complication of gonococcal infection, a well-known complication of the pathology. No health professional exceeded a 50% success rate in terms of knowledge of possible complications in gonococcal infection. The non-existence of a vaccine is a notion familiar to more than 98.2% of the interviewees. Consequently, it is clear that the modes of transmission, as well as the means of screening, are still poorly understood by French health professionals and students.
4.12. Level of Knowledge on Herpes Infections
Overall, the means of transmission of genital herpes are well known to health professionals and students, with a score of more than 80% correct responses indicating unprotected sexual intercourse, penile–oral sexual contact, kissing, and skin or mucous contact as main transmission modes. In fact, more than 50% of all healthcare professionals selected all the correct items. The results are similar for health students, with a correct answer rate of 72.3%. Curiously, 23.5% of respondents think that herpes can be asymptomatic when this is not the case.
Only 25.5% of students are familiar with all the possible clinical manifestations of herpes, compared to 22.3% of health professionals. Some symptoms, such as edema or rash, or even fever, are often forgotten.
Concerning genital herpes screening, 90% of respondents agree on a diagnosis by swab. However, more than 40% of them still believe that genital herpes is first detected through the blood, which is a somewhat high figure for health professionals and students.
Unfortunately, 39.5% of health professionals and students believe that herpes can be cured with antivirals, even though there is no curative treatment, and the existing antiviral treatments used during the flare-up do not prevent the recurrences. It should be noted that less than 50% of the same interviewed population is familiar with all the possible complications of genital herpes infection. The non-existence of a genital herpes vaccine is a notion familiar to more than 96.5%.
Thus, the knowledge of genital herpes infection is generally well acquired, apart from screening methods and the clinical complications, two points that remain still unclear.
5. Strengths and Limitations
This study provided important information on the knowledge of French health professionals and students on major circulating STIs with the objective of improving STI healthcare ability. The advantage of this study is based on the quantitative method, allowing the collection of data providing valuable insights and in-depth understanding of the know-how, the education system, and the need for additional training of French health professionals in terms of STI management. It is also the first nationwide survey that recruited over 1100 replies from health professionals and students from different professional horizons and French provinces. One of the limitations of this study is the high proportion of middle-aged health professionals included, as well as the education level and seniority, which may bias the results. In addition, the questionnaire was self-reported, and respondents may tend to give a positive answer concerning the question of the seriousness of the reply.
6. Conclusions
Facing the resurgence of certain sexually transmitted infections, this study aimed to evaluate the knowledge of STIs of French health professionals and students through a multiple-choice survey questionnaire.
The results of this study clearly show that certain notions about sexually transmitted infections remain gray zones for French health professionals and students. Several notions concerning the transmission, clinical manifestations, and evolution of these pathologies remain areas to be clarified for most health sectors. Globally, screening and vaccination seem to be the areas where the knowledge is well acquired. It is noteworthy that 60% of the respondents do not believe they have received sufficient initial training and that 82% of them would like to have more in-depth training concerning STIs.
It appears that, even if the basics of knowledge on STIs are present among French health professionals and students, it is far from being complete and acquired. It appears necessary to fill these gaps through additional training. Indeed, all health professionals are confronted on a daily basis, whether in the office, at the counter, or at the hospital, with situations concerning sexually transmitted infections. It is the duty of healthcare professionals to guide the patient through pathology and support prevention efforts in order to ensure the most optimal conditions for healthcare.
This questionnaire allowed us to detect areas in STI knowledge to be explored further by means of additional training. Globally, knowledge of STIs is scarce among French healthcare professionals and students. This study underlines the urgent need for specific training on STIs for this target population, with appropriate educational interventions (theoretical and practical), warranting solid scientifically based know-how on STIs, to be implemented in French Universities and French Health Centers. Thanks to the collaboration with Lunéville Sexual Health Center, several additional modules allowing CPD validations will soon be offered in Meurthe-et-Moselle (France) to allow health professionals to deepen their knowledge of sexual health and STIs.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/venereology3020006/s1, Table S1: percentage of responses checked per item out of all applicants in the questionnaire.
Author Contributions
Conceptualization, M.C., S.D., L.B. and M.V.; methodology, S.D., L.B. and M.V.; validation, M.C., S.D., L.B. and M.V.; formal analysis, M.C.; investigation, M.C.; resources, M.C.; data curation, M.C.; writing—original draft preparation, M.C., S.D., L.B. and M.V.; writing—review and editing, M.C., S.D., L.B., T.H. and M.V.; supervision, S.D. and M.V.; project administration, M.C., S.D. and M.V. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
All participants have been fully informed of the nature of the study and their participation. The anonymity of participants has been ensured. Since this study poses no risk to participants, ethical approval is not required.
