Abstract
The classical approach for the preparation of an endodontically treated molar with a post and core involves widening the anatomically complex system of canals, which may be narrow or curved with variable angulation. The aforementioned along with the fact that restorative dentistry stands against the wastage of tooth tissue make endocrowns an appealing alternative. Bindl and Mörmann first described an all-ceramic crown anchored to the internal portion of the pulp chamber and on the cavity margins, thus obtaining macromechanical retention provided by the axial opposing pulpal walls and microretention attained with the use of adhesive cementation. The purpose of this report is to describe the protocol for the treatment plan selection, preparation, impression, and adhesive cementation of an endocrown with a follow-up of 5 years. A 56-year-old male patient presented to the Postgraduate Clinic of Prosthodontics seeking rehabilitation for tooth No. #36. A clinical examination revealed multiple immediate composite resin restorations with unacceptable morphology and adaptation to the remaining tooth as well as a lack of a contact point but, rather, a large, concave contact area facilitating food entrapment. Since the tooth was endodontically treated, the proposed treatment plan included the fabrication of an all-ceramic endocrown. The steps of preparation, attribution of the correct shape, impression, and adhesive luting under rubber dam isolation are thoroughly described. The final functional and aesthetic result, patient’s satisfaction, and the 5-year follow-up render restorations such as endocrowns, which draw their retention from adhesive luting, a viable alternative to conventional approaches.
1. Introduction
Coronal defects, carious lesions, and access cavity that lead to the loss of the continuity of the dental structure result in severely reduced dental resistance to forces by 63% [1]. Moreover, removal of the pulp tissue leads to deterioration of proprioception, thus reducing protective mechanisms against excessive masticatory forces [2].
Post and core systems along with a full-coverage prosthesis comprise the traditional approach for the restoration of an endodontically treated tooth. This technique involves widening the root canal system, which vary in terms of width and angulation [3]. This procedure results both in the excessive loss of the tooth structure and a high risk of root perforation [4,5].
Plenty of contemporary literature reports, which claim that teeth restored with posts have similar fracture resistance to those without posts, suggest that posts are not a prerequisite for the restoration of endodontically treated teeth [6]. Anchorage provided only by the pulp chamber has been proven enough to provide sufficient retention [6].
The aforementioned along with the ongoing need for healthy dental tissue preservation gave birth to the concept of endocrowns. Pissis and Bindl and Mormann first described this term as an all-ceramic crown extended within the pulp chamber that gained micromechanical retention from adhesive cementation and macromechanical retention offered by the axial pulpal walls [4,6,7].
Even though recent studies have confirmed the efficacy of endocrowns with survival rates similar to those of conventional crowns, epidemiological studies have shown that they are still outweighed by conventional crowns regarding dental practitioners’ preference for the restoration of endodontically treated teeth, mainly due to insufficient informing and training [8,9]. Moreover, there is a lack of studies elaborating on their use and application. Therefore, the purpose of this report is to describe the protocol for treatment plan selection, preparation, management of the remaining dental tissues in terms of adhesive luting facilitation, impression, and delivery via the adhesive luting of an endocrown fabricated for an endodontically treated molar, with a follow-up of 5 years.
