Abstract
Background: Identifying sex-related differences/variables associated with 30 day/1 year mortality in patients with chronic limb-threatening ischemia (CLTI). Methods: Multicenter/retrospective/observational study. A database was sent to all the Italian vascular surgeries to collect all the patients operated on for CLTI in 2019. Acute lower-limb ischemia and neuropathic-diabetic foot are not included. Follow-up: One year. Data on demographics/comorbidities, treatments/outcomes, and 30 day/1 year mortality were investigated. Results: Information on 2399 cases (69.8% men) from 36/143 (25.2%) centers. Median (IQR) age: 73 (66–80) and 79 (71–85) years for men/women, respectively (p < 0.0001). Women were more likely to be over 75 (63.2% vs. 40.1%, p = 0.0001). More men smokers (73.7% vs. 42.2%, p < 0.0001), are on hemodialysis (10.1% vs. 6.7%, p = 0.006), affected by diabetes (61.9% vs. 52.8%, p < 0.0001), dyslipidemia (69.3% vs. 61.3%, p < 0.0001), hypertension (91.8% vs. 88.5%, p = 0.011), coronaropathy (43.9% vs. 29.4%, p < 0.0001), bronchopneumopathy (37.1% vs. 25.6%, p < 0.0001), underwent more open/hybrid surgeries (37.9% vs. 28.8%, p < 0.0001), and minor amputations (22% vs. 13.7%, p < 0.0001). More women underwent endovascular revascularizations (61.6% vs. 55.2%, p = 0.004), major amputations (9.6% vs. 6.9%, p = 0.024), and obtained limb-salvage if with limited gangrene (50.8% vs. 44.9%, p = 0.017). Age > 75 (HR = 3.63, p = 0.003) is associated with 30 day mortality. Age > 75 (HR = 2.14, p < 0.0001), nephropathy (HR = 1.54, p < 0.0001), coronaropathy (HR = 1.26, p = 0.036), and infection/necrosis of the foot (dry, HR = 1.42, p = 0.040; wet, HR = 2.04, p < 0.0001) are associated with 1 year mortality. No sex-linked difference in mortality statistics. Conclusion: Women exhibit fewer comorbidities but are struck by CLTI when over 75, a factor associated with short- and mid-term mortality, explaining why mortality does not statistically differ between the sexes.
1. Introduction
Chronic limb-threatening ischemia (CLTI) affects 1–10% of patients with peripheral arterial disease (PAD), represents its advanced stages, and is characterized by rest pain or tissue necrosis in the foot. It generally results from involvement of at least two arterial segments (aorto-iliac, femoropopliteal, and tibiopedal) or severe tibiopedal disease. The latter is particularly involved in patients with diabetes mellitus, end-stage renal disease, or the very elderly. It represents a very broad range of severe malperfusion of the lower limb and the associated limb threat. The general and limb prognosis of these patients is adverse: they are at continuous risk of a major cardiovascular event, sudden death, and, of course, amputation [1].
The survival of female and male patients who underwent treatment for CLTI has been investigated with discordant results. For instance, some studies from Germany and the USA showed that 30 day mortality was significantly higher in females, while others from Japan and Sweden, respectively, identified female sex as a significant positive predictor of 2 year survival or reported that male sex was significantly associated with an increased risk of death [2,3,4,5,6,7,8,9,10,11].
Understanding the pathophysiological differences between the sexes is important to improving the quality of care. In this setting, it is reported that a lower rate of diagnostic angiograms and interventional procedures are performed in women compared with men [12]. This has raised the concern that the therapeutic approach to cardiovascular diseases should be sex-specific because of the existence of sex-related disparities in cardiovascular physiology [13,14]. Sex differences have been identified as additional determinants in diagnostic definitions and referral requirements for some diseases and sex-specific treatments are set including percutaneous coronary intervention, coronary artery bypass graft surgery, and PAD [15]. In particular, factors such as older age, late presentation, delayed diagnosis, smaller-size vessels, and other sex-related biases have been postulated to account, at least in part, for the portended less-favorable outcome in women with PAD. In addition, most studies on PAD have had low enrollment rates for women. Fortunately, the sex disparity in the management of PAD has been recognized, and more effort and resources have been dedicated to studying this issue. Men and women have distinct and significant biological differences. Physiologically, women differ from men in many respects (e.g., they have smaller blood vessels; their menopausal state and eventual estrogen replacement therapy can affect their cardiovascular risk; etc.) [16,17,18]. It is possible that these differences may contribute to the different presentations of the disease between the sexes and the postoperative complications of major vascular procedures.
Related to the increased awareness of sex differences, the objective of the present study is to evaluate sex-related differences in the immediate post-surgery outcome and 1 year mortality in patients affected by CLTI. Secondary endpoints consist of the identification of any demographic, risk factor for atherosclerosis, comorbidity, or treatment significantly associated with operative and 1 year mortality.
2. Materials and Methods
CLIMATE (Chronic Limb-threatening Ischemia Mortality At short-medium Term and Sex) is a multicenter and retrospective observational study.
The same ad hoc electronic questionnaire was sent by email to all 143 Italian Divisions of Vascular Surgery, which consist of 20 (14% academic) and 123 (86% non-academic) centers. The questionnaire asked to anonymously collect data regarding all the patients treated in each center from 1 January to 31 December 2019 for the first episode of CLTI on the target limb (by endovascular, surgical, hybrid revascularization, regenerative cellular therapy, or major amputation). Patients with acute lower limb ischemia or exclusively neuropathic diabetic foot (non-ischemic, i.e., with triphasic wave distal arterial blood-flow at duplex scan) were not an object of this study and were not considered in the database. Follow-up was limited to the first year after the operative treatment.
