Abstract
Background/Objectives: Elevated plasma homocysteine levels constitute a risk factor for vascular and cardiovascular disorders. Ferulic acid (FA), a polyphenol is tested on L-methionine-induced hyperhomocysteinemia (hHcy). The present study investigated the protective effect of ferulic acid (FA) on hyperhomocysteinemia (hHcy) induced changes in hemodynamic, biochemical, anti-oxidant, anti-inflammatory parameters as well as histopathological changes in abdominal aorta and heart. Methodology: The Wistar rats were divided into six groups (n = 6) and treated orally for 36 days. The rats were treated with Met (1 gm/kg) to induce Hcy. They were treated with either standard (Vit. B12 + Folic acid; 15 + 70 mg) or test FA (20/40/60 mg/kg, respectively) post-Met treatment. Homocysteine, cholesterol, lactate dehydrogenase (LDH), creatinine kinase (CK-MB), and liver enzymes were estimated in blood followed by the measurement of hemodynamic parameters. The liver was estimated for antioxidant parameters and nitric oxide (NO). Heart and abdominal aorta were studied histopathologically. Result: Diseased rats showed increased Hcy, cholesterol, LDH, CK-MB, alanine transaminase (ALT), aspartate transaminase (AST), malondialdehyde (MDA), NO, and reduced glutathione (GSH). Following FA treatment, these parameters returned to normal. Atherosclerotic lesions in the aorta were observed in the hHcy group; however, in the FA treatment groups, they were lessened. Conclusions: Ferulic acid reduces oxidative and nitrosive stress, thereby reducing hypercyteinemia and improving the lipid profile. It might be acting by increasing the activity of methylation dependent on S-adenosylmethionine (SAM)/S-adenosylhomocysteine (SAH), which in turn prevents the formation of Hcy and reduces hHcy. The docking study supports these findings.
1. Introduction
Cardiovascular disease (CVD) is now the major cause contributing to disability and premature death globally. According to the report of Global Burden of Diseases, Injuries, and Risk Factor Study 2015 and the WHO, CVD affected an estimated 422.7 million people and caused an estimated 17.9 million deaths worldwide in 2019, comprising 32% of all deaths worldwide [1,2]. By 2030, the annual cardiovascular disease mortality is expected to reach 23.6 million. The large and progressively increasing burden of CVDs on people, families, and healthcare systems is an indicative of an urge to conduct the research on atherosclerotic diseases and the adoption of preventive measures [3,4].
Research is always focused on identifying reliable biomarkers for CVD. Numerous biomarkers linked to the development of CVD include a series of events initiated by inflammation and endothelial damage [5]. Potential biomarkers for CVD prediction include elevated levels of homocysteine, the erythrocyte sedimentation rate, and C-reactive protein [6].
Homocysteine (Hcy) is a naturally occurring non-proteinogenic sulfur-containing α-amino acid in human body that functions as a key intermediate in the biosynthesis of methionine and cysteine [7,8]. Methionine undergoes methylation by methionine adenosyltransferase (MATs) (also known as S-Adenosylmethioninesynthetase) to form S-Adenosylmethionine (SAM), which further irreversibly converts to S-adenosylhomocysteine (SAH), and SAH is further converted to Hcy. The metabolism of Hcy stands at the intersection of two pathways. The first pathway involves the remethylation to methionine, which requires folate and vitamin B12; second, Hcy is trans-sulfurated to cystathionine to cysteine, which requires vitamin B6 [7,9]. The blockage of either the cysteine or methionine pathway may increase the Hcy levels, leading to hyperhomocysteinemia (hHcy). An abnormally high level of Hcy in the serum is major risk factor for the development of a wide range of disorders such as thrombosis, neuropsychiatric illness, and fractures [10]. Significant associations exist between hHcy and cardiovascular disease and its repercussions such as cardiac arrests and strokes. Additionally, it has been discovered to be linked to microalbuminuria, a significant predictor of future cardiovascular disease [11,12].
Thus, the hHcy may be involved in oxidative stress, inflammation, and ischaemic alterations [13]. The blood artery structure and function are modified by hHcy, and oxidative stress seems to be the main mechanism causing these changes [14,15]. Cardiovascular illnesses are caused by the reactive oxygen species that are produced, which also promote the production of superoxide radicals, lipid peroxidation, and protein oxidation [16,17]. Studies have demonstrated a reduction in levels of homocysteine with folate, which is the primary vitamin utilized to lower homocysteine levels. A greater reduction in homocysteine levels can be achieved with vitamin B12 plus folate than with folate alone. Other than vitamin supplements, there are no other treatments available. Strong potential exists for plants high in phenolic acids to serve as major sources of naturally occurring antioxidants [18]. Numerous traditional plants, primarily ferulic acid, are excellent sources of phenolic acid. Ferulic acid, also known as 3-(4-hydroxy-3-methoxy-phenyl) prop-2-enoic acid, is a common phenolic acid that may be found in a wide variety of plants [19]. It is abundant in many staple foods, including citrus fruits, whole grains, spinach, broccoli, and grain bran, and it is found in plant tissues [20]. In China, it is used clinically to treat hypertensive disorders and angina pectoris [21]. Furthermore, the evidence from epidemiological research suggests that consuming whole grains high in FA lowers the chance of developing chronic illnesses, such as cardiovascular disease [20]. Its therapeutic effects are multifaceted and include antioxidant [22,23], anti-hypertensive [24], anti-inflammatory [25], neuroprotective [26], and cardioprotective [27] properties. The present investigation was conducted with the aim of assessing the impact of FA on hHcy in Wistar rats induced by L-methionine.
2. Results
2.1. Evaluation of Serum Parameters
Table 1 shows the effect of l-methionine-induced hHcy on different serum parameters in all six groups viz. normal, hHcy control, Vit. B12 + FoA, FA (20 mg/kg), FA (40 mg/kg), and FA (60 mg/kg). The administration of methionine (1 gm/kg) to animals resulted in hHcy, as observed in hHcy when compared to normal (### p < 0.001). The homocysteine levels observed in the groups supplemented with FoA (70 mg/kg) + vit. B12 (15 mg/kg), FA (20 mg/kg), FA (40 mg//kg), and FA (60 mg//kg) were almost equivalent to the normal group (4.6 µmole/L) (*** p < 0.001).

Table 1.
Effect of FA (20, 40, and 60 mg/kg) on serum parameters in l-methionine-induced in rats.
The cholesterol level was found to be significantly decreased (almost 2.5 folds, p < 0.001) by the 28th day of treatment with FoA (70 mg/kg) + vit. B12 (15 mg/kg) and FA (20, 40, and 60 mg/kg). The LDH levels was decreased by almost 61% in groups treated with FoA (70 mg/kg) + vit. B12 (15 mg/kg), and FA (20, 40, and 60 mg/kg) in comparison to the Hcy control group and was found to be analogous with that of the normal group. The total protein level in serum was also reverted to the normal levels effectively in FA (20, 40, and 60 mg/kg)-treated groups (around 7.5 g/dL), which was observed to be elevated in the hHcy control group (around 17.37 g/dL).
The measured serum CK-MB, AST, and ALT activities were found to be reduced significantly by the treatment of FoA (70) + vit. B12 (15), FA (20 mg/kg), FA (40 mg/kg), and FA (60 mg/kg) in comparison with the hHcy control group. The data showed that the treatment with FA reduced Hcy, total cholesterol, total protein, and other parameters; however, there was no significant difference between the groups.