2. Materials and Methods
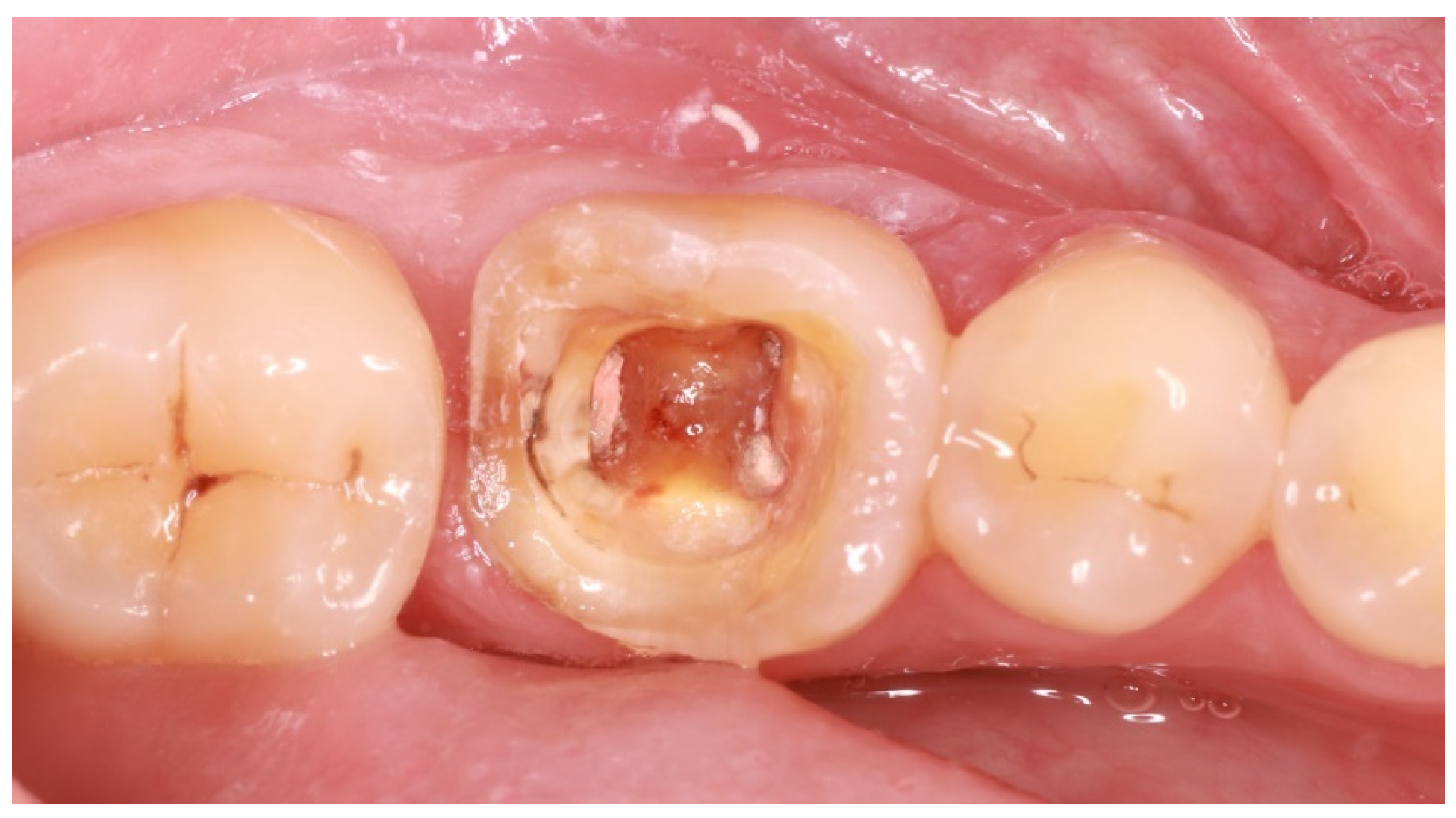
A 57-year-old male patient presented to the XXX Clinic of the XXX University of XXX seeking dental rehabilitation. The chief complaint was the compromised restoration of tooth No. #36 (Figure 1). His medical record did not reveal any disease or medication intake. Clinical examination revealed multiple immediate composite resin restorations with unacceptable morphology and adaptation to the remaining tooth structure as well as lack of contact point but rather a large, concave contact area facilitating food entrapment. After radiographic examination and given that the tooth was endodontically treated and the antagonist was slightly overerupted and limited prosthetic space would be available, the proposed treatment plan included the fabrication of an all-ceramic endocrown. Implant-supported restorations were also proposed for the restoration of missing teeth No. #46 and 47 but due to financial limitations, the patient only wished for the restoration of tooth No. #36 (Figure 1).

Figure 1.
Initial situation.
First, existing restorations and decayed tissue were removed. Given that the tooth was restorable, a provisional restoration was placed in order to prevent microleakage and the patient was referred for an endodontic reintervention as the existing root canal treatment was not satisfactory. Enamel presence at a percentage higher than 80% of the tooth circumference substantiated the choice of an endocrown restoration (Figure 2). This type of prosthesis demands the presence of healthy enamel for the adhesive procedures to be more effective [10]. This condition is so crucial that many reports have placed a lack of cervical enamel among the contraindications for endocrown restorations [11].

Figure 2.
Adequate enamel presence after removal of previous restorations.
As endocrowns primarily gain retention from adhesive cementation procedures, steps in order to increase micromechanical retention should be incorporated in the applied protocols [11]. In the case described and after the successful endodontic reintervention, the technique of immediate dentin sealing (IDS) was applied on the freshly cut dentin after rubber dam placement [12]. Dentin bonding agent and flowable composite were applied on exposed dentin after removal of the superficial 2 mm of gutta-percha in order to acquire adequate composite resin thickness to avoid microleakage. Cuspal reduction was also performed at this stage so as to both acquire enough interocclusal space for the restorative material of choice, which, in this case, was lithium disilicate, and confirm the presence of dental walls of adequate thickness (Figure 3). Lithium disilicate was chosen because of the positive results regarding the survival rates reported by clinical trials [13].

Figure 3.
Confirmation of adequate interocclusal space presence.
Some of the benefits that have been reported for the IDS technique are the superior bond strength acquired by the contaminant-free dentin, avoidance of hybrid layer collapse during restoration placement, maturation of the dentin bond in a stress-free environment, and reduction in bacterial penetration [14].
After IDS application, the tooth was initially prepared to expose any enamel areas that were covered by dentin bonding agent or composite. Care must be given to keep margins as supragingival as possible both to preserve cervical enamel and facilitate the steps of impression-making and adhesive luting. Pulp chamber walls were prepared according to the reverse preparation technique in a 5–7° occlusal divergence. A 90° circumferential butt joint margin was attributed [11]. All transitions should be as smooth as possible [15] (Figure 4).

