ESKAPE: Navigating the Global Battlefield for Antimicrobial Resistance and Defense in Hospitals
Abstract
1. Introduction
2. Treatment and Control Measures Currently Implemented with Limitations
2.1. Antibiotic Stewardship Programs
2.1.1. Infection Prevention and Control Practices
2.1.2. Environmental Cleaning and Disinfection
2.1.3. Surveillance Programs with Patient/Staff Education
3. Effects of ASP on ESKAPE Pathogens
4. Future Measures for Successful Mitigation
4.1. Incentives for Novel Antibiotic Development
4.2. Interdisciplinary Research
4.3. Alternative Therapies and Treatment Modalities
4.4. Precision Medicine for Infectious Diseases
- -
- Genetic variability: Precision medicine often involves genomic analysis to identify genetic variations in pathogens that contribute to drug resistance. For example, the identification of specific mutations in the genes responsible for antibiotic targets can inform the development of drugs that overcome these resistance mechanisms. In the case of Mycobacterium tuberculosis, whole-genome sequencing can reveal mutations associated with resistance to anti-tuberculosis drugs, guiding the selection of personalized treatment regimens [71].
- -
- Tailored treatments: Precision medicine aims to develop drugs that specifically target the vulnerabilities of multidrug-resistant pathogens. The use of targeted therapies, such as monoclonal antibodies, that focus on specific components of the bacterial cell wall can be explored for bacteria like MRSA [72].
- -
- Pharmacogenomic studies: They can help understand how an individual’s genetic makeup influences their response to medications, aiding in the selection of the most effective and least toxic drugs. Identifying genetic markers associated with resistance to certain antibiotics can guide clinicians in choosing alternative drugs for treating infections caused by multidrug-resistant bacteria [73,74].
- -
- Host factors: Precision medicine recognizes the importance of host–pathogen interactions and incorporates host factors into treatment strategies. Understanding the host’s immune response and genetic factors can inform the development of immunotherapies or adjunctive therapies that enhance the host’s ability to combat infections caused by multidrug-resistant pathogens [75].
4.5. Technological Innovations
4.6. Global Surveillance Networks
4.7. One Health Approach
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Raoofi, S.; Kan, F.P.; Rafiei, S.; Hosseinipalangi, Z.; Mejareh, Z.N.; Khani, S.; Abdollahi, B.; Talab, F.S.; Sanaei, M.; Zarabi, F.; et al. Global prevalence of nosocomial infection: A systematic review and meta-analysis. PLoS ONE 2023, 18, e0274248. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Long, Y.; Greenhalgh, C.; Steeg, S.; Wilkinson, J.; Li, H.; Verma, A.; Spencer, A. A systematic review and meta-analysis of risk factors associated with healthcare-associated infections among hospitalised patients in Chinese general hospitals from 2001 to 2022. J. Hosp. Infect. 2023, 135, 37–49. [Google Scholar] [CrossRef] [PubMed]