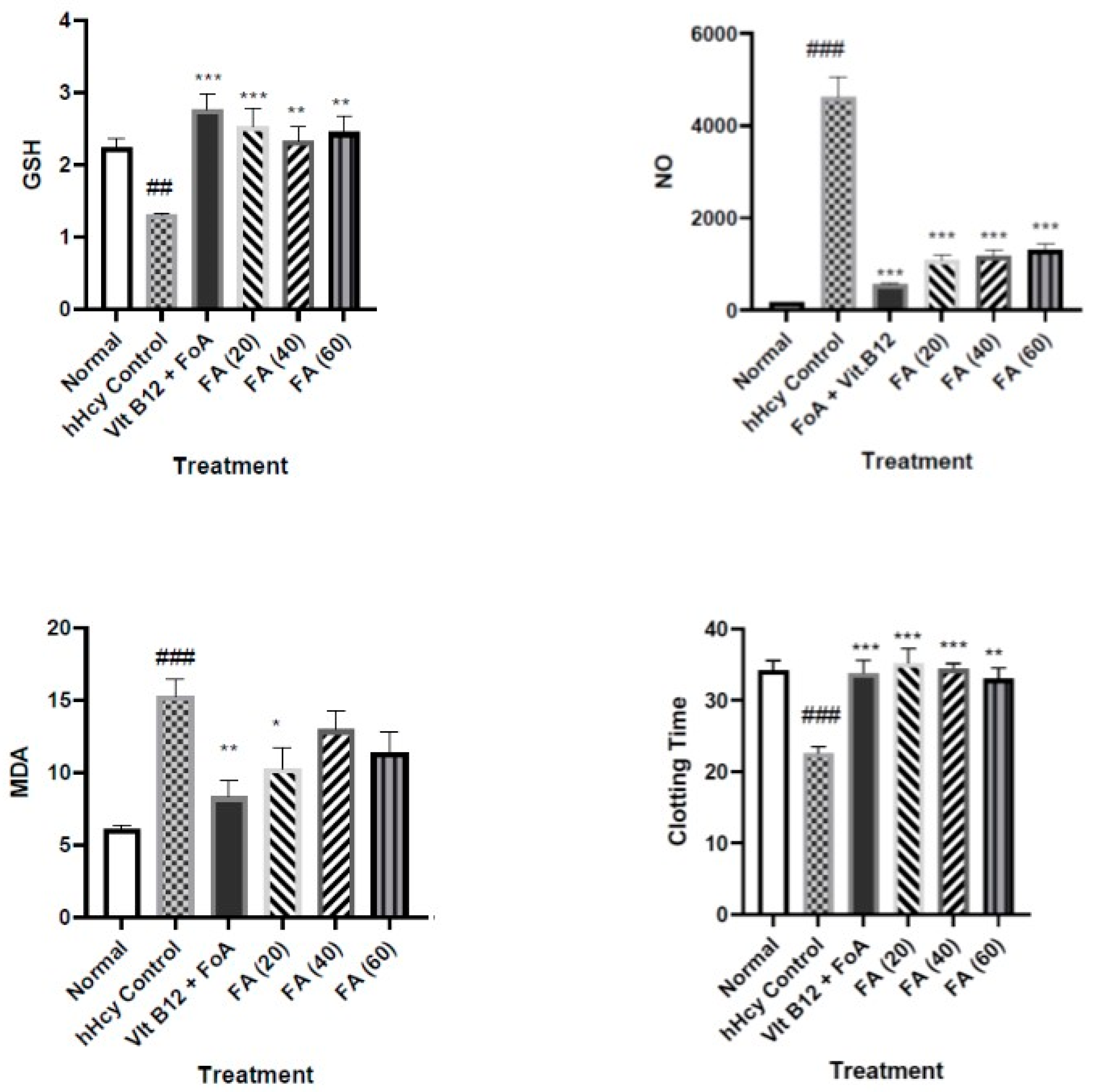
2.2. Effect on Tissue Parameters: Effect of FA (20, 40, and 60 mg/kg) on GSH, NO, MDA
Myocardial GSH was reduced significantly (p < 0.001) in hHcy control compared with the normal group, while the treatment with FoA + vit. B12 (70 + 15 mg/kg), FA (20 mg/kg), FA (40 mg/kg), and FA (60 mg/kg) significantly improved (p < 0.001, p < 0.01, p < 0.001) the level of myocardial GSH compared to hHcy control (Figure 1).
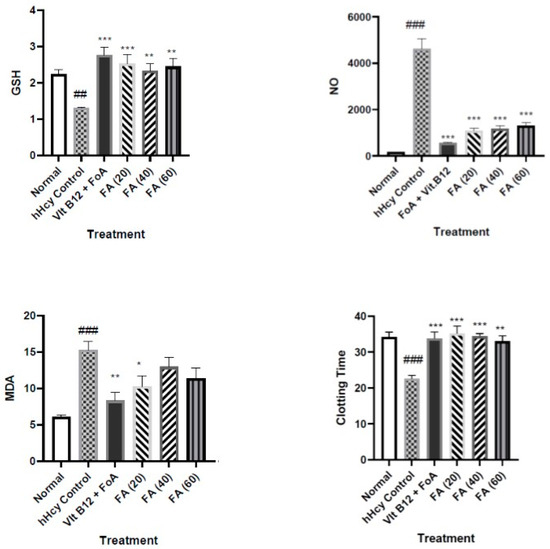
Figure 1.
Effect of FA (20, 40, and 60 mg/kg) on tissue parameters and blood clotting time in l-methionine-induced hHcy in rats. Data are expressed as mean ± SEM (n = 6). ### p < 0.001, ## p < 0.01 compared to normal, * p < 0.05, ** p < 0.01, *** p < 0.001 compared to control. hHcy: Hyperhomocysteinemia, FoA: Folic acid, FA: Ferulic acid.
The tissue nitric oxide content of the hHcy control group was significantly higher compared to the normal group (p < 0.001). The nitric oxide content in Std. Vit. B12 + FoA and FA groups were significantly reduced compared to the hHcy control group (p < 0.001) (Figure 1).
The tissue MDA content of the hHcy control group was significantly higher than that of the normal group (p < 0.001). The MDA content was significantly reduced by the standard drug Vit. B12+ FoA group (70 + 15 mg/kg) (p < 0.01) and by FA (20 mg/kg) (p < 0.05). In other groups, a nonsignificant reduction was observed (Figure 1).
2.3. Effect of FA (20, 40, and 60 mg/kg) on Blood Clotting Time
The blood clotting time in the hHcy control group was significantly decreased (*** p < 0.001) compared to normal. All the treatment groups significantly brought the parameters back to normal (** p < 0.01, *** p < 0.001) (Figure 1).
2.4. Effect on Hemodynamic and Electrocardiographic Parameters
There was no significant change observed in the systolic blood and diastolic blood pressure in all treatment groups and the hHcy control group compared to normal. There was no significant change occurred on the heart rate and QTc interval in all treatment groups and the hHcy control group compared to normal (Table 2).

Table 2.
Effect of FA (20, 40, and 60 mg/kg) on hemodynamic and electrocardiographic parameters in l-methionine-induced hHcy in rats.