Figure 4.
Final preparation after IDS application, with supragingival butt joint margins and smooth internal transitions.
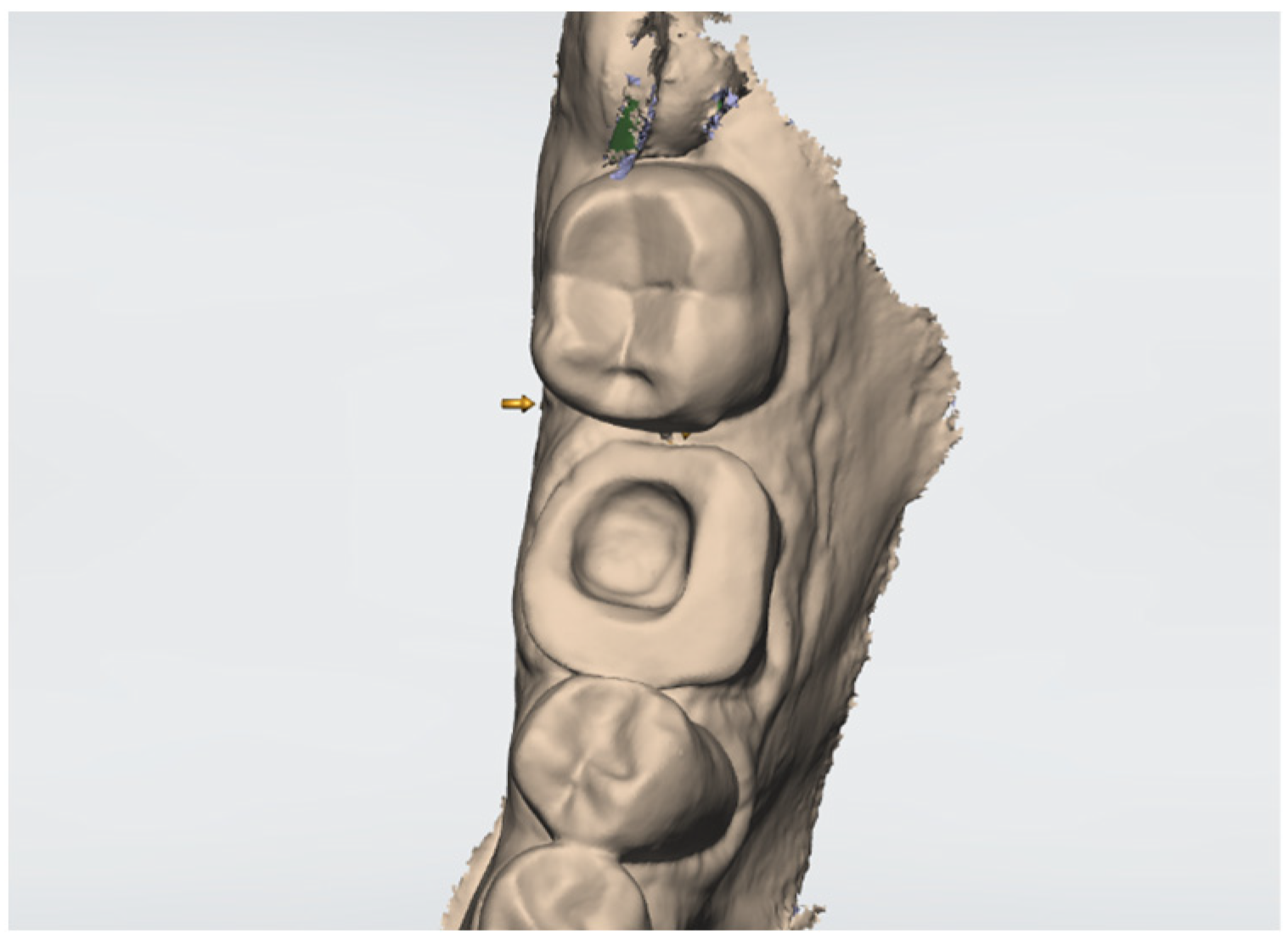
A digital impression was made at the same appointment. No cord placement was necessary due to absence of subgingival margins. Smooth internal transitions facilitate this step and reduce stress concentration areas at the final restoration. Digital impression offers the opportunity for area inspection at magnification to exclude the possibility of any inaccuracy or absence of adequate interocclusal space (Figure 5). Shade selection was also made with the aid of the intraoral scanner and the case order was sent to the dental laboratory. Since IDS was applied and the prosthesis would be delivered in a few days, there was no need for provisional restoration placement.

Figure 5.
Scan overview under magnification. Digital image should correspond to the clinical situation.
