Trends of Cause-Specific Mortality and Association with Economic Status, Education Level, as Well as Health Investment among Adolescents Aged 10 to 24 Years in China, 2004–2019
Abstract
:1. Introduction
- Question: How have adolescent mortality rates and death patterns changed in China and what factors were associated with the changes?
- Findings: This study found significant reductions in adolescent all-cause mortality, but some causes, such as HIV/AIDS, malnutrition, lymphoma, and multiple myeloma had higher burdens in 2019 than in 2004, while subgroup differences still existed. Increasing health investment might contribute to decreasing trends in deaths.
- Interpretation: It will be important to prioritize interventions based on the specific causes of death and associated patterns to ensure that no one is left behind.
2. Methods
2.1. Data Sources
2.2. Data Recode
2.3. Statistical Analysis
2.3.1. The Trend for All-Cause Mortality and Cause-Specific Mortality
2.3.2. Association between Mortality and Economic Status, Education Level, as Well as Health Investment
2.4. Sensitivity Analysis
3. Results
3.1. Current Status of Mortality among Adolescents Aged 10 to 24 Years
3.2. The Trend of Mortality among Adolescents Aged 10 to 24 Years, 2004–2019
3.3. APC Analysis of Mortality among Adolescents Aged 10 to 24 Years, 2004–2019
3.4. Overall Status of Cause-Specific Mortality among Adolescents Aged 10 to 24 Years, 2004–2019
3.5. Status of Cause-Specific Mortality by Gender and Areas
3.6. Status of Cause-Specific Mortality by Region
3.7. Status of Cause-Specific Mortality by Age Group
3.8. Association between Mortality and Economic Status, Education Level, as Well as Health Investment
4. Discussion
5. Limitations and Future Reflections
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Millennium Development Goals (MDGs). Available online: https://www.who.int/news-room/fact-sheets/detail/millennium-development-goals-(mdgs) (accessed on 29 September 2023).
- Sustainable Development Goals: 17 Goals to Transform Our World. Available online: https://www.un.org/sustainabledevelopment/ (accessed on 14 February 2023).
- Kassebaum, N.; Kyu, H.H.; Zoeckler, L.; Olsen, H.E.; Thomas, K.; Pinho, C.; Bhutta, Z.A.; Dandona, L.; Ferrari, A.; Ghiwot, T.T.; et al. Child and Adolescent Health from 1990 to 2015: Findings from the Global Burden of Diseases, Injuries, and Risk Factors 2015 Study. JAMA Pediatr. 2017, 171, 573–592. [Google Scholar] [CrossRef] [PubMed]
- Patton, G.C.; Sawyer, S.M.; Santelli, J.S.; Ross, D.A.; Afifi, R.; Allen, N.B.; Arora, M.; Azzopardi, P.; Baldwin, W.; Bonell, C.; et al. Our future: A Lancet commission on adolescent health and wellbeing. Lancet 2016, 387, 2423–2478. [Google Scholar] [CrossRef]
- Global Strategy for Women’s, Children’s and Adolescents’ Health Data Portal. Available online: https://platform.who.int/data/maternal-newborn-child-adolescent-ageing/global-strategy-data (accessed on 16 February 2023).
- Global Accelerated Action for the Health of Adolescents (AA-HA!): Guidance to Support Country Implementation. Available online: https://www.who.int/publications/i/item/9789241512343 (accessed on 20 September 2023).