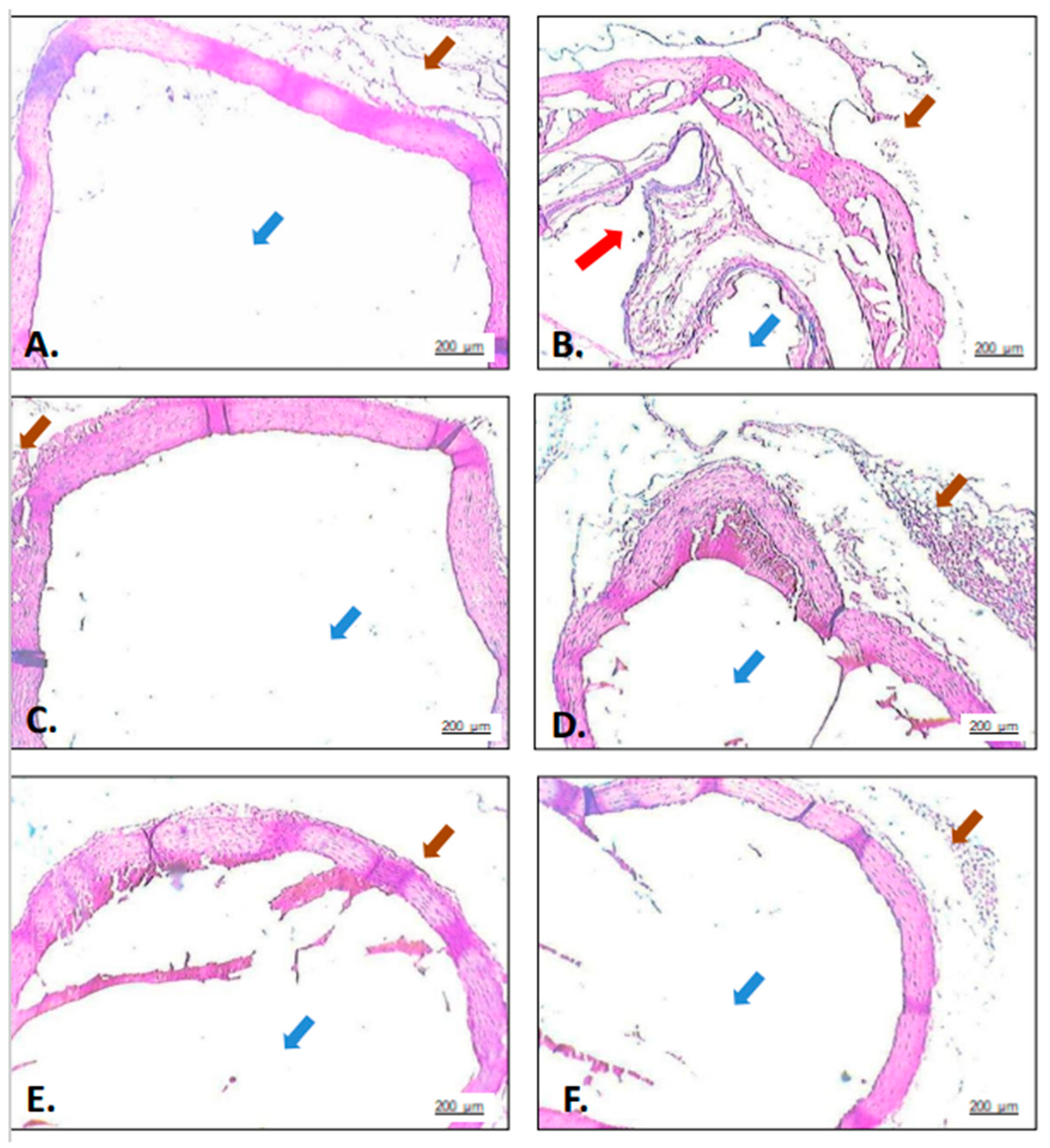
2.5. Effect of FA (20, 40, and 60 mg/kg) on Orcein Staining
The histopathology study of the abdominal aorta is shown in Figure 2. The sections from normal rats (A) showed the normal structure and architecture of the abdominal aorta. hHcy control rats (B) showed marked atherosclerotic lesions at the interior surface of the abdominal aorta indicated using Orcein stain. The lesions were identified as vulnerable plaque with a lipid-rich core covered by a thin fibrous cap. The lesions were of low density in the FA (40 mg/kg) group (F). A marked reduction was observed in the standard drug (C) and FA (60 mg/kg) group (F).
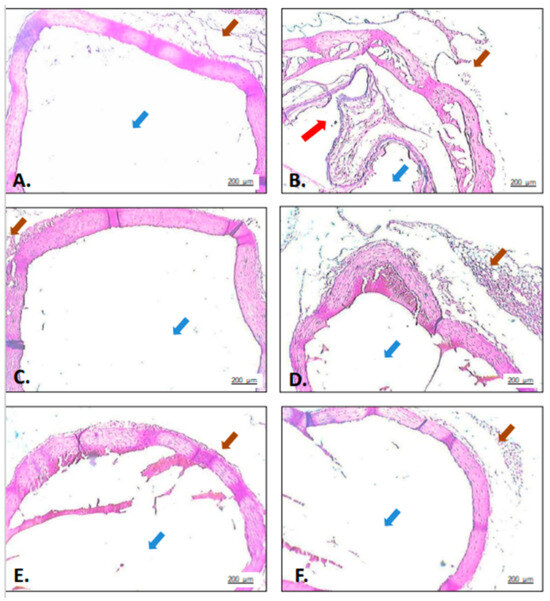
Figure 2.
Effects of FA (20, 40, and 60 mg/kg) on histopathological changes (Orcein dye staining 40×) in l-methionine-induced hHcy in rats. (A): Normal—section shows normal structure and architecture of abdominal aorta; (B): hHcy control—section shows (red arrow) atherosclerotic lesions in the aortic roots; (C): Standard (Vit. B12 + FoA)—section shows normal aortic structure and architecture, with no evidence of atherosclerotic lesions.; (D–F) were the treatment groups treated with FA (20/40/60 mg/kg), respectively, and shows significantly decreased lesion size compared to hHcy control group. (brown arrow): Connective tissue, (blue arrow): Lumen.
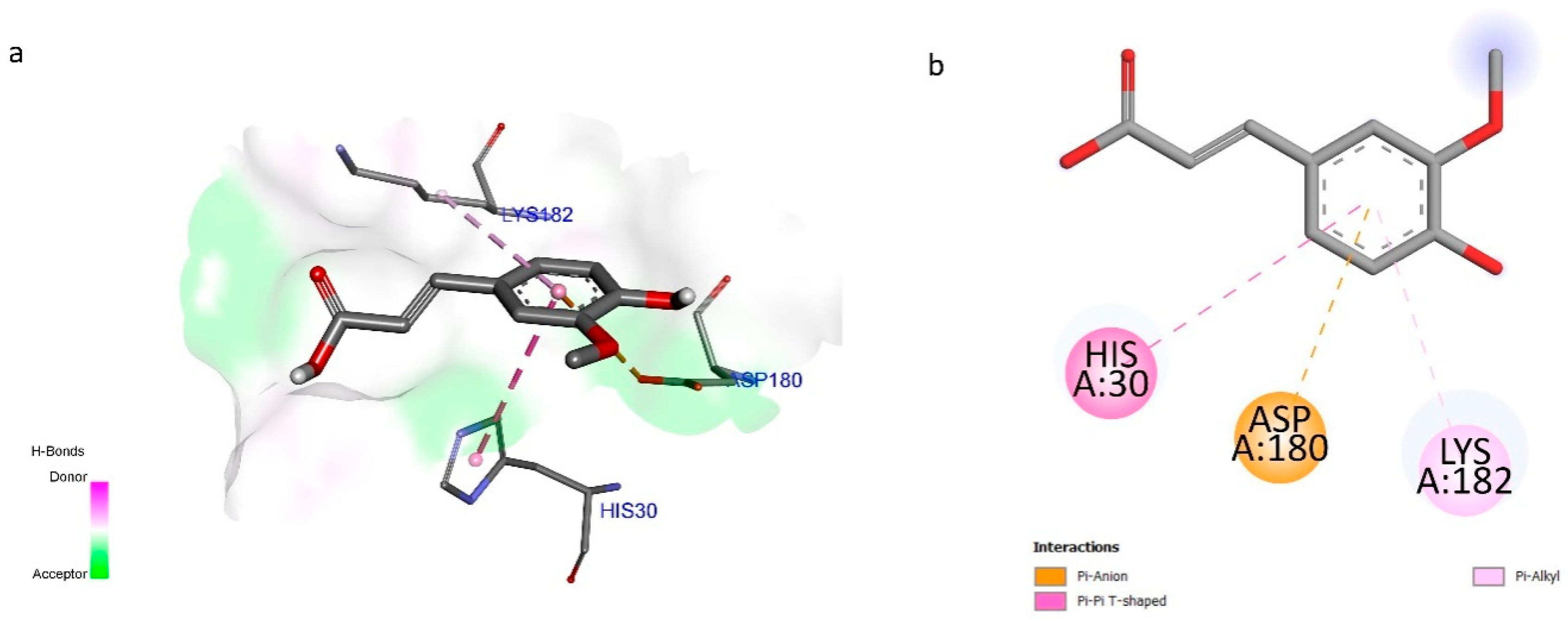
2.6. Results of Docking Studies
In the present study, Ferulic acid was demonstrated to modulate MAT as observed by a favorable binding energy of −10.62 kcal/mol. Notably, the phenyl ring demonstrated three significant interactions with amino acid residues, His30, Asp180, and Lys182, in HAT (Figure 3).