Data on demographics, risk factors for atherosclerosis, comorbidities, clinical presentation, treatment, technical and clinical success, postoperative medical therapy, limb salvage, 30 day and 1 year mortality, and cause of death were collected from clinical charts, operator reports, discharge letters, institutions’ archives, and reported on the electronic database by each division of vascular surgery. The result from each variable in the database was classified as reported in Table 1 (for instance, 0 = no, 1 = yes), that is, ready for statistical analysis. Each center provided two surgeons for this study: one deputed to data collection and the other the chief of the division, who was responsible for the accuracy and integrity of the data. All the 35 databases were checked for congruency and summarized together in the original database from the first author (E.M.). Further supervision of all the data collected from all the centers was performed by the co-first author (M.Z.) and by the statistician co-authors #3, 4, and 7 (G.S., L.S., and M.P.). Data supporting the findings of this study are available from the corresponding author upon reasonable request. Weekly web meetings were held between the authors and the study group while drafting the protocol and over the following two months of patient recruitment, to standardize data collection.
Here are some definitions we adopted; the remaining are reported in the tables. Hyperlipemia: low-density lipoprotein ≥ 70 mg/dL, total cholesterol > 135 mg/dL, or triglyceride > 150 mg/dL. Arterial hypertension is defined as having a systolic and/or diastolic blood pressure of ≥140 mmHg and ≥90 mmHg, respectively. Coronary artery disease (CAD): stable or unstable angina, ejection fraction < 30%, history of myocardial infarction or congestive heart failure. Chronic obstructive pulmonary disease (COPD): symptomatic, but sometimes with only radiological signs. Cerebrovascular disease (CVD): previous TIA or stroke. Minor amputation: toe or trans-metatarsal amputation. Limb salvage (LS): any treatment for CLTI that is successful in avoiding a major amputation. Use of antiplatelets, anticoagulants, and statins was classified as monotherapy, two medications, or three or more medications.
Institutional review board approval and patient-informed consent were waived. The current Italian legislation on observational studies (our study falls under this category) does not request the above-mentioned documents when clinical data are anonymized (Official Gazette of the Italian Republic #76, 31 March 2008).
Statistical Analysis
Sample characteristics were collected in an ad hoc dataset (Supplementary file dataset S1).
Qualitative variables were summarized with absolute and relative (percentage) frequencies; quantitative ones with medians and interquartile ranges (IQR). Pearson’s or Fisher’s exact tests were used to evaluate differences in qualitative variables between males and females, whereas the Mann–Whitney test was performed to compare quantitative variables.
Survival analysis at 30 days and at 1 year was performed by Cox proportional hazard regression. Candidate variables for multivariate analysis were chosen if they were statistically significant at univariate analysis or clinically relevant.
The Kaplan–Meier curve and log-rank tests were performed to describe survival according to gender.
A p-value of less than 0.05 was considered statistically significant. The STATA13 statistical software was used for all statistical computations.
3. Results
Thirty-six (25.2%) of the 143 divisions of vascular surgery from 17 of the 20 Italian regions replied to the invitation and joined the study. The proportion between the typology of the adhering centers, compared to the typology of the Italian Divisions of Vascular Surgery, was found to be constant: five (14.3%) academic vs. thirty-five (85.6%) non-academic. Information on 2399 cases was collected. All the data requested from the database was obtained from each vascular surgery center, and at follow-up, no patient was lost at 30 days, while 20 (0.8%) were missing at 1 year.
Table 1 shows the sample characteristics stratified by sex.

Table 1.
Sample characteristics.
Table 1.
Sample characteristics.
| Variables | Total Cohort (n = 2399) | Men (n = 1677) | Women (n = 722) | p-Value | |
|---|---|---|---|---|---|
| Median (IQR) age, yrs | 75 (67–81) | 73 (66-80) | 79 (71–85) | <0.0001 | |
| Age > 75 yrs | 1128 (47.0) | 672 (40.1) | 456 (63.2) | 0.0001 | |
| Tobacco use: | 1538 (64.2) | 1234 (73.7) | 304 (42.2) | <0.0001 | |
| never | 857 (35.8) | 441 (26.3) | 416 (57.8) | <0.0001 | |
| former (stop > 10 yrs) | 840 (35.1) | 693 (41.4) | 147 (20.4) | <0.0001 | |
| smoker | 698 (29.1) | 541 (32.3) | 157 (21.8) | <0.0001 | |
| Overt diabetes mellitus (yes vs. no): | 1418 (59.2) | 1038 (61.9) | 380 (52.8) | <0.0001 | |
| no | 978 (40.8) | 638 (38.1) | 340 (47.2) | <0.0001 | |
| non-insulin dependent | 717 (29.9) | 529 (31.6) | 188 (26.1) | 0.007 | |
| insulin dependent | 701 (29.3) | 509 (30.4) | 192 (26.7) | 0.068 | |
| Hyperlipemia: | 1601(66.9) | 1160 (69.3) | 441 (61.3) | <0.0001 | |
| no | 794 (33.1) | 515 (30.8) | 279 (38.6) | 0.001 | |