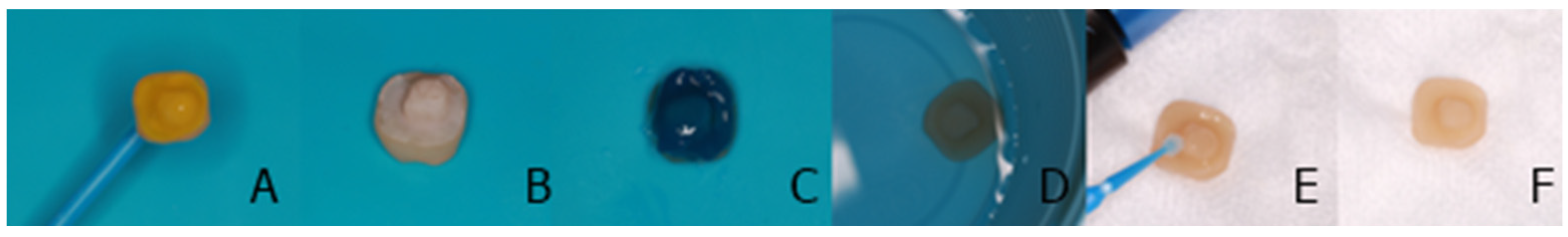
The final lithium disilicate restoration was first inspected on the working cast to check fit, contact points, and occlusal contacts. Intraoral check rendered all the aforementioned satisfactory. Since the patient approved the aesthetic appearance of the restoration, surface treatment procedures took place. Hyfrofluoric acid 9% for 20 s, phosphoric acid 37% for 30 s, ultrasonic cleaning, and silane were applied to the internal surface of the endocrown [16] (Figure 6).

Figure 6.
Steps for the lithium disilicate endocrown internal surface treatment. (A) Hydrofluoric acid application, (B) surface inspection for adequate etching, (C) 37% orthophosphoric acid application, (D) ultrasonic cleaning, (E) restoration primer application, (F) endocrown internal surface after gentle air-blow.
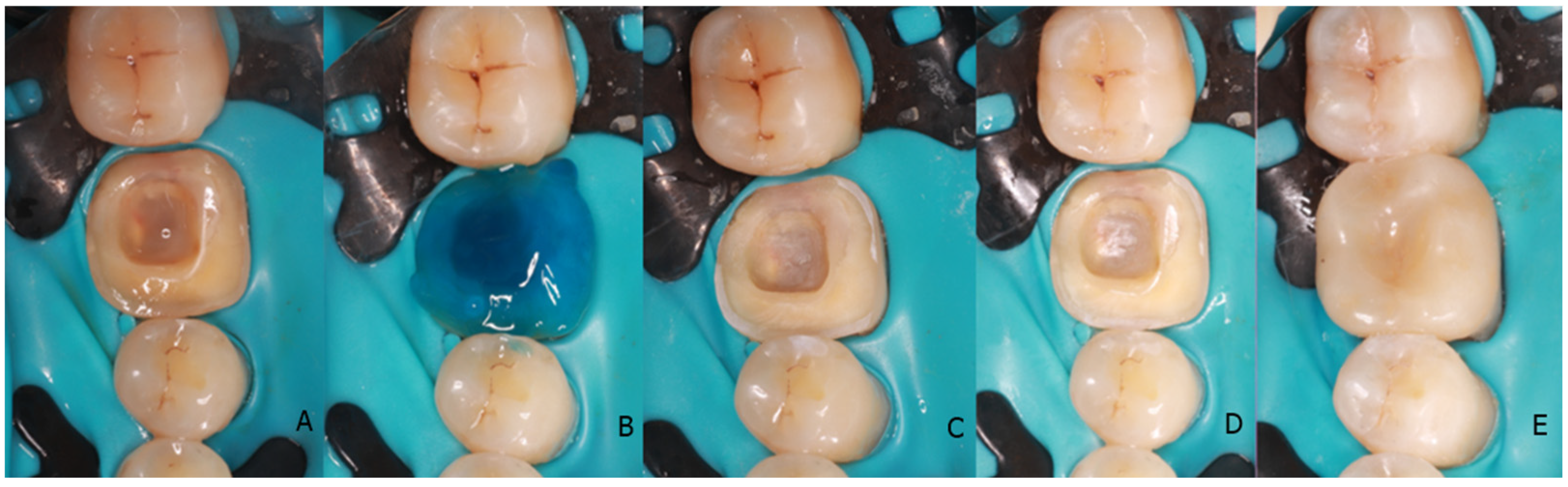
After rubber dam isolation, air-particle abrasion (50 μm Al2O3) and phosphoric acid were applied on the prepared area [14] (Figure 7). A dual-cure resin cement (Panavia V5, Kuraray Europe GmbH, Hattersheim, Germany) was chosen for this case. Primer was applied on both the endocrown internal surface and prepared tooth before resin cement application. The restoration was placed in the correct position and excess cement was meticulously removed after tack cure [17]. Final polymerization was performed for 20 s from the buccal, lingual, and occlusal area and an additional 20 s polymerization was performed at all sides with the presence of glycerine gel to remove the oxygen inhibition layer [18].

Figure 7.
Tooth surface treatment protocol. (A) Rubber dam placement, (B) application of 37% orthophosphoric acid, (C) surface inspection for adequate etching, (D) tooth primer application, (E) endocrown adhesive luting.
