1. Introduction
Education has seen a major change recently in the era of the Fourth Industrial Revolution. “EduTech”, combining education and technology, was newly coined and is now widely used throughout college education [
1,
2,
3,
4]. An array of lesson plans, curriculum, and educational techniques and methodology, backed up with technology, are now being used, and new concepts such as virtual reality (VR) and augmented reality (AR) as well as mixed reality (MR) are also actively applied within educational institutions [
5,
6,
7,
8]. Many educational institutions have introduced non-face-to-face classes due to COVID-19 to curb infectious diseases [
9,
10]. Class platforms such as non-face-to-face real-time recorded classes and metaverse classes are also gaining attention. Papers on classes that introduce the latest technology have been widely reported since 2019, and several EduTech-related companies have also emerged, and their corporate values have gained notoriety as well [
11,
12]. Virtual reality (VR) has been highlighted as it can be easily applied to education and is highly useful for non-face-to-face classes among others [
13,
14,
15].
The adage, “Seeing is believing”, is now being replaced by, “Doing is believing”, which indicates the importance of hands-on activities. In the COVID-19 era, where communication between educators and learners is limited, VR is expected to greatly contribute to improving the efficiency of education [
15]. VR has been widely applied across various education fields such as medical education, physical education, industrial engineering, computer engineering, and art [
13,
16,
17,
18,
19]. For medical education, VR can be highly useful in medical data visualization, surgery planning, training, and anatomy study [
20,
21,
22,
23,
24,
25,
26]. Stanford University School of Medicine is already using VR for training in its Neurosurgical Simulation [
27], and the University of California, San Francisco, and the University of Michigan have utilized VR within an anatomy class [
28,
29]. VR is widely used in medical school education to study the structure of the human body because it can create and show the world around you in 3D [
30]. VR is an ideal and effective educational tool where practicum and hands-on activities, which generally entail considerable expense are crucial. VR also overcomes the limitations of time and space that enables people to participate from distance and to easily grasp spatial/structural information through three-dimensional visualization [
31,
32,
33,
34,
35]. In addition, VR makes accessing clinical experiences simple, repeatable, and flexible, allowing the integration of simulation-based education for the learners with reducing costs from the institutional standpoint.
For anatomy education, human body models, practice videos, and cadavers are the main teaching aids. Recently, a mixed-methods study on using a 3D skull model to improve traditional anatomy education programs, and this paper concluded that the skull virtual learning resource was equally as efficient as the cadaver skull and atlas in teaching anatomy structure [
36].
In Korea, most medical school/college has traditional anatomy education class using cadavers (1 cadaver for around 10 students). Most faculty members pointed out that the number of cadavers is not sufficient for the anatomy practice. In addition, the COVID-19 pandemic made it more difficult to collect cadavers. From this point of view, the development of a new education strategy for the anatomy practice is needed. Herein, we introduce a blended (hybrid) anatomy class, whole-body gross anatomy and VR-based anatomy, conducted at the College of Medicine of Kyung Hee University (Seoul, Republic of Korea in 2021). VR was introduced to the existing gross anatomy class, and the state-of-the-art VR anatomy devices and programs were employed in addition to the traditional cadaver dissection. This is the first trial of its kind in Korean medical schools, and this paper specifies the class methods, analysis of strengths and weaknesses of VR introduction, and VR development plans. The class was designed and conducted for 95 students at the College of Medicine of Kyung Hee University. In this study, we aimed to figure out that the VR could be used as a new tool for anatomy education to improve learning efficiency in the COVID-19 pandemic as well as post-pandemic and understand the educational effect of the adaption of high-tech educational tools to the medical class.
2. Materials and Methods
Cadaver procurement for gross anatomy was carried out by the Department of Medicine with the approval of the IRB board. Students and professors wore personal protective equipment (gloves, medical gown, arm sleeves, a medical cap, a mask, goggles) to ensure personal safety during the practice during the COVID-19 pandemic. The VR-introduced anatomy dissection class was conceptualized by the researchers (D.K., Y.H.). The anatomy VR program and devices (VR headset, laptop, cable,) were purchased from an online website. VR devices and anatomy VR programs used for the practice are stated in the “VR set-up” section. All questions proposed by the researchers were selected for review purposes.
2.1. Design of the Study
Details of undergraduate anatomy course before COVID-19 pandemic at Kyung Hee University are as follows: (1) Total hours of lectures: 72 h. (2) Total hours of laboratories: 64 h. (3) Use of cadavers: dissection and pro-section. (4) Types of instructions: flip-leaning, classroom lecture, training lecture, discussion, examination (mid-term, final-term), and image-based formative evaluation. (5) Resources: textbook, power points slide, and video clips (training lecture). (6) Methods of assessment: theory (mid-term, final-term) and laboratory (final-term).