Informed Consent Statement
Permission was acquired from the individuals partaking in the research, and the study’s aims were effectively conveyed to them. Engagement was entirely optional, and no manipulation or inappropriate persuasion was applied to the participants. The research upheld confidentiality and privacy, with all participants being guaranteed that their personal details and provided information would remain undisclosed and safeguarded.
Data Availability Statement
The data employed in this investigation are not accessible to the general public due to a confidentiality arrangement with the study participants. Nonetheless, the data can be obtained by reaching out to the designated author upon request.
Acknowledgments
We thank Cecile Henry for the careful proofreading of the manuscript, and for useful comments on the work.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Available online: https://www.who.int/fr/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis) (accessed on 30 December 2023).
- Ndeikoundam Ngangro, N.; Viriot, D.; Fournet, N.; Pioche, C.; De Barbeyrac, B.; Goubard, A.; Dupin, N.; Berçot, B.; Fouéré, S.; Alcaraz, I.; et al. Bacterial sexually transmitted infections in France: Recent trends and patients’ characteristics in 2016. Eurosurveillance 2019, 24, 1800038. [Google Scholar] [CrossRef]
- Available online: https://www.ecdc.europa.eu/en/sexually-transmitted-infections (accessed on 19 February 2024).
- Available online: https://www.cdc.gov/std/life-stages-populations/stdfact-teens.htm (accessed on 30 December 2023).
- Available online: https://www.nichd.nih.gov/health/topics/stds/conditioninfo/causes (accessed on 30 December 2023).
- Kumi Smith, M.; Jewell, B.L.; Hallett, T.B.; Cohen, M.S. Treatment of HIV for the Prevention of Transmission in Discordant Couples and at the Population Level. Adv. Exp. Med. Biol. 2018, 1075, 125–162. [Google Scholar] [CrossRef] [PubMed]
- Migueres, M.; Lhomme, S.; Izopet, J. Hepatitis A: Epidemiology, High-Risk Groups, Prevention and Research on Antiviral Treatment. Viruses 2021, 13, 1900. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.cdc.gov/std/statistics/2021/overview.htm (accessed on 30 December 2023).
- Available online: https://www.cdc.gov/std/treatment-guidelines/references.htm (accessed on 30 December 2023).
- Available online: https://link.springer.com/chapter/10.1007/978-3-030-02200-6_1 (accessed on 30 December 2023).
- Available online: https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-11-727 (accessed on 30 December 2023).
- Available online: https://www.cdc.gov/std/statistics/2021/tables/1.htm (accessed on 30 December 2023).
- Available online: https://apps.who.int/iris/bitstream/handle/10665/246296/WHO-RHR-16.09-eng.pdf (accessed on 30 December 2023).
- Available online: https://www.cdc.gov/std/statistics/2021/default.htm (accessed on 30 December 2023).
- Available online: https://www.cdc.gov/std/statistics/default.htm? (accessed on 30 December 2023).
- Stoltey, J.E.; Cohen, S.E. Syphilis transmission: A review of the current evidence. Sex. Health 2015, 12, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Winer, R.L.; Hughes, J.P.; Feng, Q.; O’Reilly, S.; Kiviat, N.B.; Holmes, K.K.; Koutsky, L.A. Condom use and the risk of genital human papillomavirus infection in young women. N. Engl. J. Med. 2006, 354, 2645–2654. [Google Scholar] [CrossRef] [PubMed]
- Peeling, R.W.; Mabey, D.; Chen, X.S.; Garcia, P.J. Syphilis. Lancet 2023, 402, 336–346. [Google Scholar] [CrossRef] [PubMed]
- Tortolero-Luna, G. Epidemiology of genital human papillomavirus. Hematol. Oncol. Clin. N. Am. 1999, 13, 245–257. [Google Scholar] [CrossRef] [PubMed]
- Browne, S.; Feemster, K.A. Human papillomavirus: Optimizing opportunities for prevention. Curr. Opin. Pediatr. 2022, 34, 132–139. [Google Scholar] [CrossRef]