- Naz, S.; Paritosh, K.; Sanyal, P.; Khan, S.; Singh, Y.; Varshney, U.; Nandicoori, V.K. GWAS and functional studies suggest a role for altered DNA repair in the evolution of drug resistance in Mycobacterium tuberculosis. elife 2023, 12, e75860. [Google Scholar] [CrossRef] [PubMed]
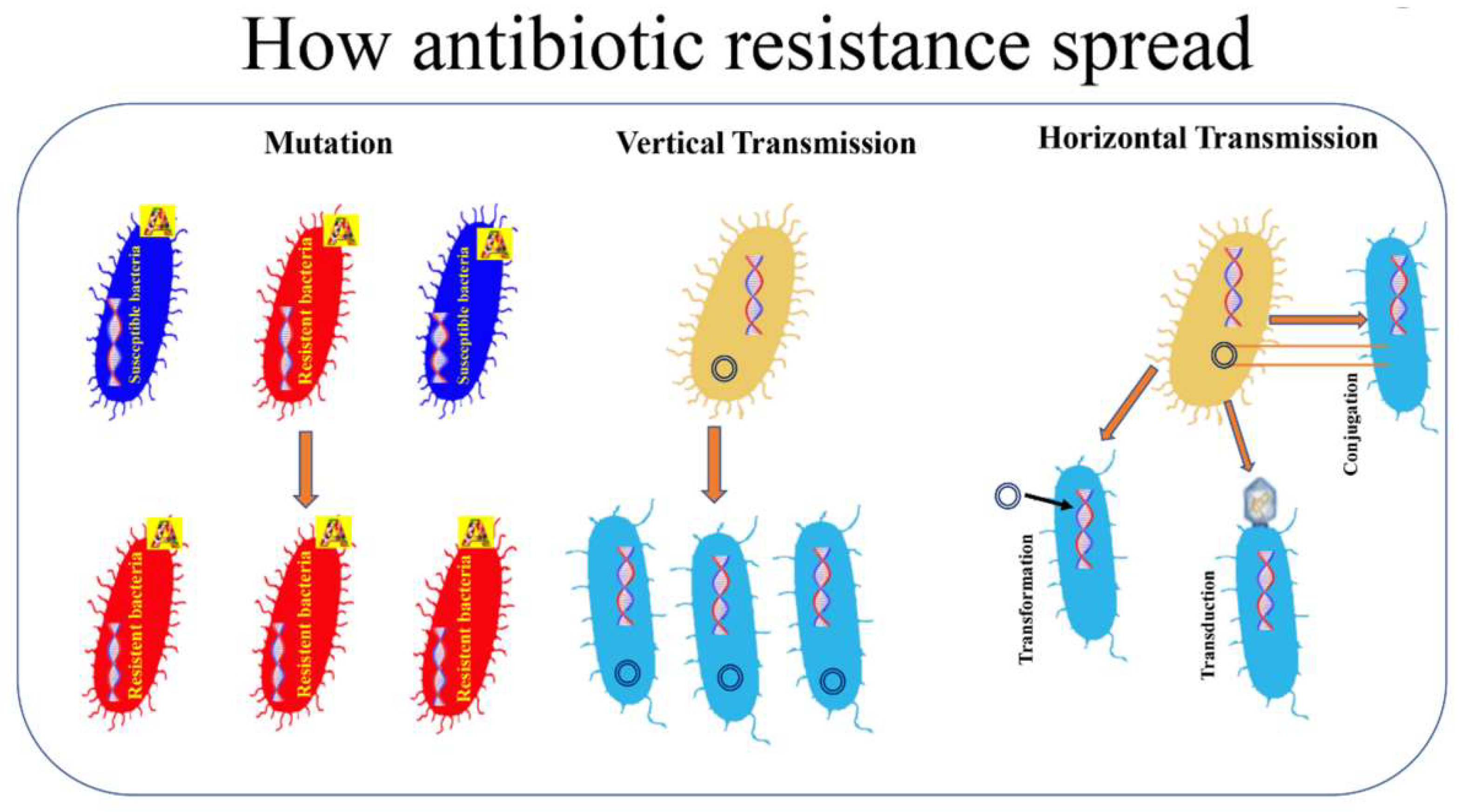
- Michaelis, C.; Grohmann, E. Horizontal gene transfer of antibiotic resistance genes in biofilms. Antibiotics 2023, 12, 328. [Google Scholar] [CrossRef] [PubMed]
- Mancuso, G.; Midiri, A.; Gerace, E.; Biondo, C. Bacterial antibiotic resistance: The most critical pathogens. Pathogens 2021, 10, 1310. [Google Scholar] [CrossRef] [PubMed]
- Bodendoerfer, E.; Marchesi, M.; Imkamp, F.; Courvalin, P.; Böttger, E.C.; Mancini, S. Co-occurrence of aminoglycoside and β-lactam resistance mechanisms in aminoglycoside- non-susceptible Escherichia coli isolated in the Zurich area, Switzerland. Int. J. Antimicrob. Agents 2020, 56, 106019. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, V.; Tiwari, A.; Varadwaj, P. An Extensive Review on β-lactamase Enzymes and their Inhibitors. Curr. Med. Chem. 2023, 30, 783–808. [Google Scholar] [CrossRef] [PubMed]
- Wang, N.; Luo, J.; Deng, F.; Huang, Y.; Zhou, H. Antibiotic combination therapy: A strategy to overcome bacterial resistance to aminoglycoside antibiotics. Front. Pharmacol. 2022, 13, 839808. [Google Scholar] [CrossRef]
- Varela, M.F.; Stephen, J.; Lekshmi, M.; Ojha, M.; Wenzel, N.; Sanford, L.M.; Hernandez, A.J.; Parvathi, A.; Kumar, S.H. Bacterial resistance to antimicrobial agents. Antibiotics 2021, 10, 593. [Google Scholar] [CrossRef]
- Gaurav, A.; Bakht, P.; Saini, M.; Pandey, S.; Pathania, R. Role of bacterial efflux pumps in antibiotic resistance, virulence, and strategies to discover novel efflux pump inhibitors. Microbiology 2023, 169, 001333. [Google Scholar] [CrossRef]
- Kulshrestha, M.; Tiwari, M.; Tiwari, V. Bacteriophage therapy against ESKAPE bacterial pathogens: Current status, strategies, challenges, and future scope. Microb. Pathog. 2023, 186, 106467. [Google Scholar] [CrossRef] [PubMed]
- O’Toole, R.F.; Leong, K.W.; Cumming, V.; Van Hal, S.J. Vancomycin-resistant Enterococcus faecium and the emergence of new sequence types associated with hospital infection. Res. Microbiol. 2023, 174, 104046. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Antimicrobial Resistance Surveillance in Europe 2022–2020 Data; World Health Organization, Re-gional Office for Europe: Copenhagen, Denmark, 2022. [Google Scholar]
- Kourtis, A.P.; Hatfield, K.; Baggs, J.; Mu, Y.; See, I.; Epson, E.; Nadle, J.; Kainer, M.A.; Dumyati, G.; Petit, S.; et al. Vital signs: Epidemiology and recent trends in methicillin-resistant and in methicillin-susceptible staphylococcus aureus bloodstream infections—United States. Morb. Mortal. Wkly. Rep. 2019, 68, 214–219. [Google Scholar] [CrossRef] [PubMed]
- Cassini, A.; Högberg, L.D.; Plachouras, D.; Quattrocchi, A.; Hoxha, A.; Simonsen, G.S.; Colomb-Cotinat, M.; Kretzschmar, M.E.; Devleesschauwer, B.; Cecchini, M.; et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: A population-level modelling analysis. Lancet Infect. Dis. 2019, 19, 56–66. [Google Scholar] [CrossRef] [PubMed]