After removal of the rubber dam, the area was inspected for any cement remnants. Occlusion was checked as well as contact points. The final result was approved by the patient, who also received thorough oral hygiene instructions (Figure 8).

Figure 8.
Postoperative view after excess cement removal.
Five years later, the patient returned for the rehabilitation of missing teeth No. #46 and 47. Tooth No. #48 was extracted and two implants were placed. After 4 months, two screw-retained implant-supported crowns were delivered. The endocrown on tooth No. #36 was still in place and in excellent condition (Figure 9).

Figure 9.
Occlusal view five years after the endocrown delivery on tooth No. #36. The restoration is still in place, scoring “Alfa” in all of the USPHS criteria utilized for the re-evaluation.
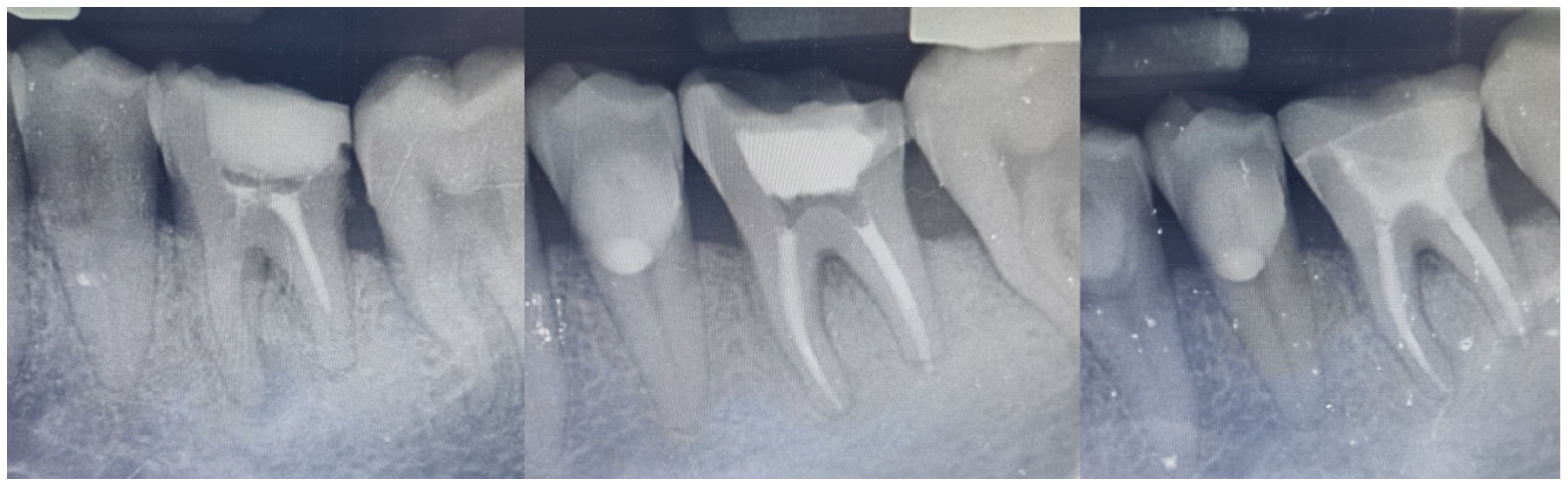
The Modified US Public Health Service (USPHS) criteria were used for the objective evaluation of the restoration at the five-year recall [19]. Two authors (E.P. and T.K.S.), other than the one who delivered the endocrown (D.P.), were chosen to evaluate the restoration, and both of them rated the restoration as “Alfa” in all of the included parameters, which corresponds to the ideal clinical situation. Radiographic evaluation (Figure 10) did not reveal any pathology or defective areas.

Figure 10.
Radiographic images at baseline, after the RCT reintervention and at the 5-year recall.
3. Results
The present case report aims to describe the step-by-step protocol for treatment plan selection, preparation, impression, and adhesive luting of an endocrown fabricated for an endodontically treated molar. The main benefit of such a restoration is the avoidance of excessive dentin removal for post placement, as required in the traditional post and core approach, thus omitting the risk of recontamination [20]. According to some researchers, posts are not necessary, given that the pulpal walls and pulp floor provide adequate retention and resistance [21]. This is justified by systematic reviews reporting survival rates greater than 90% after 10 years for endocrowns on molars [22].
Another advantage is the use of one homogenous monoblock restoration. The traditional approach encompasses a combination of different materials, and thus, a higher number of interfaces that influences stress distribution [23]. Moreover, these materials have different elastic moduli, some of which might vary greatly and present a stiffness mismatch with dental tissues [23].
The materials utilized in this type of prosthesis must have the potential to be adhesively bonded to dental tissues, since endocrown retention mainly relies on bonding [24]. Resin composite and lithium disilicate are among the most preferred materials, with the latter combining both mechanical and aesthetic properties [25]. Zirconia-reinforced silicate ceramic endocrowns have been connected with a high percentage of non-restorable mechanical failures due to the material greater stiffness [26].
