A 3D-Printed Modular Microreservoir for Drug Delivery
Abstract
:1. Introduction
2. Materials and Methods
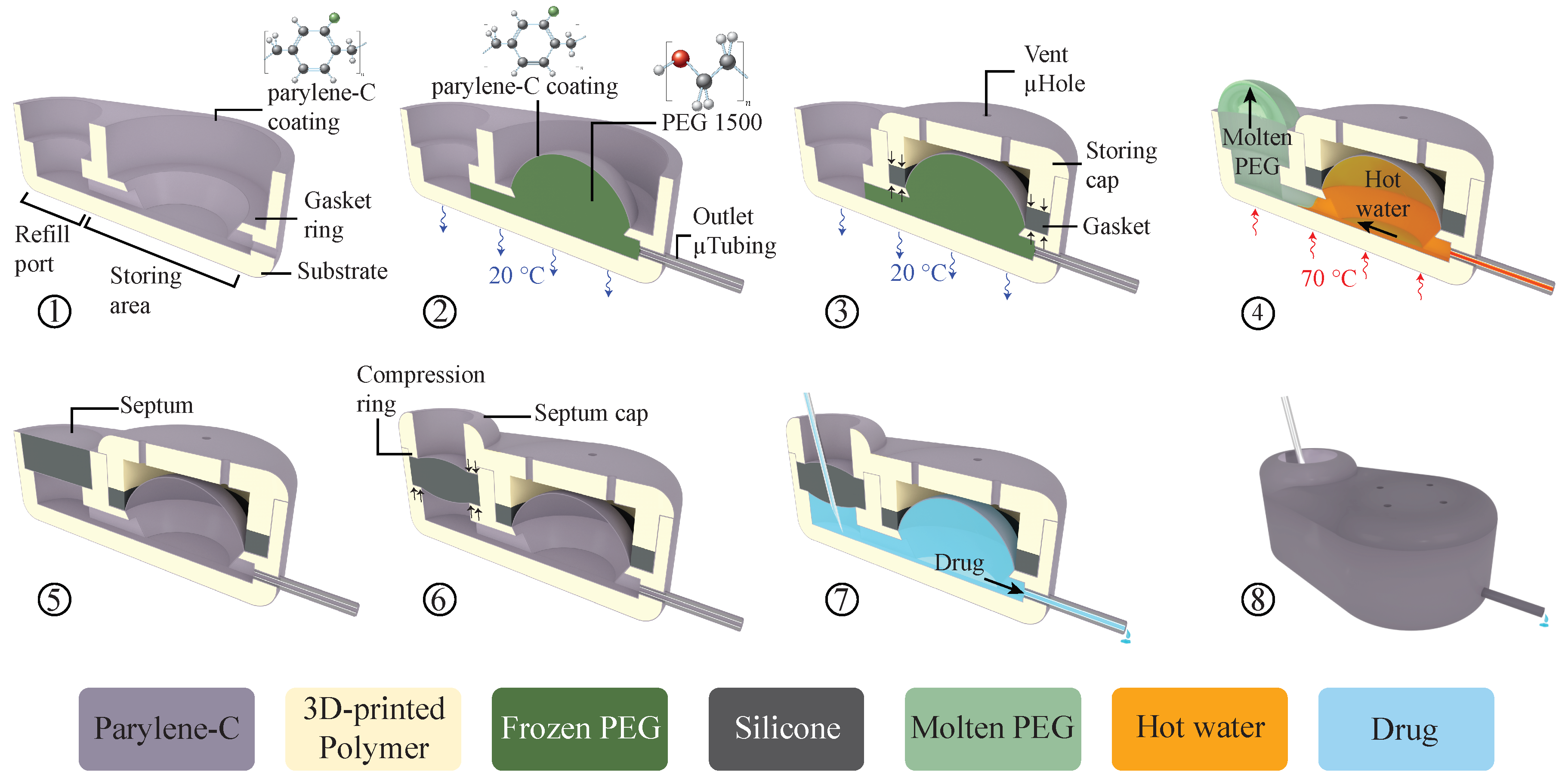
2.1. System Operation Concept and Architecture
2.2. Fabrication Process
2.3. Experimental Methods
2.3.1. Septum Test
2.3.2. Storing Membrane Test
2.3.3. In Vitro Test
3. Results
3.1. Septum Characterization
3.2. Storing Membrane Characterization
3.3. In Vitro Characterization
4. Discussion
5. Summary and Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Stevenson, C.L.; Santini, J.T.; Langer, R. Reservoir-based drug delivery systems utilizing microtechnology. Adv. Drug Deliv. Rev. 2012, 64, 1590–1602. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nagai, N.; Kaji, H.; Onami, H.; Katsukura, Y.; Ishikawa, Y.; Nezhad, Z.K.; Sampei, K.; Iwata, S.; Ito, S.; Nishizawa, M.; et al. A Platform for Controlled Dual-Drug Elivery to the Retina: Protective Effects against Light-Induced Retinal Damage in Rats. Adv. Healthc. Mater. 2014, 3, 1555–1560. [Google Scholar] [CrossRef]
- Chung, A.J.; Huh, Y.S.; Erickson, D. A Robust, Electrochemically Driven Microwell Drug Delivery System for Controlled Vasopressin Release. Biomed. Microdevices 2009, 11, 861–867. [Google Scholar] [CrossRef] [PubMed]
- Elman, N.M.; Ho Duc, H.L.; Cima, M.J. An Implantable MEMS Drug Delivery Device for Rapid Delivery in Ambulatory Emergency Care. Biomed. Microdevices 2009, 11, 625–631. [Google Scholar] [CrossRef]
- Humayun, M.; Santos, A.; Altamirano, J.C.; Ribeiro, R.; Gonzalez, R.; de la Rosa, A.; Shih, J.; Pang, C.; Jiang, F.; Calvillo, P.; et al. Implantable MicroPump for Drug Delivery in Patients with Diabetic Macular Edema. Transl. Vis. Sci. Technol. 2014, 3, 5. [Google Scholar] [CrossRef] [Green Version]
- Salt, A.; Hartsock, J.; Gill, R.; Smyth, D.; Kirk, J.; Verhoeven, K. Perilymph Pharmacokinetics of Marker Applied through a Cochlear Implant in Guinea Pigs. PLoS ONE 2017, 12, 1–20. [Google Scholar] [CrossRef]
- Sanjay, S.T.; Zhou, W.; Dou, M.; Tavakoli, H.; Ma, L.; Xu, F.; Li, X. Recent Advances of Controlled Drug Delivery Using Microfluidic Platforms. Adv. Drug Deliv. Rev. 2018, 128, 3–28. [Google Scholar] [CrossRef]
- Mousoulis, C.; Ochoa, M.; Papageorgiou, D.; Ziaie, B. A Skin-Contact-Actuated Micropump for Transdermal Drug Delivery. IEEE Trans. Biomed. Eng. 2011, 58, 1492–1498. [Google Scholar] [CrossRef]
- Cantwell, C.T.; Wei, P.; Ziaie, B.; Rao, M.P. Modular Reservoir Concept for MEMS-Based Transdermal Drug Delivery Systems. J. Micromech. Microeng. 2014, 24. [Google Scholar] [CrossRef]
- Oka, K.; Aoyagi, S.; Arai, Y.; Isono, Y.; Hashiguchi, G.; Fujita, H. Fabrication of a Micro Needle for a Trace Blood Test. Sens. Actuators A Phys. 2002, 97–98, 478–485. [Google Scholar] [CrossRef]