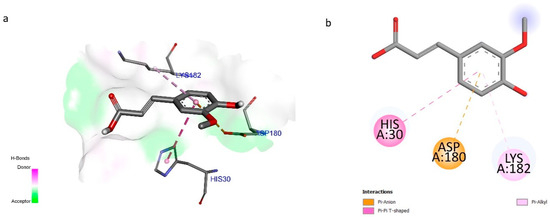
Figure 3.
(a) Three-dimensional and (b) two-dimensional interaction of ferulic acid with Methionine adenosyltransferases.
3. Discussion
This epidemiological study indicates that a mild elevation of plasma Hcy concentration is an independent risk for atherothrombotic diseases [28,29]. In the general population, increased Hcy is common with individual suffering from coronary, cerebro-vascular, and peripheral atherosclerotic diseases [30,31]. A common reason for increase Hcy is the inadequate concentration of vitamins required for Hcy metabolism such as folic acid and vitamin B12 and B6 [32,33]. In addition to low supply, an increased requirement for folic acid or the interference of drugs with folate metabolism can cause a folate deficiency. Drugs like aminopterin (immunosuppressive), methotrexate (anti-cancer), pyrimethamine (anti-protozoal), trimethoprim (urinary tract infection), and triamterene (sodium channel blocker) affect the folate metabolism [34,35]. A higher concentration of Hcy is also common in pregnant women, smokers, alcoholics, and users of contraceptive medicines due to an alteration in the enzymes controlling Hcy metabolism [36,37,38,39]. Elevated levels of Hcy can modify the morphology of the blood vessel wall, increase platelet activity, and stimulate smooth muscle proliferation and LDL oxidation. Hcy adversely affects the endothelial morphology of arteries and arterioles. hHcy has also been reported to affect the cardiovascular system, thereby leading to cardiovascular diseases [9].
In the present study, we administered methionine (1 gm/kg) for 36 days to Wistar rats to induce hHcY. It was observed that Hcy was increased five-fold in hHcy-controlled animals, while FA was able to reduce it significantly. The effects were comparable to the standard, vit. B12, and FoA group. Previously, we have reported the cardioprotective activity of FA in the abdominal aortic banding (AAB) model of myocardial infarction [40] and in doxorubicin-induced cardiac toxicity [41]. The potential cardioprotective activity of FA is attributed to its potent antioxidant profile [42]. FA is a derivative of oryzanol, which is now intentionally added to edible oils and is a key component of rice bran oil. The oryzanol component of rice bran oil is a fraction containing FA that accounts for 80% of oryzanol. Oryzanol is reported to be a potent antioxidant due to its FA content being higher than vitamin E [43]. As previously mentioned, FA is known to reduce cholesterol, oxidized LDL-C, and oxidative stress and can therefore improve the lipid profile and blood vessel activity, hence reducing cardiovascular disease risk factors [20,21,44,45]. Ferulic acid is abundantly found in fruits and vegetables, such as sweet corn, tomatoes, and in rice grain, thus the intake of FA-rich food can help to alleviate the risk of hHcy.
Although hyperhomocysteinemia is commonly caused by vitamin deficiency, other causes may include the dysfunction of enzymes and cofactors associated with the process of homocysteine biosynthesis, excessive methionine intake, certain diseases, and the side effects of some drugs. Persistent hHcy leads to increased serum cholesterol, increased LDL, and reduced HDL cholesterol [46,47], which are similar findings we have obtained. Hyperhomocysteinemia produces oxidative stress, which contribute to atherosclerosis. The free oxygen radicals forms oxidized LDL in the endothelial tissues of blood vessels, and oxidized LDL promotes the formation of foam cells, leading to atherosclerotic lesions. FA has been reported to lower the plasma levels of total cholesterol, VLDL, and LDL [48]. It has also been reported to inhibit hepatic HMG-CoA reductase, the rate-limiting enzyme in cholesterol biosynthesis and acyl-CoA cholesterol esterifying enzyme in tissue [49]; our results are in agreement with the reported studies. The histopathology of the aorta in the present study confirms these findings. The histopathology indicated the presence of atherosclerotic lesions in the hHcy group while it was absent in treatment groups. Although betaine, a byproduct of choline oxidation, is known to lower hHcy, it also has a negative impact on hyperlipidemia. As a result, FA is a superior option for the treatment of hHcy due to its homocysteine-lowering property and its hypolipidemic effect.
Oxidative stress brought on by hHcy may also result in reduced glutathione, lipid peroxidation (MDA), and an increase in total proteins. Our findings are close to those of the earlier research [40]. Peroxynitrite is formed when nitric oxide and superoxide anion, which are generated during hHcy-induced oxidative stress [50]. We measured the amount of NO metabolites and discovered a substantial rise in hHcy, which may be related to nitrosive stress. We speculate that both peroxide and peroxy nitrite production are responsible for the oxidative stress generated in hHcy. As previously noted, FA has a strong effect on inhibiting the development of both nitrite and oxide [51]. According to Woo et al. (2006), hHcy induces oxidative stress in the liver, which might raise ALT and AST levels [52]. Based on AST and ALT data, FA, a free radical scavenger, reduced liver damage. As previously reported, we also found a prominent effect at the lower dose of FA (at 20 mg/kg, p.o.) [53]. The reason could be attributed to the formation of undesired metabolites of FA (as given in earlier reports) or it may be due to the prolonged use (36 days of administration) of FA leading to the achievement of the steady-state concentration.
Increased oxidative stress causes damage to the heart’s cells in hHcy, which raises the blood levels of LDH and CK-MB. In the current investigation, hHcy’s detrimental effect on cardiac cells has been found to raise the serum levels of CK-MB and LDH, whereas the FA treatment significantly decreased both of these levels, indicating its cardioprotective action. It has been reported that an increased level of Hcy is an independent risk factor for premature cardiovascular diseases [9]. An elevated Hcy concentration leads to the constriction of blood vessels, resulting in atherogenesis and thrombosis. The present study demonstrated the influence of hHcy on hemodynamic and electrocardiographic parameters, but we found that hHcy did not increase blood pressure and did not affect ECG. However, the increased treatment days of methionine can cause an alteration in BP and ECG; this possibility cannot be denied. It has been reported that a higher plasma total Hcy concentration is linked to enhanced platelet aggregation and thromboxane synthesis, which is a key factor for blood clotting [54]. In our study, we have observed similar findings; the blood clotting time has been increased due to increased Hcy concentration. FA restored the clotting time to normal.