| under therapy | 1498 (62.6) | 1089 (65.0) | 409 (56.8) | 0.0001 | |
| no therapy | 103 (4.3) | 71 (4.2) | 32 (4.4) | 0.825 | |
| Arterial hypertension: | 2176 (90.8) | 1538 (91.8) | 638 (88.5) | 0.011 | |
| no | 221 (9.2) | 138 (8.2) | 83 (11.5) | 0.011 | |
| under therapy | 2147 (89.6) | 1515 (90.4) | 632 (87.7) | 0.047 | |
| no therapy | 29 (1.2) | 23 (1.4) | 6 (0.8) | 0.245 | |
| Chronic renal insufficiency: | 626 (26.1) | 453 (27.0) | 173 (24.0) | 0.123 | |
| no | 1769 (73.9) | 1222 (73.0) | 547 (76.0) | 0.125 | |
| creatinine > 2 mg/dL | 408 (17.0) | 283 (16.9) | 125 (17.4) | 0.765 | |
| hemodialysis treatment | 218 (9.1) | 170 (10.1) | 48 (6.7) | 0.006 | |
| Coronary artery disease: | 947 (39.6) | 736 (43.9) | 211 (29.4) | <0.0001 | |
| no | 1447 (60.4) | 939 (56.0) | 508 (70.7) | <0.0001 | |
| revascularized | 705 (29.5) | 559 (33.4) | 146 (20.3) | <0.0001 | |
| non-revascularized | 242 (10.1) | 177 (10.6) | 65 (9.0) | 0.246 | |
| Chronic obstructive pulmonary disease: | 806 (33.7) | 622 (37.1) | 184 (25.6) | <0.0001 | |
| no | 1589 (66.3) | 1054 (62.9) | 535 (74.4) | <0.0001 | |
| only radiological signs | 479 (20.0) | 363 (21.7) | 116 (16.1) | 0.002 | |
| symptomatic | 327 (13.7) | 259 (15.4) | 68 (9.5) | 0.0001 | |
| Cerebrovascular disease: | 186 (7.8) | 128 (7.6) | 58 (8.0) | 0.736 | |
| no | 2213 (92.2) | 1549 (92.4) | 664 (92.0) | 0.918 | |
| previous TIA | 139 (5.8) | 95 (5.7) | 44 (6.1) | ||
| previous stroke | 47 (2.0) | 33 (2.0) | 14 (1.9) | ||
| Rutherford category: | 4 (rest pain) | 964 (40.2) | 697 (41.6) | 267 (37.0) | 0.107 |
| 5 (minor tissue loss) | 1078 (44.9) | 738 (44.0) | 340 (47.1) | ||
| 6 (major tissue loss) | 357 (14.9) | 242 (14.4) | 115 (15.9) | ||
| Necrosis/infection of the foot: | no | 1194 (49.9) | 854 (51.0) | 340 (47.4) | 0.202 |
| dry | 603 (25.2) | 407 (24.3) | 196 (27.3) | ||
| wet | 596 (24.9) | 414 (24.7) | 182 (25.4) | ||
| First intervention: | endovascular only (rarely, regenerative cellular therapy) | 1366 (57.1) | 922 (55.2) | 444(61.6) | 0.004 |
| any open revascularization surgery | 840 (35.2) | 632 (37.9) | 208 (28.8) | <0.0001 | |
| any major amputation | 184 (7.7) | 115 (6.9) | 69 (9.6) | 0.024 | |
| Any intervention below the knee | 1287 (53.9) | 912 (54.6) | 375 (52.3) | 0.313 | |
| Technical success of CLTI revascularization: | no | 211 (9.5) | 152 (9.7) | 59 (9.0) | 0.611 |
| yes | 2004 (90.5) | 1410 (90.3) | 594 (91.0) | ||
| Associated minor amputation | 467 (19.5) | 368 (22.0) | 99 (13.7) | <0.0001 | |
| Postoperative antiplatelets, anticoagulants, statins: | monotherapy | 561 (24.3) | 373 (23.1) | 188 (26.9) | 0.105 |
| two medications | 1229 (53.2) | 863 (53.6) | 366 (52.4) | ||
| three or more medications | 519 (22.5) | 375 (23.3) | 144 (20.6) | ||
| Clinical success of CLTI revascularization: | worsen | 157 (7.1) | 109 (7.0) | 48 (7.4) | 0.951 |
| no change | 343 (15.5) | 142 (15.5) | 101 (15.5) | ||
| improved | 1716 (77.4) | 1212 (77.5) | 504 (77.2) | ||
| Limb salvage: | 1965 (82.1) | 1382 (82.6) | 583 (80.9) | 0.307 | |
| in Rutherford category 4 | 882 (44.9) | 638 (46.2) | 244 (41.9) | 0.080 | |
| in Rutherford category 5 | 917 (46.7) | 621 (44.9) | 296 (50.8) | 0.017 | |
| in Rutherford category 6 | 166 (8.5) | 123 (8.9) | 43 (7.4) | 0.275 | |
| 30 day mortality | 74 (3.1) | 44 (2.6) | 30 (4.2) | 0.047 | |
| 1 year mortality | 317 (13.5) | 211 (12.8) | 106 (14.9) | 0.167 | |
| Cause of death: | cardiac | 141 (42.1) | 91 (41.2) | 50 (43.9) | 0.635 |
| neurologic | 19 (5.7) | 10 (4.5) | 9 (7.9) | 0.202 | |
| pulmonary | 33 (9.9) | 31 (14.0) | 3 (2.6) | 0.001 | |
| cancer | 19 (5.7) | 13 (5.9) | 6 (5.3) | 0.822 | |
| multi-organ failure | 46 (13.7) | 25 (11.3) | 21 (12.4) | 0.074 | |
| other | 77 (23.0) | 51 (23.1) | 25 (21.9) | 0.804 | |
Quantitative variables are expressed with a median and interquartile range (IQR), and qualitative ones as absolute and relative (percentage) frequencies, n (%). TIA, or transient ischemic attack. CLTI, chronic limb-threatening ischemia.
Among 2399 patients, 1677 (69.9%) were males; the median (IQR) age in the sample was 75 (67–81) years old, with a significant difference between men and women [73 (66–80) years vs. 79 (71–85) years, p < 0.0001, respectively]. Women were older than 75 compared to men (63.2% vs. 40.1%, p = 0.0001). The age 75 cutoff (≤75 or >75) was chosen on the basis of the median value.
The most common cardiovascular risk factor and comorbidity in the total cohort are, respectively, arterial hypertension and CAD, followed by hyperlipemia, tobacco use, diabetes mellitus, COPD, chronic renal insufficiency, and CVD.
A significantly greater proportion of men who were smokers and affected by diabetes, dyslipidemia, end-stage renal disease on hemodialysis treatment, arterial hypertension, CAD and COPD underwent significantly more open or hybrid surgeries for CLTI revascularization, and amputations of the toes or the forefoot as a complementary treatment for LS. On the contrary, a significantly greater proportion of women underwent less-invasive direct or indirect revascularizations for CLTI, mainly endovascular (cellular therapy was used in only 18, 2.5% of women, and 27, 1.6% of men) and major amputations.