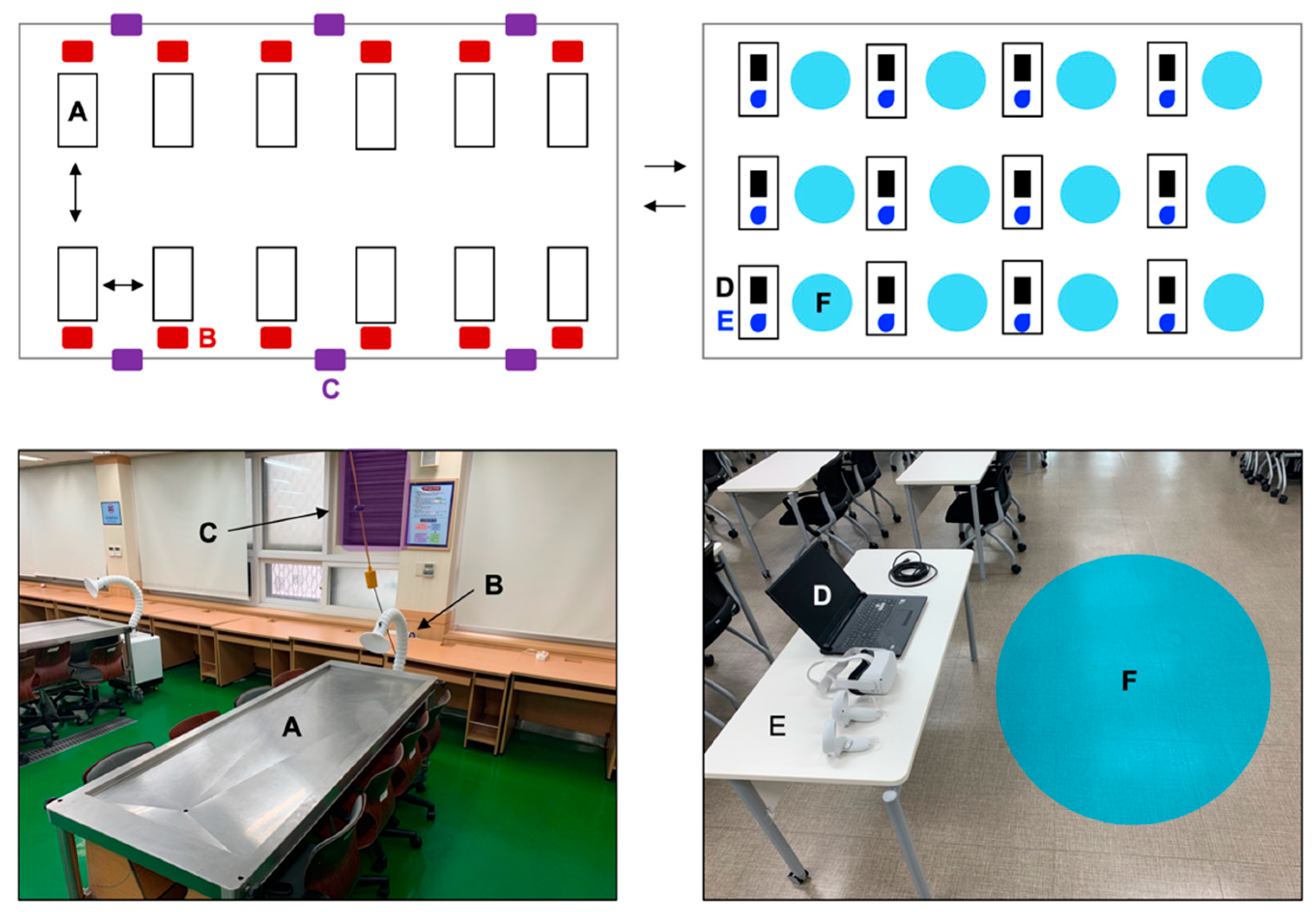
Design of the study during COVID-19 pandemic: The class was delivered in two practicum rooms (
Figure 1). Room 1: this room was used for the gross anatomy class. The 95 students (age: 20–22, sex: 68 male, 27 female, experience with anatomy class: 10, experience with anatomy with VR: none) were divided into 12 teams with one team per cadaver. The cadavers were donated (aged from the 50 s to 80 s). Four anatomy professors and 1 endocrinology professor conducted the class, providing the list of the structures, and the students then located the structures during the cadaver practice and VR-assisted class. Considering the COVID-19 situation, a local ventilation system and air extractor were installed for protection, along with the personal protective equipment (PPE) use, and each dissection table was arranged 2–3 m apart from each other. Room 2: this room was used for the practice class by using the VR devices and programs. A total of 12 desks and 12 VR set-ups (VR headset, laptop, controller, cable) were prepared. VR set-ups were placed on each desk arranged in a way to secure a sufficient workspace. Students could borrow VR equipment after getting professors’ permission and use it away from the institution at their place and time of day. Except for the classroom setting, the others are the same as the before COVID-19 pandemic. Total hours of laboratories (Room 1: 14 h average, Room 2: 50 h average).
The students conducted gross anatomy and used VR for the following purposes: (1) to preview and understand the location of human structures before the practice. (2) to classify human structures that were missed or difficult to construct during the gross anatomy practice considering the age of most cadavers. (3) to identify the small structures that are difficult to observe during the gross anatomy practice. (4) to construct the three-dimensional aspect of human structures that cannot be classify during the gross anatomy practice. (5) to identify the structures (genital organs, etc.) that cannot be observed, dependent on the gender of the cadaver. (6) to explain the physiological and biochemical aspects of the disease-induced internal organ damage.
Practices were mainly conducted in Room 1. The VR induction training was provided 30 min before the practice by experienced teaching assistants (5 people) and assistance was given when needed. Practices were conducted with extra precautions considering the COVID-19 situation in both rooms.