- Roxhed, N.; Samel, B.; Nordquist, L.; Griss, P.; Stemme, G. Painless Drug Delivery through Microneedle-Based Transdermal Patches Featuring Active Infusion. IEEE Trans. Biomed. Eng. 2008, 55, 1063–1071. [Google Scholar] [CrossRef] [PubMed]
- Stoeber, B.; Liepmann, D. Design, Fabrication and Testing of a MEMS Syringe. In Proceedings of the Solid-State Sensor and Actuator Workshop, Hilton Head, SC, USA, 2–6 June 2002; pp. 2–7. [Google Scholar]
- Kochhar, J.S.; Lim, W.X.S.; Zou, S.; Foo, W.Y.; Pan, J.; Kang, L. Microneedle Integrated Transdermal Patch for Fast Onset and Sustained Delivery of Lidocaine. Mol. Pharm. 2013, 10, 4272–4280. [Google Scholar] [CrossRef]
- Li, T.; Evans, A.T.; Chiravuri, S.; Gianchandani, R.Y.; Gianchandani, Y.B. Compact, Power-Efficient Architectures Using Microvalves and Microsensors, for Intrathecal, Insulin, and Other Drug Delivery Systems. Adv. Drug Deliv. Rev. 2012, 64, 1639–1649. [Google Scholar] [CrossRef]
- Reynaerts, D.; Peirs, J.; Van Brussel, H. A SMA-Actuated Implantable System for Delivery of Liquid Drugs. In Proceedings of the 5th International Conference on New Actuators, Bremen, Germany, 26–28 June 1996. [Google Scholar]
- Lee, M.W.; An, S.; Yoon, S.S.; Yarin, A.L. Advances in Self-Healing Materials Based on Vascular Networks with Mechanical Self-Repair Characteristics. Adv. Colloid Interface Sci. 2018, 252, 21–37. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, R.F.; Stokes, A.A.; Nunes, R.M.D.; Whitesides, G.M. Soft Machines That Are Resistant to Puncture and That Self Seal. Adv. Mater. 2013, 25, 6709–6713. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Armani, D.; Liu, C.; Aluru, N. Re-Configurable Fluid Circuits by PDMS Elastomer Micromachining. In Proceedings of the Technical Digest. IEEE International MEMS 99 Conference. Twelfth IEEE International Conference on Micro Electro Mechanical Systems, Orlando, FL, USA, 21–21 January 1999; pp. 222–227. [Google Scholar] [CrossRef]
- Chaudhury, M.K.; Whitesides, G.M. Direct Measurement of Interfacial Interactions between Semispherical Lenses and Flat Sheets of Poly(dimethylsiloxane) and Their Chemical Derivatives. Langmuir 1991, 7, 1013–1025. [Google Scholar] [CrossRef]
- Andrews, J.C.; Walker-Andrews, S.C.; Ensminger, W.D. Long-Term Central Venous Access with a Peripherally Placed Subcutaneous Infusion Port: Initial Results. Radiology 1990, 176, 45–47. [Google Scholar] [CrossRef]
- Strum, S.B.; Mcdermed, J.; Korn, A.; Joseph, C. Improved Methods for Venous Access: The Port-A-Cath, a Totally Implanted Catheter System. J. Clin. Oncol. 1986, 4, 596–603. [Google Scholar] [CrossRef]