- Karakonstantis, S.; Kritsotakis, E.I.; Gikas, A. Treatment options for K. pneumoniae, P. aeruginosa and A. baumannii co-resistant to carbapenems, aminoglycosides, polymyxins and tigecycline: An approach based on the mechanisms of resistance to car-bapenems. Infection 2020, 48, 835–851. [Google Scholar] [CrossRef] [PubMed]
- Bennett, J.W.; Chung, K.T. Alexander Fleming and the discovery of penicillin. Adv. Appl. Microb. 2001, 49, 163–184. [Google Scholar]
- Du, X.; Xu, X.; Yao, J.; Deng, K.; Chen, S.; Shen, Z.; Yang, L.; Feng, G. Predictors of mortality in patients infected with carbapenem-resistant Acinetobacter baumannii: A systematic review and meta-analysis. Am. J. Infect. Control 2019, 47, 1140–1145. [Google Scholar] [CrossRef]
- Li, Y.; Roberts, J.A.; Walker, M.M.; Aslan, A.T.; Harris, P.N.; Sime, F.B. The global epidemiology of ventilator-associated pneumonia caused by multi-drug resistant Pseudomonas aeruginosa: A systematic review and meta-analysis. Int. J. Infect. Dis. 2023, 139, 78–85. [Google Scholar] [CrossRef]
- Murray, C.J.L.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Aguilar, G.R.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E.; et al. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef]
- Wozniak, T.M.; Barnsbee, L.; Lee, X.J.; Pacella, R.E. Using the best available data to estimate the cost of antimicrobial resistance: A systematic review. Antimicrob. Resist. Infect. Control 2019, 8, 1–12. [Google Scholar] [CrossRef]
- O’kelly, B.; Rueda-Benito, A.; O’regan, M.; Finan, K. An audit of community-acquired pneumonia antimicrobial compliance using an intervention bundle in an Irish hospital. J. Glob. Antimicrob. Resist. 2020, 23, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Patel, D.; Ng, T.; Madani, L.S.; Persell, S.D.; Greg, M.; Roemer, P.E.; Oberoi, S.K.; Linder, J.A. Antibiotic stewardship to reduce inappropriate antibiotic prescribing in integrated academic health-system urgent care clinics. Infect. Control. Hosp. Epidemiology 2023, 44, 736–745. [Google Scholar] [CrossRef] [PubMed]
- Bankar, N.J.; Ugemuge, S.; Ambad, R.S.; Hawale, D.V.; Timilsina, D.R. Implementation of antimicrobial stewardship in the healthcare setting. Cureus 2022, 14, e26664. [Google Scholar] [CrossRef] [PubMed]
- Doll, M.; Stevens, M.; Bearman, G. Environmental cleaning and disinfection of patient areas. Int. J. Infect. Dis. 2018, 67, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Verma, M.; Shafiq, N.; Tripathy, J.P.; Nagaraja, S.B.; Kathirvel, S.; Chouhan, D.K.; Arora, P.; Singh, T.; Jain, K.; Gautam, V.; et al. Antimicrobial stewardship programme in a trauma centre of a tertiary care hospital in North India: Effects and implementation challenges. J. Glob. Antimicrob. Resist. 2019, 17, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Shekelle, P.G.; Wachter, R.M.; Pronovost, P.J.; Schoelles, K.; McDonald, K.M.; Dy, S.M.; Shojania, K.; Reston, J.; Berger, Z.; Johnsen, B.; et al. Making health care safer II: An updated critical analysis of the evidence for patient safety practices. Evid. Rep. Technol. Assess. Full Rep. 2013, 211, 1–945. Available online: https://pubmed.ncbi.nlm.nih.gov/24423049/ (accessed on 10 April 2024).