- Sawyer, S.M.; Azzopardi, P.S.; Wickremarathne, D.; Patton, G.C. The age of adolescence. Lancet Child Adolesc. Health 2018, 2, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Azzopardi, P.S.; Hearps, S.J.; Francis, K.L.; Kennedy, E.C.; Mokdad, A.H.; Kassebaum, N.J.; Lim, S.; Irvine, C.M.; Vos, T.; Brown, A.D.; et al. Progress in adolescent health and wellbeing: Tracking 12 headline indicators for 195 countries and territories, 1990–2016. Lancet 2019, 393, 1101–1118. [Google Scholar] [CrossRef]
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Boonen, T.J.; Li, H. Modeling and Forecasting Mortality with Economic Growth: A Multipopulation Approach. Demography 2017, 54, 1921–1946. [Google Scholar] [CrossRef]
- Gavurova, B.; Khouri, S.; Kovac, V.; Ferkova, M. Exploration of Influence of Socioeconomic Determinants on Mortality in the European Union. Int. J. Environ. Res. Public Health 2020, 17, 4699. [Google Scholar] [CrossRef] [PubMed]
- Honjo, K.; Iso, H.; Fukuda, Y.; Nishi, N.; Nakaya, T.; Fujino, Y.; Tanabe, N.; Suzuki, S.; Subramanian, S.V.; Tamakoshi, A.; et al. Influence of Municipal- and Individual-level Socioeconomic Conditions on Mortality in Japan. Int. J. Behav. Med. 2014, 21, 737–749. [Google Scholar] [CrossRef] [PubMed]
- Edney, L.C.; Haji Ali Afzali, H.; Cheng, T.C.; Karnon, J. Mortality reductions from marginal increases in public spending on health. Health Policy 2018, 122, 892–899. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Wu, X.; Lopez, A.D.; Wang, L.; Cai, Y.; Page, A.; Yin, P.; Liu, Y.; Li, Y.; Liu, J.; et al. An integrated national mortality surveillance system for death registration and mortality surveillance, China. Bull. World Health Organ. 2016, 94, 46–57. [Google Scholar] [CrossRef]
- Yang, G.; Hu, J.; Rao, K.Q.; Ma, J.; Rao, C.; Lopez, A.D. Mortality registration and surveillance in China: History, current situation and challenges. Popul. Health Metr. 2005, 3, 3. [Google Scholar] [CrossRef] [PubMed]
- Zhou, M.; Wang, H.; Zhu, J.; Chen, W.; Wang, L.; Liu, S.; Li, Y.; Wang, L.; Liu, Y.; Yin, P.; et al. Cause-specific mortality for 240 causes in China during 1990–2013: A systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet 2016, 387, 251–272. [Google Scholar] [CrossRef] [PubMed]
- Chinese Center for Disease Control and Prevention CfCN-CDC. National Disease Surveillance System Cause of Death Surveillance Data Set 2004; Military Medical Science Press: Beijing, China, 2009. (In Chinese) [Google Scholar]
- Chinese Center for Disease Control and Prevention CfCN-CDC; NCHS Statistical Information Center. China Cause of Death Surveillance Dataset 2019; China Science and Technology Press: Beijing, China, 2020. (In Chinese) [Google Scholar]
- Age-Period-Cohort Analysis. Available online: https://www.publichealth.columbia.edu/research/population-health-methods/age-period-cohort-analysis#Description (accessed on 15 April 2023).
- Yang, Y.; Land, K.C. Age-Period-Cohort Analysis: New Models, Methods, and Empirical Applications, 1st ed.; Chapman and Hall/CRC: Boca Raton, FL, USA, 2013. [Google Scholar]
- Rosenberg, P.S.; Anderson, W.F. Age-period-cohort models in cancer surveillance research: Ready for prime time? Cancer Epidemiol. Biomark. Prev. 2011, 20, 1263–1268. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, P.S.; Check, D.P.; Anderson, W.F. A web tool for age-period-cohort analysis of cancer incidence and mortality rates. Cancer Epidemiol. Biomark. Prev. 2014, 23, 2296–2302. [Google Scholar] [CrossRef]
- Ho, T.C.; Gifuni, A.J.; Gotlib, I.H. Psychobiological risk factors for suicidal thoughts and behaviors in adolescence: A consideration of the role of puberty. Mol. Psychiatry 2022, 27, 606–623. [Google Scholar] [CrossRef] [PubMed]
- Luo, D.M.; Yan, X.J.; Lei, Y.T.; Hu, P.J.; Zhang, J.S.; Song, Y.; Ma, J. Secular trends and geographic disparities of all-cause mortality among Chinese adolescents aged 10–24 years, between 1953 and 2010. Zhonghua Liu Xing Bing Xue Za Zhi Zhonghua Liuxingbingxue Zazhi 2020, 41, 184–189. [Google Scholar]
- Casey, B.J.; Jones, R.M.; Hare, T.A. The adolescent brain. Ann. N. Y. Acad. Sci. 2008, 1124, 111–126. [Google Scholar] [CrossRef]
- Gomes, M.G.S.; Tractenberg, S.G.; Orso, R.; Viola, T.W.; Grassi-Oliveira, R. Sex differences in risk behavior parameters in adolescent mice: Relationship with brain-derived neurotrophic factor in the medial prefrontal cortex. Neurosci. Lett. 2022, 766, 136339. [Google Scholar] [CrossRef]
- Miovsky, M.; Gavurova, B.; Ivankova, V.; Rigelsky, M.; Sejvl, J. Fatal injuries and economic development in the population sample of Central and Eastern European Countries: The perspective of adolescents. Int. J. Public Health 2020, 65, 1403–1412. [Google Scholar] [CrossRef]
- Adolescent and Young Adult Health. Available online: https://www.who.int/news-room/fact-sheets/detail/adolescents-health-risks-and-solutions (accessed on 25 October 2021).