A recently described approach incorporated the use of stress-tolerant base materials such as fiber-reinforced composites to support indirect restorations [27]. Fiber-reinforced composite resins may impede crack propagation, thereby increasing fracture resistance [28]. Moreover, glass fibers have been shown to limit polymerization shrinkage, and these materials can be packed in bulk up to 4 mm [29]. This type of material has also been recommended as one of the treatment options for large-sized cavities and direct onlays [30].
Some of the abovementioned properties have been substantiated in the literature. There are also some reports indicating that there is no significant effect concerning fracture resistance and a negative effect on marginal adaptation [31]. Regarding bond strength, it has been reported that fiber-reinforced composites have no significant effect on the shear bond strength [27].
However, this treatment choice entails certain limitations and concerns [28]. The higher viscosity of this type of composite resin could cause more voids, especially at the internal line angles and corners of the tooth preparation due to insufficient cavity adaptation [28]. Clinicians should also be aware of the type of the fiber-reinforced composite indicated for each case, as each of the bidirectional, unidirectional, and short-fiber-reinforced resin composites responds differently depending on the type and direction of the applied force [32]. It has been stated that fracture resistance mainly depends on the type of cover used for indirect onlay and is independent of the type of core buildup material used [28]. For these materials to perform optimally, the fiber-reinforced composite should follow the shape of the underlying dentin, thereby making this type of restoration clinically challenging [32]. At the time the described case was in progress, there was a gap in the knowledge regarding the use of this type of material due to the absence of clinical trials to validate its clinical performance [29].
Adhesive failure is the most common problem associated with endocrowns [33]. The higher the elastic modulus of the material, the higher the stress transferred to the adhesive interface. This fact makes adhesive luting procedures a crucial aspect of the treatment protocol. Techniques such as IDS, which have been proven to offer superior bonding strength and facilitate the applied procedures, should be implemented [14]. Care should be taken so that the materials chosen undergo proper surface treatment so as to enhance their surface quality for proper bonding [34].
Rubber dam placement is among the prerequisites associated with this type of restoration. Except for the substantiated effect on the success of root canal treatment, rubber dam placement has been shown to increase bond strength independent of the adhesive system [35,36]. Besides superior adhesive bonding, rubber dam placement has also been connected with reduced levels of patient stress, making procedures executed by the dental clinician easier to perform [37].
The present review aims to cover a gap in the literature regarding the detailed protocols applied for the restoration of endodontically treated teeth using endocrowns. The objective is to thoroughly describe, along with the corresponding figures, each of the individual steps that should be followed to gain the benefits of a minimally invasive restorative technique as endocrowns, compared to the traditional post and core approaches that have been extensively analyzed in the literature. Moreover, the novelty of this report refers to the incorporation and inclusion of justified techniques, such as IDS, that facilitate adhesive luting procedures, within the described protocol. The efficacy of this protocol is verified by the clinical and radiographic images of the 5-year follow-up, which proves that an adequate endodontic therapy should always be followed by a carefully executed and delivered prosthetic restoration. This case report also entails certain limitations. Even though useful conclusions can be derived from the study of case reports, well-designed, randomized clinical trials are needed to safely study the effect of a treatment modality. The USPHS criteria applied for the recall evaluation were chosen because of their broad use in many clinical reports. However, they do not evaluate all the numerous variables but only the degree of deviation from an ideal restoration.
4. Conclusions
The purpose of this report is to describe the protocol for the treatment plan selection, preparation, impression, and adhesive luting of an endocrown for an endodontically treated molar. The use of one homogenous monoblock restoration offers several advantages and omits the problems connected with traditional restorative approaches. If certain conditions are met in terms of the remaining tooth structure and the presence of adequate ferrule and mainly supragingival margins, and adhesive protocols regarding material surface treatment and adhesive luting under rubber dam isolation are respected, this type of prosthesis can achieve similar survival rates as those of conventional prostheses. The final functional and aesthetic result, patient satisfaction, and the 5-year follow-up render restorations such as endocrowns, which draw their retention from adhesive luting, a viable alternative to conventional approaches.
Author Contributions
Conceptualization, D.P. and T.-K.S.; methodology, A.T.; writing—original draft preparation, D.P. and E.P.; writing—review and editing, A.T. and T.-K.S.; supervision, E.P. and T.-K.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Informed consent for participation was not required for this retrospective study, as approved by the Institutional Review Board of National and Kapodistrian University of Athens.