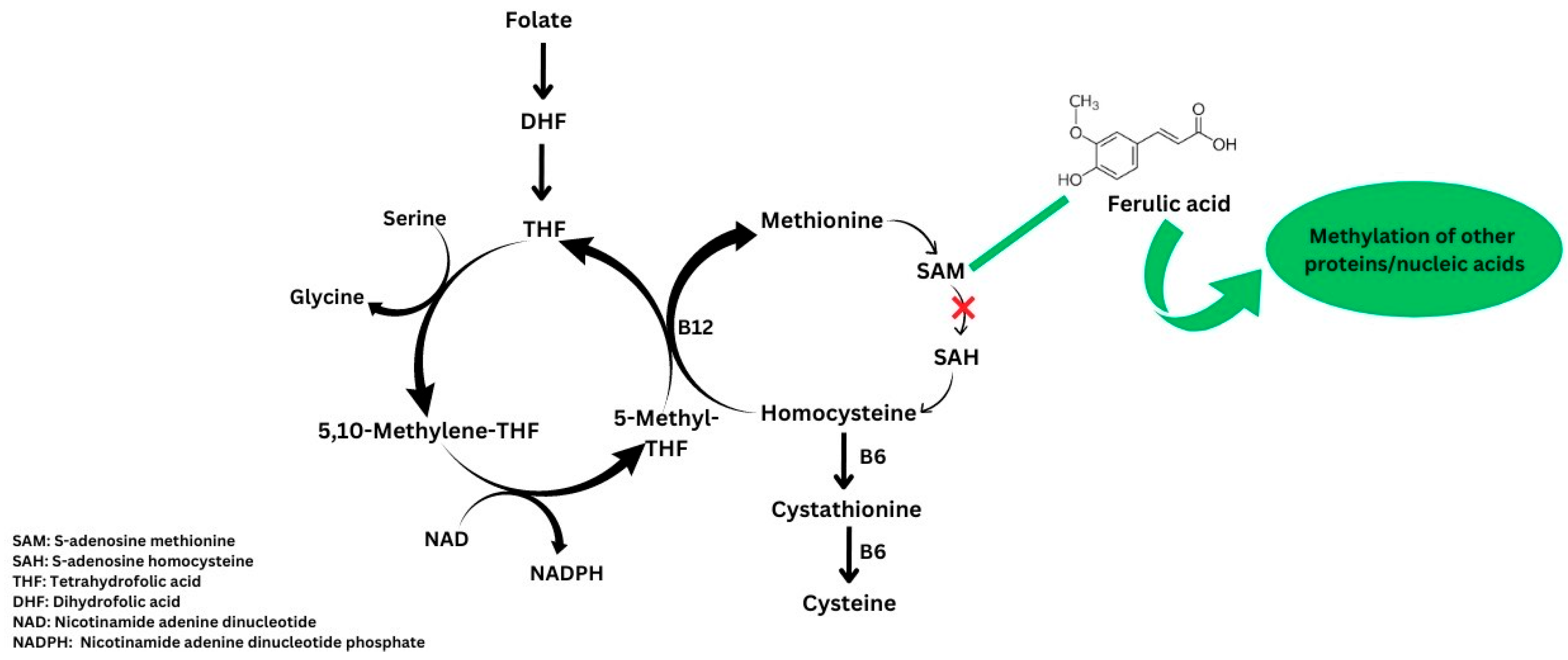
FA is a powerful antioxidant, but our research is the first to suggest that it affects the homocysteine and methionine cycle. The figure illustrates the possible mechanism of action (Figure 4). As previously noted, ferulic acid may increase the effectiveness of SAM for the further methylation of biomolecules including proteins, nucleic acid, etc., thereby lowering the production of homocysteine [55].
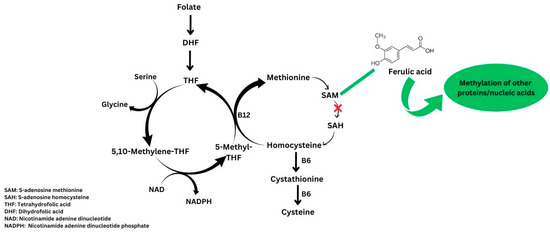
Figure 4.
Probable mechanism of action of ferulic acid.
The primary function of MAT, a rate-limiting enzyme in the methionine cycle, is to catalyze the conversion of methionine and adenosine triphosphate (ATP) into S-adenosylmethionine (SAM), and SAM serves as the methyl donor in almost all methylation reactions within the body. SAM is irreversibly transformed into the metabolic precursor of homocysteine, S-adenosylhomocysteine (SAH). Hence, the modulation of SAM levels through MAT inhibition could be a possible mechanism of action, as shown by the Hcy level in the treatment group compared to the diseased group in the present study, and is further supported by the docking results. Thus, docking and biochemical studies show that FA may increase the activity of the SAM/SAH-dependent methylation of other proteins and allows progress towards Hcy formation. However, it is necessary to measure the levels of SAM and SAH to further confirm this mechanism.
4. Materials and Methods
4.1. Animals
Adult male Wistar rats (160–200 g) were obtained from the Institutional Animal House of SIOP (CPCSEA/1139/a/07) and housed in groups of six animals per cage at standard laboratory conditions with a temperature of 25 ± 1 °C, relative humidity of 45–55%, and 12:12 h dark and light cycle. Animals had free access to food (standard chow pellet, Nutrivet Life Sciences, Pune, India) and water ad libitum. The experimental protocol was approved by the Institutional Animal Ethics Committee (IAEC) of Sinhgad Institute of Pharmacy, Narhe, Pune, India, constituted according to guidelines of Committee for the Purpose of Control and Supervision of Experiment on Animals (reg. no. SIOP/IAEC/2014/22).
4.2. Chemicals
Ferulic Acid (Sigma Aldrich, St. Louis, MO, USA), L-Methionine (Loba Chemicals, Mumbai, India), and reduced glutathione (GSH) were obtained from LobaChemie Pvt. Ltd. (Mumbai, India). CK-MB, alanine transferase (ALT) and aspartate transferase (AST) kits (Pathozyme Diagnostics, Kolhapur, Maharashtra, India), and lactate dehydrogenase (LDH) kits (Bio-Lab Diagnostics, Mumbai, India), total cholesterol (Span Diagnostics Ltd., Pune, India), and Rat Hcy ELISA (Blue Gene Biotech Co., Ltd., Shanghai, China) were purchased.
4.3. Experimental Protocol for L-Methionine-Induced hHcy in Rats
Thirty-six healthy adult male Wistar rats (160–200 g) were used for this study. The animals were randomly divided into six groups (n = 6). Group I: normal was given distilled water. Group II: hHcy control (disease induced) was treated with L-methionine (1 gm/kg). Group III: standard group received a standard treatment of vit. B12 (15 mg/kg) + folic acid (FoA); 70 mg/kg). Group IV, V, and VI were treated with test drug, FA (20/40/60 mg/kg, respectively). All the treatments were given orally for 36 days simultaneously, and Met (1 gm/kg. p.o.) administration was performed prior to 1 h in all the groups except normal control. On day 28, blood was removed using retroorbital plexus method and serum was separated. Levels of Hcy, cholesterol, LDH, CK-MB, ALT, AST were determined in serum. On day 36, blood pressure, both systolic and diastolic, heart rate, and ECG were determined. The animals were then sacrificed humanely. Liver was carefully separated and used for the estimation of MDA, GSH, and nitric oxide (NO). Heart and abdominal aorta were separated for histopathological studies [56,57].
4.4. Pharmacological Evaluation: Assessment of Hemodynamic and Electrocardiographic Parameters
On the last day of study, animals were anesthetized with urethane (1.25 g/kg, i.p.). The right carotid artery of each rat was cannulated for the measurement of systolic blood pressure (SBP) and diastolic blood pressure (DBP). The cannula was filled with heparinized saline and connected to pressure transducer. After 30 min of stabilization, hemodynamic parameters were recorded by eight channel recorder Power lab (AD Instruments Pty Ltd. with LABCHART Pro software version 7, Bella Vista, NSW, Australia). For the measurement of the electrocardiograph, the leads were placed on the right foreleg (positive electrode), left foreleg (negative electrode), and right hind leg (neutral electrode) [58,59].
4.5. Serum Parameters
Blood was removed; serum was separated and kept at −20 °C for the estimation of CKMB, LDH, AST, ALT, cholesterol, Hcy, and total protein level. The serum CK-MB, LDH, AST, and ALT activity was measured using reagent kits and an automated biochemistry analyzer (Mindray BC-2800, Shenzhen, China) [60]. The serum Hcy level was measured using an ELISA kit (Blue Gene Biotech Co., Ltd., Shanghai, China) [61].