- Simons, A.; Govender, R.; Saunders, C.J.; Singh-Adriaanse, R.; Van Niekerk, A. Childhood vulnerability to drowning in the Western Cape, South Africa: Risk differences across age and sex. Child Care Health Dev. 2020, 46, 607–616. [Google Scholar] [CrossRef]
- GBD 2016 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1345–1422. [Google Scholar] [CrossRef] [PubMed]
- The Ministry of Education and Other Four Departments Plans to Prevent Drowning among Primary and Middle School Students. Available online: http://www.moe.gov.cn/jyb_xwfb/gzdt_gzdt/s5987/202207/t20220729_649584.html (accessed on 26 April 2023). (In Chinese)
- Global Tuberculosis Report 2021. Available online: https://www.who.int/publications/i/item/9789240037021 (accessed on 22 January 2022).
- Office of the State Council on the Issuance of the National Tuberculosis Prevention and Control Plan (2001–2010) Notice. Available online: http://www.gov.cn/zhengce/zhengceku/2016-10/10/content_5116899.htm (accessed on 25 January 2022). (In Chinese)
- Office of the State Council on the Issuance of the National Tuberculosis Prevention and Control Plan (2011–2015) Notice. Available online: http://www.gov.cn/gongbao/content/2011/content_2020914.htm (accessed on 25 January 2022). (In Chinese)
- Patton, G.C.; Coffey, C.; Sawyer, S.M.; Viner, R.M.; Haller, D.M.; Bose, K.; Vos, T.; Ferguson, J.; Mathers, C.D. Global patterns of mortality in young people: A systematic analysis of population health data. Lancet 2009, 374, 881–892. [Google Scholar] [CrossRef] [PubMed]
- National Center for Health Statistics Mortality Data on CDC Wonder. Available online: https://wonder.cdc.gov/Deaths-by-Underlying-Cause.html (accessed on 20 September 2023).
- Heron, M. Deaths: Leading Causes for 2017. Natl. Vital Stat. Rep. 2019, 68, 1–77. [Google Scholar] [PubMed]
- Lozano, R.; Naghavi, M.; Foreman, K.; Lim, S.; Shibuya, K.; Aboyans, V.; Abraham, J.; Adair, T.; Aggarwal, R.; Ahn, S.Y.; et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2095–2128. [Google Scholar] [CrossRef]
- The Program for the Development of Chinese Children 2001–2010. Available online: http://www.scio.gov.cn/xwfbh/xwbfbh/wqfbh/39595/41756/xgzc41762/Document/1664775/1664775.htm (accessed on 19 January 2021). (In Chinese)