Informed Consent Statement
Informed consent was obtained from the patient.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Reeh, E.S.; Messer, H.H.; Douglas, W.H. Reduction in tooth stiffness as a result of endodontic and restorative procedures. J. Endod. 1989, 15, 512–516. [Google Scholar] [CrossRef] [PubMed]
- Lander, E.; Dietschi, D. Endocrowns: A clinical report. Quintessence Int. 2008, 39, 99–106. [Google Scholar] [PubMed]
- Plotino, G.; Tocci, L.; Grande, N.M.; Testarelli, L.; Messineo, D.; Ciotti, M.; Glassman, G.; D’Ambrosio, F.; Gambarini, G. Symmetry of root and root canal morphology of maxillary and mandibular molars in a white population: A cone-beam computed tomography study in vivo. J. Endod. 2013, 39, 1545–1548. [Google Scholar] [CrossRef] [PubMed]
- Pissis, P. Fabrication of a metal-free ceramic restoration utilizing the monobloc technique. Pract. Periodontics Aesthet. Dent. 1995, 7, 83–94. [Google Scholar]
- Ferrari, M.; Vichi, A.; Grandini, S. Efficacy of different adhesive techniques on bonding to root canal walls: An SEM investigation. Dent. Mater. 2001, 17, 422–429. [Google Scholar] [CrossRef]
- Bindl, A.; Mormann, W.H. Clinical evaluation of adhesively placed Cerec endo-crowns after 2 years-preliminary results. J. Adhes. Dent. 1999, 1, 255–265. [Google Scholar]
- Mormann, W.H.; Bindl, A.; Luthy, H.; Rathke, A. Effects of preparation and luting system on all-ceramic computer-generated crowns. Int. J. Prosthodont. 1998, 11, 333–339. [Google Scholar]
- Morimoto, S.; Arakaki, Y.; Raggio, D.P.; Ozcan, M. One-piece endodontic crowns in posterior teeth: An overview of systematic reviews. J. Prosthet. Dent. 2024; ahead-of-print. [Google Scholar]
- Li, W.; Zheng, Z.; Zeng, Y.; Zhou, Z.; Xiao, P.; Zhong, X.; Yan, W. Chinese dentists’ restorative preferences and choices for endodontically treated teeth: A representative survey. BMC Oral Health 2024, 24, 1489. [Google Scholar] [CrossRef]
- Zhu, J.; Rong, Q.; Wang, X.; Gao, X. Influence of remaining tooth structure and restorative material type on stress distribution in endodontically treated maxillary premolars: A finite element analysis. J. Prosthet. Dent. 2017, 117, 646–655. [Google Scholar] [CrossRef]
- Papalexopoulos, D.; Samartzi, T.K.; Sarafianou, A. A Thorough Analysis of the Endocrown Restoration: A Literature Review. J. Contemp. Dent. Pract. 2021, 22, 422–426. [Google Scholar] [CrossRef]
- Magne, P. Immediate dentin sealing: A fundamental procedure for indirect bonded restorations. J. Esthet. Restor. Dent. 2005, 17, 144–154; discussion 55. [Google Scholar] [CrossRef] [PubMed]
- Margvelashvili-Malament, M.; Thompson, V.; Polyakov, V.; Malament, K.A. Over 14-year survival of pressed e.max lithium disilicate glass-ceramic complete and partial coverage restorations in patients with severe wear: A prospective clinical study. J. Prosthet. Dent. 2024; ahead-of-print. [Google Scholar]
- Samartzi, T.K.; Papalexopoulos, D.; Sarafianou, A.; Kourtis, S. Immediate Dentin Sealing: A Literature Review. Clin. Cosmet. Investig. Dent. 2021, 13, 233–256. [Google Scholar] [CrossRef] [PubMed]
- Turkyilmaz, I.; Wilkins, G.N.; Varvara, G. Tooth preparation, digital design and milling process considerations for CAD/CAM crowns: Understanding the transition from analog to digital workflow. J. Dent. Sci. 2021, 16, 1312–1314. [Google Scholar] [CrossRef]
- Noronha Filho, J.D.; Delforge, G.E.; Xing, Y.; da Cruz Silva Trugilho Duarte, M.; Medeiros, I.S.; Rabello, T.B.; Poskus, L.T.; da Silva, E.M. The Impact of Different Surface Treatments on Topography and Bond Strength of Resin Cement to Lithium Disilicate Glass Ceramic. Oper. Dent. 2023, 48, 186–195. [Google Scholar] [CrossRef]
- Stegall, D.; Tantbirojn, D.; Perdigao, J.; Versluis, A. Does Tack Curing Luting Cements Affect the Final Cure? J. Adhes. Dent. 2017, 19, 239–243. [Google Scholar]
- Gauthier, M.A.; Stangel, I.; Ellis, T.H.; Zhu, X.X. Oxygen inhibition in dental resins. J. Dent. Res. 2005, 84, 725–729. [Google Scholar] [CrossRef]
- Gianordoli-Neto, R.; Padovani, G.C.; Mondelli, J.; de Lima Navarro, M.F.; Mendonca, J.S.; Santiago, S.L. Two-year clinical evaluation of resin composite in posterior teeth: A randomized controlled study. J. Conserv. Dent. 2016, 19, 306–310. [Google Scholar]