- Stangerup, M.; Hansen, M.B.; Hansen, R.; Sode, L.P.; Hesselbo, B.; Kostadinov, K.; Olesen, B.S.; Calum, H. Hand hygiene compliance of healthcare workers before and during the COVID-19 pandemic: A long-term follow-up study. Am. J. Infect. Control. 2021, 49, 1118–1122. [Google Scholar] [CrossRef] [PubMed]
- Lotfinejad, N.; Peters, A.; Tartari, E.; Fankhauser-Rodriguez, C.; Pires, D.; Pittet, D. Hand hygiene in health care: 20 years of ongoing advances and perspectives. Lancet Infect. Dis. 2021, 21, e209–e221. [Google Scholar] [CrossRef] [PubMed]
- Chernet, A.Z.; Dasta, K.; Belachew, F.; Zewdu, B.; Melese, M.; Ali, M.M. Burden of healthcare-associated infections and associated risk factors at Adama Hospital Medical College, Adama, Oromia, Ethiopia. Drug Heal. Patient Saf. 2020, 12, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Park, S.H. Personal protective equipment for healthcare workers during the COVID-19 pandemic. Infect. Chemother. 2020, 52, 165–182. [Google Scholar] [CrossRef]
- Cai, Y.; Liu, J.; Li, G.; Wong, P.K.; An, T. Formation mechanisms of viable but nonculturable bacteria through induction by light-based disinfection and their antibiotic resistance gene transfer risk: A review. Crit. Rev. Environ. Sci. Technol. 2022, 52, 3651–3688. [Google Scholar] [CrossRef]
- Sadowy, E.; Luczkiewicz, A. Drug-resistant and hospital-associated Enterococcus faecium from wastewater, riverine estuary and anthropogenically impacted marine catchment basin. BMC Microbiol. 2014, 14, 66. [Google Scholar] [PubMed]
- Higgins, P.G.; Hrenovic, J.; Seifert, H.; Dekic, S. Characterization of Acinetobacter baumannii from water and sludge line of secondary wastewater treatment plant. Water Res. 2018, 140, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Surleac, M.; Barbu, I.C.; Paraschiv, S.; Popa, L.I.; Gheorghe, I.; Marutescu, L.; Popa, M.; Sarbu, I.; Talapan, D.; Nita, M.; et al. Whole genome sequencing snapshot of multi-drug resistant Klebsiella pneumoniae strains from hospitals and receiving wastewater treatment plants in Southern Romania. PLoS ONE 2020, 15, e0228079. [Google Scholar]
- Merrill, K.; Hanson, S.F.; Sumner, S.; Vento, T.; Veillette, J.; Webb, B. Antimicrobial stewardship: Staff nurse knowledge and attitudes. Am. J. Infect. Control 2019, 47, 1219–1224. [Google Scholar] [PubMed]
- Wilken, D.; Baur, X.; Barbinova, L.; Preisser, A.; Meijer, E.; Rooyackers, J.; Heederik, D. What are the benefits of medical screening and surveillance? Eur. Respir. Rev. 2012, 21, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Blake, K.S.; Choi, J.; Dantas, G. Approaches for characterizing and tracking hospital-associated multidrug-resistant bacteria. Cell. Mol. Life Sci. 2021, 78, 2585–2606. [Google Scholar] [CrossRef] [PubMed]
- Schinas, G.; Polyzou, E.; Spernovasilis, N.; Gogos, C.; Dimopoulos, G.; Akinosoglou, K. Preventing Multidrug-Resistant Bacterial Transmission in the Intensive Care Unit with a Comprehensive Approach: A Policymaking Manual. Antibiotics 2023, 12, 1255. [Google Scholar] [CrossRef] [PubMed]
- Tacconelli, E.; Sifakis, F.; Harbarth, S.; Schrijver, R.; van Mourik, M.; Voss, A.; Sharland, M.; Rajendran, N.B.; Rodríguez-Baño, J.; Bielicki, J.; et al. Surveillance for control of antimicrobial resistance. Lancet Infect. Dis. 2018, 18, e99–e106. [Google Scholar] [CrossRef]
- Dyer, C.; Hutt, L.P.; Burky, R.; Joshi, L.T. Biocide resistance and transmission of Clostridium difficile spores spiked onto clinical surfaces from an American health care facility. Appl. Environ. Microbiol. 2019, 85, e01090-19. [Google Scholar] [CrossRef]
- Sargeant, J.M.; O’Connor, A.M.; Winder, C.B. Editorial: Systematic reviews reveal a need for more, better data to inform antimicrobial stewardship practices in animal agriculture. Anim. Heal. Res. Rev. 2019, 20, 103–105. [Google Scholar] [CrossRef]
- Walker, S. Effective antimicrobial resistance communication: The role of information design. Palgrave Commun. 2019, 5, 24. [Google Scholar] [CrossRef]
- Kinnear, C.L.; Patel, T.S.; Young, C.L.; Marshall, V.; Newton, D.W.; Read, A.F.; Woods, R.J. Impact of an antimicrobial stewardship inter-vention on within-and between-patient daptomycin resistance evolution in vancomycin-resistant Enterococcus faecium. Timicrobial Agents Chemother. 2019, 63, 10–128. [Google Scholar]
