The Laparoscopic Cholecystectomy and Common Bile Duct Exploration: A Single-Step Treatment of Pediatric Cholelithiasis and Choledocholithiasis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Outcomes of the Study
2.3. Study Design
2.4. Diagnostic Procedure and Indications for Surgery
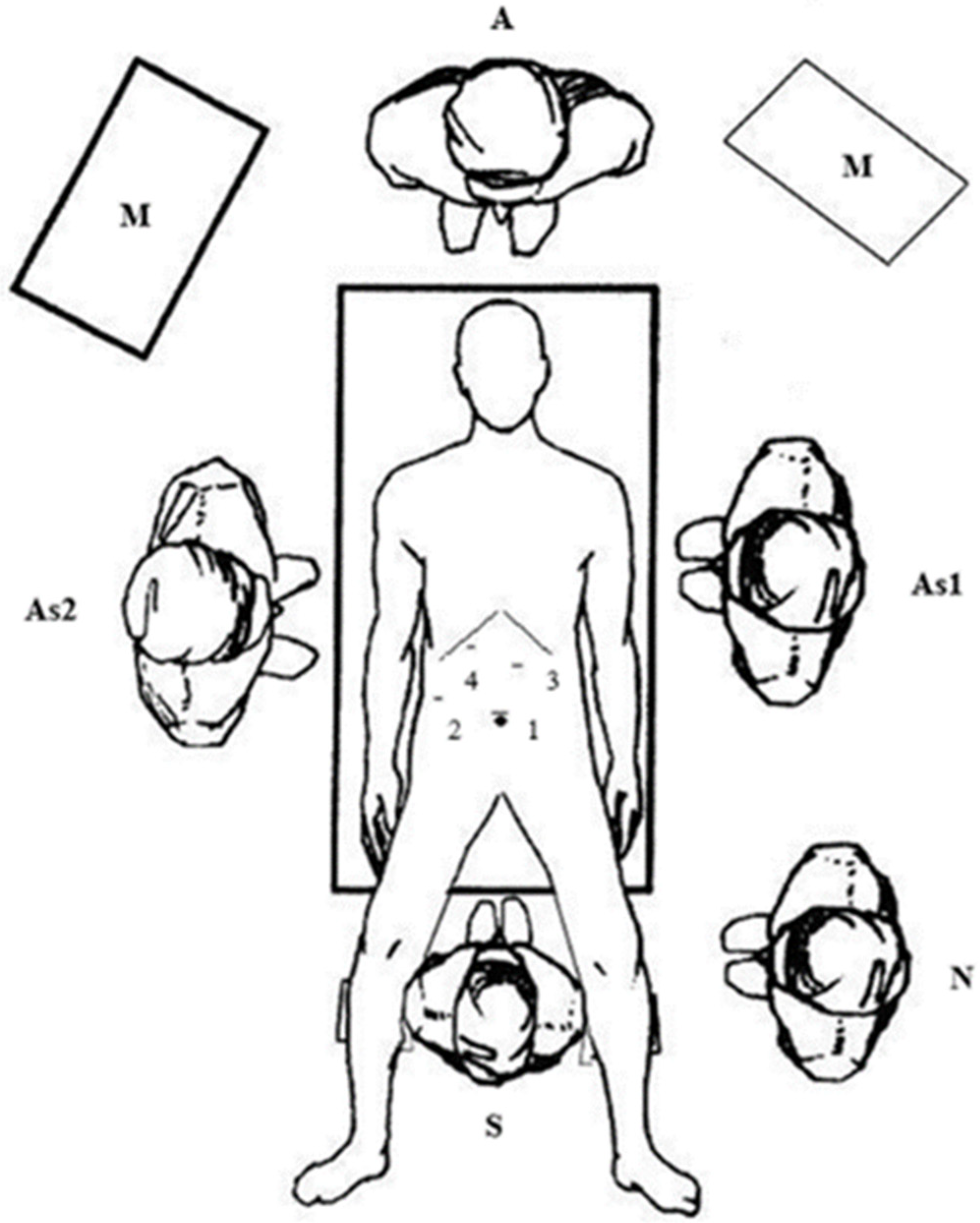
2.5. Surgical Technique (LCBDE)
2.6. Follow-Up
2.7. Statistical Analysis
3. Results
4. Discussion
Limitations of Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Murphy, P.; Vogt, K.; Winick-Ng, J.; McClure, J.; Welk, B.; Jones, S. The increasing incidence of gallbladder disease in children: A 20 year perspective. J. Pediatr. Surg. 2016, 51, 748–752. [Google Scholar] [CrossRef] [PubMed]
- Poddar, U. Gallstone disease in children. Indian Pediatr. 2010, 47, 945–953. [Google Scholar] [CrossRef] [PubMed]
- Walker, S.K.; Maki, A.C.; Cannon, R.M.; Foley, D.S.; Wilson, K.M.; Galganski, L.A.; Wiesenauer, C.A.; Bond, S.J. Etiology and incidence of pediatric gallbladder disease. Surgery 2013, 154, 927–933. [Google Scholar] [CrossRef] [PubMed]
- Rothstein, D.; Harmon, C. Gallbladder disease in children. Semin. Pediatr. Surg. 2016, 25, 225–231. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Aralica, M.; Jukić, M.; Žitko, V.; Despot, R.; Jurić, I. Gallbladder disease in children: A 20-year single-center experience. Indian Pediatr. 2019, 56, 384–386. [Google Scholar] [CrossRef]
- Wong, M.C.Y.; Incerti, F.; Avanzini, S.; Palo, F.; Sertorio, F.; Damasio, M.B.; Arrigo, S.; Gandullia, P.; Mattioli, G. Cholelithiasis management in a third-level pediatric center: Case series and literature review. Updates Surg. 2022, 74, 963–968. [Google Scholar] [CrossRef]
- Agrawal, V.; Tiwari, A.; Sharma, D.; Agrawal, R. Etiology-based decision-making protocol for pediatric cholelithiasis. Indian Pediatr. 2021, 58, 729–732. [Google Scholar] [CrossRef]
- Guo, T.; Wang, L.; Xie, P.; Zhang, Z.; Huang, X.; Yu, Y. Surgical methods of treatment for cholecystolithiasis combined with choledocholithiasis: Six years’ experience of a single institution. Surg. Endosc. 2022, 36, 4903–4911. [Google Scholar] [CrossRef]
- Cianci, P.; Restini, E. Management of cholelithiasis with choledocholithiasis: Endoscopic and surgical approaches. World J. Gastroenterol. 2021, 27, 4536–4554. [Google Scholar] [CrossRef]
- Mohseni, S.; Bass, G.A.; Forssten, M.P.; Casas, I.M.; Martin, M.; Davis, K.A.; Haut, E.R.; Sugrue, M.; Kurihara, H.; Sarani, B.; et al. Common bile duct stones management: A network meta-analysis. J. Trauma Acute Care Surg. 2022. [Google Scholar] [CrossRef]
- Samara, O.; Azzam, M.I.; Alshrouf, M.A.; Khanfar, A.N.; Mohialdeen, R.R.; Barham, O.F.; Barham, M.F.; AlRyalat, S.A. Diagnostic accuracy of ultrasonography compared with magnetic resonance cholangiopancreatography in the detection of choledocholithiasis. J. Clin. Ultrasound 2022, 50, 247–253. [Google Scholar] [CrossRef]
