Anti-Yo Paraneoplastic Cerebellar Degeneration and Breast Cancer: A Long Survival of Persistent Cerebellar Syndrome
Abstract
:1. Introduction
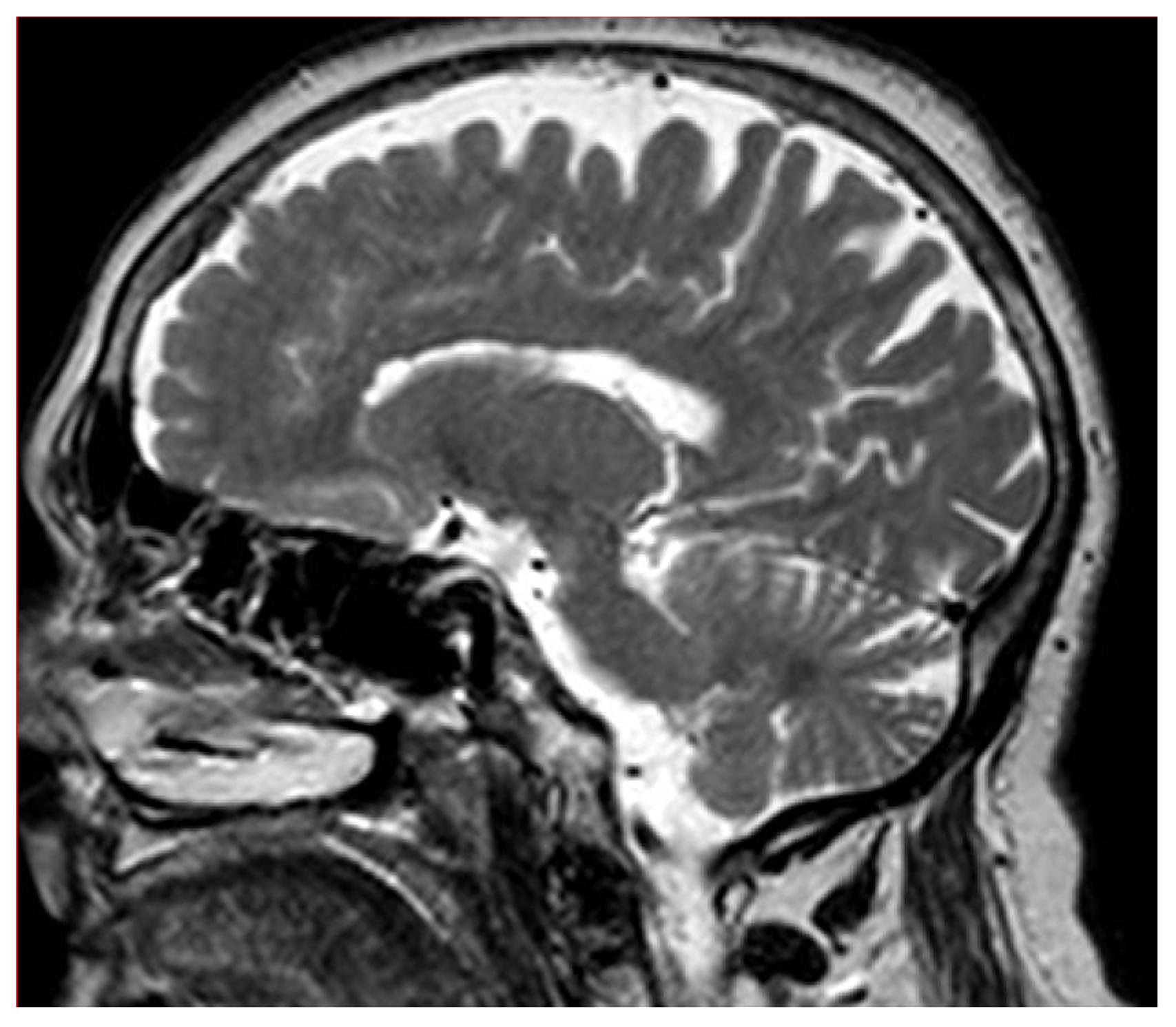
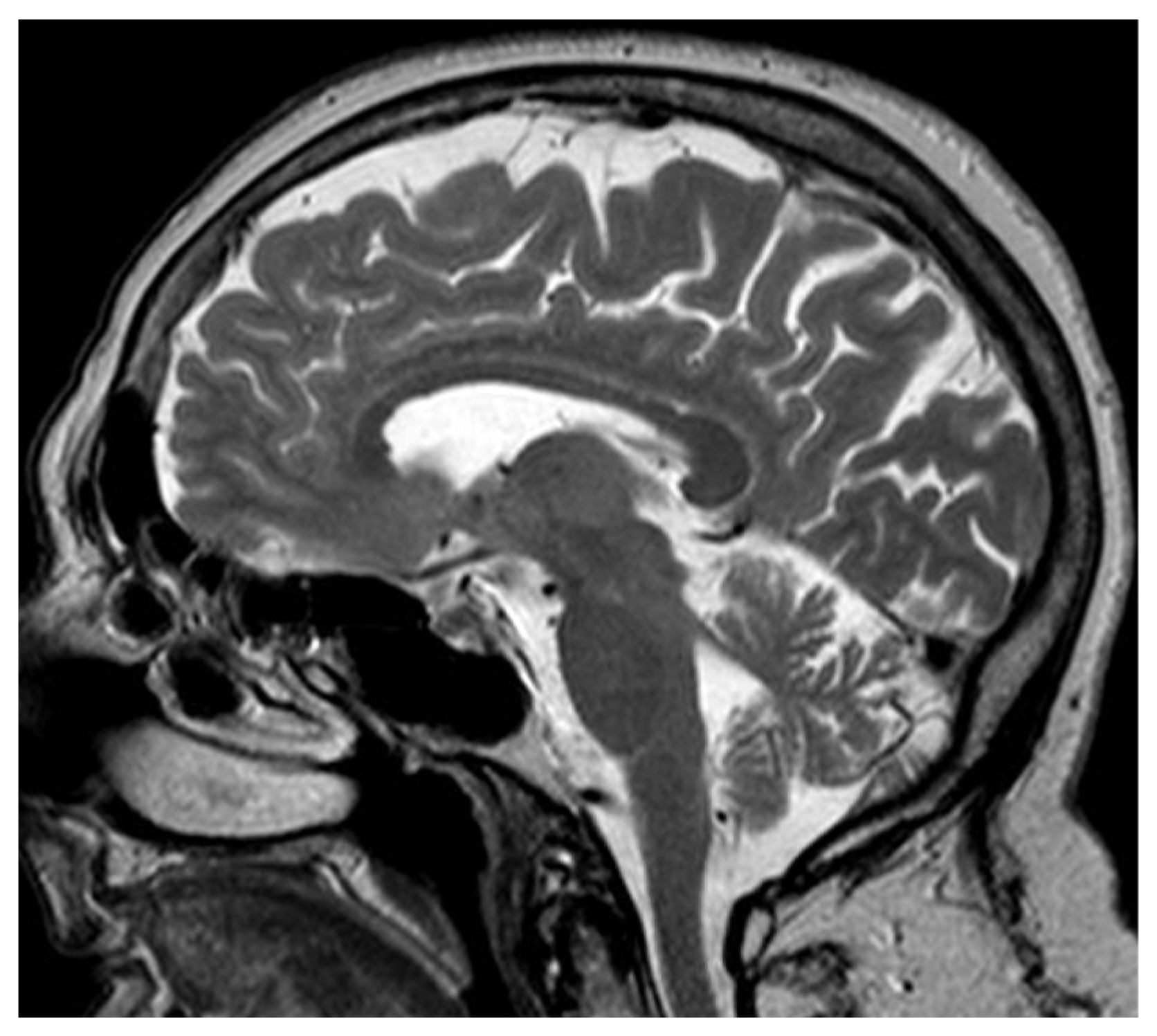
2. Case Description
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dalmau, J.; Rosenfeld, M.R. Paraneoplastic syndromes of the CNS. Lancet Neurol. 2008, 7, 327–340. [Google Scholar] [CrossRef] [Green Version]
- Shams’ili, S.; Grefkens, J.; de Leeuw, B.; van den Bent, M.; Hooijkaas, H.; van der Holt, B.; Vecht, C.; Sillevis Smitt, P. Paraneoplastic cerebellar degeneration associated with antineuronal antibodies: Analysis of 50 patients. Brain 2003, 126, 1409–1418. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mason, W.P.; Graus, F.; Lang, B.; Honnorat, J.; Delattre, J.Y.; Valldeoriola, F.; Antoine, J.C.; Rosenblum, M.K.; Rosenfeld, M.R.; Newsom-Davis, J.; et al. Small-Cell Lung Cancer, Paraneoplastic Cerebellar Degeneration and the Lambert-Eaton Myasthenic Syndrome. Brain A J. Neurol. 1997, 120, 1279–1300. [Google Scholar] [CrossRef] [PubMed]
- Rojas-Marcos, I.; Rousseau, A.; Keime-Guibert, F.; Reñé, R.; Cartalat-Carel, S.; Delattre, J.Y.; Graus, F. Spectrum of Paraneoplastic Neurologic Disorders in Women with Breast and Gynecologic Cancer. Medicine 2003, 82, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Honnorat, J.; Cartalat-Carel, S.; Ricard, D.; Camdessanche, J.P.; Carpentier, A.F.; Rogemond, V.; Chapuis, F.; Aguera, M.; Decullier, E.; Duchemin, A.M.; et al. Onco-Neural Antibodies and Tumour Type Determine Survival and Neurological Symptoms in Paraneoplastic Neurological Syndromes with Hu or CV2/CRMP5 Antibodies. J. Neurol. Neurosurg. Psychiatry 2009, 80, 412–416. [Google Scholar] [CrossRef] [Green Version]