- O’Riordan, F.; Shiely, F.; Byrne, S.; O’Brien, D.; Ronayne, A.; Fleming, A. Antimicrobial use and antimicrobial resistance in Entero-bacterales and Enterococcus faecium: A time series analysis. J. Hosp. Infect. 2022, 120, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, C.T.; Gandhi, T.; Chenoweth, C.; Lassiter, J.; Dela Pena, J.; Eschenauer, G.; Nagel, J.L. Impact of an antimicrobial stewardship-led intervention for Staphylococcus aureus bacteraemia: A quasi-experimental study. J. Antimicrob. Chemother. 2015, 70, 3390–3396. [Google Scholar]
- Jover-Sáenz, A.; Ramírez-Hidalgo, M.; Bellés, A.B.; Murillo, E.R.; Bosch, M.B.; Miró, A.R.; López, A.M.; Cabanillas, J.C.; Palacín, N.P.; Garrido-Calvo, S.; et al. Effects of a Primary Care Antimicrobial Stewardship Program on Meticillin-Resistant Staphylococcus aureus Strains across a Region of Catalunya (Spain) over 5 Years. Antibiotics 2024, 13, 92. [Google Scholar] [CrossRef]
- Giacobbe, D.R.; Salsano, A.; Del Puente, F.; Campanini, F.; Mariscalco, G.; Marchese, A.; Viscoli, C.; Santini, F. Reduced incidence of carbapenem-resistant klebsiella pneumoniae infections in cardiac surgery patients after implementation of an antimicrobial stewardship project. Antibiotics 2019, 8, 132. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Hu, S.; Sun, J.; Zhang, L.; Dong, H.; Feng, W.; Lei, J.; Dong, Y. Antibiotic consumption versus the prevalence of carbapenem-resistant Gram-negative bacteria at a tertiary hospital in China from 2011 to 2017. J. Infect. Public Heal. 2019, 12, 195–199. [Google Scholar] [CrossRef]
- Marra, A.R.; de Almeida, S.M.; Correa, L.; Silva, M., Jr.; Martino, M.D.; Silva, C.V.; Cal, R.G.; Edmond, M.B.; dos Santos, O.F. The effect of limiting antimicrobial therapy duration on antimicrobial resistance in the critical care setting. Am. J. Infect. Control 2009, 37, 204–209. [Google Scholar] [CrossRef] [PubMed]
- Yusef, D.; A Hayajneh, W.; Issa, A.B.; Haddad, R.; Al-Azzam, S.; A Lattyak, E.; Lattyak, W.J.; Gould, I.; Conway, B.R.; Bond, S.; et al. Impact of an antimicrobial stewardship programme on reducing broad-spectrum antibiotic use and its effect on carbapenem-resistant Acinetobacter baumannii (CRAb) in hospitals in Jordan. J. Antimicrob. Chemother. 2020, 76, 516–523. [Google Scholar] [CrossRef]
- Rizk, N.A.; Zahreddine, N.; Haddad, N.; Ahmadieh, R.; Hannun, A.; Bou Harb, S.; Haddad, S.F.; Zeenny, R.M.; Kanj, S.S. The Impact of antimicrobial stewardship and infection control interventions on Acinetobacter baumannii resistance rates in the ICU of a ter-tiary care center in Lebanon. Antibiotics 2022, 11, 911. [Google Scholar] [CrossRef] [PubMed]
- Sid Ahmed, M.A.; Abdel Hadi, H.; Abu Jarir, S.; Al Khal, A.L.; Al-Maslamani, M.A.; Jass, J.; Ibrahim, E.B.; Ziglam, H. Impact of an antimi-crobial stewardship programme on antimicrobial utilization and the prevalence of MDR Pseudomonas aeruginosa in an acute care hospital in Qatar. JAC-Antimicrob. Resist. 2020, 2, dlaa050. [Google Scholar] [CrossRef] [PubMed]
- Slain, D.; Sarwari, A.R.; Petros, K.O.; McKnight, R.L.; Sager, R.B.; Mullett, C.J.; Wilson, A.; Thomas, J.G.; Moffett, K.; Palmer, H.C.; et al. Impact of a multimodal antimicrobial stewardship program on Pseudomonas aeruginosa susceptibility and antimicrobial use in the intensive care unit setting. Crit. Care Res. Pr. 2011, 2011, 416426. [Google Scholar]
- Strazzulla, A.; Bokobza, S.; Ombandza, E.; Kherallah, K.; Hommel, S.; Draidi, R.; Bonutto, C.; Zamponi, D.B.; Gauzit, R.; Diamantis, S. Impact of an antimicrobial stewardship program on resistance to fluoroquinolones of urinary enterobacteriaceae isolated from nursing home residents: A retrospective cohort study. J. Am. Med. Dir. Assoc. 2020, 21, 1322–1326. [Google Scholar] [CrossRef] [PubMed]
- Cipko, K.; Cuenca, J.; Wales, E.; Harris, J.; Bond, S.; Newton, P.; Miyakis, S. Implementation of an antimicrobial stewardship programme and reduction in carbapenemase-producing Enterobacterales in an Australian local health district. JAC-Antimicrob. Resist. 2020, 2, dlaa041. [Google Scholar] [CrossRef] [PubMed]
- Udaondo, Z.; Matilla, M.A. Mining for novel antibiotics in the age of antimicrobial resistance. Microb. Biotechnol. 2020, 13, 1702–1704. [Google Scholar] [CrossRef] [PubMed]
- Miethke, M.; Pieroni, M.; Weber, T.; Brönstrup, M.; Hammann, P.; Halby, L.; Arimondo, P.B.; Glaser, P.; Aigle, B.; Bode, H.B.; et al. Towards the sustainable discovery and development of new antibiotics. Nat. Rev. Chem. 2021, 5, 726–749. [Google Scholar] [CrossRef]