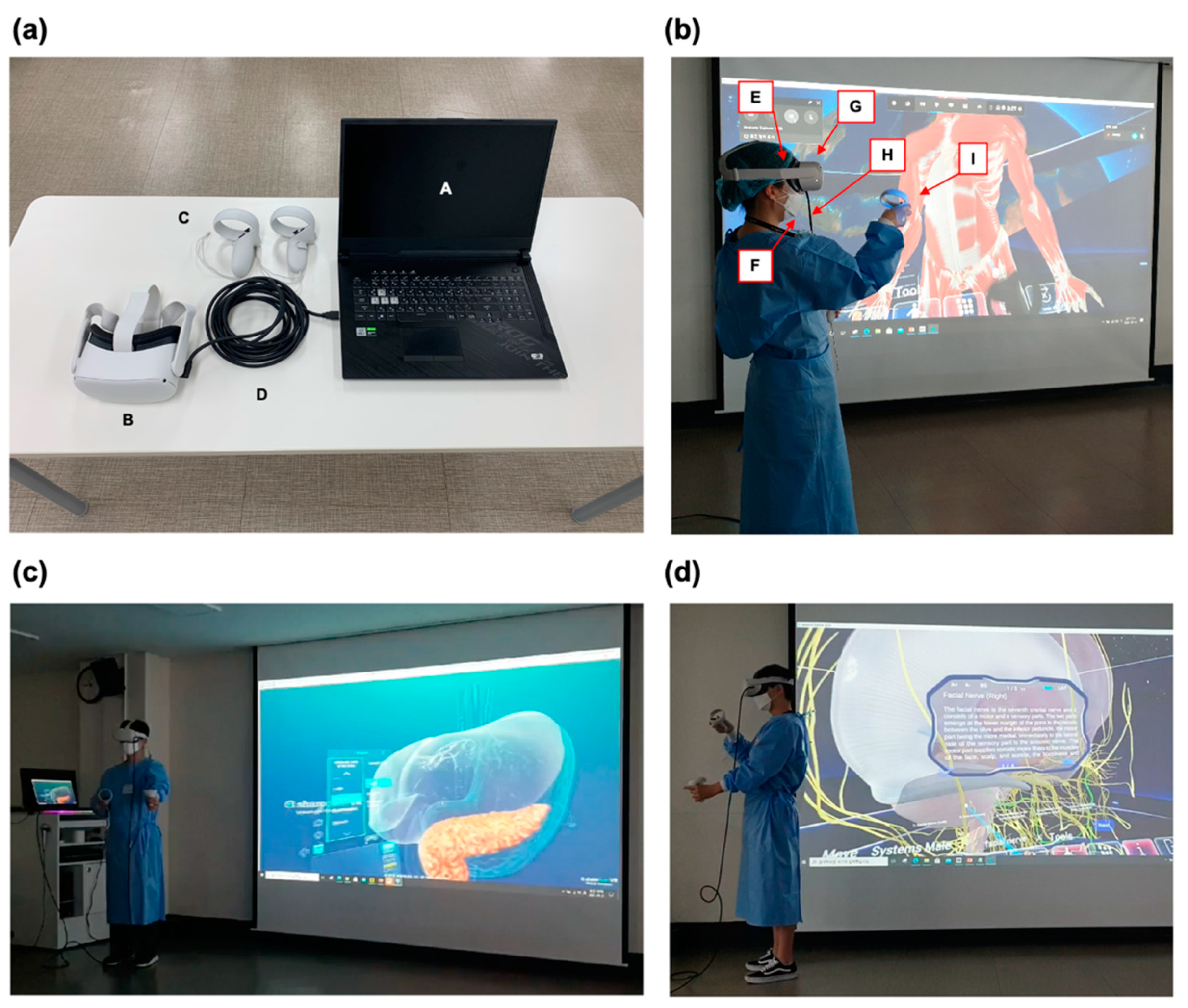
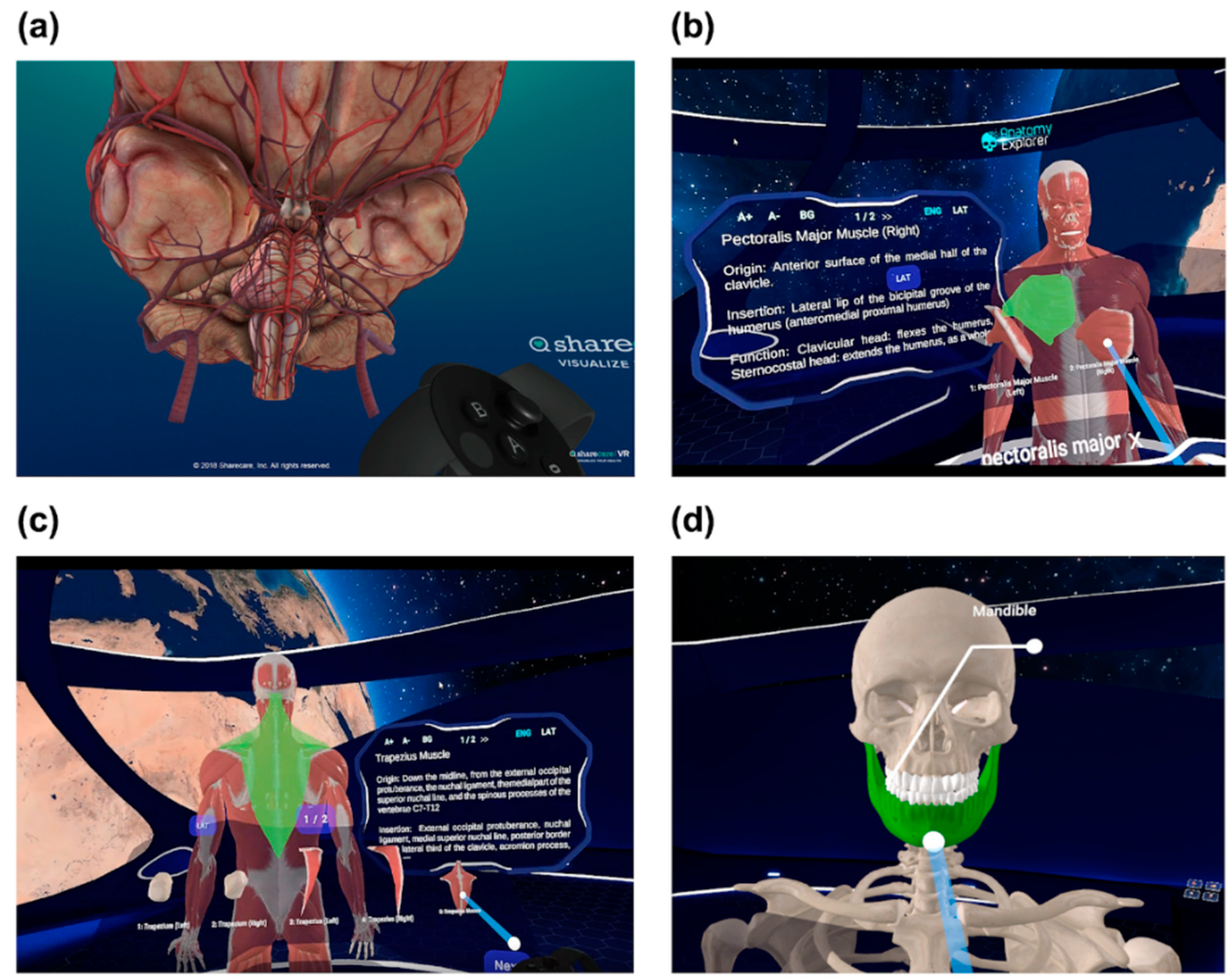
2.2. Blended Gross Anatomy Class
Gross anatomy practice and VR-based anatomy practice was conducted in Room 1 and 2, respectively. Students first practiced gross anatomy in Room 1 and then moved to Room 2 for VR-assisted practice. As stated in
Table 1, two VR anatomy programs used in this class have different purposes (
Figure 2 and
Figure 3). Program Sharecare You has a good database for checking internal organs (brain, heart, lung, liver, kidney, pancreas, etc.) (HMD: Oculus, 2020), but has limitations with learning muscles, bones, blood vessels, or nerves. Anatomy Explorer specializes in the observation of muscles, bones, blood vessels, and nerves, but has limitations in observing internal organs (HMD: Oculus, 2020). These two programs can be complementary to each other.
