Vectors for Inhaled Gene Therapy in Lung Cancer. Application for Nano Oncology and Safety of Bio Nanotechnology
Abstract
:1. Introduction
2. Search Methods
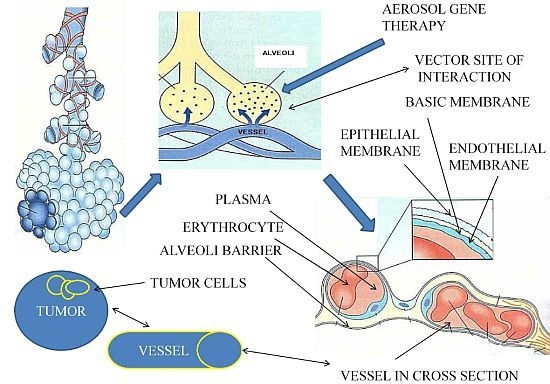
3. Lung Microenvironment
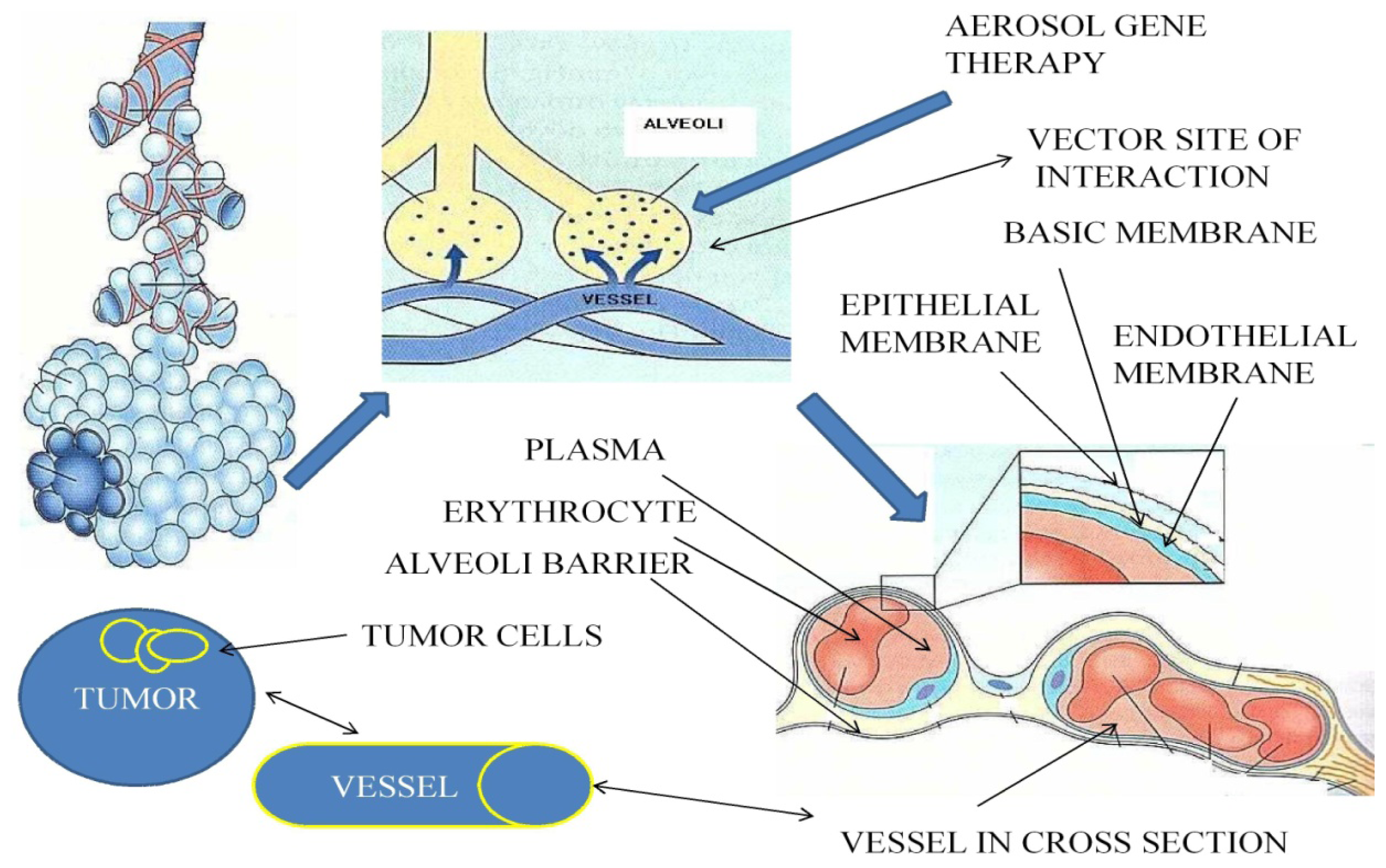
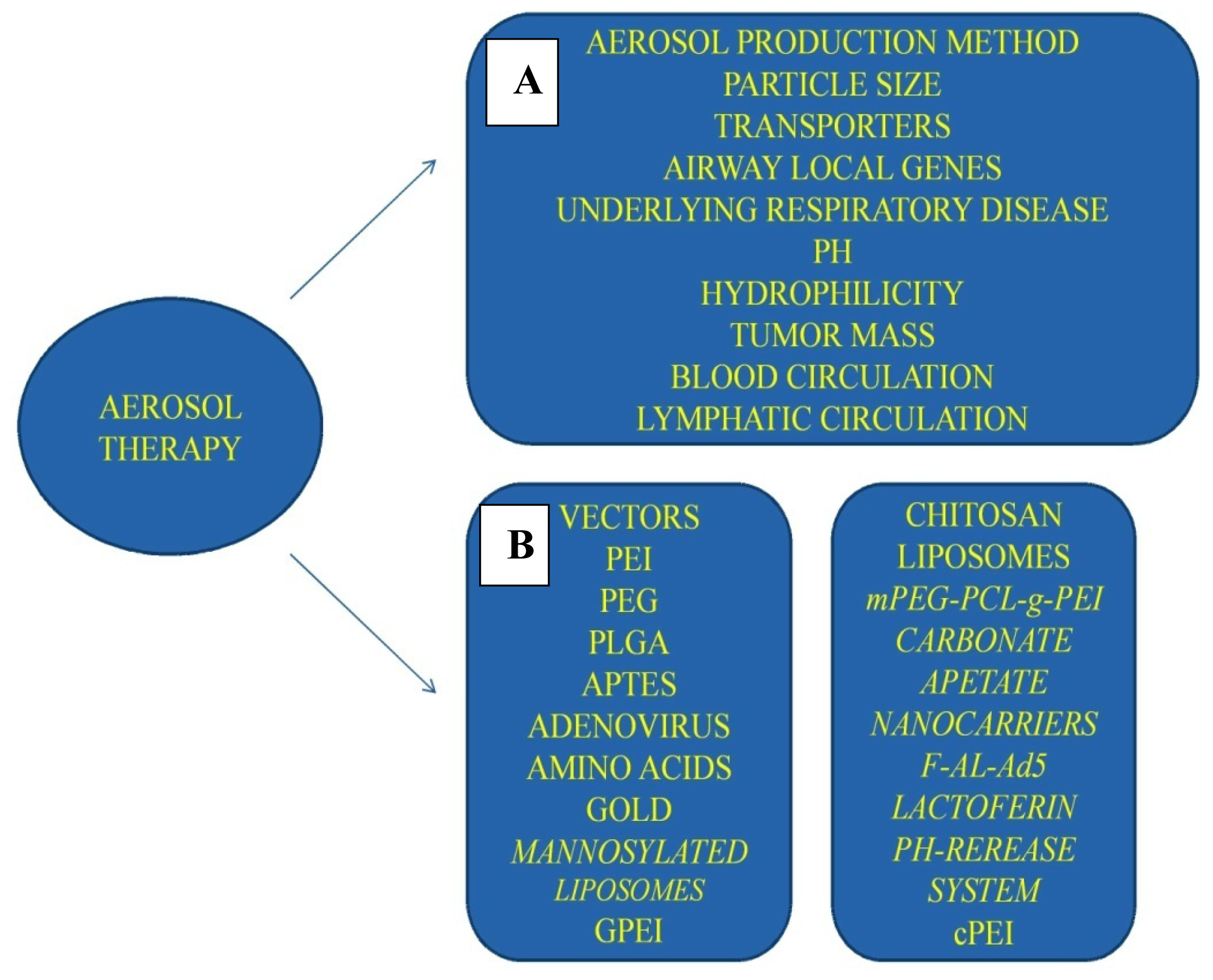
4. Aerosol Drug Formulation
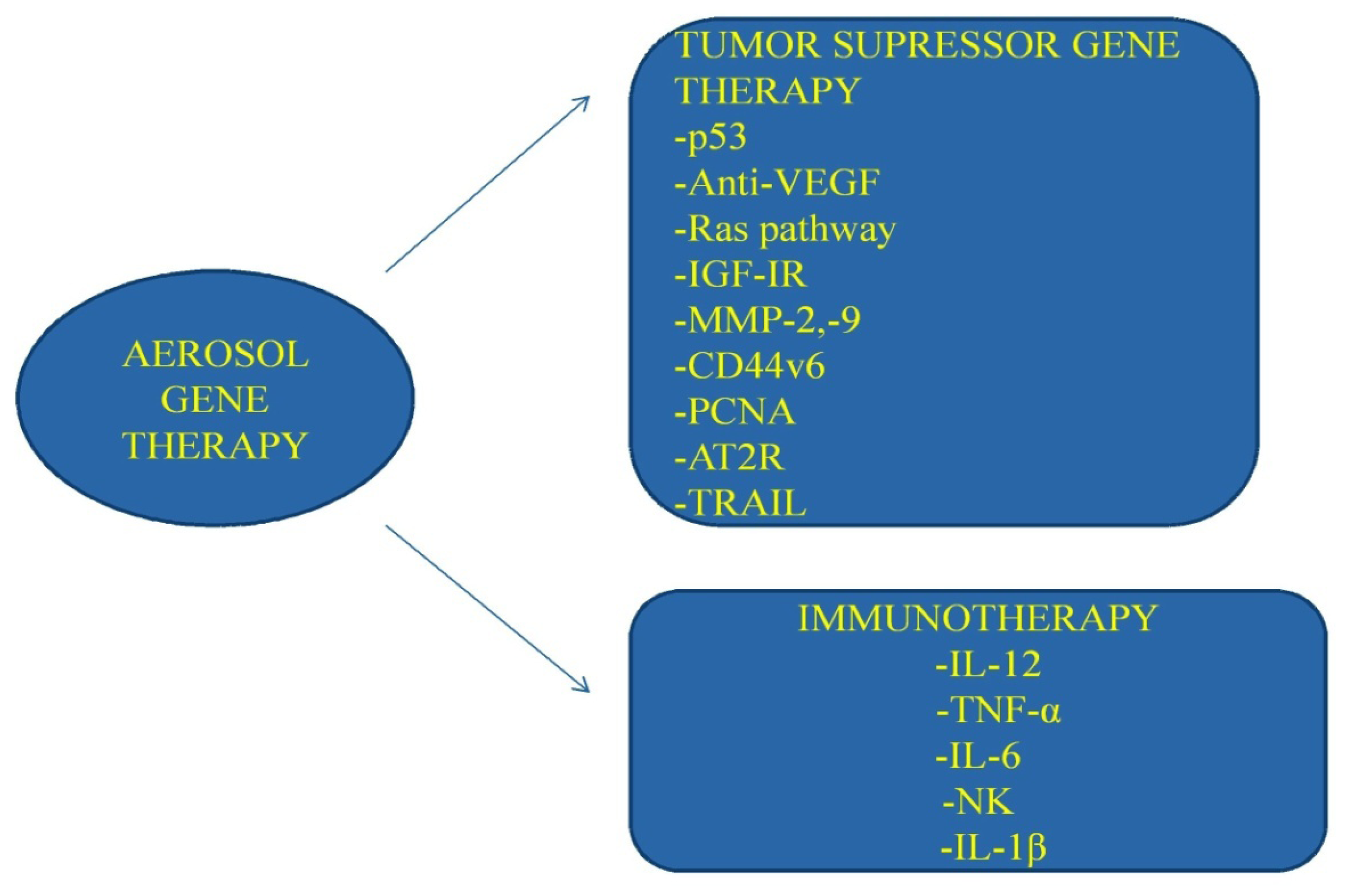
4.1. Aerosolized Vectors Safety Concerns
4.1.1. PEI
4.1.2. cPEI
4.1.3. GPEI
4.1.4. PEI/PEG Noncomplex
4.1.5. Tetrafunctional Amphiphilic Block Copolymer 704
4.1.7. dTAT
4.1.8. Liposome-pDNA
4.1.9. UAC
4.1.10. AND
4.2. Future Nanocomplexes
4.2.1. Cross-Linked Small PEIs
4.2.2. PEIs with PEG Shielding
4.2.3. Solvoplex
4.2.4. APTES
4.2.5. PLGA Delivery System for Immunotherapy
4.2.6. Gene and Chemotherapy in One Complex (mPEG-PCL-g-PEI)
4.2.7. Carbonate Apatite nano-Carriers
4.2.8. F-AL-Ad5
4.2.9. Amino Acids to Enhance the Aerosol Deposition
4.2.10. GOLD Nanoparticles
4.2.11. PH-Release System
4.2.12. Lactoferin Nanoparticles
4.2.13. Mannosylated Liposomes
5. Conclusions
Acknowledgements
- Conflict of InterestThe authors declare no conflict of interest.