- The Program for the Development of Chinese Children 2011–2020. Available online: https://www.scio.gov.cn/ztk/xwfb/46/11/Document/976030/976030.htm,2011-08-08/2019-09-04 (accessed on 19 January 2021). (In Chinese)
- Niu, G.; Melenberg, B. Trends in mortality decrease and economic growth. Demography 2014, 51, 1755–1773. [Google Scholar] [CrossRef]
- Stewart, C.H.; Dundas, R.; Leyland, A.H. The Scottish school leavers cohort: Linkage of education data to routinely collected records for mortality, hospital discharge and offspring birth characteristics. BMJ Open 2017, 7, e015027. [Google Scholar] [CrossRef]
- Gallet, C.A.; Doucouliagos, H. The impact of healthcare spending on health outcomes: A meta-regression analysis. Soc. Sci. Med. 2017, 179, 9–17. [Google Scholar] [CrossRef]
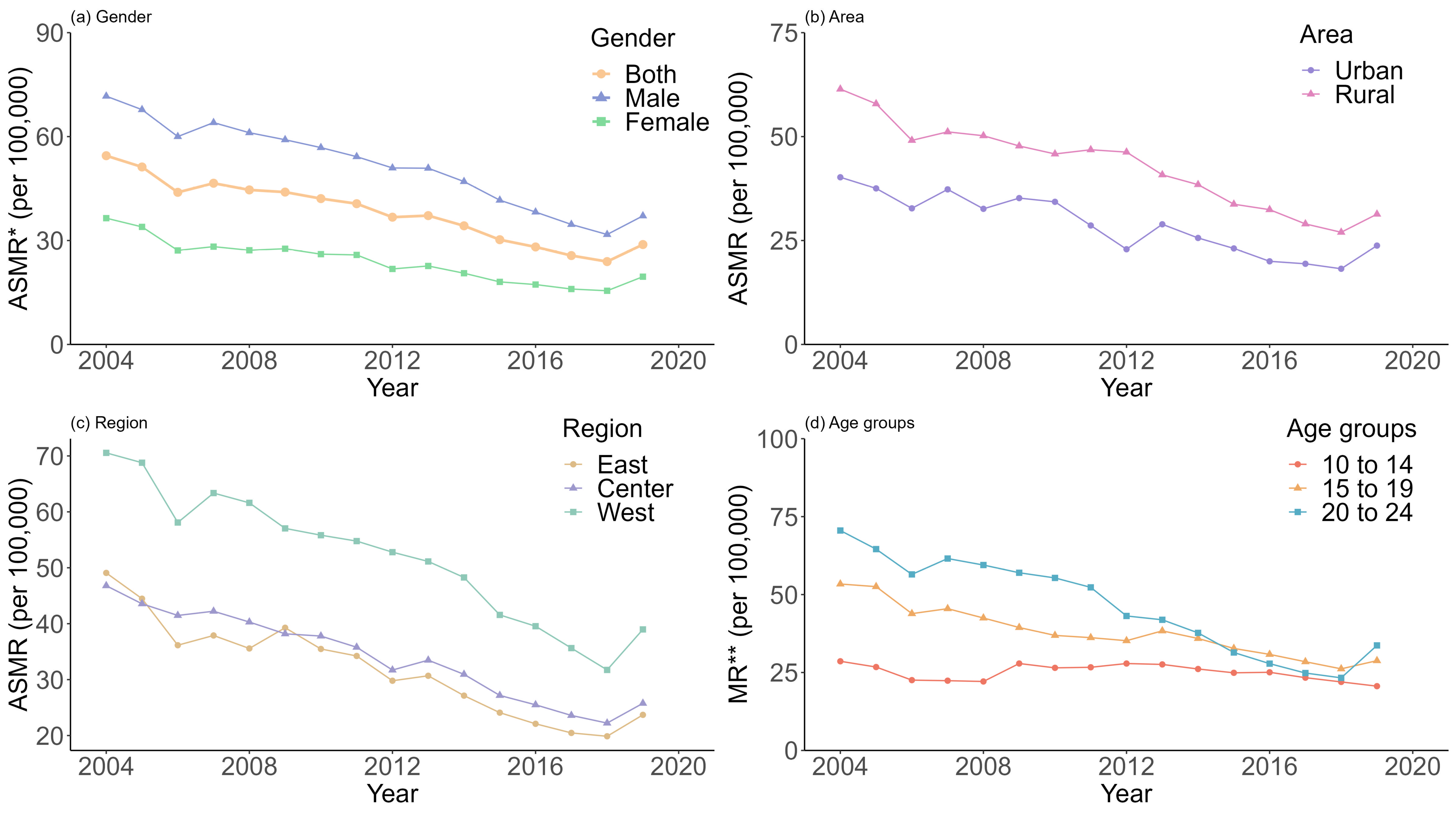



| Group | (AS)MR */per 100,000 | APC **/% | ||
|---|---|---|---|---|
| 2004 | 2010 | 2019 | ||
| Country | 54.48 | 42.10 | 28.84 | −4.02 (−4.30, −3.74) |
| Gender | ||||
| Male | 71.67 | 56.82 | 37.11 | −4.01 (−4.35, −3.67) |
| Female | 36.45 | 26.06 | 19.55 | −4.27 (−4.77, −3.77) |
| Area | ||||
| Urban | 40.22 | 34.31 | 23.78 | −4.38 (−4.95, −3.80) |
| Rural | 61.42 | 45.82 | 31.34 | −3.79 (−4.34, −3.24) |
| Region | ||||
| East | 49.08 | 35.48 | 23.70 | −4.50 (−5.02, −3.98) |
| Center | 46.79 | 37.79 | 25.76 | −3.52 (−4.27, −2.77) |
| West | 70.55 | 55.82 | 38.98 | −4.07 (−4.58, −3.56) |
| Age group *** | ||||
| 10 to 14 | 28.60 | 26.50 | 20.62 | −0.28 (−0.83, 0.28) |
| 15 to 19 | 53.38 | 36.90 | 28.80 | −4.17 (−4.56, −3.78) |
| 20 to 24 | 70.55 | 55.34 | 33.69 | −7.46 (−7.84, −7.08) |
| Group | GDP per Capita (Thousand Yuan) | Illiteracy Rate (%) | Health Beds per 1000 Population |
|---|---|---|---|
| Country | −0.09 | 0.33 | −5.18 |
| (−0.22, 0.04) | (−0.33, 1.00) | (−7.08, −3.27) | |
| Gender | |||
| Male | −0.23 | −0.09 | −6.23 |
| (−0.39, −0.06) | (−0.90, 0.72) | (−8.56, −3.89) | |
| Female | 0.03 | 0.82 | −3.76 |
| (−0.09, 0.15) | (0.23, 1.41) | (−5.46, −2.06) | |
| Area | |||