Students were asked to submit a PowerPoint (Microsoft PowerPoint, Microsoft, Redmond, Seattle, WA, USA) slides report comparing cadaver photos in Room 1, screenshots, and videos of VR anatomy practice in Room 2, and photos from an anatomy textbook (Ethical approval for taking picture of cadavers: Document No. 2021-129). The submitted PowerPoint slides were used for the formative evaluation and final examination.
The Professor provided a list of 150 structures (a rough guide) for the students to study one month before the practice. The structure dissection sequence could then be decided before the practice by students after a group discussion. Students were asked to provide opinions (strengths, weaknesses, and any improvement points for the VR set-up and program) on how the VR practice could contribute to the anatomy practice, and each sequence was set and controlled by their own group. As the professors did not engage in deciding the dissection practice sequence, they asked each group to check how the VR practice helped them during the practice.
2.3. Virtual Reality Set-up
One of the most important factors to consider for the VR technique introduction to the anatomy class was a VR device. We needed to purchase the best-performing VR device that was commercially available and within a limited budget. We listed the VR devices and analyzed their characteristics, platforms, and prices (
Table 2). Another factor to consider was if the device was a PCVR (VR requiring personal computer), as most of the VR anatomy programs can run only on a PCVR. Most of the VR devices in the market have head-mounted displays and PCVR functions with each VR manufacturer operating its own platform. The VR price varies from USD 400 to USD 2000. We chose Quest 2 (Oculus Quest 2, Meta Quest, Menlo Park, CA, USA) by Oculus (
Figure 2a). This model functions both as a PCVR and a standalone VR, which enables the user to enjoy the VR technology without needing to be connected to a smartphone or computer. It also has a good picture quality considering the price and high compatibility with VR anatomy programs.
Running VR anatomy programs requires a laptop equipped with a high-performance graphics processing unit (GPU) Oculus Quest 2 is a standalone VR, but as most VR anatomy programs require a connection through a computer, we listed all laptops equipped with a central processing unit (CPU) Core-i7-10th generation, solid-state drive (SSD) 512 GB, Memory DDR4 (8G), USB 3.1 Type-C, and we chose the ROG STRIX G model (STRIX G17, Asus, Taipei, Taiwan) for the class (
Figure 2a, GPU: Core-i7-10th generation GPU (GTX1660 Ti), SSD: 970 PRO M.2 PCle NVME (Samsung electronics, Suwon, Rep. of Korea), DDR4: PC3-12800 (Samsung electronics, Suwon, Rep. of Korea)). Connecting the VR Head-mounted display (HMD) to a laptop (ROG STRIC G model), requires a long cable to enable the free movement of students in the workspace during practice. However, the image transmission efficiency from the laptop to VR HMD deteriorates significantly if the cable length exceeds 5 m (m), so we chose a 5 m cable (
Figure 2a, Oculus Link cable, Meta Quest, Menlo Park, CA, USA). As a precaution to the COVID-19 pandemic, we prepared disposable VR masks (AMVR 100 pcs disposable VR face mask, Amazon, Seattle, WA, USA) for VR HMD (
Figure 2b) and made it mandatory to wear a medical gown and a face mask during the practice.
VR anatomy programs that can run on Oculus Quest 2, including (1) 3D organon VR (3D organon VR anatomy Standard, 3D Organon, San Francisco, CA, USA), (2) Anatomy Explorer 2020 (Anatomy Explorer 2020, Virtual Medicine, Bratislava, Slovakia), (3) Sharecare You (Sharecare You VR Standard, Sharecare, Atlanta, GA, USA), and (4) VEDAVI VR human anatomy (VEDAVI VR Human Anatomy, VEDAVI Medical, Susenbergstrasse, Zurich, Swiss) (
Table 1,
Figure 3).
2.4. Survey
An anonymous survey was conducted with the students after the practices. A total of 95 students (95% of the total students, regular anatomy class of the medicine department, third-grader) participated in the survey. The survey questionnaire (delivered to the participants by hard copy) consists of ten Likert scale questions and three essay questions. On Likert scale question, students were asked to rate the VR program and the practice class on a scale of 1 to 5 (1 = very dissatisfied, 5 = very satisfied). In the essay questions, the students were asked to write their opinions about the blended class, its strengths, weaknesses, and any improvement points for the VR set-up and program.
2.5. Statistical Analysis
All contributors agreed on the survey after the anatomy dissection class. Statistical analysis was conducted using the Likert scale questions survey (10 questions) and statistical software; (i) Prism 8.0 (GraphPad, La Jolla, CA, USA), (ii) Microsoft Excel (Redmond, USA). See the details for the survey in the section “Survey” above.
3. Results
3.1. Likert Scale Questions Survey Results
The survey was collected from 95 students (see the descriptive demographics in the section of Design of the Study) and analyzed after the practice was completed. The summary of survey results is represented in
Figure 4 and
Table 3 (ad-hoc survey, Cronbach’s α: 0.985).