References
- Siegel, R.; Naishadham, D.; Jemal, A. Cancer statistics, 2012. CA Cancer J. Clin 2012, 62, 10–29. [Google Scholar]
- Peng, G.; Hakim, M.; Broza, Y.Y.; Billan, S.; Abdah-Bortnyak, R.; Kuten, A.; Tisch, U.; Haick, H. Detection of lung, breast, colorectal, and prostate cancers from exhaled breath using a single array of nanosensors. Br. J. Cancer 2010, 103, 542–551. [Google Scholar]
- Barash, O.; Peled, N.; Tisch, U.; Bunn, P.A., Jr; Hirsch, F.R.; Haick, H. Classification of lung cancer histology by gold nanoparticle sensors. Nanomedicine 2012, 8, 580–589. [Google Scholar]
- Hakim, M.; Billan, S.; Tisch, U. Bad breath: Can analysis of exhaled breath help sniff out cancer? Expert Rev. Mol. Diagn 2011, 11, 469–471. [Google Scholar]
- Peng, G.; Tisch, U.; Adams, O.; Hakim, M.; Shehada, N.; Broza, Y.Y.; Billan, S.; Abdah-Bortnyak, R.; Kuten, A.; Haick, H. Diagnosing lung cancer in exhaled breath using gold nanoparticles. Nat. Nanotechnol 2009, 4, 669–673. [Google Scholar]
- Peng, G.; Tisch, U.; Haick, H. Detection of nonpolar molecules by means of carrier scattering in random networks of carbon nanotubes: Toward diagnosis of diseases via breath samples. Nano Lett 2009, 9, 1362–1368. [Google Scholar]
- Dovgolevsky, E.; Tisch, U.; Haick, H. Chemically sensitive resistors based on monolayer-capped cubic nanoparticles: Towards configurable nanoporous sensors. Small 2009, 5, 1158–1161. [Google Scholar]
- Zarogoulidis, K.; Eleftheriadou, E.; Kontakiotis, T.; Gerasimou, G.; Zarogoulidis, P.; Sapardanis, I.; Galaktidou, G.; Sakkas, L.; Gotzamani-Psarrakou, A.; Karatzas, N. Long acting somatostatin analogues in combination to antineoplastic agents in the treatment of small cell lung cancer patients. Lung Cancer 2012, 76, 84–88. [Google Scholar]
- Liu, L.; Wu, J.; Zhong, R.; Wu, C.; Zou, L.; Yang, B.; Chen, W.; Zhu, B.; Duan, S.; Yu, D.; et al. Multi-loci analysis reveals the importance of genetic variations in sensitivity of platinum-based chemotherapy in non-small-cell lung cancer. Mol. Carcinog 2012. [Google Scholar] [CrossRef]
- Wang, M.; Zhao, J.; Zhang, L.M.; Li, H.; Yu, J.P.; Ren, X.B.; Wang, C.L. Combined Erlotinib and Cetuximab overcome the acquired resistance to epidermal growth factor receptors tyrosine kinase inhibitor in non-small-cell lung cancer. J. Cancer Res. Clin. Oncol 2012. .10.1007/s00432-012-1291-2. [Google Scholar]
- Gridelli, C.; Rossi, A.; Airoma, G.; Bianco, R.; Costanzo, R.; Daniele, B.; Chiara, G.D.; Grimaldi, G.; Irtelli, L.; Maione, P.; et al. Treatment of pulmonary neuroendocrine tumours: State of the art and future developments. Cancer Treat. Rev 2012. .10.1016/j.ctrv.2012.06.012. [Google Scholar]
- Michaelsen, S.R.; Christensen, C.L.; Sehested, M.; Cramer, F.; Poulsen, T.T.; Patterson, A.V.; Poulsen, H.S. Single agent- and combination treatment with two targeted suicide gene therapy systems is effective in chemo-resistant small cell lung cancer (SCLC) cells. J. Gene Med 2012. .10.1002/jgm.2630. [Google Scholar]
- Metro, G.; Chiari, R.; Duranti, S.; Siggillino, A.; Fischer, M.J.; Giannarelli, D.; Ludovini, V.; Bennati, C.; Marcomigni, L.; Baldi, A.; et al. Impact of specific mutant KRAS on clinical outcome of EGFR-TKI-treated advanced non-small cell lung cancer patients with an EGFR wild type genotype. Lung Cancer 2012. .10.1016/j.lungcan.2012.06.005. [Google Scholar]
- Passaro, A.; Palazzo, A.; Trenta, P.; Mancini, M.L.; Morano, F.; Cortesi, E. Molecular and clinical analysis of predictive biomarkers in non-small-cell lung Cancer. Curr. Med. Chem 2012. [Google Scholar] [CrossRef]
- Liu, P.; Morrison, C.; Wang, L.; Xiong, D.; Vedell, P.; Cui, P.; Hua, X.; Ding, F.; Lu, Y.; James, M.; et al. Identification of somatic mutations in non-small cell lung carcinomas using whole-exome sequencing. Carcinogenesis 2012. .10.1093/carcin/bgs148. [Google Scholar]
- Markman, M. Intraperitoneal chemotherapy in the management of ovarian cancer: Focus on carboplatin. Ther. Clin. Risk Manag 2009, 5, 161–168. [Google Scholar]
- Fujiwara, S.; Wada, H.; Miyata, H.; Kawada, J.; Kawabata, R.; Nishikawa, H.; Gnjatic, S.; Sedrak, C.; Sato, E.; Nakamura, Y.; et al. Clinical trial of the intratumoral administration of labeled DC combined with systemic chemotherapy for esophageal cancer. J. Immunother 2012, 35, 513–521. [Google Scholar]
- Zarogoulidis, P.; Eleftheriadou, E.; Sapardanis, I.; Zarogoulidou, V.; Lithoxopoulou, H.; Kontakiotis, T.; Karamanos, N.; Zachariadis, G.; Mabroudi, M.; Zisimopoulos, A.; et al. Feasibility and effectiveness of inhaled carboplatin in NSCLC patients. Invest. New Drugs 2012, 30, 1628–1640. [Google Scholar]
- Zarogoulidis, P.; Chatzaki, E.; Porpodis, K.; Domvri, K.; Hohenforst-Schmidt, W.; Goldberg, E.P.; Karamanos, N.; Zarogoulidis, K. Inhaled chemotherapy in lung cancer: Future concept of nanomedicine. Int. J. Nanomed 2012, 7, 1551–1572. [Google Scholar]
- Zarogoulidis, P.; Chatzaki, E.; Hohenforst-Schmidt, W.; Goldberg, E.P.; Galaktidou, G.; Kontakiotis, T.; Karamanos, N.; Zarogoulidis, K. Management of malignant pleural effusion by suicide gene therapy in advanced stage lung cancer: A case series and literature review. Cancer Gene Ther 2012. .10.1038/cgt.2012.36. [Google Scholar]
- Yu, K.N.; Minai-Tehrani, A.; Chang, S.H.; Hwang, S.K.; Hong, S.H.; Kim, J.E.; Shin, J.Y.; Park, S.J.; Kim, J.H.; Kwon, J.T.; et al. Aerosol delivery of small hairpin osteopontin blocks pulmonary metastasis of breast cancer in mice. PLoS One 2010, 5, e15623. [Google Scholar]
- Tatsumura, T.; Yamamoto, K.; Murakami, A.; Tsuda, M.; Sugiyama, S. New chemotherapeutic method for the treatment of tracheal and bronchial cancers—Nebulization chemotherapy. Gan No Rinsho 1983, 29, 765–770. [Google Scholar]