- iPRECIO®. Available online: http://www.iprecio.com (accessed on 8 March 2020).
- Prometra Pump | Flowonix. Available online: http://www.flowonix.com/healthcare-provider/products/prometra-pump (accessed on 8 March 2020).
- Lo, R.; Li, P.-Y.; Saati, S.; Agrawal, R.N.; Humayun, M.S.; Meng, E. A Passive MEMS Drug Delivery Pump for Treatment of Ocular Diseases. Biomed. Microdevices 2009, 11, 959–970. [Google Scholar] [CrossRef]
- Lo, R.; Li, P.-Y.; Saati, S.; Agrawal, R.; Humayun, M.S.; Meng, E. A Refillable Microfabricated Drug Delivery Device for Treatment of Ocular Diseases. Lab Chip 2008, 8, 1027. [Google Scholar] [CrossRef]
- Lo, R.; Kuwahara, K.; Li, P.Y.; Agrawal, R.; Humayun, M.S.; Meng, E. IEEE A Passive Refillable Intraocular MEMS Drug Delivery Device. Int. Conf. Microtechnol. Med. Biol. 2006, 74–77. [Google Scholar] [CrossRef] [Green Version]
- Li, P.Y.; Shih, J.; Lo, R.; Saati, S.; Agrawal, R.; Humayun, M.S.; Tai, Y.C.; Meng, E. An Electrochemical Intraocular Drug Delivery Device. Sens. Actuators A Phys. 2008, 143, 41–48. [Google Scholar] [CrossRef]
- Gensler, H.; Sheybani, R.; Li, P.Y.; Mann, R.L.; Meng, E. An Implantable MEMS Micropump System for Drug Delivery in Small Animals. Biomed. Microdevices 2012, 14, 483–496. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsu, M.; Alfadhel, A.; Forouzandeh, F.; Borkholder, D.A. Biocompatible Magnetic Nanocomposite Microcapsules as Microfluidic One-Way Diffusion Blocking Valves with Ultra-Low Opening Pressure. Mater. Des. 2018, 150, 86–93. [Google Scholar] [CrossRef]
- Evans, A.T.; Chiravuri, S.; Gianchandani, Y.B. A Multidrug Delivery System Using a Piezoelectrically Actuated Silicon Valve Manifold With Embedded Sensors. J. Microelectromech. Syst. 2011, 20, 231–238. [Google Scholar] [CrossRef]
- Trull, F.L.; Rich, B.A. More Regulation of Rodents. Science 1999, 284, 1463. [Google Scholar] [CrossRef]
- Benedikz, E.; Kloskowska, E.; Winblad, B. The Rat as an Animal Model of Alzheimer’s Disease. J. Cell. Mol. Med. 2009, 13, 1034–1042. [Google Scholar] [CrossRef] [Green Version]
- Lo, R.; Meng, E. Integrated and Reusable In-Plane Microfluidic Interconnects. Sens. Actuators B Chem. 2008, 132, 531–539. [Google Scholar] [CrossRef]
- Gensler, H.M. A Wireless Implantable MEMS Micropump System for Site-specific Anti-cancer Drug Delivery. Ph.D. Thesis, University of South California, Los Angeles, CA, USA, December 2013. [Google Scholar]
- Systems, S.C. Parylene for Medical Devices | Specialty Coating Systems. Available online: https://scscoatings.com/corporate/blog/parylene-for-medical-devices/ (accessed on 30 March 2020).