Question 1. Question 1 was regarding the VR setup. When asked about the quality of the display on the VR HMD and the sensitivity of the controller, about 75% of the students rated it as good or very good. However, as most of the students were first-time users of the VR devices, they found it rather difficult to use the device within the program, and about 25% of the students showed moderate or negative opinions. The mean average score of question 1 was 4.03 out of 5 (Likert scale question).
Questions 2 and 3. Questions 2 and 3 were about the program quality to monitor internal organs and disease models. When asked about the display quality of internal organs (Question 2), about 87% of the students gave a positive opinion and about 13% of students gave a moderate or negative opinion. The mean average score of question 2 was 4.27 out of 5 (Likert scale question). When asked about the quality of the disease model (Question 3), about 70% of students gave positive opinions and 30% gave moderate or negative opinions, which is a relatively high ratio compared to other questions. It can be surmised from the essay answers that negative opinions from Question 3 are related to the sense of the human organs and diseases in the programs being too virtual and that the imagery lacks definition and a sense of reality. The mean average score of question 3 was 3.95 out of 5 (Likert scale question).
Questions 4 and 5. Questions 4 (indexes in VR program) and 5 (helpfulness of indexes in VR program) were about the index accuracy of body structures. The question was about the accuracy of the index marked on the human structure and how useful it was to distinguish between the structures that cannot be discerned in an actual cadaver. Most students said that the indices were accurately marked (positive: 94%, average: 6%) and showed a positive opinion rating stating that it helped to find structures in the cadaver with the indices of the VR program (positive: 66%), and a 28% average rating and a 4% who expressed a negative opinion. The mean average score of question 4 and 5 was 4.40 and 3.96 out of 5, respectively (Likert scale question).
Question 6. Question 6 was about how accurately the VR practice program reproduced the anatomy of a real human body, and a high percentage of negative opinions were presented (very negative: 8.4%, negative: 27.3%, average: 28.4%). The mean average score of question 6 was 3.12 out of 5 (Likert scale question).
Question 7. Question 7 was about the price of the VR program. Sharecare You and Anatomy Explorer can be purchased for less than about $50 per computer. About 61% of the students said that the programs were reasonably priced, but some students expressed negative opinions about the price (average: 27%, somewhat expensive: 5%, very expensive: 5%). The mean average score of question 7 was 3.83 out of 5 (Likert scale question). There is a correlation between the program quality and the price. Students who had a positive opinion about the quality and use of the program showed a positive opinion about the price of the program, while the students who had a negative opinion about the program had a negative opinion about the price.
Questions 8 to 10. Questions 8–10 were about the blended anatomy class using VR. Question 8 asked how satisfied the VR-assisted practice was, and about 73% of the students rated positively with 16.8% marking average and 8.4% marking not satisfied. Question 9 asking if the program improved the learning anatomy gained similar results from Question 8. The mean average score of question 8 and 9 was 3.95 and 3.93 out of 5, respectively (Likert scale question). When asked if the students agreed to use the VR system for cadaver anatomy practice as a supplementary learning aid (Question 10), 51% of them said highly agreed with 32% rating agreed, 12 % rating average, and 3% showing a negative reaction. The mean average score of question 10 was 4.31 out of 5 (Likert scale question).
Overall opinions on the VR-based anatomy practice class suggested that most of the students were highly satisfied with the programs and expressed positive opinions, stating that the VR was helpful for the gross anatomy practice using a cadaver. However, a high percentage of respondents felt that the VR-assisted program lacked reality in reproducing the anatomy of the human body due to the disparity between the body model in the VR program and the actual cadaver, which needs improvement.
3.2. Essay Questions Survey Results
Alongside the Likert scale questions, we asked students’ opinions (from 95 students) about the strengths, weaknesses, and improvement points of the VR-assisted anatomy practice in the essay questions. Main keywords derived from the answers, and the detailed explanations for each keyword are described in the following.
Strengths: When asked about the “strength of the VR-assisted anatomy practice”, the main keywords were “Efficient (the number of respondents: 80)”, “Iterative learning (the number of respondents: 72)”, “Easy to find structure (the number of respondents: 65)”, “High accessibility (the number of respondents: 62)”, “Easy disease simulation (the number of respondents: 59)”, “Safe & Clean (the number of respondents: 57)”. Most respondents stated that the biggest advantage of the VR-based anatomy practice lies in its effective and repetitive learning capability. Other most frequently mentioned strengths are as follows: (1) It allows a clear three-dimensional observation of the structures at different locations and angles and can even restore the removed tissue (the number of respondents: 37). The VR strength lies in its ability to enable anyone to find a structure, regardless of the participant’s medical techniques, whereas the cadaver practice is highly dependent on those skills. (2) It is efficient as it is less tiring and less time-consuming (the number of respondents: 35). (3) It easily detects the structures that are hard to find in an actual cadaver (the number of respondents: 32). (4) It is easy to find the observation site through the search function and enables efficient learning through easy access to information on the specific site (the number of respondents: 30). (5) It enables observation of the physiological processes of how organs work in a living body rather than a cadaver (the number of respondents: 30). (6) It is safer and simpler as it does not use the formalin needed for cadaver production (similar opinion with the “Safe & Clean”).
Weaknesses: When asked about the “weakness of the VR-assisted anatomy practice”, the main keywords were “Lack of Detail (the number of respondents: 73)”, “Low Reality (the number of respondents: 72)”, “Difficult Control (the number of respondents: 69)”, “Program Error (the number of respondents: 55)”, “Limitation of Team study (the number of respondents: 49)”, “Dizziness & Fatigue (the number of respondents: 37)”. Weaknesses such as Lack of Detail, Low reality, difficult control, program error stems from its short development history. It has limitations in team study. Metaverse can be applied to the anatomy practice, but it also has limitations mostly due to “Dizziness & Fatigue” caused by the VR program. More than 90% of the students who used the VR anatomy program for more than one hour felt dizziness and fatigue and asked for a break. Other most frequently mentioned weaknesses are as follows: (1) It is excessively simplified and lacks the sense of reality in comparison to an actual cadaver. (2) It does not deliver any physical processes to reach the structure during the anatomy practice. (3) It lacks reality as it does not present any unexpected variables from an actual cadaver. (4) Detailed control for site detection is challenging. (5) Overall device and program quality needs improvement. (6) Long-term use incurs dizziness and fatigue. Although there were opinions about the drawbacks, students gave overall positive responses to the blended gross anatomy class, and that is reflected in the Likert scale questions survey (
Table 3, mean average score over 4 out of 5).