- Hershey, A.E.; Kurzman, I.D.; Forrest, L.J.; Bohling, C.A.; Stonerook, M.; Placke, M.E.; Imondi, A.R.; Vail, D.M. Inhalation chemotherapy for macroscopic primary or metastatic lung tumors: Proof of principle using dogs with spontaneously occurring tumors as a model. Clin. Cancer Res 1999, 5, 2653–2659. [Google Scholar]
- Hureaux, J.; Lagarce, F.; Gagnadoux, F.; Vecellio, L.; Clavreul, A.; Roger, E.; Kempf, M.; Racineux, J.L.; Diot, P.; Benoit, J.P.; et al. Lipid nanocapsules: Ready-to-use nanovectors for the aerosol delivery of paclitaxel. Eur. J. Pharm. Biopharm 2009, 73, 239–246. [Google Scholar] [Green Version]
- El-Gendy, N.; Berkland, C. Combination chemotherapeutic dry powder aerosols via controlled nanoparticle agglomeration. Pharm. Res 2009, 26, 1752–1763. [Google Scholar]
- Knight, V.; Koshkina, N.V.; Golunski, E.; Roberts, L.E.; Gilbert, B.E. Cyclosporin A aerosol improves the anticancer effect of paclitaxel aerosol in mice. Trans. Am. Clin. Climatol. Assoc 2004, 115, 395–404, Discussion 404. [Google Scholar]
- Wittgen, B.P.; Kunst, P.W.; Perkins, W.R.; Lee, J.K.; Postmus, P.E. Assessing a system to capture stray aerosol during inhalation of nebulized liposomal cisplatin. J. Aerosol. Med 2006, 19, 385–391. [Google Scholar]
- Tseng, C.L.; Su, W.Y.; Yen, K.C.; Yang, K.C.; Lin, F.H. The use of biotinylated-EGF-modified gelatin nanoparticle carrier to enhance cisplatin accumulation in cancerous lungs via inhalation. Biomaterials 2009, 30, 3476–3485. [Google Scholar]
- Wittgen, B.P.; Kunst, P.W.; van der Born, K.; van Wijk, A.W.; Perkins, W.; Pilkiewicz, F.G.; Perez-Soler, R.; Nicholson, S.; Peters, G.J.; Postmus, P.E. Phase I study of aerosolized SLIT cisplatin in the treatment of patients with carcinoma of the lung. Clin. Cancer Res 2007, 13, 2414–2421. [Google Scholar]
- Otterson, G.A.; Villalona-Calero, M.A.; Hicks, W.; Pan, X.; Ellerton, J.A.; Gettinger, S.N.; Murren, J.R. Phase I/II study of inhaled doxorubicin combined with platinum-based therapy for advanced non-small cell lung cancer. Clin. Cancer Res 2010, 16, 2466–2473. [Google Scholar]
- Otterson, G.A.; Villalona-Calero, M.A.; Sharma, S.; Kris, M.G.; Imondi, A.; Gerber, M.; White, D.A.; Ratain, M.J.; Schiller, J.H.; Sandler, A.; et al. Phase I study of inhaled Doxorubicin for patients with metastatic tumors to the lungs. Clin. Cancer Res 2007, 13, 1246–1252. [Google Scholar]
- Verschraegen, C.F.; Gilbert, B.E.; Loyer, E.; Huaringa, A.; Walsh, G.; Newman, R.A.; Knight, V. Clinical evaluation of the delivery and safety of aerosolized liposomal 9-nitro-20(s)-camptothecin in patients with advanced pulmonary malignancies. Clin. Cancer Res 2004, 10, 2319–2326. [Google Scholar]
- Chirmule, N.; Hughes, J.V.; Gao, G.P.; Raper, S.E.; Wilson, J.M. Role of E4 in eliciting CD4 T-cell and B-cell responses to adenovirus vectors delivered to murine and nonhuman primate lungs. J. Virol 1998, 72, 6138–6145. [Google Scholar]
- Gautam, A.; Densmore, C.L.; Waldrep, J.C. Pulmonary cytokine responses associated with PEI-DNA aerosol gene therapy. Gene Ther 2001, 8, 254–257. [Google Scholar]
- West, J.; Rodman, D.M. Gene therapy for pulmonary diseases. Chest 2001, 119, 613–617. [Google Scholar]
- Manunta, M.D.; McAnulty, R.J.; Tagalakis, A.D.; Bottoms, S.E.; Campbell, F.; Hailes, H.C.; Tabor, A.B.; Laurent, G.J.; O’Callaghan, C.; Hart, S.L. Nebulisation of receptor-targeted nanocomplexes for gene delivery to the airway epithelium. PLoS One 2011, 6, e26768. [Google Scholar]
- Gautam, A.; Densmore, C.L.; Xu, B.; Waldrep, J.C. Enhanced gene expression in mouse lung after PEI-DNA aerosol delivery. Mol. Ther 2000, 2, 63–70. [Google Scholar]
- Zamora-Avila, D.E.; Zapata-Benavides, P.; Franco-Molina, M.A.; Saavedra-Alonso, S.; Trejo-Avila, L.M.; Resendez-Perez, D.; Mendez-Vazquez, J.L.; Isaias-Badillo, J.; Rodriguez-Padilla, C. WT1 gene silencing by aerosol delivery of PEI-RNAi complexes inhibits B16-F10 lung metastases growth. Cancer Gene Ther 2009, 16, 892–899. [Google Scholar]
- Densmore, C.L. The re-emergence of aerosol gene delivery: A viable approach to lung cancer therapy. Curr. Cancer Drug Targets 2003, 3, 275–286. [Google Scholar]
- Frederiksen, K.S.; Abrahamsen, N.; Cristiano, R.J.; Damstrup, L.; Poulsen, H.S. Gene delivery by an epidermal growth factor/DNA polyplex to small cell lung cancer cell lines expressing low levels of epidermal growth factor receptor. Cancer Gene Ther 2000, 7, 262–268. [Google Scholar]
- Kim, H.W.; Park, I.K.; Cho, C.S.; Lee, K.H.; Beck, G.R., Jr; Colburn, N.H.; Cho, M.H. Aerosol delivery of glucosylated polyethylenimine/phosphatase and tensin homologue deleted on chromosome 10 complex suppresses Akt downstream pathways in the lung of K-ras null mice. Cancer Res. 2004, 64, 7971–7976. [Google Scholar]
- Zou, Y.; Tornos, C.; Qiu, X.; Lia, M.; Perez-Soler, R. p53 aerosol formulation with low toxicity and high efficiency for early lung cancer treatment. Clin. Cancer Res 2007, 13, 4900–4908. [Google Scholar]
- Gautam, A.; Densmore, C.L.; Melton, S.; Golunski, E.; Waldrep, J.C. Aerosol delivery of PEI-p53 complexes inhibits B16-F10 lung metastases through regulation of angiogenesis. Cancer Gene Ther 2002, 9, 28–36. [Google Scholar]
- Lumb, A.B.; Nunn, J.F. Nunn’s Applied Respiratory Physiology, 5th ed; Butterworth-Heinemann: Oxford, UK; Boston, MA, USA, 2000; p. 687. [Google Scholar]
- El-Chemaly, S.; Levine, S.J.; Moss, J. Lymphatics in lung disease. Ann. N. Y. Acad.Sci 2008, 1131, 195–202. [Google Scholar]