CVD, the clinical presentation according to Rutherford’s classification, infection/necrosis of the foot, above the knee vs. below the knee revascularization, technical and clinical success of revascularization for CLTI, postoperative medical therapy, 1 year mortality, cardiac, neurologic, malignant, and multi-organ failure causes of death do not statistically differ between the sexes, as well as 30 day mortality, which, despite being close to being so, is not statistically significant (p = 0.047, which is approximately p = 0.05). Instead, significantly more women with limited tissue loss (Rutherford category 5) obtain LS, and significantly more males die from pulmonary causes.
Table 2 reports the Cox regression analysis to assess the relationship between demographic, epidemiological, and clinical characteristics, and 30 day mortality.

Table 2.
Cox regression analysis to assess risk factors for 30 day mortality.
Results from multivariate analysis show that age > 75 years was the only variable associated with the 30 day mortality rate (HR = 3.69, 95%CI: 1.53–8.62; p = 0.003).
Table 3 shows the results of a Cox regression analysis to assess the relationship between demographic, epidemiological, clinical characteristics, and 1 year mortality.

Table 3.
Cox regression analysis to assess risk factors for 1 year mortality.
Results from multivariate analysis show that the following factors were found to be associated with 1 year mortality: age > 75 years (HR = 2.14, 95%CI: 1.60–2.87; p < 0.0001); therapy for hyperlipemia (HR = 0.69, 95%CI: 0.51–0.93; p = 0.015); chronic renal insufficiency (CRI) (HR = 1.54, 95%CI: 1.28–1.84; p < 0.0001); CAD (HR = 1.26, 95%CI: 1.02–1.57; p = 0.036); dry necrosis (HR = 1.42, 95%CI: 1.02–1.98; p = 0.040); and wet necrosis (HR = 2.04, 95%CI: 1.46–2.85; p < 0.0001) of the foot.
Figure 1 and Figure 2 show the Kaplan–Meier survival curves (overall distribution and for men/women) at 30 days and 1 year, respectively. Again, no statistically significant difference is noted between the sexes.
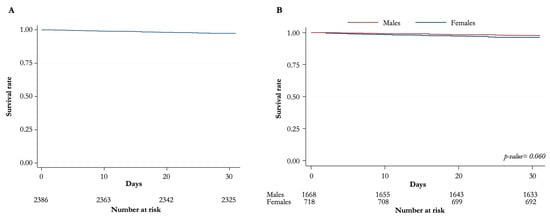
Figure 1.
Kaplan–Meier curves for overall survival at 30 days. (A) Distribution of overall survival (B) Overall survival for males and females.
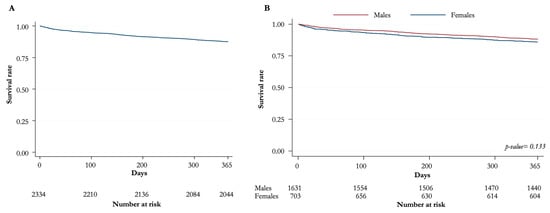
Figure 2.
Kaplan–Meier curves for overall survival at 1 year. (A) Distribution of overall survival (B) Overall survival for males and females.
4. Discussion
The aim of the study was to evaluate the differences between men and women in 30 days and 1 year mortality. Our findings showed that no differences were observed between the sexes.
The overall 30 day mortality rate in this study of 2399 CLTI patients is 3.1%. One-year mortality is 13.5%, which is much lower than the 23.1–28.7% reported in the COPART French registry on 411 patients treated for CLTI [19]. Differences in risk factors and comorbidities between the French and Italian populations may explain the difference in 1 year mortality between these two studies.
Notwithstanding that our male patients were significantly more smokers, affected by diabetes, end-stage renal disease on hemodialysis treatment, arterial hypertension, CAD, and COPD, and revascularized for CLTI by open surgery, they were also significantly younger, more on statin therapy, and more revascularized for CAD, potentially inducing more protection from cardiovascular risk.
Additionally, the male patients in the Medicare population affected by CLTI and analyzed from 2015 to 2017 received significantly more statin therapy compared to females [4].
The current clinical practice guidelines from the European Society for Vascular Surgery strongly recommend the use of moderate or high-intensity statin therapy to reduce all-cause and cardiovascular mortality in patients with CLTI [20].
Cardiologists from the University of Minnesota found that patients with unprotected left main coronary artery disease benefit from preoperative coronary artery revascularization before vascular surgery [21].
Our findings that some vascular beds are more affected than others when comparing men and women (i.e., the coronary district vs. the peripheral arterial district) and that some risk factors are so disparate between the groups suggest a potentially different phenotypic expression of the disease process. However, it is important to notice that this result might merely be a function of which men and women were selected for the treatment.
Anesthesiologists from Melbourne, Toronto, and Auckland have recently evaluated the effects of randomized interventions by sex in large international perioperative trials and concluded that women were healthier than men, but outcomes were similar. These authors encouraged further research to understand the reason for this discrepancy [22].
Colleagues from Auckland and Hamilton analyzed 1773 patients with CLTI in the midland region of New Zealand over a 12 year period. They found a worse long-term survival rate for women with CLTI, despite 30 day mortality not differing depending on sex [23].
A recent German study from the cardiologists at the University of Muenster on almost 200,000 unselected patients treated for CLTI over an 8 year period showed that 30 day mortality is significantly higher in women [3]. The same results were obtained from the US National Inpatient Sample database [7,10].
Other French colleagues from the University of Strasbourg demonstrated a significantly lower survival rate at 6 years, but not at 30 days, among women compared to men undergoing infra-inguinal open surgery for CLTI. They concluded that female sex was an independent factor predicting death [24].
A possible explanation for this worse long-term survival in women treated for CLTI is that they are associated with more severe disease at presentation (although in our study Rutherford categories were similar in both sexes), develop arteriosclerotic changes later in life, and require treatment at an older age [16].