3.3. Improvement Points
When asked about the “improvement points for the VR-assisted anatomy practice”, frequently mentioned points are as follows: (1) It can be used for the cadaver pre-practice, post-practice review, and as a supplementary tool during the practice. (2) More devices can be purchased for students to use during the practice. (3) The curriculum can be revised to improve the use of advanced educational tools such as VR from the first year of Premed. (4) VR programs and systems for group practice can be developed. (5) Haptic-based VR programs functioning via tactile senses can be developed. (6) New programs that can overcome the limitations of the current VR system and equipped with noble functions can be developed. New functions to be considered are; Real images, quiz function, histology data, muscle-motion relationship, fat/skin function, clinical information, more language selection, discussion function, community, and group study. Kyung Hee University is currently developing a program that complements the limits of the existing program and displays both clinical images (MRI, CT, PET, etc.) and cadaver images together on VR display. Through our advanced VR program, the quality of anatomy practice can be significantly improved.
3.4. Formative Evaluation Result
After the blended gross anatomy class based on the traditional cadaver dissection and virtual reality devices, the objective outcomes in terms of image-based formative evaluation were conducted by comparing the test score of Group A (students, n = 118, class in 2020) who trained only by cadaver dissection versus Group B (students, n = 95, class in 2021) who trained by the blended method using cadaver dissection and VR-based training. Both groups had similar difficulty in the test (both years had the same class hours and lab hours). We found that Group B received higher scores (85.28 out of 100, average score) than Group A (79.06 out of 100, average score), and this result represents that the hybrid method could improve the academic efficiency and support the understanding of the three-dimensional (3D) structure of the body.
4. Discussion and Limitation of the Study
The VR-assisted class cannot yet replace the actual cadaver dissection practice, but it can improve the anatomy class by serving as a supplementary practice aid. As the cadaver cannot be restored once damaged, practicing with the VR program is helpful to classify the position of the anatomical structure before the actual cadaver practice. On the other hand, as anatomy on actual human tissues can only be achieved through cadaver practice, the VR practice and cadaver practice can complement each other. In this vein, the VR to teach anatomy has been spotlighted as a powerful learning tool that helps to understand the anatomical structures [
37]. Recently, a pilot study of an anatomy education for medical students in a totally virtual workspace was introduced, but it showed various limitations such as quality of 3D models, technical issues, instrument set-up issues, and learning efficiency [
38].
VR education has room for improvement. In our cases, we conducted a blended gross anatomy class using cadaver dissection with VR-support, and students presented several suggestions to advance VR anatomy education after the class. Firstly, the VR class should be conducted independently from the cadaver practice as the cadaver practice requires a substantial amount of time and concentration. The VR practice after the cadaver practice is also mentally and physically challenging. Utilizing VR in anatomy class can stimulate students’ interests and allow students to have a clearer concept on the overall human anatomy before the actual cadaver practice. Secondly, more VR practice time and VR devices should be provided at the school practice. As each team was allowed only one VR device for an hour, the actual time allocated to each team member was not sufficient to get used to the system. A more refined and intuitive user-friendly VR program can be developed.
In this class, we used four different programs as described above. These programs were chosen by website searches and suggestions from experts in this field (professors, managers in companies). The 3D Organon VR has a high image quality and various tools for anatomy practice, but it is relatively expensive and has limited compatibility for Oculus Quest 2 (in March 2021) and contains some bugs and errors. Thus, we concluded that it was not appropriate for this class (according to the VR experts; VR-based education major). The second-best were Sharecare You VR and Anatomy Explorer 2020 in terms of budget and accessibility and we believed that these two can work in a classroom environment. During the blended gross anatomy class in the COVID-19 pandemic, students had experiences of traditional cadaver dissection with VR-supported training, and satisfaction in most areas was highly investigated. We understand that there are drawbacks, such as the reproducibility of the VR program to the actual cadaver practice, but we believe they will be overcome through program enhancements and updates. To understand the negative opinions from questions 2–6, we have reviewed the students’ answers on the weakness of the VR-assisted practice and concluded that the negative opinions were mainly caused by the images of the VR program being too different from the actual cadaver used for the gross anatomy. The actual cadavers were mostly from older age groups, but the human body model in the VR showed an average body type of men/women in their 20s and 30s. This discrepancy should be considered when developing a new anatomy VR program in the future (the elderly and infants shall be included in the VR program model).
Students suggested ideas for the anatomy program as follows, and it is a good starting point for future implementation based on evidence-based education: pictures of the actual cadaver, scalpel function for the actual sense of cutting, quizzes, histological content, depiction of fat and skin to add reality, additional disease states, and additional physiological contents. As the current VR technology allows single-person practice only, integrating VR education with technology such as the Metaverse that enables group work and simultaneous access for several devices will take VR education into the next level and might replace cadaver practice in the future. In addition, the development of a new program that allows one to show the actual clinical images and cadaver images alongside the VR image could be a watershed moment that can greatly contribute to the anatomy practice class.
This thesis is based on short-term anatomical classes, which has led to a lack of depth in terms of reflective research. The study can be improved if the series of classes is observed for as long as 6 months to see the incremental learning outcomes of the students, therefore gaining more quantitative and qualitative data from these experiments. Additionally, more devices per group can be provided with an advanced software program for future practice. Proper guidance by a VR expert and professors during the class can also facilitate the students’ learning capabilities. Students need access to the VR devices outside of the class time to develop the technical dexterity to fully focus on the practical applications.