- Morel, C.M.; Lindahl, O.; Harbarth, S.; de Kraker, M.E.; Edwards, S.; Hollis, A. Industry incentives and antibiotic resistance: An intro-duction to the antibiotic susceptibility bonus. J. Antibiot. 2020, 73, 421–428. [Google Scholar] [CrossRef]
- Ehsan, F. Boosting innovation in small- and medium-sized enterprises through tax incentives: Lessons from the UK. Sci. Public Policy 2021, 48, 712–726. [Google Scholar] [CrossRef]
- Dutescu, I.A.; Hillier, S.A. Encouraging the development of new antibiotics: Are financial incentives the right way forward? A systematic review and case study. Infect. Drug Resist. 2021, 14, 415–434. [Google Scholar] [CrossRef]
- Arslan, B.; Vasudeva, G.; Hirsch, E.B. Public–Private and Private–Private Collaboration as Pathways for Socially Beneficial Innovation: Evidence from Antimicrobial Drug-Development Tasks. Acad. Manag. J. 2023. [Google Scholar] [CrossRef]
- Zhang, N.; Shan, W.; Gao, L.; Kou, S.H.; Lu, C.; Yang, H.; Peng, B.; Tam, K.Y.; Lee, L.T.O.; Zheng, J. Repurposing the Hedgehog pathway inhibitor, BMS-833923, as a phosphatidylglycerol-selective membrane-disruptive colistin adjuvant against ESKAPE pathogens. Int. J. Antimicrob. Agents 2023, 62, 106888. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Hou, H.; Gao, F. Current scenario of quinolone hybrids with potential antibacterial activity against ESKAPE pathogens. Eur. J. Med. Chem. 2023, 247, 115026. [Google Scholar] [CrossRef] [PubMed]
- Lu, J.; Sheldenkar, A.; Lwin, M.O. A decade of antimicrobial resistance research in social science fields: A scientometric review. Antimicrob. Resist. Infect. Control. 2020, 9, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Liu, Y.; Gong, Y.; Yan, X.; Wang, L.; Zheng, W.; Ai, H.; Zhao, Y. Recent advances in nanoantibiotics against multidrug-resistant bacteria. Nanoscale Adv. 2023, 5, 6278–6317. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.R.; Sinha, D.K.; Agrawal, R.K.; Singh, V. Alternative Approaches to Mitigate Antimicrobial Drug Resistance. Bareilly: Division of Epidemiology; ICAR-Indian Veterinary Research Institute: Bareilly, India, 2021. [Google Scholar]
- Düzgüneş, N.; Sessevmez, M.; Yildirim, M. Bacteriophage therapy of bacterial infections: The rediscovered frontier. Pharmaceuticals 2021, 14, 34. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.; Ding, M.; Song, Y.; Hu, Y.; Xiu, W.; Yuwen, L.; Xie, Y.; Song, Y.; Shao, J.; Song, X.; et al. Nanotherapeutics with immunoregulatory functions for the treatment of bacterial infection. Biomater. Res. 2023, 27, 73. [Google Scholar] [CrossRef] [PubMed]
- Merker, M.; Tueffers, L.; Vallier, M.; Groth, E.E.; Sonnenkalb, L.; Unterweger, D.; Baines, J.F.; Niemann, S.; Schulenburg, H. Evolutionary approaches to combat antibiotic resistance: Opportunities and challenges for precision medicine. Front. Immunol. 2020, 11, 568485. [Google Scholar] [CrossRef] [PubMed]
- Watney, A.A.; Cosgrove, C.A.; Arnold, A.; Hinds, J.; Stoker, N.G.; Butcher, P.D. Clinical use of whole genome sequencing for Myco-bacterium tuberculosis. BMC Med. 2016, 14, 46. [Google Scholar]
- Speziale, P.; Pietrocola, G. Monoclonal antibodies targeting surface-exposed and secreted proteins from staphylococci. Vaccines 2021, 9, 459. [Google Scholar] [CrossRef]
- Marimani, M.; Ahmad, A.; Duse, A. The Role of Advanced Therapeutic Techniques to Combat Multi-drug Resistance. In Non-traditional Approaches to Combat Antimicrobial Drug Resistance; Springer Nature: Singapore, 2023; pp. 29–55. [Google Scholar] [CrossRef]
- Topp, E.; Larsson, D.G.J.; Miller, D.N.; Eede, C.V.D.; Virta, M.P.J. Antimicrobial resistance and the environment: Assessment of advances, gaps and recommendations for agriculture, aquaculture and pharmaceutical manufacturing. FEMS Microbiol. Ecol. 2017, 94, fix185. [Google Scholar] [CrossRef] [PubMed]
- Hancock, R.E.; Nijnik, A.; Philpott, D.J. Modulating immunity as a therapy for bacterial infections. Nat. Rev. Microbiol. 2012, 10, 243–254. [Google Scholar] [CrossRef] [PubMed]
- Wheeler, N.E.; Price, V.; Cunningham-Oakes, E.; Tsang, K.K.; Nunn, J.G.; Midega, J.T.; Anjum, M.F.; Wade, M.J.; Feasey, N.A.; Peacock, S.J.; et al. Innovations in genomic antimicrobial resistance surveillance. Lancet Microbe 2023, 4, e1063–e1070. [Google Scholar] [CrossRef] [PubMed]