On the contrary, a recent multicenter study from Japan has identified female sex as a significant positive predictor of 2 year overall survival in patients treated for CLTI [11].
Another Swedish population-based study conducted between 2008 and 2013 on over 10,000 patients who underwent revascularization for CLTI and were followed up for a median of 2.7 years reported that male sex was significantly associated with an increased risk of amputation or death at multivariate analysis [6].
This dichotomy could open a reflection on the genetic, environmental, and dietary factors implied on the outcome of CLTI patients. The Atherosclerosis Risk in Communities (ARIC) study has already focused attention on the association of race (“Blacks vs. Whites” in the ARIC study) with incident CLTI-related hospitalizations that leads to differences in clinical disease risk and presentation [25].
We have found advanced age over 75 years old to be a negative prognostic factor, both for 30 day and 1 year mortality. A Dutch study recently reported a similar result for 1 year mortality in advanced age, as did a Yale School of Medicine study [26,27].
The older population is increasing, and this knowledge of worse CLTI outcomes for the elderly population is important for clinical decision making.
Our female patients treated for CLTI are significantly older compared to males, and this is in contrast with the exception of the Italian data (females are 0.9 years younger than males) reported in the VASCUNET and International Consortium of Vascular Registries [28].
Our analysis demonstrates that females are struck by CLTI at an age >75 years, a pivotal factor associated with short- and mid-term mortality. This fact may explain why the mortality rate does not significantly differ between the sexes, although females have fewer risk factors and comorbidities associated with this condition.
Our study confirms other independent predictive factors for mortality at 1 year, namely CRI, CAD, and tissue loss.
CLTI is a terminal manifestation of systemic atherosclerosis. Therefore, it is often accompanied by clinically significant CAD, resulting in high mortality. The goal of treating patients with CLTI is not only to save a functional limb but also to improve cardiovascular outcomes. While some risk factors (age and sex) are immutable, others are (cigarette smoking, dyslipidemia, diabetes mellitus, a sedentary lifestyle, and treatable hypertension). In the absence of an efficient cardiovascular work-up and aggressive treatment of risk factors and associated comorbidities, the prognosis of CLTI is generally poor [29,30,31].
End-stage renal disease and tissue loss are established critical factors for mid-term mortality in patients undergoing revascularization for CLTI [32,33,34,35].
Interestingly, in our study, although significantly more women underwent major amputations, LS was achieved significantly more often in women with minor tissue loss. Perhaps the reason is that CLTI treatment differs between sexes, with women receiving significantly more minimally invasive therapies and men receiving significantly more open surgery.
Additionally, the US National Inpatient Sample database shows that women are more likely to undergo endovascular surgery for CLTI than men, and this is associated with a higher incidence of major amputation [10,36]. Therefore, in our series, it seems that endovascular treatment has been more successful than open or hybrid treatment in terms of LS in women with CLTI in the Rutherford category of 5.
In parallel, men had significantly undergone more open or hybrid surgeries for CLTI revascularization together with minor amputations and significantly achieved less LS in Rutherford category 5. It seems that in men, minor amputation as a complementary act of open or hybrid revascularization for CLTI does not give benefits in terms of LS.
Our study has limitations. Firstly, data were retrospectively collected, and some key clinical information might be missing or might not be recorded appropriately in the clinical records. The selection criteria for offering CLTI interventions are based on real-world data and are not systematic. For instance, we could not collect data on hormonal replacement/supplementation therapy for the two groups. Furthermore, we did not collect data on the extent of CLTI (for instance, below-the-knee vs. multi-level disease). Finally, the role played by unknown confounders can be relevant in an observational design. In order to mitigate potential documentation errors, patients’ data was collected from multiple hospital records, and several web meetings and phone calls were performed between the first author and the other authors during the writing of the study protocol and the patient’s recruitment period to standardize data collection.
Secondly, the timing of patient recruitment does not coincide with the actual appearance of the disease. This may cause an artificial extension, as the atherosclerosis and symptomology may have developed earlier. Thirdly, we evaluated only one year of patients treated for CLTI; as such, inter-annual variability cannot be excluded.
Finally, the staging of CLTI has not been performed using the current WIfI (Wound, Ischemia, and foot Infection) classification system. We have preferred to adopt the standard Rutherford classification, together with the presence/absence of necrosis/infection of the foot, and to exclude patients with only neuropathic (non-ischemic) diabetic foot, to make data collection easier and more realistic for the participating centers, which are mostly non-academic [37]. For the same reason, the current international suggested standards for reports dealing with risk factors and comorbidities have been adjusted or synthetized (for instance, asymptomatic carotid stenosis has not been included in CVD since in the real world not all patients treated for CLTI undergo a carotid duplex scan) [38].
5. Conclusions
Our observational evaluation of patients operated on for CLTI demonstrates that women are less represented and have fewer risk factors and comorbidities compared to men. However, women are struck by CLTI at an age > 75 years, a pivotal factor associated with short- and mid-term mortality, explaining why the mortality rate does not differ between the two sexes. Additionally, CRI, CAD, and tissue loss are independent negative prognostic factors for 1 year survival.
Endovascular techniques for limited tissue loss are more likely to be successful in women.
Statin therapy is an independent positive prognostic factor for 1 year survival; once again, its aggressive use in CLTI patients appears justified.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jpm13020316/s1, File S1: dataset.