- Laser, D.J.; Santiago, J.G. A Review of Micropumps. J. Micromech. Microeng. 2004, 14, R35–R64. [Google Scholar] [CrossRef]
- Formlabs. Dental SG Biocompatible Photopolymer Resin for Form 2. Available online: https://formlabs.com/media/upload/DentalLTClear-DataSheet-EN.pdf (accessed on 29 March 2020).
- Forouzandeh, F.; Zhu, X.; Alfadhel, A.; Ding, B.; Walton, J.P.; Cormier, D.; Frisina, R.D.; Borkholder, D.A. A Nanoliter Resolution Implantable Micropump for Murine Inner Ear Drug Delivery. J. Control Release 2019, 298, 27–37. [Google Scholar] [CrossRef]
- Medical - Henkel Adhesives. Available online: https://www.henkel-adhesives.com/us/en/industries/medical.html (accessed on 7 March 2020).
- Liu, X.Y.; Nothias, J.M.; Scavone, A.; Garfinkel, M.; Millis, J.M. Biocompatibility Investigation of Polyethylene Glycol and Alginate-Poly-l-Lysine for Islet Encapsulation. ASAIO J. 2010, 56, 241–245. [Google Scholar] [CrossRef] [PubMed]
- Systems, S.C. SCS Parylene Properties. Available online: https://scscoatings.com/parylene-coatings/parylene-expertise/parylene-properties/ (accessed on 30 March 2020).
- Avantor. NuSil MED-6215 Optically Clear Low Consistency Silicone Elastomer. Available online: https://www.avantorsciences.com/assetsvc/asset/en_US/id/29019912/contents/en_us_tds_nusimed-6215.pdf (accessed on 29 June 2020).
- Hamilton Reference Guide—Syringes and Needles. Available online: www.hamiltoncompany.com (accessed on 30 March 2020).
- Kort, W.; Hekking-Weijma, J.M.; Tenkate, M.T.; Sorm, V.; VanStrik, R. A Microchip Implant System as a Method to Determine Body Temperature of Terminally Ill Rats and Mice. Lab. Anim. 1999, 32, 260–269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bierman, W. The Temperature of the Skin Surface. J. Am. Med. Assoc. 1936, 106, 1158–1162. [Google Scholar] [CrossRef]
- Berteau, C.; Filipe-Santos, O.; Wang, T.; Roja, H.E.; Granger, C.; Schwarzenbach, F. Evaluation of the Impact of Viscosity, Injection Volume, and Injection Flow Rate on Subcutaneous Injection Tolerance. Med. Devices Evid. Res. 2015, 8, 473–484. [Google Scholar] [CrossRef] [Green Version]
- Zini, E.; Padrutt, I.; Macha, K.; Riederer, A.; Pesaresi, M.; Lutz, T.A.; Reusch, C.E. Use of an Implantable Pump for Controlled Subcutaneous Insulin Delivery in Healthy Cats. Vet. J. 2017, 219, 60–64. [Google Scholar] [CrossRef]
- Rauck, R.; Deer, T.; Rosen, S.; Padda, G.; Barsa, J.; Dunbar, E.; Dwarakanath, G. Accuracy and efficacy of intrathecal administration of morphine sulfate for treatment of intractable pain using the Prometra® Programmable Pump. Neuromodulation 2010, 13, 102–107. [Google Scholar] [CrossRef]
- Sheybani, R.; Cobo, A.; Meng, E. Wireless Programmable Electrochemical Drug Delivery Micropump with Fully Integrated Electrochemical Dosing Sensors. Biomed. Microdevices 2015, 17, 74. [Google Scholar] [CrossRef]
- Species Specific Information: Mouse. Available online: http://web.jhu.edu/animalcare/procedures/mouse.html (accessed on 8 March 2020).