- Nayarisseri, A.; Khandelwal, R.; Tanwar, P.; Madhavi, M.; Sharma, D.; Thakur, G.; Speck-Planche, A.; Singh, S.K. Artificial intelligence, big data and machine learning approaches in precision medicine & drug discovery. Curr. Drug Targets 2021, 22, 631–655. [Google Scholar] [PubMed]
- Sakagianni, A.; Koufopoulou, C.; Feretzakis, G.; Kalles, D.; Verykios, V.S.; Myrianthefs, P. Using Machine Learning to Predict Anti-microbial Resistance―A Literature Review. Antibiotics 2023, 12, 452. [Google Scholar] [CrossRef] [PubMed]
- Simonsen, G.S. Antimicrobial resistance surveillance in Europe and beyond. Eurosurveillance 2018, 23, 1800560–1800564. [Google Scholar] [CrossRef]
- World Health Organization. Global Antimicrobial Resistance Surveillance System (GLASS) Report: Early Implementation; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- White, A.; Hughes, J.M. Critical Importance of a One Health Approach to Antimicrobial Resistance. Ecohealth 2019, 16, 404–409. [Google Scholar] [CrossRef]
- Golding, S.E. Exploring Antimicrobial Stewardship in UK Veterinary Medicine and Livestock Agriculture: A Mixed-Method, one Health Approach. Ph.D. Thesis, University of Surrey, Surrey, UK, 2020. [Google Scholar]
- Zhang, X.; Liu, J.; Han, L.; Xia, S.; Li, S.; Li, O.; Kassegne, K.; Li, M.; Yin, K.; Hu, Q.; et al. Towards a global One Health index: A potential assessment tool for One Health performance. Infectious diseases of poverty. Infect. Dis. Poverty 2022, 11, 12–26. [Google Scholar] [CrossRef]
- Zhou, N.; Cheng, Z.; Zhang, X.; Lv, C.; Guo, C.; Liu, H.; Dong, K.; Zhang, Y.; Liu, C.; Chang, Y.F.; et al. Global antimicrobial resistance: A system-wide comprehensive investigation using the Global One Health Index. Infect. Dis. Poverty 2022, 11, 92. [Google Scholar] [CrossRef]

| S. No. | Measures Implemented | Advantages of Implementation | Disadvantages of Implementation |
|---|---|---|---|
| 1. | Antibiotic stewardship programs | These programs involve the development of guidelines for antibiotic prescribing, education for healthcare professionals, and regular monitoring of antibiotic use to ensure that these medications are used appropriately and only when necessary. | Some hospitals may face challenges in effectively implementing antibiotic stewardship programs due to resource constraints, lack of dedicated personnel, or resistance from healthcare professionals. |
| 2. | Infection Prevention and Control Practices | Healthcare workers are trained to adhere to strict hand hygiene protocols, including the use of hand sanitizers and thorough handwashing techniques. Infected or colonized patients may be placed in isolation to prevent the transmission of MDR bacteria. Healthcare workers may use PPE, such as gloves and gowns, when caring for patients with multidrug-resistant infections to minimize the risk of contamination. | Achieving consistent compliance with hand hygiene protocols can be challenging. Placing patients in isolation may negatively impact their psychological well-being and overall experience. The consistent use of PPE can be resource-intensive, requiring a constant supply of gloves, gowns, masks, and other protective gear. |
| 3. | Environmental cleaning and disinfection | Rigorous cleaning and disinfection of hospital environments are crucial to eliminate MDR bacteria on surfaces. | Certain MDR bacteria, such as C. difficile, can form spores that are resistant to many disinfectants. |
| 4. | Screening and surveillance programs | Hospitals may implement active surveillance programs to identify patients carrying MDR bacteria upon admission. | False negatives can occur, leading to potential underestimation of the actual prevalence. |
| 5. | Patient and staff education | Hospitals conduct educational programs for both healthcare staff and patients to raise awareness about the importance of infection prevention, proper antibiotic use. | The impact of educational programs on long-term behavior change may be challenging to sustain. |
| 6. | Research and surveillance | Ongoing research and surveillance efforts are critical to monitor the prevalence of MDR strains, understand emerging resistance patterns, and adapt control measures accordingly. | Ongoing research and surveillance efforts require substantial resources, including funding, skilled personnel, and advanced laboratory facilities. |