Author Contributions
Conceptualization, resources, supervision, project administration, E.M., M.Z., G.S., L.S., M.F. (Massimo Federici), G.M.S., M.V.P., A.R.M., T.M., P.F., C.R., P.R., L.C., E.G., F.M.F., G.V., F.R., E.F., P.V., D.M., M.F. (Mauro Ferrari), P.M., U.M.B., M.M. (Mario Monaco), G.N., G.M.C., M.M. (Massimiliano Martelli), D.R., G.C., G.L., B.D.B., M.T., P.C., S.T., A.C. (Adolfo Crinisio), G.B. (Giuseppe Battaglia), S.D.V., V.S.T., R.C. (Ruggiero Curci), G.D., D.F., G.F.V., A.I. and A.M.S.; methodology, validation, investigation, data curation, visualization, E.M., M.Z., G.S., L.S., M.F. (Massimo Federici), G.M.S., M.V.P., A.R.M., T.M., M.P.B., I.F., F.P., A.A. (Andrea Angelini), L.C.D.P., A.P. (Armando Palmieri), G.M., A.B. (Antonio Bozzani), C.C., M.M. (Mafalda Massara), E.P., T.P., N.T., M.M. (Maurizio Maiorano), M.P. (Marco Panagrosso), G.G. (Giovanni Giordano), A.B. (Antonella Biello), A.A. (Alessio Amico), M.D.B., R.M., F.B., A.C. (Antonio Cardini), M.D.L., P.S., A.E., S.R., A.P. (Andrea Padricelli), G.G. (Giorgio Giudice), G.D.N., R.T., R.C. (Rita Compagna), I.D., S.G., G.B. (Giusi Basile), L.M., F.M.O. and A.M.S. Software, E.M., G.S., L.S., M.V.P. and A.M.S.; formal analysis, writing—original draft preparation, E.M., M.Z., G.S., L.S., M.F. (Massimo Federici), G.M.S., M.V.P., A.R.M., T.M. and A.M.S.; writing—review and editing, E.M., M.Z., G.S., L.S., M.F. (Massimo Federici), G.M.S., M.V.P., A.R.M., T.M., P.F., M.P.B., C.R., I.F., P.R., F.P., L.C., A.A. (Andrea Angelini), E.G., L.C.D.P., F.M.F., A.P. (Armando Palmieri), G.V., G.M., F.R., A.B. (Antonio Bozzani), E.F., C.C., P.V., M.M. (Mafalda Massara), D.M., E.P., T.P., M.F. (Mauro Ferrari), N.T., P.M., M.M. (Maurizio Maiorano), U.M.B., M.P. (Marco Panagrosso), M.M. (Mario Monaco), G.G. (Giovanni Giordano), G.N., A.B. (Antonella Biello), G.M.C., A.A. (Alessio Amico), M.D.B., M.M. (Massimiliano Martelli), R.M., D.R., G.C., F.B., G.L., A.C. (Antonio Cardini), B.D.B., M.D.L., M.T., P.S., P.C., A.E., S.T., S.R., A.P. (Andrea Padricelli), G.G. (Giorgio Giudice), A.C. (Adolfo Crinisio), G.D.N., G.B. (Giuseppe Battaglia), R.T., S.D.V., R.C. (Rita Compagna), V.S.T., I.D., R.C. (Ruggiero Curci), S.G., G.D., G.B. (Giusi Basile), D.F., G.F.V., L.M., A.I., F.M.O. and A.M.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived. Being an observational study, according to Italian law, a mandatory approval is not needed.
Informed Consent Statement
Patient consent was waived due to the retrospective and aggregate nature of the study analysis.
Data Availability Statement
Raw data were obtained from 25% of the Italian Divisions of Vascular Surgery and are readily available for presentation to the referees and the editors of the journal, if requested.
Acknowledgments
The authors gratefully acknowledge Edoardo Guarino, Meng, MSc for the English revision of this manuscript, and IMED s.r.l. for its unconditioned support in the open access of this paper.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Conte, M.S. Lower Extremity Arterial Occlusive Disease Epidemiology and Natural History. In Rutherford’s Vascular Surgery and Endovascular Therapy, 9th ed.; Sidawy, A.P., Perler, B.A., Eds.; Elsevier-OHCE: Philadelphia, PA, USA, 2018; Volume 2, pp. 1368–1376. [Google Scholar]
- Wu, B.; Lancaster, E.M.; Ramirez, J.L.; Zarkowsky, D.S.; Reyzelman, A.M.; Gasper, W.J.; Conte, M.S.; Hiramoto, J.S. Increased Reintervention after Infrainguinal Revascularization for Chronic Limb-Threatening Ischemia in Women. Ann. Vasc. Surg. 2020, 69, 307–316. [Google Scholar] [CrossRef] [PubMed]
- Makowski, L.; Köppe, J.; Engelbertz, C.; Kühnemund, L.; Fischer, A.J.; A Lange, S.; Dröge, P.; Ruhnke, T.; Günster, C.; Malyar, N.; et al. Sex-related differences in treatment and outcome of chronic limb-threatening ischaemia: A real-world cohort. Eur. Heart J. 2022, 43, 1759–1770. [Google Scholar] [CrossRef]
- Mentias, A.; Vaughan-Sarrazin, M.; Saad, M.; Girotra, S. Sex Differences in Management and Outcomes of Critical Limb Ischemia in the Medicare Population. Circ. Cardiovasc. Interv. 2020, 13, e009459. [Google Scholar] [CrossRef] [PubMed]
- Anantha-Narayanan, M.; Doshi, R.P.; Patel, K.; Sheikh, A.B.; Llanos-Chea, F.; Abbott, J.D.; Shishehbor, M.H.; Guzman, R.J.; Hiatt, W.R.; Duval, S.; et al. Contemporary Trends in Hospital Admissions and Outcomes in Patients with Critical Limb Ischemia. Circ. Cardiovasc. Qual. Outcomes 2021, 14, e007539. [Google Scholar] [CrossRef] [PubMed]
- Fridh, E.B.; Andersson, M.; Thuresson, M.; Sigvant, B.; Kragsterman, B.; Johansson, S.; Hasvold, P.; Nordanstig, J.; Falkenberg, M. Editor’s Choice—Impact of Comorbidity, Medication, and Gender on Amputation Rate Following Revascularisation for Chronic Limb Threatening Ischaemia. Eur. J. Vasc. Endovasc. Surg. 2018, 56, 681–688. [Google Scholar] [CrossRef]