- Urquhart, J.; Fara, J.W.; Willis, K.L. Rate-Controlled Delivery Systems in Drug and Hormone Research. Annu. Rev. Pharmacol. Toxicol. 2002, 24, 199–236. [Google Scholar] [CrossRef]
- U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER). Guidance for Industry: Estimating the Maximum Safe Starting Dose in Initial Clinical Trials for Therapeutics in Adult Healthy Volunteers. July 2005. [Google Scholar]
- Rogers, C.I.; Qaderi, K.; Woolley, A.T.; Nordin, G.P. 3D Printed Microfluidic Devices with Integrated Valves. Biomicrofluidics 2015, 9. [Google Scholar] [CrossRef]
- Nordquist, L.; Roxhed, N.; Griss, P.; Ran Stemme, G. Novel Microneedle Patches for Active Insulin Delivery are Efficient in Maintaining Glycaemic Control: An Initial Comparison with Subcutaneous Administration. Pharm. Res. 2007, 24, 1381–1388. [Google Scholar] [CrossRef] [PubMed]
- Cobo, A.; Sheybani, R.; Tu, H.; Meng, E. A Wireless Implantable Micropump for Chronic Drug Infusion against Cancer. Sens. Actuators A Phys. 2016, 239, 18–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, D.G.; Borkholder, D.A. Towards an Implantable, Low Flow Micropump That Uses No Power in the Blocked-Flow State. Micromachines 2016, 7, 99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Forouzandeh, F. Implantable Microsystem Technologies For Nanoliter-Resolution Inner Ear Drug Delivery. Ph.D. Thesis, Rochester Institute of Technology, Rochester, NY, USA, August 2019. [Google Scholar]
- Forouzandeh, F.; Alfadhel, A.; Zhu, X.; Walton, J.P.; Cormier, D.R.; Frisina, R.D.; Borkholder, D.A. A Wirelessly Controlled Fully Implantable Microsystem for Nano-Liter Resolution Inner Ear Drug Delivery. In Proceedings of the 18th Solid-State Sensors, Actuators, and Microsystems Workshop, Hilton Head Island, SC, USA, 3–7 June 2018; pp. 38–41. [Google Scholar]
- Johnson, D.G.; Frisina, R.D.; Borkholder, D.A. In-Plane Biocompatible Microfluidic Interconnects for Implantable Microsystems. IEEE Trans. Biomed. Eng. 2011, 58, 943–948. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Häfeli, U.O.; Mokhtari, A.; Liepmann, D.; Stoeber, B. In Vivo Evaluation of a Microneedle-Based Miniature Syringe for Intradermal Drug Delivery. Biomed. Microdevices 2009, 11, 943–950. [Google Scholar] [CrossRef]
- Van Der Maaden, K.; Jiskoot, W.; Bouwstra, J. Microneedle Technologies for (Trans)Dermal Drug and Vaccine Delivery. J. Control Release 2012, 161, 645–655. [Google Scholar] [CrossRef]





© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Forouzandeh, F.; Ahamed, N.N.; Hsu, M.-C.; Walton, J.P.; Frisina, R.D.; Borkholder, D.A. A 3D-Printed Modular Microreservoir for Drug Delivery. Micromachines 2020, 11, 648. https://doi.org/10.3390/mi11070648
Forouzandeh F, Ahamed NN, Hsu M-C, Walton JP, Frisina RD, Borkholder DA. A 3D-Printed Modular Microreservoir for Drug Delivery. Micromachines. 2020; 11(7):648. https://doi.org/10.3390/mi11070648
Chicago/Turabian StyleForouzandeh, Farzad, Nuzhet N. Ahamed, Meng-Chun Hsu, Joseph P. Walton, Robert D. Frisina, and David A. Borkholder. 2020. "A 3D-Printed Modular Microreservoir for Drug Delivery" Micromachines 11, no. 7: 648. https://doi.org/10.3390/mi11070648
APA StyleForouzandeh, F., Ahamed, N. N., Hsu, M. -C., Walton, J. P., Frisina, R. D., & Borkholder, D. A. (2020). A 3D-Printed Modular Microreservoir for Drug Delivery. Micromachines, 11(7), 648. https://doi.org/10.3390/mi11070648