- Agostini, Â.F.P.; Hochhegger, B.; Forte, G.C.; Susin, L.A.; Difini, J.P.M. Accuracy of abbreviated protocol of magnetic resonance cholangio-pancreatography in the diagnosis of choledocholithiasis. Arq. Gastroenterol. 2022, 59, 188–192. [Google Scholar] [CrossRef]
- Lau, B.J.; Sydorak, R.M.; Shaul, D.B. Laparoscopic techniques for safe and successful removal of common bile duct stones in pediatric patients. J. Laparoendosc. Adv. Surg. Technol. A 2014, 24, 362–365. [Google Scholar] [CrossRef]
- Cohen, R.Z.; Tian, H.; Sauer, C.G.; Willingham, F.F.; Santore, M.T.; Mei, Y.; Freeman, A.J. Creation of a Pediatric Choledocholithiasis Prediction Model. J. Pediatr. Gastroenterol. Nutr. 2021, 73, 636–641. [Google Scholar] [CrossRef]
- Menon, S.; Patel, B.; Saekang, E.; Thomas, G.; Soundappan, S.; Shun, A. Laparoscopic exploration of the common bile duct to relieve choledocholithiasis in children. Pediatr. Surg. Int. 2011, 27, 537–540. [Google Scholar] [CrossRef]
- Kumar, R.; Nguyen, K.; Shun, A. Gallstones and common bile duct calculi in infancy and childhood. Aust. N. Z. J. Surg. 2000, 70, 188–191. [Google Scholar] [CrossRef]
- Frybova, B.; Drabek, J.; Lochmannova, J.; Douda, L.; Hlava, S.; Zemkova, D.; Mixa, V.; Kyncl, M.; Zeman, L.; Rygl, M.; et al. Cholelithiasis and choledocholithiasis in children; risk factors for development. PLoS ONE 2018, 13, e0196475. [Google Scholar] [CrossRef] [Green Version]
- Bogue, C.; Murphy, A.; Gerstle, J.; Moineddin, R.; Daneman, A. Risk factors, complications, and outcomes of gallstones in children: A single-center review. J. Pediatr. Gastroenterol. Nutr. 2010, 50, 303–308. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.; Shin, S.; Hwang, J.; Lee, J. Outcomes of laparoscopic common bile duct exploration (LCBDE) after failed endoscopic retrograde cholangiopancreatography versus primary LCBDE for managing cholecystocholedocholithiasis. J. Int. Med. Res. 2020, 48, 300060520957560. [Google Scholar] [CrossRef]
- Wang, C.C.; Tsai, M.C.; Wang, Y.T.; Yang, T.W.; Chen, H.Y.; Sung, W.W.; Huang, S.M.; Tseng, M.H.; Lin, C.C. Role of cholecystectomy in choledocholithiasis patients underwent endoscopic retrograde cholangiopancreatography. Sci. Rep. 2019, 9, 2168. [Google Scholar] [CrossRef]
- Giefer, M.J.; Kozarek, R.A. Technical outcomes and complications of pediatric ERCP. Surg. Endosc. 2015, 29, 3543–3550. [Google Scholar] [CrossRef]
- Enestvedt, B.K.; Tofani, C.; Lee, D.Y.; Abraham, M.; Shah, P.; Chandrasekhara, V.; Ginsberg, G.G.; Long, W.; Ahmad, N.; Jaffe, D.L.; et al. Endoscopic retrograde cholangiopancreatography in the pediatric population is safe and efficacious. J. Pediatr. Gastroenterol. Nutr. 2013, 57, 649–654. [Google Scholar] [CrossRef]