- Cryan, S.A. Carrier-based strategies for targeting protein and peptide drugs to the lungs. AAPS J 2005, 7, E20–E41. [Google Scholar]
- Leclerc, J.; Courcot-Ngoubo Ngangue, E.; Cauffiez, C.; Allorge, D.; Pottier, N.; Lafitte, J.J.; Debaert, M.; Jaillard, S.; Broly, F.; Lo-Guidice, J.M. Xenobiotic metabolism and disposition in human lung: Transcript profiling in non-tumoral and tumoral tissues. Biochimie 2011, 93, 1012–1027. [Google Scholar]
- Bosquillon, C. Drug transporters in the lung—Do they play a role in the biopharmaceutics of inhaled drugs? J. Pharm. Sci 2010, 99, 2240–2255. [Google Scholar]
- Corti, A.; Pastorino, F.; Curnis, F.; Arap, W.; Ponzoni, M.; Pasqualini, R. Targeted drug delivery and penetration into solid tumors. Med. Res. Rev 2011. .10.1002/med.20238. [Google Scholar]
- Waite, C.L.; Roth, C.M. Nanoscale drug delivery systems for enhanced drug penetration into solid tumors: Current progress and opportunities. Crit. Rev. Biomed. Eng 2012, 40, 21–41. [Google Scholar]
- Cuong, N.V.; Hsieh, M.F. Molecular targeting of liposomal nano-particles to lymphatic system. Curr. Cancer Drug Targets 2011, 11, 147–155. [Google Scholar]
- Shinohara, H. Distribution of lymphatic stomata on the pleural surface of the thoracic cavity and the surface topography of the pleural mesothelium in the golden hamster. Anat. Rec 1997, 249, 16–23. [Google Scholar]
- Swift, D.L. Aerosols and humidity therapy. Generation and respiratory deposition of therapeutic aerosols. Am. Rev. Respir. Dis 1980, 122, 71–77. [Google Scholar]
- Houtmeyers, E.; Gosselink, R.; Gayan-Ramirez, G.; Decramer, M. Regulation of mucociliary clearance in health and disease. Eur. Respir. J 1999, 13, 1177–1188. [Google Scholar]
- Dolovich, M.B.; Killian, D.; Wolff, R.K.; Obminski, G.; Newhouse, M.T. Pulmonary aerosol deposition in chronic bronchitis: Intermittent positive pressure breathing vs. quiet breathing. Am. Rev. Respir. Dis 1977, 115, 397–402. [Google Scholar]
- Dolovich, M.B.; Sanchis, J.; Rossman, C.; Newhouse, M.T. Aerosol penetrance: A sensitive index of peripheral airways obstruction. J. Appl. Physiol 1976, 40, 468–471. [Google Scholar]
- Messina, M.S.; Smaldone, G.C. Evaluation of quantitative aerosol techniques for use in bronchoprovocation studies. J. Allergy Clin. Immunol 1985, 75, 252–257. [Google Scholar]
- Nunn, J.F. Nunn’s Applied Respiratory Physiology, 4th ed; Butterworth-Heinemann: Oxford, UK; Boston, MA, USA, 1993; p. 658. [Google Scholar]
- Zarogoulidis, P.; Papanas, N.; Kouliatsis, G.; Spyratos, D.; Zarogoulidis, K.; Maltezos, E. Inhaled insulin: Too soon to be forgotten? J. Aerosol. Med. Pulm. Drug Deliv 2011, 24, 213–223. [Google Scholar]
- Gautam, A.; Densmore, C.L.; Golunski, E.; Xu, B.; Waldrep, J.C. Transgene expression in mouse airway epithelium by aerosol gene therapy with PEI-DNA complexes. Mol. Ther 2001, 3, 551–556. [Google Scholar]
- Densmore, C.L.; Kleinerman, E.S.; Gautam, A.; Jia, S.F.; Xu, B.; Worth, L.L.; Waldrep, J.C.; Fung, Y.K.; T’Ang, A.; Knight, V. Growth suppression of established human osteosarcoma lung metastases in mice by aerosol gene therapy with PEI-p53 complexes. Cancer Gene Ther 2001, 8, 619–627. [Google Scholar]
- Davies, L.A.; McLachlan, G.; Sumner-Jones, S.G.; Ferguson, D.; Baker, A.; Tennant, P.; Gordon, C.; Vrettou, C.; Baker, E.; Zhu, J.; et al. Enhanced lung gene expression after aerosol delivery of concentrated pDNA/PEI complexes. Mol. Ther 2008, 16, 1283–1290. [Google Scholar]
- Gautam, A.; Waldrep, J.C.; Kleinerman, E.S.; Xu, B.; Fung, Y.K.; T’Ang, A.; Densmore, C.L. Aerosol gene therapy for metastatic lung cancer using PEI-p53 complexes. Methods Mol. Med 2003, 75, 607–618. [Google Scholar]
- Gautam, A.; Waldrep, J.C.; Orson, F.M.; Kinsey, B.M.; Xu, B.; Densmore, C.L. Topical gene therapy for pulmonary diseases with PEI-DNA aerosol complexes. Methods Mol. Med 2003, 75, 561–572. [Google Scholar]
- Davis, J.N.; Stagg, D. Interrelationships of the volume and time components of individual breaths in resting man. J. Physiol 1975, 245, 481–498. [Google Scholar]
- Anderson, M.; Svartengren, M.; Bylin, G.; Philipson, K.; Camner, P. Deposition in asthmatics of particles inhaled in air or in helium-oxygen. Am. Rev. Respir. Dis 1993, 147, 524–528. [Google Scholar]
- Summers, Q.A. Inhaled drugs and the lung. Clin. Exp. Allergy 1991, 21, 259–268. [Google Scholar]
- Labiris, N.R.; Dolovich, M.B. Pulmonary drug delivery. Part II: The role of inhalant delivery devices and drug formulations in therapeutic effectiveness of aerosolized medications. Br. J. Clin. Pharmacol 2003, 56, 600–612. [Google Scholar]
- Labiris, N.R.; Dolovich, M.B. Pulmonary drug delivery. Part I: Physiological factors affecting therapeutic effectiveness of aerosolized medications. Br. J. Clin. Pharmacol 2003, 56, 588–599. [Google Scholar]
- Dong, A.Q.; Kong, M.J.; Ma, Z.Y.; Qian, J.F.; Xu, X.H. Down-regulation of IGF-IR using small, interfering, hairpin RNA (siRNA) inhibits growth of human lung cancer cell line A549 in vitro and in nude mice. Cell Biol. Int 2007, 31, 500–507. [Google Scholar]
- Kawabata, A.; Baoum, A.; Ohta, N.; Jacquez, S.; Seo, G.M.; Berkland, C.; Tamura, M. Intratracheal administration of a nanoparticle-based therapy with the angiotensin II type 2 receptor gene attenuates lung cancer growth. Cancer Res 2012, 72, 2057–2067. [Google Scholar]
- Zhong, Z.; Wan, Y.; Han, J.; Shi, S.; Zhang, Z.; Sun, X. Improvement of adenoviral vector-mediated gene transfer to airway epithelia by folate-modified anionic liposomes. Int. J. Nanomed 2011, 6, 1083–1093. [Google Scholar]
- Klonne, D.R.; Dodd, D.E.; Losco, P.E.; Troup, C.M.; Tyler, T.R. Two-week aerosol inhalation study on polyethylene glycol (PEG) 3350 in F-344 rats. Drug Chem. Toxicol 1989, 12, 39–48. [Google Scholar]