4.6. Tissue Parameters
Liver was quickly transferred to ice-cold phosphate-buffered saline (pH 7.4). It was blotted free of blood and tissue fluids. The hearts were cross-chopped with a surgical scalpel into fine slices, suspended in chilled 0.25 M sucrose solution, and quickly blotted on a filter paper. The tissues were then minced and homogenized in chilled tris hydrochloride buffer (10 mM, pH 7.4) to a concentration of 10% w/v. Prolonged homogenization under hypotonic condition was designed to disrupt, as far as possible, the structure of the cells so as to release soluble proteins. The homogenate was centrifuged at 7000 rpm at 25 min using high-speed cooling centrifuge (Remi R-8C, Remi laboratory Instruments, Mumbai, India). The clear supernatant was used for the estimation of tissue parameters.
4.7. GSH Estimation
Equal volumes of liver tissue homogenate (supernatant) and 20% trichloroacetic acid (TCA) were mixed. This precipitated fraction was centrifuged, and to 0.25 mL of supernatant, 2.0 mL of DTNB reagent was added. Final volume was made up to 3.0 mL with phosphate buffer. The color developed was read at 412 nM against the reagent blank. The amount of reduced glutathione was expressed as mg of GSH/g of wet tissue [62].
4.8. Malondialdehyde (MDA) Estimation
An amount of 0.2 mL of liver tissue homogenate was added in each test tube; 0.2 mL of reagent-A, 1.5 mL of B, and 1.5 mL of C were added in each test tube mixture, which finally made up a total of 4 mL with water and was then heated at 95 °C for 60 min in oil bath. Then, solution was cooled under tap water, and 1 mL water and 5 mL of Reagent D were added in each test tube. These mixtures were vortexed and centrifuged at 2200 g for 5 m. Organic layer (upper layer) was discarded and aqueous layer (lower layer) was used to determine the absorbance colorimetrically at 532 nm against reagent blank [62].
4.9. Nitric Oxide (NO) Estimation
An amount of 0.1 mL of tissue homogenate was added to each test tube containing 10mL, followed by the addition of 500 μL of Griess reagent to each test tube; the absorbance was determined at 546 nm. Then, concentration was measured against reagent blank by interpolating absorbance on standard curve and the values were expressed as µg/mL [63,64].
4.10. Histopathology
The animals were euthanized and the abdominal aorta was removed and placed in 10% formalin solution. The organ specimens were subjected to dehydration with xylene (one hour each) and alcohol of 70, 90, and 100% strength each for two hours. The infiltration and impregnation were carried out by treatment with paraffin wax twice for each time for one hour. Paraffin wax was used to prepare paraffin L molds. Specimens were cut into sections of 3–5 mm thickness and stained with orcein dye. For 10 randomly chosen microscopic fields (40× magnification) of each left ventricle, Masson’s trichome stained myocardial sections were imaged. This served as an estimate of the atherosclerotic lesions [41].
4.11. Docking Studies
The docking studies were performed using AutoDock-4.2 software, employing the Lamarckian Genetic Algorithm (LGA) for conformational search. Visualization of the docking results was performed using Discovery Studio Visualizer-2019. The protein models for methionine adenosyltransferase with PDB id-190 was obtained from the protein databank (https://www.rcsb.org/; accessed on 25 October 2023). The refinement of protein structures was performed through dockprep utility within Chimera-1.17. Ferulic acid structures were minimized through the MMFF94s force field. The grid box was characterized by dimensions of 68 units along each axis (X, Y, Z), with its center located at coordinates (2.054, 36.636, 54.828) for the X, Y, and Z dimensions, respectively, and then the binding energy and conformation was assessed [65,66,67].
4.12. Statistical Analysis
Data for each parameter was analyzed by one-way ANOVA followed by Dunnett’s post hoc test using a graph pad and Prism software, version 5.0, Prism Software Inc., La Jolla, CA, USA.
5. Conclusions
Since ferulic acid can reduce nitrosive and oxidative stress, homocysteine levels will gradually decrease and the lipid profile will improve. Therefore, in order to avoid hHcy and prevent CVDs, it can be utilized as a nutritional adjunct or incorporated into the diet. This experiment could be extended in order to determine the most likely FA mechanism for returning the increased level of Hcy to normal.
Author Contributions
Conceptualization, U.A. and M.A.; methodology, U.A., A.J. and A.G.; formal analysis, investigation, data curation, U.A., M.A. and S.B.; writing—original draft preparation and review U.A., S.B. and A.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Institutional Review Board Statement
The animal study protocol was approved by the Institutional Animal Ethics Committee (IAEC) of Sinhgad Institute of Pharamcy, Narhe, Pune, India, constituted according to guidelines of Committee for the Purpose of Control and Supervision of Experiment on Animals reg. no. SIOP/IAEC/2014/22.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data is available on Figshare (https://doi.org/10.6084/m9.figshare.27186210).
Acknowledgments
We acknowledge the principal of all the colleges for providing the facilities.
Conflicts of Interest
All authors declare that there is no conflicts of interest for this manuscript.
References
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: Update from the GBD 2019 study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef] [PubMed]
- Feigin, V.L.; Forouzanfar, M.H.; Krishnamurthi, R.; Mensah, G.A.; Connor, M.; Bennett, D.A.; Moran, A.E.; Sacco, R.L.; Anderson, L.; Truelsen, T.; et al. Global Burden of Diseases, Injuries, and Risk Factors Study 2010 (GBD 2010) and the GBD Stroke Experts Group. Global and regional burden of stroke during 1990–2010: Findings from the global burden of disease study 2010. Lancet 2014, 383, 245–254. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Health Topics: Cardiovascular Diseases. Fact Sheet. Available online: http://www.who.int/cardiovascular_diseases/en/ (accessed on 11 December 2020).