5. Conclusions
In this paper, the preparation (device, program, laptop, other set-ups) and implementation process of the blended gross anatomy class introducing VR, its strengths and weaknesses, and improvement points were systematically presented in the context of the Fourth Industrial Revolution and the COVID-19 pandemic. The class introduced VR to the existing gross anatomy lecture, and the state-of-the-art VR anatomy devices and programs were employed for the traditional cadaver dissection. Our report specifies the VR-introduced blended lecture concept to the traditional cadaver dissection and analysis, the results of strengths and weaknesses of VR introduction, satisfaction score of students, and VR development plans. After the blended gross anatomy class, we surveyed (10 questions) the convenience of VR set-up, quality of the VR program, and class satisfaction for the students, and most of the questions were high scores (over 4.0 out of 5 (Likert scale question). Through this lecture, we were able to derive many elements (strong points, drawbacks, future plans), and we believed that the VR-introduced blended gross anatomy class could be used as a powerful tool for anatomy education with a significant educational effect.
Author Contributions
Conceptualization, D.K. and Y.H.; methodology, D.K.; validation, D.K., Y.H. and S.O.C.; formal analysis, N.C., E.K., J.H.A. (Jae Hyun Ahn), J.H.A. (Jae Ha Ahn), J.Y.P., S.H.K., J.H.B., C.P., J.J., S.O.C. and D.K.; investigation, D.K.; resources, D.K.; data curation, N.C., E.K., J.H.A. (Jae Hyun Ahn), J.H.A. (Jae Ha Ahn), J.Y.P., S.H.K., J.H.B., C.P., J.J., S.O.C. and D.K.; writing—original draft preparation, D.K.; writing—review and editing, D.K., Y.H.; visualization, D.K.; supervision, D.K., Y.H.; project administration, D.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Rep. of Korea, and approved by the Institutional Review Board (and Ethics Committee) of Kyung Hee University, College of Medicine (Ethical approval for cadaver dissection and related research projects; Ethics Committee on Human Research, Document No. 2021-129 (Date: 4 April 2021) and 2021-299 (Date: 10 June 2021)). The blended anatomy class is integrated into the regular curriculum of the medicine department. The consent of students and ethical approval was obtained before the class. The ethics approval information included study, recruiting student participants, collecting survey responses, etc.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
The authors would like to express their sincerest gratitude to the VR/AR TF team at Kyung Hee University and Support Program for University Development.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Larson, R.C.; Strehle, G.P. Edu-tech: What’sa president to do. Technol. Enhanc. Learn. Oppor. Change 2002, 21–59. [Google Scholar]
- Trelease, R.B. From chalkboard, slides, and paper to e-learning: How computing technologies have transformed anatomical sciences education. Anat. Sci. Educ. 2016, 9, 583–602. [Google Scholar] [CrossRef] [PubMed]
- Shwab, K. The Fourth Industrial Revolution: What It Means, How to Respond; World Economic Forum: Cologny, Switzerland, 2016. [Google Scholar]
- Garcia Barrios, A.; Cisneros Gimeno, A.I.; Garza García, M.C.; Lamiquiz Moneo, I.; Whyte Orozco, J. Online Teaching Alternative in Human Anatomy. Anatomia 2022, 1, 86–90. [Google Scholar] [CrossRef]
- Hsieh, M.-C.; Lee, J.-J. Preliminary study of VR and AR applications in medical and healthcare education. J. Nurs. Health Stud. 2018, 3, 1. [Google Scholar] [CrossRef]
- Daling, L.M.; Khodaei, S.; Thurner, S.; Abdelrazeq, A.; Isenhardt, I. A Decision Matrix for Implementing AR, 360° and VR Experiences into Mining Engineering Education. In Proceedings of International Conference on Human-Computer Interaction, Málaga, Spain, 22–24 September 2021; Springer: Berlin/Heidelberg, Germany; pp. 225–232. [Google Scholar]
- Chytas, D.; Johnson, E.O.; Piagkou, M.; Mazarakis, A.; Babis, G.C.; Chronopoulos, E.; Nikolaou, V.S.; Lazaridis, N.; Natsis, K. The role of augmented reality in Anatomical education: An overview. Ann. Anat. Anat. Anz. 2020, 229, 151463. [Google Scholar] [CrossRef]
- Taylor, L.; Dyer, T.; Al-Azzawi, M.; Smith, C.; Nzeako, O.; Shah, Z. Extended reality anatomy undergraduate teaching: A literature review on an alternative method of learning. Ann. Anat. Anat. Anz. 2022, 239, 151817. [Google Scholar] [CrossRef]
- Caruso, J.; Harmon, L.; Born, G.; Dufeau, D. Efficacy and Benefits of Augmented and Virtual Reality Based Learning during COVID-19. FASEB J. 2021, 35. Available online: https://faseb.onlinelibrary.wiley.com/doi/10.1096/fasebj.2021.35.S1.04933 (accessed on 13 September 2022). [CrossRef]
- Mateen, M.; Kan, C.Y.P. Education during COVID-19: Ready, headset, go! Clin. Teach. 2021, 18, 90–91. [Google Scholar] [CrossRef]
- Daniel, S.J. Education and the COVID-19 pandemic. Prospects 2020, 49, 91–96. [Google Scholar] [CrossRef] [Green Version]
- Rose, S. Medical student education in the time of COVID-19. JAMA 2020, 323, 2131–2132. [Google Scholar] [CrossRef]
- Ahir, K.; Govani, K.; Gajera, R.; Shah, M. Application on virtual reality for enhanced education learning, military training and sports. Augment. Hum. Res. 2020, 5, 7. [Google Scholar] [CrossRef]
- Liagkou, V.; Salmas, D.; Stylios, C. Realizing virtual reality learning environment for industry 4.0. Procedia Cirp 2019, 79, 712–717. [Google Scholar] [CrossRef]