- Minai-Tehrani, A.; Park, Y.C.; Hwang, S.K.; Kwon, J.T.; Chang, S.H.; Park, S.J.; Yu, K.N.; Kim, J.E.; Shin, J.Y.; Kim, J.H.; et al. Aerosol delivery of kinase-deficient Akt1 attenuates Clara cell injury induced by naphthalene in the lungs of dual luciferase mice. J. Vet. Sci 2011, 12, 309–317. [Google Scholar]
- Maestrelli, P.; Schlunssen, V.; Mason, P.; Sigsgaard, T. Contribution of host factors and workplace exposure to the outcome of occupational asthma. Eur. Respir. Rev 2012, 21, 88–96. [Google Scholar]
- Godbey, W.T.; Wu, K.K.; Mikos, A.G. Tracking the intracellular path of poly(ethylenimine)/ DNA complexes for gene delivery. Proc. Natl. Acad. Sci. USA 1999, 96, 5177–5181. [Google Scholar]
- Ferrari, S.; Pettenazzo, A.; Garbati, N.; Zacchello, F.; Behr, J.P.; Scarpa, M. Polyethylenimine shows properties of interest for cystic fibrosis gene therapy. Biochim. Biophys. Acta 1999, 1447, 219–225. [Google Scholar]
- Densmore, C.L.; Orson, F.M.; Xu, B.; Kinsey, B.M.; Waldrep, J.C.; Hua, P.; Bhogal, B.; Knight, V. Aerosol delivery of robust polyethyleneimine-DNA complexes for gene therapy and genetic immunization. Mol. Ther 2000, 1, 180–188. [Google Scholar]
- Ernst, N.; Ulrichskotter, S.; Schmalix, W.A.; Radler, J.; Galneder, R.; Mayer, E.; Gersting, S.; Plank, C.; Reinhardt, D.; Rosenecker, J. Interaction of liposomal and polycationic transfection complexes with pulmonary surfactant. J. Gene Med 1999, 1, 331–340. [Google Scholar]
- Gautam, A.; Densmore, C.L.; Waldrep, J.C. Inhibition of experimental lung metastasis by aerosol delivery of PEI-p53 complexes. Mol. Ther 2000, 2, 318–323. [Google Scholar]
- Koshkina, N.V.; Agoulnik, I.Y.; Melton, S.L.; Densmore, C.L.; Knight, V. Biodistribution and pharmacokinetics of aerosol and intravenously administered DNA-polyethyleneimine complexes: Optimization of pulmonary delivery and retention. Mol. Ther 2003, 8, 249–254. [Google Scholar]
- Hasenpusch, G.; Pfeifer, C.; Aneja, M.K.; Wagner, K.; Reinhardt, D.; Gilon, M.; Ohana, P.; Hochberg, A.; Rudolph, C. Aerosolized BC-819 inhibits primary but not secondary lung cancer growth. PLoS One 2011, 6, e20760. [Google Scholar]
- Duan, X.; Jia, S.F.; Koshkina, N.; Kleinerman, E.S. Intranasal interleukin-12 gene therapy enhanced the activity of ifosfamide against osteosarcoma lung metastases. Cancer 2006, 106, 1382–1388. [Google Scholar]
- Tan, Y.; Li, S.; Pitt, B.R.; Huang, L. The inhibitory role of CpG immunostimulatory motifs in cationic lipid vector-mediated transgene expression in vivo. Hum. Gene Ther 1999, 10, 2153–2161. [Google Scholar]
- Freimark, B.D.; Blezinger, H.P.; Florack, V.J.; Nordstrom, J.L.; Long, S.D.; Deshpande, D.S.; Nochumson, S.; Petrak, K.L. Cationic lipids enhance cytokine and cell influx levels in the lung following administration of plasmid: Cationic lipid complexes. J. Immunol 1998, 160, 4580–4586. [Google Scholar]
- Li, S.; Wu, S.P.; Whitmore, M.; Loeffert, E.J.; Wang, L.; Watkins, S.C.; Pitt, B.R.; Huang, L. Effect of immune response on gene transfer to the lung via systemic administration of cationic lipidic vectors. Am. J. Physiol 1999, 276, L796–L804. [Google Scholar]
- Jia, S.F.; Worth, L.L.; Densmore, C.L.; Xu, B.; Duan, X.; Kleinerman, E.S. Aerosol gene therapy with PEI: IL-12 eradicates osteosarcoma lung metastases. Clin. Cancer Res 2003, 9, 3462–3468. [Google Scholar]
- Jia, S.F.; Worth, L.L.; Densmore, C.L.; Xu, B.; Zhou, Z.; Kleinerman, E.S. Eradication of osteosarcoma lung metastases following intranasal interleukin-12 gene therapy using a nonviral polyethylenimine vector. Cancer Gene Ther 2002, 9, 260–266. [Google Scholar]
- Cohen, J. IL-12 deaths: Explanation and a puzzle. Science 1995, 270, 908. [Google Scholar]
- Tehrani, A.M.; Hwang, S.K.; Kim, T.H.; Cho, C.S.; Hua, J.; Nah, W.S.; Kwon, J.T.; Kim, J.S.; Chang, S.H.; Yu, K.N.; et al. Aerosol delivery of Akt controls protein translation in the lungs of dual luciferase reporter mice. Gene Ther 2007, 14, 451–458. [Google Scholar]
- Hwang, S.K.; Jin, H.; Kwon, J.T.; Chang, S.H.; Kim, T.H.; Cho, C.S.; Lee, K.H.; Young, M.R.; Colburn, N.H.; Beck, G.R., Jr; et al. Aerosol-delivered programmed cell death 4 enhanced apoptosis, controlled cell cycle and suppressed. AP-1 activity in the lungs of AP-1 luciferase reporter mice. Gene Ther. 2007, 14, 1353–1361. [Google Scholar]
- Jere, D.; Yoo, M.K.; Arote, R.; Kim, T.H.; Cho, M.H.; Nah, J.W.; Choi, Y.J.; Cho, C.S. Poly (amino ester) composed of poly (ethylene glycol) and aminosilane prepared by combinatorial chemistry as a gene carrier. Pharm. Res 2008, 25, 875–885. [Google Scholar]
- Xu, C.X.; Jere, D.; Jin, H.; Chang, S.H.; Chung, Y.S.; Shin, J.Y.; Kim, J.E.; Park, S.J.; Lee, Y.H.; Chae, C.H.; et al. Poly(ester amine)-mediated, aerosol-delivered Akt1 small interfering RNA suppresses lung tumorigenesis. Am. J. Respir. Crit. Care Med 2008, 178, 60–73. [Google Scholar]
- Park, M.R.; Han, K.O.; Han, I.K.; Cho, M.H.; Nah, J.W.; Choi, Y.J.; Cho, C.S. Degradable polyethylenimine-alt-poly(ethylene glycol) copolymers as novel gene carriers. J. Control. Release 2005, 105, 367–380. [Google Scholar]
- Pitard, B.; Bello-Roufai, M.; Lambert, O.; Richard, P.; Desigaux, L.; Fernandes, S.; Lanctin, C.; Pollard, H.; Zeghal, M.; Rescan, P.Y.; et al. Negatively charged self-assembling DNA/poloxamine nanospheres for in vivo gene transfer. Nucleic Acids Res 2004, 32, e159. [Google Scholar]
- Richard-Fiardo, P.; Cambien, B.; Pradelli, E.; Beilvert, F.; Pitard, B.; Schmid-Antomarchi, H.; Schmid-Alliana, A. Effect of fractalkine-Fc delivery in experimental lung metastasis using DNA/704 nanospheres. Cancer Gene Ther 2011, 18, 761–772. [Google Scholar]