- Einarson, T.R.; Acs, A.; Ludwig, C.; Panton, U.H. Prevalence of cardiovascular disease in type 2 diabetes: A systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc. Diabetol. 2018, 17, 83. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.J. Assessing the role of circulating, genetic, and imaging biomarkers in cardiovascular risk prediction. Circulation 2011, 123, 551–565. [Google Scholar] [CrossRef] [PubMed]
- Gilstrap, L.G.; Wang, T.J. Biomarkers and cardiovascular risk assessment for primary prevention: An update. Clin. Chem. 2012, 58, 72–82. [Google Scholar] [CrossRef]
- Hermann, A.; Sitdikova, G. Homocysteine: Biochemistry, molecular biology and role in disease. Biomolecules 2021, 11, 737. [Google Scholar] [CrossRef]
- Kim, J.; Kim, H.; Roh, H.; Kwon, Y. Causes of hyperhomocysteinemia and its pathological significance. Arch. Pharmacal Res. 2018, 41, 372–383. [Google Scholar] [CrossRef]
- Ganguly, P.; Alam, S.F. Role of homocysteine in the development of cardiovascular disease. Nutr. J. 2015, 14, 6. [Google Scholar] [CrossRef]
- Guieu, R.; Ruf, J.; Mottola, G. Hyperhomocysteinemia and cardiovascular diseases. Ann. Biol. Clin. 2022, 80, 7–14. [Google Scholar] [CrossRef]
- Sabanayagam, C.; Shankar, A. Association between plasma homocysteine and microalbuminuria in persons without hypertension, diabetes mellitus, and cardiovascular disease. Clin. Exp. Nephrol. 2011, 15, 92–99. [Google Scholar] [CrossRef]
- Kuang, Z.M.; Wang, Y.; Feng, S.J.; Jiang, L.; Cheng, W.L. Association between plasma homocysteine and microalbuminuria in untreated patients with essential hypertension: A case-control study. Kidney Blood Press. Res. 2017, 42, 1303–1311. [Google Scholar] [CrossRef] [PubMed]
- Lehotský, J.; Tothová, B.; Kovalská, M.; Dobrota, D.; Beňová, A.; Kalenská, D.; Kaplán, P. Role of homocysteine in the ischemic stroke and development of ischemic tolerance. Front. Neurosci. 2016, 10, 538. [Google Scholar] [CrossRef] [PubMed]
- Esse, R.; Barroso, M.; Tavares de Almeida, I.; Castro, R. The contribution of homocysteine metabolism disruption to endothelial dysfunction: State-of-the-art. Int. J. Mol. Sci. 2019, 20, 867. [Google Scholar] [CrossRef] [PubMed]
- Kopetz, V.; Kennedy, J.; Heresztyn, T.; Stafford, I.; Willoughby, S.R.; Beltrame, J.F. Endothelial function, oxidative stress and inflammatory studies in chronic coronary slow flow phenomenon patients. Cardiology 2012, 121, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Ho, E.; Galougahi, K.K.; Liu, C.C.; Bhindi, R.; Figtree, G.A. Biological markers of oxidative stress: Applications to cardiovascular research and practice. Redox Biol. 2013, 1, 483–491. [Google Scholar] [CrossRef]
- Senoner, T.; Dichtl, W. Oxidative stress in cardiovascular diseases: Still a therapeutic target? Nutrients 2019, 11, 2090. [Google Scholar] [CrossRef]
- Xu, D.P.; Li, Y.; Meng, X.; Zhou, T.; Zhou, Y.; Zheng, J.; Zhang, J.J.; Li, H.B. Natural antioxidants in foods and medicinal plants: Extraction, assessment and resources. Int. J. Mol. Sci. 2017, 18, 96. [Google Scholar] [CrossRef]
- Li, D.; Rui, Y.X.; Guo, S.D.; Luan, F.; Liu, R.; Zeng, N. Ferulic acid: A review of its pharmacology, pharmacokinetics and derivatives. Life Sci. 2021, 284, 119921. [Google Scholar] [CrossRef]
- Pandi, A.; Raghu, M.H.; Chandrashekar, N.; Kalappan, V.M. Cardioprotective effects of Ferulic acid against various drugs and toxic agents. Beni-Suef Univ. J. Basic Appl. Sci. 2022, 11, 92. [Google Scholar] [CrossRef]
- Zhang, X.X.; Zhao, D.S.; Wang, J.; Zhou, H.; Wang, L.; Mao, J.L.; He, J.X. The treatment of cardiovascular diseases: A review of ferulic acid and its derivatives. Pharm.-Int. J. Pharm. Sci. 2021, 76, 55–60. [Google Scholar]
- Zduńska, K.; Dana, A.; Kolodziejczak, A.; Rotsztejn, H. Antioxidant properties of ferulic acid and its possible application. Skin Pharmacol. Physiol. 2018, 31, 332–336. [Google Scholar] [CrossRef] [PubMed]
- Zheng, M.; Liu, Y.; Zhang, G.; Yang, Z.; Xu, W.; Chen, Q. The Antioxidant Properties, Metabolism, Application and Mechanism of Ferulic Acid in Medicine, Food, Cosmetics, Livestock and Poultry. Antioxidants 2024, 13, 853. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.A. Anti-hypertensive effect of cereal antioxidant ferulic acid and its mechanism of action. Front. Nutr. 2019, 6, 121. [Google Scholar] [CrossRef] [PubMed]
- Yin, Z.N.; Wu, W.J.; Sun, C.Z.; Liu, H.F.; Chen, W.B.; Zhan, Q.P.; Lei, Z.G.; Xuan, X.I.; Juan, J.; Kun, Y.A.; et al. Antioxidant and anti-inflammatory capacity of ferulic acid released from wheat bran by solid-state fermentation of Aspergillus niger. Biomed. Environ. Sci. 2019, 32, 11–21. [Google Scholar] [PubMed]
- Sultan, S.; Acharya, Y.; Barrett, N.; Hynes, N. A pilot protocol and review of triple neuroprotection with targeted hypothermia, controlled induced hypertension, and barbiturate infusion during emergency carotid endarterectomy for acute stroke after failed tPA or beyond 24-hour window of opportunity. Ann. Transl. Med. 2020, 8, 1275. [Google Scholar] [CrossRef]
- Neto-Neves, E.M.; da Silva Maia Bezerra Filho, C.; Dejani, N.N.; de Sousa, D.P. Ferulic acid and cardiovascular health: Therapeutic and preventive potential. Mini Rev. Med. Chem. 2021, 21, 1625–1637. [Google Scholar] [CrossRef]
- Mallamaci, F.; Zoccali, C.; Tripepi, G.; Fermo, I.; Benedetto, F.A.; Cataliotti, A.; Bellanuova, I.; Malatino, L.S.; Soldarini, A. Hyperhomocysteinemia predicts cardiovascular outcomes in hemodialysis patients. Kidney Int. 2002, 61, 609–614. [Google Scholar] [CrossRef]
- Zhang, S.; Lv, Y.; Luo, X.; Weng, X.; Qi, J.; Bai, X.; Zhao, C.; Zeng, M.; Bao, X.; Dai, X.; et al. Homocysteine promotes atherosclerosis through macrophage pyroptosis via endoplasmic reticulum stress and calcium disorder. Mol. Med. 2023, 29, 73. [Google Scholar] [CrossRef]
- Ulivelli, M.; Priora, R.; Di Giuseppe, D.; Coppo, L.; Summa, D.; Margaritis, A.; Frosali, S.; Bartalini, S.; Martini, G.; Cerase, A.; et al. Homocysteinemia control by cysteine in cerebral vascular patients after methionine loading test: Evidences in physiological and pathological conditions in cerebro-vascular and multiple sclerosis patients. Amino Acids 2016, 48, 1477–1489. [Google Scholar] [CrossRef]
- Durand, P.; Prost, M.; Loreau, N.; Lussier-Cacan, S.; Blache, D. Impaired homocysteine metabolism and atherothrombotic disease. Lab. Investig. 2001, 81, 645–672. [Google Scholar] [CrossRef]
- Graham, I.M.; O’Callaghan, P. Vitamins, homocysteine and cardiovascular risk. Cardiovasc. Drugs Ther. 2002, 16, 383–389. [Google Scholar] [CrossRef] [PubMed]
- Breilmann, J.; Pons-Kühnemann, J.; Brunner, C.; Richter, M.; Neuhäuser-Berthold, M. Effect of antioxidant vitamins on the plasma homocysteine level in a free-living elderly population. Ann. Nutr. Metab. 2011, 57, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Desouza, C.; Keebler, M.; McNamara, D.B.; Fonseca, V. Drug’s affecting homocysteine metabolism: Impact on cardiovascular risk. Drugs 2002, 62, 605–616. [Google Scholar] [CrossRef]
- Reynolds, E.H. Antiepileptic drugs, folate and one carbon metabolism revisited. Epilepsy Behav. 2020, 112, 107336. [Google Scholar] [CrossRef]