- Vashisht, S.; Mishra, H.; Mishra, P.K.; Ekielski, A.; Talegaonkar, S. Structure, Genome, Infection Cycle and Clinical Manifestations Associated with Human Papillomavirus. Curr. Pharm. Biotechnol. 2019, 20, 1260–1280. [Google Scholar] [CrossRef] [PubMed]
- Ahmadi, M.H.; Mirsalehian, A.; Bahador, A. Association of Chlamydia trachomatis with infertility and clinical manifestations: A systematic review and meta-analysis of case-control studies. Infect. Dis. 2016, 48, 517–523. [Google Scholar] [CrossRef]
- Elwell, C.; Mirrashidi, K.; Engel, J. Chlamydia cell biology and pathogenesis. Nat. Rev. Microbiol. 2016, 14, 385–400. [Google Scholar] [CrossRef] [PubMed]
- Bébéar, C.; de Barbeyrac, B. Genital Chlamydia trachomatis infections. Clin. Microbiol. Infect. 2009, 15, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Moreno, I.; Cicinelli, E.; Garcia-Grau, I.; Gonzalez-Monfort, M.; Bau, D.; Vilella, F.; De Ziegler, D.; Resta, L.; Valbuena, D.; Simon, C. The diagnosis of chronic endometritis in infertile asymptomatic women: A comparative study of histology, microbial cultures, hysteroscopy, and molecular microbiology. Am. J. Obs. Gynecol. 2018, 218, 602.e1–602.e16. [Google Scholar] [CrossRef] [PubMed]
- Garner, A.L.; Schembri, G.; Cullen, T.; Lee, V. Should we screen heterosexuals for extra-genital chlamydial and gonococcal infections? Int. J. STD AIDS 2015, 26, 462–466. [Google Scholar] [CrossRef]
- Hook, E.W., 3rd; Holmes, K.K. Gonococcal infections. Ann. Intern. Med. 1985, 102, 229–243. [Google Scholar] [CrossRef] [PubMed]
- Corey, L.; Adams, H.G.; Brown, Z.A.; Holmes, K.K. Genital herpes simplex virus infections: Clinical manifestations, course, and complications. Ann. Intern. Med. 1983, 98, 958–972. [Google Scholar] [CrossRef] [PubMed]
- Omarova, S.; Cannon, A.; Weiss, W.; Bruccoleri, A.; Puccio, J. Genital Herpes Simplex Virus-An Updated Review. Adv. Pediatr. 2022, 69, 149–162. [Google Scholar] [CrossRef] [PubMed]
- Jaishankar, D.; Shukla, D. Genital Herpes: Insights into Sexually Transmitted Infectious Disease. Microb. Cell 2016, 3, 438–450. [Google Scholar] [CrossRef]
- OMS|Projet de Stratégie Mondiale du Secteur de la Santé sur le VIH/Sida, 2016–2021. Available online: https://www.who.int/hiv/proposed-hiv-strategy2016-2021/fr/ (accessed on 29 October 2019).
- Antela, A.; Aguiar, C.; Compston, J.; Hendry, B.M.; Boffito, M.; Mallon, P.; Pourcher-Martinez, V.; Di Perri, G. The role of tenofovir alafenamide in future HIV management. HIV Med. 2016, 17 (Suppl. S2), 4–16. [Google Scholar] [CrossRef]
- Fung, H.B.; Stone, E.A.; Piacenti, F.J. Tenofovir disoproxil fumarate: A nucleotide reverse transcriptase inhibitor for the treatment of HIV infection. Clin. Ther. 2002, 24, 1515–1548. [Google Scholar] [CrossRef]
- Quercia, R.; Perno, C.F.; Koteff, J.; Moore, K.; McCoig, C.; St Clair, M.; Kuritzkes, D. Twenty-Five Years of Lamivudine: Current and Future Use for the Treatment of HIV-1 Infection. J. Acquir. Immune Defic. Syndr. 2018, 78, 125–135. [Google Scholar] [CrossRef]
- Perry, C.M.; Faulds, D. Lamivudine. A review of its antiviral activity, pharmacokinetic properties and therapeutic efficacy in the management of HIV infection. Drugs 1997, 53, 657–680. [Google Scholar] [CrossRef]
- Wang, L.H.; Begley, J.; St Claire, R.L., 3rd; Harris, J.; Wakeford, C.; Rousseau, F.S. Pharmacokinetic and pharmacodynamic characteristics of emtricitabine support its once daily dosing for the treatment of HIV infection. AIDS Res. Hum. Retroviruses 2004, 20, 1173–1182. [Google Scholar] [CrossRef] [PubMed]
- Modrzejewski, K.A.; Herman, R.A. Emtricitabine: A once-daily nucleoside reverse transcriptase inhibitor. Ann. Pharmacother. 2004, 38, 1006–1014. [Google Scholar] [CrossRef] [PubMed]
- Frampton, J.E.; Perry, C.M. Emtricitabine: A review of its use in the management of HIV infection. Drugs 2005, 65, 1427–1448. [Google Scholar] [CrossRef]
- Available online: https://www.vidal.fr/sante/voyage/avant-voyage/vaccins-voyage/hepatite-a.html (accessed on 30 December 2023).