- Xing, Z.; Ohkawara, Y.; Jordana, M.; Graham, F.; Gauldie, J. Transfer of granulocyte-macrophage colony-stimulating factor gene to rat lung induces eosinophilia, monocytosis, and fibrotic reactions. J. Clin. Invest 1996, 97, 1102–1110. [Google Scholar]
- Xing, Z.; Braciak, T.; Jordana, M.; Croitoru, K.; Graham, F.L.; Gauldie, J. Adenovirus-mediated cytokine gene transfer at tissue sites. Overexpression of IL-6 induces lymphocytic hyperplasia in the lung. J. Immunol 1994, 153, 4059–4069. [Google Scholar]
- Arndt, C.A.; Koshkina, N.V.; Inwards, C.Y.; Hawkins, D.S.; Krailo, M.D.; Villaluna, D.; Anderson, P.M.; Goorin, A.M.; Blakely, M.L.; Bernstein, M.; et al. Inhaled granulocyte-macrophage colony stimulating factor for first pulmonary recurrence of osteosarcoma: Effects on disease-free survival and immunomodulation. a report from the Children’s Oncology Group. Clin. Cancer Res 2010, 16, 4024–4030. [Google Scholar]
- Takagi, T.; Nakano, Y.; Takekoshi, S.; Inagami, T.; Tamura, M. Hemizygous mice for the angiotensin II type 2 receptor gene have attenuated susceptibility to azoxymethane-induced colon tumorigenesis. Carcinogenesis 2002, 23, 1235–1241. [Google Scholar]
- Kanehira, T.; Tani, T.; Takagi, T.; Nakano, Y.; Howard, E.F.; Tamura, M. Angiotensin II type 2 receptor gene deficiency attenuates susceptibility to tobacco-specific nitrosamine-induced lung tumorigenesis: Involvement of transforming growth factor-beta-dependent cell growth attenuation. Cancer Res 2005, 65, 7660–7665. [Google Scholar]
- Takeda, K.; Smyth, M.J.; Cretney, E.; Hayakawa, Y.; Yamaguchi, N.; Yagita, H.; Okumura, K. Involvement of tumor necrosis factor-related apoptosis-inducing ligand in NK cell-mediated and IFN-gamma-dependent suppression of subcutaneous tumor growth. Cell. Immunol 2001, 214, 194–200. [Google Scholar]
- Kedinger, V.; Muller, S.; Gronemeyer, H. Targeted expression of tumor necrosis factor-related apoptosis-inducing ligand TRAIL in skin protects mice against chemical carcinogenesis. Mol. Cancer 2011, 10, 34. [Google Scholar]
- Jin, H.; Kim, T.H.; Hwang, S.K.; Chang, S.H.; Kim, H.W.; Anderson, H.K.; Lee, H.W.; Lee, K.H.; Colburn, N.H.; Yang, H.S.; et al. Aerosol delivery of urocanic acid-modified chitosan/programmed cell death 4 complex regulated apoptosis, cell cycle, and angiogenesis in lungs of K-ras null mice. Mol. Cancer Ther 2006, 5, 1041–1049. [Google Scholar]
- Koping-Hoggard, M.; Tubulekas, I.; Guan, H.; Edwards, K.; Nilsson, M.; Varum, K.M.; Artursson, P. Chitosan as a nonviral gene delivery system. Structure-property relationships and characteristics compared with polyethylenimine in vitro and after lung administration in vivo. Gene Ther 2001, 8, 1108–1121. [Google Scholar]
- Jiang, H.L.; Park, I.K.; Shin, N.R.; Yoo, H.S.; Akaike, T.; Cho, C.S. Controlled release of Bordetella bronchiseptica dermonecrotoxin (BBD) vaccine from BBD-loaded chitosan microspheres in vitro. Arch. Pharm. Res 2004, 27, 346–350. [Google Scholar]
- Okamoto, H.; Shiraki, K.; Yasuda, R.; Danjo, K.; Watanabe, Y. Chitosan-interferon-beta gene complex powder for inhalation treatment of lung metastasis in mice. J. Control. Release 2011, 150, 187–195. [Google Scholar]
- Okamoto, H.; Nishida, S.; Todo, H.; Sakakura, Y.; Iida, K.; Danjo, K. Pulmonary gene delivery by chitosan-pDNA complex powder prepared by a supercritical carbon dioxide process. J. Pharm. Sci 2003, 92, 371–380. [Google Scholar]
- Huang, Y.C.; Vieira, A.; Huang, K.L.; Yeh, M.K.; Chiang, C.H. Pulmonary inflammation caused by chitosan microparticles. J. Biomed. Mater. Res. A 2005, 75, 283–287. [Google Scholar]
- Takeuchi, H.; Matsui, Y.; Sugihara, H.; Yamamoto, H.; Kawashima, Y. Effectiveness of submicron-sized, chitosan-coated liposomes in oral administration of peptide drugs. Int. J. Pharm 2005, 303, 160–170. [Google Scholar]
- Lotze, M.T.; Kost, T.A. Viruses as gene delivery vectors: Application to gene function, target validation, and assay development. Cancer Gene Ther 2002, 9, 692–699. [Google Scholar]
- Thomas, M.; Ge, Q.; Lu, J.J.; Chen, J.; Klibanov, A.M. Cross-linked small polyethylenimines: While still nontoxic, deliver DNA efficiently to mammalian cells in vitro and in vivo. Pharm. Res 2005, 22, 373–380. [Google Scholar]
- Panyam, J.; Labhasetwar, V. Biodegradable nanoparticles for drug and gene delivery to cells and tissue. Adv. Drug Deliv. Rev 2003, 55, 329–347. [Google Scholar]
- Wang, Y.Q.; Su, J.; Wu, F.; Lu, P.; Yuan, L.F.; Yuan, W.E.; Sheng, J.; Jin, T. Biscarbamate cross-linked polyethylenimine derivative with low molecular weight, low cytotoxicity, and high efficiency for gene delivery. Int. J. Nanomed 2012, 7, 693–704. [Google Scholar]
- Uchida, S.; Itaka, K.; Chen, Q.; Osada, K.; Ishii, T.; Shibata, M.A.; Harada-Shiba, M.; Kataoka, K. PEGylated polyplex with optimized peg shielding enhances gene introduction in lungs by minimizing inflammatory responses. Mol. Ther 2012, 20, 1196–1203. [Google Scholar]
- Brissault, B.; Kichler, A.; Leborgne, C.; Danos, O.; Cheradame, H.; Gau, J.; Auvray, L.; Guis, C. Synthesis, characterization, and gene transfer application of poly(ethylene glycol-b-ethylenimine) with high molar mass polyamine block. Biomacromolecules 2006, 7, 2863–2870. [Google Scholar]
- Fan, W.; Wu, X.; Ding, B.; Gao, J.; Cai, Z.; Zhang, W.; Yin, D.; Wang, X.; Zhu, Q.; Liu, J.; et al. Degradable gene delivery systems based on Pluronics-modified low-molecular-weight polyethylenimine: Preparation, characterization, intracellular trafficking, and cellular distribution. Int. J. Nanomed 2012, 7, 1127–1138. [Google Scholar]