- Maru, L.; Verma, M.; Jinsiwale, N. Homocysteine as predictive marker for pregnancy-induced hypertension—A comparative study of homocysteine levels in normal versus patients of PIH and its complications. J. Obstet. Gynecol. India 2016, 66, 167–171. [Google Scholar] [CrossRef] [PubMed]
- O’callaghan, P.; Meleady, R.; Fitzgerald, T.; Graham, I. Smoking and plasma homocysteine. Eur. Heart J. 2002, 23, 1580–1586. [Google Scholar] [CrossRef]
- Gibson, A.; Woodside, J.V.; Young, I.S.; Sharpe, P.C.; Mercer, C.; Patterson, C.C.; McKinley, M.C.; Kluijtmans, L.A.; Whitehead, A.S.; Evans, A. Alcohol increases homocysteine and reduces B vitamin concentration in healthy male volunteers—A randomized, crossover intervention study. QJM Int. J. Med. 2008, 101, 881–887. [Google Scholar] [CrossRef]
- Fallah, S.; Nouroozi, V.; Seifi, M.; Samadikuchaksaraei, A.; Aghdashi, E.M. Influence of oral contraceptive pills on homocysteine and nitric oxide levels: As risk factors for cardiovascular disease. J. Clin. Lab. Anal. 2012, 26, 120–123. [Google Scholar] [CrossRef]
- Aswar, U.; Mahajan, U.; Nerurkar, G.; Aswar, M. Amelioration of cardiac hypertrophy induced by abdominal aortic banding in ferulic acid treated rats. Biomed. Aging Pathol. 2013, 3, 209–217. [Google Scholar] [CrossRef]
- Aswar, U.; Mahajan, U.; Kandhare, A.; Aswar, M. Ferulic acid ameliorates doxorubicin-induced cardiac toxicity in rats. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2019, 392, 659–668. [Google Scholar] [CrossRef]
- Trombino, S.; Serini, S.; Di Nicuolo, F.; Celleno, L.; Andò, S.; Picci, N.; Calviello, G.; Palozza, P. Antioxidant effect of ferulic acid in isolated membranes and intact cells: Synergistic interactions with α-tocopherol, β-carotene, and ascorbic acid. J. Agric. Food Chem. 2004, 52, 2411–2420. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Godber, J.S. Antioxidant activities of major components of γ-oryzanol from rice bran using a linoleic acid model. J. Am. Oil Chem. Soc. 2001, 78, 645. [Google Scholar] [CrossRef]
- Maurya, D.K.; Devasagayam, T.P. Antioxidant and prooxidant nature of hydroxycinnamic acid derivatives ferulic and caffeic acids. Food Chem. Toxicol. 2010, 48, 3369–3373. [Google Scholar] [CrossRef] [PubMed]
- Kikuzaki, H.; Hisamoto, M.; Hirose, K.; Akiyama, K.; Taniguchi, H. Antioxidant properties of ferulic acid and its related compounds. J. Agric. Food Chem. 2002, 50, 2161–2168. [Google Scholar] [CrossRef] [PubMed]
- Blom, H.J. Homocysteine and Cholesterol: Basic and Clinical Interactions. In Homocysteine and Vascular Disease. Developments in Cardiovascular Medicine; Robinson, K., Ed.; Springer: Dordrecht, The Netherlands, 2000; Volume 230. [Google Scholar] [CrossRef]
- Jain, P.G.; Surana, S.J. Isolation, characterization and hypolipidemic activity of ferulic acid in high-fat-diet-induced hyperlipidemia in laboratory rats. EXCLI J. 2016, 15, 599. [Google Scholar]
- Kamal-Eldin, A.; Frank, J.; Razdan, A.; Tengblad, S.; Basu, S.; Vessby, B. Effects of dietary phenolic compounds on tocopherol, cholesterol, and fatty acids in rats. Lipids 2000, 35, 427–435. [Google Scholar] [CrossRef]
- Kim, H.K.; Jeong, T.S.; Lee, M.K.; Park, Y.B.; Choi, M.S. Lipid-lowering efficacy of hesperetin metabolites in high-cholesterol fed rats. Clin. Chim. Acta 2003, 327, 129–137. [Google Scholar] [CrossRef]
- Pacher, P.; Beckman, J.S.; Liaudet, L. Nitric oxide and peroxynitrite in health and disease. Physiol. Rev. 2007, 87, 315–424. [Google Scholar] [CrossRef]
- Faraci, F.M.; Lentz, S.R. Hyperhomocysteinemia, oxidative stress, and cerebral vascular dysfunction. Stroke 2004, 35, 345–347. [Google Scholar] [CrossRef]
- Woo, C.W.; Prathapasinghe, G.A.; Siow, Y.L.; Karmin, O. Hyperhomocysteinemia induces liver injury in rat: Protective effect of folic acid supplementation. Biochim. Biophys. Acta-Mol. Basis Dis. 2006, 1762, 656–665. [Google Scholar] [CrossRef]
- Rukkumani, R.; Aruna, K.; Suresh Varma, P.; Padmanabhan Menon, V. Hepatoprotective role of ferulic acid: A dose-dependent study. J. Med. Food 2004, 7, 456–461. [Google Scholar] [CrossRef] [PubMed]
- Eldibany, M.M.; Caprini, J.A. Hyperhomocysteinemia and thrombosis: An overview. Arch. Pathol. Lab. Med. 2007, 131, 872–884. [Google Scholar] [CrossRef]
- Liu, Q.; Lin, B.; Tao, Y. Improved methylation in E. coli via an efficient methyl supply system driven by betaine. Metab. Eng. 2022, 72, 46–55. [Google Scholar] [CrossRef] [PubMed]
- Stead, L.M.; Brosnan, M.E.; Brosnan, J.T. Characterization of homocysteine metabolism in the rat liver. Biochem. J. 2000, 350, 685–692. [Google Scholar] [CrossRef]
- Azad, M.A.; Huang, P.; Liu, G.; Ren, W.; Teklebrh, T.; Yan, W.; Zhou, X.; Yin, Y. Hyperhomocysteinemia and cardiovascular disease in animal model. Amino Acids 2018, 50, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Macfarlane, P.W. Normal limits of ECG measurements related to atrial activity using a modified limb lead system. Anatol. J. Cardiol. 2015, 15, 7. [Google Scholar] [CrossRef][Green Version]
- Aygun, H.; Basol, N.; Gul, S.S. Cardioprotective Effect of Paricalcitol on Amitriptyline-Induced Cardiotoxicity in Rats: Comparison of [99m Tc] PYP Cardiac Scintigraphy with Electrocardiographic and Biochemical Findings. Cardiovasc. Toxicol. 2020, 20, 427–436. [Google Scholar] [CrossRef]
- Li, N.; Tian, Y.; Wang, C.; Zhang, P.; You, S. Protective effect of Lai Fu Cheng Qi decoction on severe acute pancreatitis-induced myocardial injury in a rat model. Exp. Ther. Med. 2015, 9, 1133–1140. [Google Scholar] [CrossRef]
- Tawfik, A.; Mohamed, R.; Elsherbiny, N.M.; DeAngelis, M.M.; Bartoli, M.; Al-Shabrawey, M. Homocysteine: A potential biomarker for diabetic retinopathy. J. Clin. Med. 2019, 8, 121. [Google Scholar] [CrossRef]
- El-Sherbeeny, N.A.; Nader, M.A.; Attia, G.M.; Ateyya, H. Agmatine protects rat liver from nicotine-induced hepatic damage via antioxidative, antiapoptotic, and antifibrotic pathways. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2016, 389, 1341–1351. [Google Scholar] [CrossRef]
- Sun, J.; Zhang, X.; Broderick, M.; Fein, H. Measurement of nitric oxide production in biological systems by using Griess reaction assay. Sensors 2003, 3, 276–284. [Google Scholar] [CrossRef]
- Ronco, M.T.; Francés, D.; de Luján Alvarez, M.; Quiroga, A.; Monti, J.; Parody, J.P.; Pisani, G.; Carrillo, M.C.; Carnovale, C.E. Vascular endothelial growth factor and nitric oxide in rat liver regeneration. Life Sci. 2007, 81, 750–755. [Google Scholar] [CrossRef]
- Ganeshpurkar, A.; Singh, R.; Gore, P.G.; Kumar, D.; Gutti, G.; Kumar, A.; Singh, S.K. Structure-based screening and molecular dynamics simulation studies for the identification of potential acetylcholinesterase inhibitors. Mol. Simul. 2020, 46, 169–185. [Google Scholar] [CrossRef]
- Morris, G.M.; Huey, R.; Lindstrom, W.; Sanner, M.F.; Belew, R.K.; Goodsell, D.S.; Olson, A.J. AutoDock4 and AutoDockTools4: Automated docking with selective receptor flexibility. J. Comput. Chem. 2009, 30, 2785–2791. [Google Scholar] [CrossRef] [PubMed]
- Pettersen, E.F.; Goddard, T.D.; Huang, C.C. UCSF Chimera—A visualization system for exploratory research and analysis. J. Comput. Chem. 2004, 25, 1605–1612. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).