- Gad, E.H.; Zakaria, H.; Kamel, Y.; Alsebaey, A.; Zakareya, T.; Abbasy, M.; Mohamed, A.; Nada, A.; Abdelsamee, M.A.; Housseni, M. Surgical (Open and laparoscopic) management of large difficult CBD stones after different sessions of endoscopic failure: A retrospective cohort study. Ann. Med. Surg. 2019, 43, 52–63. [Google Scholar] [CrossRef]
- Perko, Z.; Bilan, K.; Pogorelić, Z.; Srsen, D.; Druzijanić, N.; Kraljević, D.; Juricić, J.; Mimica, Z.; Jurisić, T.; Bekavac-Beslin, M. A novel algorithm for the minimal invasive treatment of choledocholithiasis. Hepatogastroenterology 2007, 54, 1009–1012. [Google Scholar] [PubMed]
- Bansal, V.K.; Misra, M.C.; Rajan, K.; Kilambi, R.; Kumar, S.; Krishna, A.; Kumar, A.; Pandav, C.S.; Subramaniam, R.; Arora, M.K.; et al. Single-stage laparoscopic common bile duct exploration and cholecystectomy versus two-stage endoscopic stone extraction followed by laparoscopic cholecystectomy for patients with concomitant gallbladder stones and common bile duct stones: A randomized controlled trial. Surg. Endosc. 2014, 28, 875–885. [Google Scholar]
- Short, S.S.; Frykman, P.K.; Nguyen, N.; Liu, Q.; Berel, D.; Wang, K.S. Laparoscopic common bile duct exploration in children is associated with decreased cost and length of stay: Results of a two-center analysis. J. Pediatr. Surg. 2013, 48, 215–220. [Google Scholar] [CrossRef]
- Lee, H.M.; Min, S.K.; Lee, H.K. Long-term results of laparoscopic common bile duct exploration by choledochotomy for choledocholithiasis: 15-year experience from a single center. Ann. Surg. Treat. Res. 2014, 86, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Capparelli, M.A.; DAlessandro, P.D.; Questa, H.A.; Ayarzabal, V.H.; Bailez, M.M.; Barrenechea, M.E. Development of a risk score for choledocholithiasis in pediatric patients. Pediatr. Surg. Int. 2021, 37, 1393–1399. [Google Scholar] [CrossRef]
- St. Peter, S.D.; Keckler, S.J.; Nair, A.; Andrews, W.S.; Sharp, R.J.; Snyder, C.L.; Ostlie, D.J.; Holcomb, G.W. Laparoscopic cholecystectomy in the pediatric population. J. Laparoendosc. Adv. Surg. Technol. A 2008, 18, 127–130. [Google Scholar] [CrossRef]
- Cabrera Chamorro, C.C.; Pabón Arteaga, J.S.; Caicedo Paredes, C.A.; Cabrera Bravo, N.; Villamil Giraldo, C.E.; Chávez Betancourt, G.; Zarama Márquez, R.A.; Rincón Torres, C.A. Cholelithiasis and associated complications in pediatric patients. Cir. Pediatr. 2020, 33, 172–176. [Google Scholar]


| Variable | 2000–2022 |
|---|---|
| Number of cholecystectomies | 84 |
| Demographic data | |
| age; years (median, IQR) | 11.4 (8, 14) |
| female; n (%) | 66 (78.5%) |
| male; n (%) | 18 (21.5%) |
| Anthropometric data | |
| body height; cm (median, IQR) | 147.5 (138.8, 154.9) |
| body mass; kg (median, IQR) | 55.9 (50.3, 63.8) |
| BMI; cm/m2 (median, IQR) | 26.7 (22.4, 29.6) |
| Main indication for surgery | |
| biliary colic; n (%) | 14 (16.7%) |
| hereditary spherocytosis; n (%) | 15 (17.9%) |