- Lo, R.C.; Bensley, R.P.; Dahlberg, S.E.; Matyal, R.; Hamdan, A.D.; Wyers, M.; Chaikof, E.L.; Schermerhorn, M.L. Presentation, treatment, and outcome differences between men and women undergoing revascularization or amputation for lower extremity peripheral arterial disease. J. Vasc. Surg. 2014, 59, 409–418.e3. [Google Scholar] [CrossRef]
- Pulli, R.; Dorigo, W.; Pratesi, G.; Fargion, A.; Angiletta, D.; Pratesi, C. Gender-related outcomes in the endovascular treatment of infrainguinal arterial obstructive disease. J. Vasc. Surg. 2012, 55, 105–112. [Google Scholar] [CrossRef]
- Ferranti, K.M.; Osler, T.M.; Duffy, R.P.; Stanley, A.C.; Bertges, D.J. Association between gender and outcomes of lower extremity peripheral vascular interventions. J. Vasc. Surg. 2015, 62, 990–997. [Google Scholar] [CrossRef]
- Elbadawi, A.; Barssoum, K.; Megaly, M.; Rai, D.; Elsherbeeny, A.; Mansoor, H.; Shishehbor, M.H.; Abdel-Latif, A.; Gulati, M.; Elgendy, I.Y. Sex Differences in Trends and In-Hospital Outcomes among Patients with Critical Limb Ischemia: A Nationwide Analysis. J. Am. Heart Assoc. 2021, 10, e022043. [Google Scholar] [CrossRef]
- Miyata, T.; Kumamaru, H.; Mii, S.; Kinukawa, N.; Miyata, H.; Shigematsu, K.; Azuma, N.; Ishida, A.; Izumi, Y.; Inoue, Y.; et al. Prediction Models for Two Year Overall Survival and Amputation Free Survival after Revascularisation for Chronic Limb Threatening Ischaemia. Eur. J. Vasc. Endovasc. Surg. 2022, 64, 367–376. [Google Scholar] [CrossRef]
- Maas, A.; Appelman, Y. Gender differences in coronary heart disease. Neth. Heart J. 2010, 18, 598–603. [Google Scholar] [CrossRef]
- Capodanno, D.; Angiolillo, D. Impact of race and gender on antithrombotic therapy. Thromb. Haemost. 2010, 104, 471–484. [Google Scholar] [CrossRef]
- Chandra, N.C.; Ziegelstein, R.C.; Rogers, W.J.; Tiefenbrunn, A.J.; Gore, J.M.; French, W.J.; Rubison, M. Observations of the Treatment of Women in the United States with Myocardial Infarction: A Report from the National Registry of Myocardial Infarction-I. Arch. Intern. Med. 1998, 158, 981–988. [Google Scholar] [CrossRef]
- Kim, C.; Redberg, R.F.; Pavlic, T.; Eagle, K.A. A Systematic Review of Gender Differences in Mortality after Coronary Artery Bypass Graft Surgery and Percutaneous Coronary Interventions. Clin. Cardiol. 2007, 30, 491–495. [Google Scholar] [CrossRef]
- Lee, M.H.-Y.; Li, P.Y.; Li, B.; Shakespeare, A.; Samarasinghe, Y.; Feridooni, T.; Cuen-Ojeda, C.; Alshabanah, L.; Kishibe, T.; Al-Omran, M. A systematic review and meta-analysis of sex- and gender-based differences in presentation severity and outcomes in adults undergoing major vascular surgery. J. Vasc. Surg. 2022, 76, 581–594.e25. [Google Scholar] [CrossRef]
- Pabon, M.; Cheng, S.; Altin, S.E.; Sethi, S.S.; Nelson, M.D.; Moreau, K.L.; Hamburg, N.; Hess, C.N. Sex Differences in Peripheral Artery Disease. Circ. Res. 2022, 130, 496–511. [Google Scholar] [CrossRef]
- Huxley, V.H. Sex and the cardiovascular system: The intriguing tale of how women and men regulate cardiovascular function differently. Adv. Physiol. Educ. 2007, 31, 17–22. [Google Scholar] [CrossRef]
- Cambou, J.; Aboyans, V.; Constans, J.; Lacroix, P.; Dentans, C.; Bura, A. Characteristics and Outcome of Patients Hospitalised for Lower Extremity Peripheral Artery Disease in France: The COPART Registry. Eur. J. Vasc. Endovasc. Surg. 2010, 39, 577–585. [Google Scholar] [CrossRef]
- Conte, M.S.; Bradbury, A.W.; Kolh, P.; White, J.V.; Dick, F.; Fitridge, R.; Mills, J.L.; Ricco, J.-B.; Suresh, K.R.; Murad, M.H.; et al. Global Vascular Guidelines on the Management of Chronic Limb-Threatening Ischemia. Eur. J. Vasc. Endovasc. Surg. 2019, 58, S1–S109.e33. [Google Scholar] [CrossRef]
- Garcia, S.; Moritz, T.E.; Ward, H.B.; Pierpont, G.; Goldman, S.; Larsen, G.C.; Littooy, F.; Krupski, W.; Thottapurathu, L.; Reda, D.J.; et al. Usefulness of Revascularization of Patients with Multivessel Coronary Artery Disease before Elective Vascular Surgery for Abdominal Aortic and Peripheral Occlusive Disease. Am. J. Cardiol. 2008, 102, 809–813. [Google Scholar] [CrossRef]
- Leslie, K.; Martin, C.; Myles, P.S.; Devereaux, P.; Peyton, P.J.; Story, D.A.; Wijeysundera, D.N.; Cuthbertson, B.H.; Short, T.G.; Corcoran, T.B.; et al. Inclusion, characteristics, and outcomes of male and female participants in large international perioperative studies. Br. J. Anaesth. 2022, 129, 336–345. [Google Scholar] [CrossRef] [PubMed]
- Hart, O.; Xue, N.; Davis-Havill, B.; Pottier, M.; Prakash, M.; Reimann, S.-A.; King, J.; Xu, W.; Khashram, M. The Incidence of Chronic Limb-Threatening Ischemia in the Midland Region of New Zealand over a 12-Year Period. J. Clin. Med. 2022, 11, 3303. [Google Scholar] [CrossRef] [PubMed]