- Zoulim, F. Entecavir: A new treatment option for chronic hepatitis B. J. Clin. Virol. 2006, 36, 8–12. [Google Scholar] [CrossRef]
- Osborn, M. Safety and efficacy of entecavir for the treatment of chronic hepatitis B. Infect. Drug Resist. 2011, 4, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Tenofovir Alafenamide: A Review in Chronic Hepatitis B. Drugs 2017, 77, 1017–1028. [CrossRef]
- Jaeckel, E.; Manns, M.P. Experience with lamivudine against hepatitis B virus. Intervirology 1997, 40, 322–336. [Google Scholar] [CrossRef]
- Schiff, E.R. Lamivudine for hepatitis B in clinical practice. J. Med. Virol. 2000, 61, 386–391. [Google Scholar] [CrossRef]
- Available online: https://www.vidal.fr/medicaments/utilisation/vaccins/vaccin-hepatite-b.html (accessed on 30 December 2023).
- Kwo, P.Y. Boceprevir: A novel nonstructural 3 (NS3) protease inhibitor for the treatment of chronic hepatitis C infection. Ther. Adv. Gastroenterol. 2012, 5, 179–188. [Google Scholar] [CrossRef]
- Chang, M.H.; Gordon, L.A.; Fung, H.B. Boceprevir: A protease inhibitor for the treatment of hepatitis C. Clin. Ther. 2012, 34, 2021–2038. [Google Scholar] [CrossRef]
- Zeuzem, S.; Andreone, P.; Pol, S.; Lawitz, E.; Diago, M.; Roberts, S.; Focaccia, R.; Younossi, Z.; Foster, G.R.; Horban, A.; et al. Telaprevir for retreatment of HCV infection. N. Engl. J. Med. 2011, 364, 2417–2428. [Google Scholar] [CrossRef]
- Jesudian, A.B.; Jacobson, I.M. Optimal treatment with telaprevir for chronic HCV infection. Liver Int. 2013, 33 (Suppl. S1), 3–13. [Google Scholar] [CrossRef]
- Galvao, T.F.; Silva, M.T.; Serruya, S.J.; Newman, L.M.; Klausner, J.D.; Pereira, M.G.; Fescina, R. Safety of benzathine penicillin for preventing congenital syphilis: A systematic review. PLoS ONE 2013, 8, e56463. [Google Scholar] [CrossRef]
- Chen, X.; Li, G.; Gan, Y.; Chu, T.; Liu, D. Availability of benzathine penicillin G for syphilis treatment in Shandong Province, Eastern China. BMC Health Serv. Res. 2019, 19, 188. [Google Scholar] [CrossRef] [PubMed]
- Dai, T.; Qu, R.; Liu, J.; Zhou, P.; Wang, Q. Efficacy of Doxycycline in the Treatment of Syphilis. Antimicrob. Agents Chemother. 2016, 61, e01092-16. [Google Scholar] [CrossRef]
- Psomas, K.C.; Brun, M.; Causse, A.; Atoui, N.; Reynes, J.; Le Moing, V. Efficacy of ceftriaxone and doxycycline in the treatment of early syphilis. Med. Mal. Infect. 2012, 42, 15–19. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.vidal.fr/medicaments/utilisation/vaccins/vaccin-papillomavirus.html (accessed on 30 December 2023).