- Meglic, B.; Graus, F.; Grad, A. Anti-Yo-Associated Paraneoplastic Cerebellar Degeneration in a Man with Gastric Ade-nocarcinoma. J. Neurol. Sci. 2001, 185, 135–138. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, K. Pathogenesis of paraneoplastic neurological syndromes. Brain Nerve 2010, 62, 309–318. [Google Scholar] [PubMed]
- Widdess-Walsh, P.; Tavee, J.O.; Schuele, S.; Stevens, G.H. Response to intravenous immunoglobulin in Anti-Yo associated paraneoplastic cerebellar degeneration: Case report and review of the literature. J. Neuro-Oncol. 2003, 63, 187–190. [Google Scholar] [CrossRef] [PubMed]
- Uchuya, M.; Graus, F.; Vega, F.; Rene, R.; Delattre, J.Y. Intravenous immunoglobulin treatment in paraneoplastic neurological syndromes with antineuronal autoantibodies. J. Neurol. Neurosurg. Psychiatry 1996, 60, 388–392. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Phuphanich, S.; Brock, C. Neurologic Improvement after High-dose Intravenous Immunoglobulin Therapy in Patients with Paraneoplastic Cerebellar Degeneration Associated with Anti-Purkinje Cell Antibody. J. Neuro-Oncol. 2006, 81, 67–69. [Google Scholar] [CrossRef] [PubMed]
- Hu, F.Q.; Shang, F.R.; Liu, J.J.; Yuan, H. Plasma Exchange for Treating Anti-Yo-Associated Paraneoplastic Cerebellar Degeneration: Case Report and Literature Review. Medicine 2020, 99, e21760. [Google Scholar] [CrossRef] [PubMed]
- Meloni, C.; Iani, C.; Dominijanni, S.; Arciprete, F.; Cipriani, S.; Caramiello, M.S.; Tozzo, C.; Lombardo, P.A.; Tatangelo, P.; Cecilia, A.; et al. A Case Report of Plasma Exchange Therapy in Non-paraneoplastic Cerebellar Ataxia Associated with Anti-Yo Antibody. Ther. Apher. Dial. 2004, 8, 500–502. [Google Scholar] [CrossRef] [PubMed]
- Vedeler, C.A.; Antoine, J.C.; Giometto, B.; Graus, F.; Grisold, W.; Hart, I.K.; Honnorat, J.; Sillevis Smitt, P.A.E.; Verschuuren, J.J.G.M.; Voltz, R.; et al. Management of Paraneoplastic Neu-rological Syndromes: Report of an EFNS Task Force. Eur. J. Neurol. 2006, 13, 682–690. [Google Scholar] [CrossRef] [PubMed]