- Lejay, A.; Schaeffer, M.; Georg, Y.; Lucereau, B.; Roussin, M.; Girsowicz, E.; Delay, C.; Schwein, A.; Thaveau, F.; Geny, B.; et al. Gender related Long-term Differences after Open Infrainguinal Surgery for Critical Limb Ischemia. Eur. J. Vasc. Endovasc. Surg. 2015, 50, 506–512. [Google Scholar] [CrossRef]
- Hicks, C.W.; Ding, N.; Kwak, L.; Ballew, S.H.; Kalbaugh, C.A.; Folsom, A.R.; Heiss, G.; Coresh, J.; Black, J.H.; Selvin, E.; et al. Risk of peripheral artery disease according to race and sex: The Atherosclerosis Risk in Communities (ARIC) study. Atherosclerosis 2021, 324, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Smet, N.; Fourneau, I.; Roeleveld, H.; Winter, L.B.-D.; Schraepen, C.; Favoreel, M.; van der Laan, L. Age-Dependent Outcome of First-Line Endovascular and Surgical Revascularization Strategies in Chronic Limb-Threatening Ischemia. Ann. Vasc. Surg. 2022, 85, 133–145. [Google Scholar] [CrossRef]
- Kim, T.I.; Aboian, E.; Fischer, U.; Zhang, Y.; Guzman, R.J.; Chaar, C.I.O. Lower Extremity Revascularization for Chronic Limb-Threatening Ischemia among Patients at the Extremes of Age. Ann. Vasc. Surg. 2021, 72, 517–528. [Google Scholar] [CrossRef]
- Behrendt, C.-A.; Sigvant, B.; Kuchenbecker, J.; Grima, M.J.; Schermerhorn, M.; Thomson, I.A.; Altreuther, M.; Setacci, C.; Svetlikov, A.; Laxdal, E.H.; et al. Editor’s Choice—International Variations and Sex Disparities in the Treatment of Peripheral Arterial Occlusive Disease: A Report from VASCUNET and the International Consortium of Vascular Registries. Eur. J. Vasc. Endovasc. Surg. 2020, 60, 873–880. [Google Scholar] [CrossRef]
- Armstrong, E.J.; Wu, J.; Singh, G.D.; Dawson, D.L.; Pevec, W.C.; Amsterdam, E.A.; Laird, J.R. Smoking cessation is associated with decreased mortality and improved amputation-free survival among patients with symptomatic peripheral artery disease. J. Vasc. Surg. 2014, 60, 1565–1571. [Google Scholar] [CrossRef]
- Faglia, E.; Clerici, G.; Scatena, A.; Caminiti, M.; Curci, V.; Morabito, A.; Prisco, V.; Greco, R.; Edmonds, M. Effectiveness of combined therapy with angiotensin-converting enzyme inhibitors and statins in reducing mortality in diabetic patients with critical limb ischemia: An observational study. Diabetes Res. Clin. Pr. 2014, 103, 292–297. [Google Scholar] [CrossRef]
- Aboyans, V.; Ricco, J.-B.; Bartelink, M.-L.E.L.; Björck, M.; Brodmann, M.; Cohnert, T.; Naylor, A.R.; Roffi, M.; Tendera, M.; Vlachopoulos, C.; et al. Editor’s Choice—2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS). Eur. J. Vasc. Endovasc. Surg. 2018, 55, 305–368. [Google Scholar] [CrossRef]
- Taylor, S.M.; Kalbaugh, C.A.; Blackhurst, D.W.; Cass, A.L.; Trent, E.A.; Langan, E.M.; Youkey, J.R. Determinants of functional outcome after revascularization for critical limb ischemia: An analysis of 1000 consecutive vascular interventions. J. Vasc. Surg. 2006, 44, 747–756. [Google Scholar] [CrossRef][Green Version]
- Soga, Y.; Iida, O.; Takahaera, M.; Hirano, K.; Suzuki, K.; Kawasaki, D.; Miyashita, Y.; Tsuchiya, T. Two-Year Life Expectancy in Patients With Critical Limb Ischemia. JACC: Cardiovasc. Interv. 2014, 7, 1444–1449. [Google Scholar] [CrossRef]
- Bradbury, A.W.; Adam, D.J.; Bell, J.; Forbes, J.F.; Fowkes, F.G.R.; Gillespie, I.; Ruckley, C.V.; Raab, G.M. Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL) trial: A survival prediction model to facilitate clinical decision making. J. Vasc. Surg. 2010, 51, 52S–68S. [Google Scholar] [CrossRef]
- Schanzer, A.; Hevelone, N.; Owens, C.D.; Beckman, J.A.; Belkin, M.; Conte, M.S. Statins are independently associated with reduced mortality in patients undergoing infrainguinal bypass graft surgery for critical limb ischemia. J. Vasc. Surg. 2008, 47, 774–781.e1. [Google Scholar] [CrossRef]
- McGinigle, K.L.; Browder, S.E.; Strassle, P.D.; Shalhub, S.; Harris, L.M.; Minc, S.D. Sex-related disparities in intervention rates and type of intervention in patients with aortic and peripheral arterial diseases in the National Inpatient Sample Database. J. Vasc. Surg. 2021, 73, 2081–2089.e7. [Google Scholar] [CrossRef]
- Mills, J.L. The application of the Society for Vascular Surgery Wound, Ischemia, and foot Infection (WIfI) classification to stratify amputation risk. J. Vasc. Surg. 2017, 65, 591–593. [Google Scholar] [CrossRef]
- Rutherford, R.B.; Baker, J.; Ernst, C.; Johnston, K.; Porter, J.M.; Ahn, S.; Jones, D.N. Recommended standards for reports dealing with lower extremity ischemia: Revised version. J. Vasc. Surg. 1997, 26, 517–538. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).