- Rocca, G.T.; Saratti, C.M.; Poncet, A.; Feilzer, A.J.; Krejci, I. The influence of FRCs reinforcement on marginal adaptation of CAD/CAM composite resin endocrowns after simulated fatigue loading. Odontology 2016, 104, 220–232. [Google Scholar] [CrossRef]
- Fages, M.; Bennasar, B. The endocrown: A different type of all-ceramic reconstruction for molars. J. Can. Dent. Assoc. 2013, 79, d140. [Google Scholar]
- Govare, N.; Contrepois, M. Endocrowns: A systematic review. J. Prosthet. Dent. 2020, 123, 411–418.e9. [Google Scholar] [CrossRef]
- Sedrez-Porto, J.A.; Rosa, W.L.; da Silva, A.F.; Munchow, E.A.; Pereira-Cenci, T. Endocrown restorations: A systematic review and meta-analysis. J. Dent. 2016, 52, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Belleflamme, M.M.; Geerts, S.O.; Louwette, M.M.; Grenade, C.F.; Vanheusden, A.J.; Mainjot, A.K. No post-no core approach to restore severely damaged posterior teeth: An up to 10-year retrospective study of documented endocrown cases. J. Dent. 2017, 63, 1–7. [Google Scholar] [CrossRef] [PubMed]
- El-Damanhoury, H.M.; Haj-Ali, R.N.; Platt, J.A. Fracture resistance and microleakage of endocrowns utilizing three CAD-CAM blocks. Oper. Dent. 2015, 40, 201–210. [Google Scholar] [CrossRef] [PubMed]
- Aktas, G.; Yerlikaya, H.; Akca, K. Mechanical Failure of Endocrowns Manufactured with Different Ceramic Materials: An In Vitro Biomechanical Study. J. Prosthodont. 2018, 27, 340–346. [Google Scholar] [CrossRef]
- Cekic, I.; Ergun, G.; Uctasli, S.; Lassila, L.V. In vitro evaluation of push-out bond strength of direct ceramic inlays to tooth surface with fiber-reinforced composite at the interface. J. Prosthet. Dent. 2007, 97, 271–278. [Google Scholar] [CrossRef]
- Chotiwutthiphatthana, D.; Angwaravong, O.; Angwarawong, T. Effect of different indirect composite onlay and core materials on fracture resistance of endodontically treated maxillary premolars. J. Prosthodont. Res. 2023, 67, 376–383. [Google Scholar] [CrossRef]
- ElAziz, R.H.; Mohammed, M.M.; Gomaa, H.A. Clinical Performance of Short-fiber-reinforced Resin Composite Restorations vs Resin Composite Onlay Restorations in Complex Cavities of Molars (Randomized Clinical Trial). J. Contemp. Dent. Pract. 2020, 21, 296–303. [Google Scholar] [CrossRef]
- Garoushi, S.; Gargoum, A.; Vallittu, P.K.; Lassila, L. Short fiber-reinforced composite restorations: A review of the current literature. J. Investig. Clin. Dent. 2018, 9, e12330. [Google Scholar] [CrossRef]
- Hitz, T.; Ozcan, M.; Gohring, T.N. Marginal adaptation and fracture resistance of root-canal treated mandibular molars with intracoronal restorations: Effect of thermocycling and mechanical loading. J. Adhes. Dent. 2010, 12, 279–286. [Google Scholar]
- Bijelic-Donova, J.; Myyrylainen, T.; Karsila, V.; Vallittu, P.K.; Tanner, J. Direct Short-Fiber Reinforced Composite Resin Restorations and Glass-Ceramic Endocrowns in Endodontically Treated Molars: A 4 -Year Clinical Study. Eur. J. Prosthodont. Restor. Dent. 2022, 30, 284–295. [Google Scholar]
- Bindl, A.; Richter, B.; Mormann, W.H. Survival of ceramic computer-aided design/manufacturing crowns bonded to preparations with reduced macroretention geometry. Int. J. Prosthodont. 2005, 18, 219–224. [Google Scholar] [CrossRef] [PubMed]
- Porto, T.S.; Medeiros da Silva, I.G.; de Freitas Vallerini, B.; de Goes, M.F. Different surface treatment strategies on etchable CAD-CAM materials: Part 1-Effect on the surface morphology. J. Prosthet. Dent. 2023, 130, 761–769. [Google Scholar] [CrossRef] [PubMed]
- Goldfein, J.; Speirs, C.; Finkelman, M.; Amato, R. Rubber dam use during post placement influences the success of root canal-treated teeth. J. Endod. 2013, 39, 1481–1484. [Google Scholar] [CrossRef] [PubMed]
- Falacho, R.I.; Melo, E.A.; Marques, J.A.; Ramos, J.C.; Guerra, F.; Blatz, M.B. Clinical in-situ evaluation of the effect of rubber dam isolation on bond strength to enamel. J. Esthet. Restor. Dent. 2023, 35, 48–55. [Google Scholar] [CrossRef]
- Ammann, P.; Kolb, A.; Lussi, A.; Seemann, R. Influence of rubber dam on objective and subjective parameters of stress during dental treatment of children and adolescents—A randomized controlled clinical pilot study. Int. J. Paediatr. Dent. 2013, 23, 110–115. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).