- Singh, R.P.; Javaid, M.; Kataria, R.; Tyagi, M.; Haleem, A.; Suman, R. Significant applications of virtual reality for COVID-19 pandemic. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 661–664. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, H.; Allaf, M.; Elghazaly, H. COVID-19 and medical education. Lancet Infect. Dis. 2020, 20, 777–778. [Google Scholar] [CrossRef] [Green Version]
- Bäck, R.; Plecher, D.A.; Wenrich, R.; Dorner, B.; Klinker, G. Mixed reality in art education. In Proceedings of 2019 IEEE Conference on Virtual Reality and 3D User Interfaces (VR), Osaka, Japan, 23–27 March 2019; IEEE: New York, NY, USA; pp. 1583–1587. [Google Scholar]
- Pouliquen, M.; Bernard, A.; Marsot, J.; Chodorge, L. Virtual hands and virtual reality multimodal platform to design safer industrial systems. Comput. Ind. 2007, 58, 46–56. [Google Scholar] [CrossRef]
- Zhang, K.; Liu, S.-J. The application of virtual reality technology in physical education teaching and training. In Proceedings of 2016 IEEE International Conference on Service Operations and Logistics, and Informatics (SOLI), Beijing, China, 10–12 July 2016; IEEE: New York, NY, USA; pp. 245–248. [Google Scholar]
- Khalil, M.; Lamar, C.; Johnson, T. Using computer-based interactive imagery strategies for designing instructional anatomy programs. Clin. Anat. Off. J. Am. Assoc. Clin. Anat. Br. Assoc. Clin. Anat. 2005, 18, 68–76. [Google Scholar] [CrossRef]
- Pereira, J.A.; Pleguezuelos, E.; Merí, A.; Molina-Ros, A.; Molina-Tomás, M.C.; Masdeu, C. Effectiveness of using blended learning strategies for teaching and learning human anatomy. Med. Educ. 2007, 41, 189–195. [Google Scholar] [CrossRef]
- Green, R.A.; Whitburn, L.Y. Impact of introduction of blended learning in gross anatomy on student outcomes. Anat. Sci. Educ. 2016, 9, 422–430. [Google Scholar] [CrossRef]
- Kharb, P.; Samanta, P.P. Blended learning approach for teaching and learning anatomy: Students’ and teachers’ perspective. J. Anat. Soc. India 2016, 65, 43–47. [Google Scholar] [CrossRef]
- Kurul, R.; Ögün, M.N.; Neriman Narin, A.; Avci, Ş.; Yazgan, B. An alternative method for anatomy training: Immersive virtual reality. Anat. Sci. Educ. 2020, 13, 648–656. [Google Scholar] [CrossRef]
- Wainman, B.; Aggarwal, A.; Birk, S.K.; Gill, J.S.; Hass, K.S.; Fenesi, B. Virtual dissection: An interactive anatomy learning tool. Anat. Sci. Educ. 2021, 14, 788–798. [Google Scholar] [CrossRef]
- Gloy, K.; Weyhe, P.; Nerenz, E.; Kaluschke, M.; Uslar, V.; Zachmann, G.; Weyhe, D. Immersive anatomy atlas: Learning factual medical knowledge in a virtual reality environment. Anat. Sci. Educ. 2022, 15, 360–368. [Google Scholar] [CrossRef]
- Chan, S.; Conti, F.; Salisbury, K.; Blevins, N.H. Virtual reality simulation in neurosurgery: Technologies and evolution. Neurosurgery 2013, 72, A154–A164. [Google Scholar] [CrossRef] [PubMed]
- UCSF Medical Education School of Medicine, VR for Anatomy, Innovations Lab. 2019. Available online: https://meded.ucsf.edu/tee/innovations (accessed on 13 September 2022).
- Micihgan Today, Virtual Reality. 2019. Available online: https://michigantoday.umich.edu/2019/09/26/virtual-reality/ (accessed on 13 September 2022).
- Codd, A.M.; Choudhury, B. Virtual reality anatomy: Is it comparable with traditional methods in the teaching of human forearm musculoskeletal anatomy? Anat. Sci. Educ. 2011, 4, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Vozenilek, J.; Huff, J.S.; Reznek, M.; Gordon, J.A. See one, do one, teach one: Advanced technology in medical education. Acad. Emerg. Med. 2004, 11, 1149–1154. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, N.; Wilson, T.D. A head in virtual reality: Development of a dynamic head and neck model. Anat. Sci. Educ. 2009, 2, 294–301. [Google Scholar] [CrossRef]
- Falah, J.; Khan, S.; Alfalah, T.; Alfalah, S.F.; Chan, W.; Harrison, D.K.; Charissis, V. Virtual Reality medical training system for anatomy education. In Proceedings of 2014 Science and Information Conference, London, UK, 27–29 August 2014; IEEE: New York, NY, USA; pp. 752–758. [Google Scholar]
- Schott, C.; Marshall, S. Virtual reality and situated experiential education: A conceptualization and exploratory trial. J. Comput. Assist. Learn. 2018, 34, 843–852. [Google Scholar] [CrossRef]
- Zhao, J.; Xu, X.; Jiang, H.; Ding, Y. The effectiveness of virtual reality-based technology on anatomy teaching: A meta-analysis of randomized controlled studies. BMC Med. Educ. 2020, 20, 127. [Google Scholar] [CrossRef]
- Chen, S.; Zhu, J.; Cheng, C.; Pan, Z.; Liu, L.; Du, J.; Shen, X.; Shen, Z.; Zhu, H.; Liu, J.; et al. Can virtual reality improve traditional anatomical education? A randomized controlled trial on use of 3D skull model. BMC Med. Educ. 2020, 20, 395. [Google Scholar] [CrossRef]
- Fairén González, M.; Farrés, M.; Moyes Ardiaca, J.; Insa, E. Virtual reality to teach anatomy. In Eurographics 2017: Education Papers; European Association for Computer Graphics (Eurographics): Reims, France, 2017; pp. 51–58. [Google Scholar]
- Nakai, K.; Terada, S.; Takahara, A.; Hage, D.; Tubbs, R.S.; Iwanaga, J. Anatomy education for medical students in a virtual reality workspace: A pilot study. Clin. Anat. 2022, 35, 40–44. [Google Scholar] [CrossRef]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).