- Titulaer, M.J.; Soffietti, R.; Dalmau, J.; Gilhus, N.E.; Giometto, B.; Graus, F.; Grisold, W.; Honnorat, J.; Sillevis Smitt, P.A.E.; Tanasescu, R.; et al. Screening for Tumours in Paraneoplastic Syndromes: Report of an EFNS Task Force: Screening for Tumours in PNS. Eur. J. Neurol. 2011, 18, 19-e3. [Google Scholar] [CrossRef] [Green Version]
- Rojas, I.; Graus, F.; Keime-Guibert, F.; Rene, R.; Delattre, J.Y.; Ramon, J.M.; Dalmau, J.; Posner, J.B. Long-Term Clinical Outcome of Para-neoplastic Cerebellar Degeneration and Anti-Yo Antibodies. Neurology 2000, 55, 713–715. [Google Scholar] [CrossRef] [PubMed]
- Rojas, I.; Graus, F.; Keime-Guibert, F.; Rene, R.; Delattre, J.Y.; Ramon, J.M.; Dalmau, J.; Posner, J.B. Paraneoplastic Cerebellar Degeneration. I. A Clinical Analysis of 55 Anti-Yo Antibody-Positive Patients. Neurology 1992, 42, 1931–1937. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Avino, G.; De Marchi, F.; Cantello, R.; Mazzini, L. Anti-Yo Paraneoplastic Cerebellar Degeneration and Breast Cancer: A Long Survival of Persistent Cerebellar Syndrome. Sclerosis 2023, 1, 5-8. https://doi.org/10.3390/sclerosis1010002
Avino G, De Marchi F, Cantello R, Mazzini L. Anti-Yo Paraneoplastic Cerebellar Degeneration and Breast Cancer: A Long Survival of Persistent Cerebellar Syndrome. Sclerosis. 2023; 1(1):5-8. https://doi.org/10.3390/sclerosis1010002
Chicago/Turabian StyleAvino, Gianluca, Fabiola De Marchi, Roberto Cantello, and Letizia Mazzini. 2023. "Anti-Yo Paraneoplastic Cerebellar Degeneration and Breast Cancer: A Long Survival of Persistent Cerebellar Syndrome" Sclerosis 1, no. 1: 5-8. https://doi.org/10.3390/sclerosis1010002
APA StyleAvino, G., De Marchi, F., Cantello, R., & Mazzini, L. (2023). Anti-Yo Paraneoplastic Cerebellar Degeneration and Breast Cancer: A Long Survival of Persistent Cerebellar Syndrome. Sclerosis, 1(1), 5-8. https://doi.org/10.3390/sclerosis1010002