| acute pancreatitis; n (%) | 16 (19%) |
| acute cholecystitis; n (%) | 19 (22.6%) |
| obstructive jaundice; n (%) | 20 (23.8%) |
| Complications; n (%) | |
| CBD injury | 1 (1.3%) |
| Variable | LC + ERCP (2000–2007) | LCBDE (2007–2022) | p |
|---|---|---|---|
| Number of procedures—LCBDE; n (%) | 6 (30) | 14 (70) | <0.001 |
| Demographic data Gender—female; n (%) Age; years (median, IQR) BMI; cm/m2 (median, IQR) | 5 (83.5) 14 (11.5, 145) 27.9 (23.5, 29.5) | 12 (85.7) 13.5 (11, 14.5) 27.4 (23, 29.6) | 0.891 0.651 0.722 |
| Clinical presentation; n (%) | |||
| obstructive jaundice colic type pain acute pancreatitis obstruction of papilla Laboratory values (median, IQR) Bilirubin, μmol/L ALP, U/L AST, U/L ALT, U/L GGT, U/L | 6 (100) 6 (100) 2 (60) 2 (40) 129 (91, 204) 1174 (1051, 1387) 133 (112, 159) 196 (173, 211) 186 (169, 201) | 14 (100) 13 (92.9) 7 (50) 5 (41.6) 132 (89, 206) 1105 (1004, 1354) 134 (114, 158) 188 (169, 206) 186 (171, 200) | 1.0 0.874 0.642 0.918 0.874 0.541 0.698 0.884 |
| Stone characteristics Diameter; mm (median, IQR) Number of stones (median, IQR) Diameter of CBD; mm (median, IQR) Surgical approach; n (%) LCBDE—Dormia basket extraction LCBDE—Laser fragmentation | 8 (6.5, 11) 1 (1, 2) 9 (8, 11) - - | 7.5 (6, 11) 1 (1, 3) 9 (7.5, 11) 10 (78.5) 4 (21.5) | 0.478 0.908 0.854 |
| Complications; n (%) | 2 (40) | 0 (0) | 0.078 |
| Operative time; min (median, IQR) LOS; days (median, IQR) | 85 (74, 105) 4 (3, 5) | 79 (68, 98) 2 (2, 4) | 0.125 0.011 |
| Variable | n (%) |
|---|---|
| Type of gallstone | |
| pigment | 6 (42.9) |
| cholesterol | 7 (50) |
| mixed | 1 (7.1) |
| Histopathology report | |
| normal | 1 (7.1) |
| acute cholecystitis | 2 (14.3) |
| chronic cholecystitis | 11 (78.6) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pogorelić, Z.; Lovrić, M.; Jukić, M.; Perko, Z. The Laparoscopic Cholecystectomy and Common Bile Duct Exploration: A Single-Step Treatment of Pediatric Cholelithiasis and Choledocholithiasis. Children 2022, 9, 1583. https://doi.org/10.3390/children9101583
Pogorelić Z, Lovrić M, Jukić M, Perko Z. The Laparoscopic Cholecystectomy and Common Bile Duct Exploration: A Single-Step Treatment of Pediatric Cholelithiasis and Choledocholithiasis. Children. 2022; 9(10):1583. https://doi.org/10.3390/children9101583
Chicago/Turabian StylePogorelić, Zenon, Marko Lovrić, Miro Jukić, and Zdravko Perko. 2022. "The Laparoscopic Cholecystectomy and Common Bile Duct Exploration: A Single-Step Treatment of Pediatric Cholelithiasis and Choledocholithiasis" Children 9, no. 10: 1583. https://doi.org/10.3390/children9101583
APA StylePogorelić, Z., Lovrić, M., Jukić, M., & Perko, Z. (2022). The Laparoscopic Cholecystectomy and Common Bile Duct Exploration: A Single-Step Treatment of Pediatric Cholelithiasis and Choledocholithiasis. Children, 9(10), 1583. https://doi.org/10.3390/children9101583