| 7. | Collaboration and communication | Hospitals often collaborate with local, national, and international health agencies to share information, best practices, and strategies for managing MDR bacteria. | Coordinating collaboration among various healthcare facilities, agencies, and jurisdictions can be challenging. |
| Pathogen | ASP Implementation Period | Description/ Specification | Results | Reference |
|---|---|---|---|---|
| E. faecium | 3 years (2014–2017) | The study on VRE treated with daptomycin, a widely used hospital drug experiencing increasing resistance. |
| [44] |
| 3 years (2017–2020) | A study investigating antimicrobial use and antimicrobial resistance in E. faecium with higher consumption of antimicrobials, particularly ceftriaxone, piperacillin/tazobactam, gentamicin, ciprofloxacin and meropenem |
| [45] | |
| S. aureus | 30 days (2015) | In a study involving 170 patients diagnosed with SAB, two groups were established: a pre-intervention group consisting of 82 patients and an ASP-intervention group comprising 88 patients. |
| [46] |
| 7 years (2014–2021) | A study conducted in the Lleida health region of north-eastern Spain primarily consisting of educational advisories related to positive microbiological samples for S. aureus, though interrupted in 2020 due to the SARS-CoV-2 pandemic. |
| [47] | |
| K. pneumoniae | 4 years (2014–2018) | Out of 2261 patients who underwent open-heart surgery encompassing various procedures including CABG, valvular procedures, thoracic aorta replacements, and other cardiac interventions, 130 (5.7%) were found to be colonized by CR-Kp via systematic screening using rectal swabs or bronchoalveolar lavage. |
| [48] |
| 7 years (2011–2017) | Seven-year analysis by Zhang et al. of a leading tertiary care hospital in northwest China post-implementation of the national ASP revealed mixed positive and negative outcomes. |
| [49] | |
| 10 months (2009) | Marra et al. reported promising outcomes of an educational intervention promoting new antibiotic protocols in a Brazilian ICU ward, with favorable results observed in a comparison before and after the intervention. |
| [50] | |
| A. baumannii | 6 years (2014–2020) | The study demonstrates that the introduction of an ASP resulted in significant reductions in the utilization of various antibiotics, notably imipenem/cilastatin, carbapenems, vancomycin, colistin, and third-generation cephalosporins. |
| [51] |
| 6 years (2014–2020) | The antimicrobial stewardship team involved in this study began daily assessments of broad-spectrum antibiotic usage in January 2019, and introduced the carbapenem-sparing strategy in the ICU from April 2019 onwards. |
| [52] | |
| P. aeruginosa | 3 years (2014–2017) | A three-year study evaluating the implementation of a multimodel ASP demonstrated positive outcomes, with improved susceptibility to specific antimicrobials observed among 6501 clinical isolates of P. aeruginosa collected prospectively from 2014 to 2017, following the initiation of the ASP in August 2015. |
| [53] |
| 3 years (2004–2007) | In the examination of a multimodal ASP implementation for P. aeruginosa, positive outcomes were observed in the temporal relationships between antibiotic use and ICU resistance patterns. |
| [54] | |
| Enterobacter spp. | 2 years (2013–2015) | In a study launched in 2015, a robust ASP was introduced in two of three nursing homes, featuring a one-day training session on an “ASP for nursing homes” and ongoing support and training for the coordinating physician provided by an AMT. |
| [55] |
| 1 year (2020) | In a study of 110 patients, 120 isolates were analyzed, showing a notable decrease in both CPE isolates and carbapenem usage. |
| [56] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ravi, K.; Singh, B. ESKAPE: Navigating the Global Battlefield for Antimicrobial Resistance and Defense in Hospitals. Bacteria 2024, 3, 76-98. https://doi.org/10.3390/bacteria3020006
Ravi K, Singh B. ESKAPE: Navigating the Global Battlefield for Antimicrobial Resistance and Defense in Hospitals. Bacteria. 2024; 3(2):76-98. https://doi.org/10.3390/bacteria3020006
Chicago/Turabian StyleRavi, Kamna, and Baljit Singh. 2024. "ESKAPE: Navigating the Global Battlefield for Antimicrobial Resistance and Defense in Hospitals" Bacteria 3, no. 2: 76-98. https://doi.org/10.3390/bacteria3020006
APA StyleRavi, K., & Singh, B. (2024). ESKAPE: Navigating the Global Battlefield for Antimicrobial Resistance and Defense in Hospitals. Bacteria, 3(2), 76-98. https://doi.org/10.3390/bacteria3020006