| Urban | −0.07 | 0.06 | −4.32 |
| (−0.23, 0.08) | (−0.71, 0.83) | (−6.54, −2.10) | |
| Rural | −0.19 | 0.37 | −4.23 |
| (−0.35, −0.03) | (−0.42, 1.16) | (−6.51, −1.95) | |
| Age group *** | |||
| 10 to 14 | −0.01 | −0.37 | −1.23 |
| (−0.15, 0.13) | (−1.06, 0.32) | (−3.22, 0.76) | |
| 15 to 19 | −0.06 | 1.48 | −3.12 |
| (−0.21, 0.09) | (0.75, 2.22) | (−5.24, −1.00) | |
| 20 to 24 | −0.16 | −0.15 | −9.11 |
| (−0.37, 0.05) | (−1.18, 0.88) | (−12.06, −6.16) | |
| Cause of death | |||
| CMNN diseases * | 0.05 | 0.29 | −0.78 |
| (0.02, 0.07) | (0.18, 0.40) | (−1.10, −0.45) | |
| NCDs ** | −0.01 | 0.24 | −1.00 |
| (−0.05, 0.04) | (0.03, 0.45) | (−1.61, −0.39) | |
| Injuries | −0.12 | −0.23 | −3.44 |
| (−0.21, −0.04) | (−0.66, 0.19) | (−4.66, −2.22) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, Y.; Zhong, P.; Dang, J.; Shi, D.; Cai, S.; Chen, Z.; Zhang, Y.; Ma, J.; Song, Y. Trends of Cause-Specific Mortality and Association with Economic Status, Education Level, as Well as Health Investment among Adolescents Aged 10 to 24 Years in China, 2004–2019. Future 2023, 1, 61-75. https://doi.org/10.3390/future1030008
Liu Y, Zhong P, Dang J, Shi D, Cai S, Chen Z, Zhang Y, Ma J, Song Y. Trends of Cause-Specific Mortality and Association with Economic Status, Education Level, as Well as Health Investment among Adolescents Aged 10 to 24 Years in China, 2004–2019. Future. 2023; 1(3):61-75. https://doi.org/10.3390/future1030008
Chicago/Turabian StyleLiu, Yunfei, Panliang Zhong, Jiajia Dang, Di Shi, Shan Cai, Ziyue Chen, Yihang Zhang, Jun Ma, and Yi Song. 2023. "Trends of Cause-Specific Mortality and Association with Economic Status, Education Level, as Well as Health Investment among Adolescents Aged 10 to 24 Years in China, 2004–2019" Future 1, no. 3: 61-75. https://doi.org/10.3390/future1030008
APA StyleLiu, Y., Zhong, P., Dang, J., Shi, D., Cai, S., Chen, Z., Zhang, Y., Ma, J., & Song, Y. (2023). Trends of Cause-Specific Mortality and Association with Economic Status, Education Level, as Well as Health Investment among Adolescents Aged 10 to 24 Years in China, 2004–2019. Future, 1(3), 61-75. https://doi.org/10.3390/future1030008