- Foulds, G.; Shepard, R.M.; Johnson, R.B. The pharmacokinetics of azithromycin in human serum and tissues. J. Antimicrob. Chemother. 1990, 25 (Suppl. SA), 73–82. [Google Scholar] [CrossRef]
- Geisler, W.M.; Uniyal, A.; Lee, J.Y.; Lensing, S.Y.; Johnson, S.; Perry, R.C.; Kadrnka, C.M.; Kerndt, P.R. Azithromycin versus Doxycycline for Urogenital Chlamydia trachomatis Infection. N. Engl. J. Med. 2015, 373, 2512–2521. [Google Scholar] [CrossRef]
- Ring, J. Highlights from the Journal of the European Academy of Dermatology and Venereology in 2022. J. Eur. Acad. Dermatol. Venereol. 2023, 37, 9–11. [Google Scholar] [CrossRef] [PubMed]
- Pronovost, A.D.; Lucia, H.L.; Dann, P.R.; Hsiung, G.D. Effect of acyclovir on genital herpes in guinea pigs. J. Infect. Dis. 1982, 145, 904–908. [Google Scholar] [CrossRef] [PubMed]
- Ormrod, D.; Goa, K. Valaciclovir: A review of its use in the management of herpes zoster. Drugs 2000, 59, 1317–1340. [Google Scholar] [CrossRef] [PubMed]
- Hull, C.; Spruance, S.; Tyring, S.; Hamed, K. Single-dose famciclovir for the treatment of herpes labialis. Curr. Med. Res. Opin. 2006, 22, 1699–1702. [Google Scholar] [CrossRef] [PubMed]
- Lowndes, C.M.; Fenton, K.A.; European Surveillance of STI’s Network. Surveillance systems for STIs in the European Union: Facing a changing epidemiology. Sex. Transm. Infect. 2004, 80, 264–271. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://doi.org/10.1016/j.lanepe.2023.100743 (accessed on 19 February 2024).
- Garcia, P.J.; Benzaken, A.S.; Galban, E.; ALAC-ITS members. STI management and control in Latin America: Where do we stand and where do we go from here? Sex. Transm. Infect. 2011, 87 (Suppl. S2), ii7–ii9. [Google Scholar] [CrossRef] [PubMed]
- Mahboob, N.; Iqbal, H.; Afrin, S.; Abedin, F.Z.; Ahmed, M. Assessment of Knowledge and Attitude about Sexually Transmitted Infections among Medical Students of Dhaka City, Bangladesh. Saudi J. Pathol. Microbiol. 2022, 7, 313–320. [Google Scholar] [CrossRef]
- Phrasisombath, K.; Thomsen, S.; Hagberg, J.; Sychareun, V.; Faxelid, E. Knowledge about sexually transmitted infections (STIs) and attitudes toward female sex workers with STI symptoms among health care providers in Laos. Asia Pac. J. Public Health 2012, 24, 940–952. [Google Scholar] [CrossRef]
- Folasayo, A.T.; Oluwasegun, A.J.; Samsudin, S.; Saudi, S.N.; Osman, M.; Hamat, R.A. Assessing the Knowledge Level, Attitudes, Risky Behaviors and Preventive Practices on Sexually Transmitted Diseases among University Students as Future Healthcare Providers in the Central Zone of Malaysia: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2017, 14, 159. [Google Scholar] [CrossRef]
- Mashingaidze, R.; Moodie, Z.; Allen, M.; Bekker, L.G.; Grove, D.; Grunenberg, N.; Huang, Y.; Janes, H.E.; Lazarus, E.M.; Malahleha, M.; et al. Sexually transmitted infections amongst men who have sex with men (MSM) in South Africa. PLOS Glob. Public Health 2023, 3, e0001782. [Google Scholar] [CrossRef]
- Werner, R.N.; Gaskins, M.; Nast, A.; Dressler, C. Incidence of sexually transmitted infections in men who have sex with men and who are at substantial risk of HIV infection—A meta-analysis of data from trials and observational studies of HIV pre-exposure prophylaxis. PLoS ONE 2018, 13, e0208107. [Google Scholar] [CrossRef] [PubMed]
- Alexander, T.S. Human Immunodeficiency Virus Diagnostic Testing: 30 Years of Evolution. Clin. Vaccine Immunol. 2016, 23, 249–253. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control y Prevention. Quick Reference Guide. Recommended Laboratory HIV Testing Algorithm for Serum or Plasma Specimens. 2018. Available online: https://stacks.cdc.gov/view/cdc/50872 (accessed on 19 February 2024).
- Griffin, D.O. The diagnosis of symptomatic acute antiretroviral syndrome during the window period with antigen/antibody testing and HIV viral load. IDCases 2018, 12, 157–160. [Google Scholar] [CrossRef] [PubMed]
- Alshuwaykh, O.; Kwo, P.Y. Current and future strategies for the treatment of chronic hepatitis C. Clin. Mol. Hepatol. 2021, 27, 246–256. [Google Scholar] [CrossRef]
- Farci, P.; Alter, H.J.; Shimoda, A.; Govindarajan, S.; Cheung, L.C.; Melpolder, J.C.; Sacher, R.A.; Shih, J.W.; Purcell, R.H. Hepatitis C virus-associated fulminant hepatic failure. N. Engl. J. Med. 1996, 335, 631–634. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).