- Jiang, Z.; Sun, C.; Yin, Z.; Zhou, F.; Ge, L.; Liu, X.; Kong, F. Comparison of two kinds of nanomedicine for targeted gene therapy: Premodified or postmodified gene delivery systems. Int. J. Nanomed 2012, 7, 2019–2031. [Google Scholar]
- Margaris, K.N.; Black, R.A. Modelling the lymphatic system: Challenges and opportunities. J. R. Soc. Interface 2012, 9, 601–612. [Google Scholar]
- Zeng, Q.; Han, J.; Zhao, D.; Gong, T.; Zhang, Z.; Sun, X. Protection of adenovirus from neutralizing antibody by cationic PEG derivative ionically linked to adenovirus. Int. J. Nanomed 2012, 7, 985–997. [Google Scholar]
- Schughart, K.; Bischoff, R.; Rasmussen, U.B.; Hadji, D.A.; Perraud, F.; Accart, N.; Boussif, O.; Silvestre, N.; Cordier, Y.; Pavirani, A.; et al. Solvoplex: A new type of synthetic vector for intrapulmonary gene delivery. Hum. Gene Ther 1999, 10, 2891–2905. [Google Scholar]
- Schughart, K.; Rasmussen, U.B. Solvoplex synthetic vector for intrapulmonary gene delivery. Preparation and use. Methods Mol. Med 2002, 69, 83–94. [Google Scholar]
- Cheang, T.Y.; Tang, B.; Xu, A.W.; Chang, G.Q.; Hu, Z.J.; He, W.L.; Xing, Z.H.; Xu, J.B.; Wang, M.; Wang, S.M. Promising plasmid DNA vector based on APTES-modified silica nanoparticles. Int. J. Nanomed 2012, 7, 1061–1067. [Google Scholar]
- He, X.; Nie, H.; Wang, K.; Tan, W.; Wu, X.; Zhang, P. In vivo study of biodistribution and urinary excretion of surface-modified silica nanoparticles. Anal. Chem 2008, 80, 9597–9603. [Google Scholar]
- Burns, A.A.; Vider, J.; Ow, H.; Herz, E.; Penate-Medina, O.; Baumgart, M.; Larson, S.M.; Wiesner, U.; Bradbury, M. Fluorescent silica nanoparticles with efficient urinary excretion for nanomedicine. Nano Lett 2009, 9, 442–448. [Google Scholar]
- Ma, W.; Chen, M.; Kaushal, S.; McElroy, M.; Zhang, Y.; Ozkan, C.; Bouvet, M.; Kruse, C.; Grotjahn, D.; Ichim, T.; et al. PLGA nanoparticle-mediated delivery of tumor antigenic peptides elicits effective immune responses. Int. J. Nanomed 2012, 7, 1475–1487. [Google Scholar]
- Li, M.; Panagi, Z.; Avgoustakis, K.; Reineke, J. Physiologically based pharmacokinetic modeling of PLGA nanoparticles with varied mPEG content. Int. J. Nanomed 2012, 7, 1345–1356. [Google Scholar]
- Shi, S.; Zhu, X.; Guo, Q.; Wang, Y.; Zuo, T.; Luo, F.; Qian, Z. Self-assembled mPEG-PCL-g-PEI micelles for simultaneous codelivery of chemotherapeutic drugs and DNA: Synthesis and characterization in vitro. Int. J. Nanomed 2012, 7, 1749–1759. [Google Scholar]
- Chowdhury, E.H.; Akaike, T. High performance DNA nano-carriers of carbonate apatite: Multiple factors in regulation of particle synthesis and transfection efficiency. Int. J. Nanomed 2007, 2, 101–106. [Google Scholar]
- Hossain, S.; Stanislaus, A.; Chua, M.J.; Tada, S.; Tagawa, Y.; Chowdhury, E.H.; Akaike, T. Carbonate apatite-facilitated intracellularly delivered siRNA for efficient knockdown of functional genes. J. Control. Release 2010, 147, 101–108. [Google Scholar]
- Hossain, S.; Tada, S.; Akaike, T.; Chowdhury, E.H. Influences of electrolytes and glucose on formulation of carbonate apatite nanocrystals for efficient gene delivery to mammalian cells. Anal. Biochem 2010, 397, 156–161. [Google Scholar]
- Sudimack, J.; Lee, R.J. Targeted drug delivery via the folate receptor. Adv. Drug Deliv. Rev 2000, 41, 147–162. [Google Scholar]
- Li, H.Y.; Seville, P.C.; Williamson, I.J.; Birchall, J.C. The use of amino acids to enhance the aerosolisation of spray-dried powders for pulmonary gene therapy. J. Gene Med 2005, 7, 343–353. [Google Scholar]
- Li, H.Y.; Neill, H.; Innocent, R.; Seville, P.; Williamson, I.; Birchall, J.C. Enhanced dispersibility and deposition of spray-dried powders for pulmonary gene therapy. J. Drug Target 2003, 11, 425–432. [Google Scholar]
- Puvanakrishnan, P.; Park, J.; Chatterjee, D.; Krishnan, S.; Tunnell, J.W. In vivo tumor targeting of gold nanoparticles: Effect of particle type and dosing strategy. Int. J. Nanomed 2012, 7, 1251–1258. [Google Scholar]
- Hirsch, L.R.; Stafford, R.J.; Bankson, J.A.; Sershen, S.R.; Rivera, B.; Price, R.E.; Hazle, J.D.; Halas, N.J.; West, J.L. Nanoshell-mediated near-infrared thermal therapy of tumors under magnetic resonance guidance. Proc. Natl. Acad. Sci. USA 2003, 100, 13549–13554. [Google Scholar]
- Loo, C.; Lowery, A.; Halas, N.; West, J.; Drezek, R. Immunotargeted nanoshells for integrated cancer imaging and therapy. Nano Lett 2005, 5, 709–711. [Google Scholar]
- Li, P.; Liu, D.; Miao, L.; Liu, C.; Sun, X.; Liu, Y.; Zhang, N. A pH-sensitive multifunctional gene carrier assembled via layer-by-layer technique for efficient gene delivery. Int. J. Nanomed 2012, 7, 925–939. [Google Scholar]
- Metz-Boutigue, M.H.; Jolles, J.; Mazurier, J.; Schoentgen, F.; Legrand, D.; Spik, G.; Montreuil, J.; Jolles, P. Human lactotransferrin: Amino acid sequence and structural comparisons with other transferrins. Eur. J. Biochem 1984, 145, 659–676. [Google Scholar]
- Teng, C.T.; Beard, C.; Gladwell, W. Differential expression and estrogen response of lactoferrin gene in the female reproductive tract of mouse, rat, and hamster. Biol. Reprod 2002, 67, 1439–1449. [Google Scholar]
- Choe, T.B.; Park, I.C.; Hong, S.I. Enhancement of cationic liposome-mediated transfection by lactoferrin. Biotechnol. Tech 1998, 12, 577–581. [Google Scholar]
- Gupta, A.K.; Curtis, A.S. Lactoferrin and ceruloplasmin derivatized superparamagnetic iron oxide nanoparticles for targeting cell surface receptors. Biomaterials 2004, 25, 3029–3040. [Google Scholar]
- Legrand, D.; Pierce, A.; Elass, E.; Carpentier, M.; Mariller, C.; Mazurier, J. Lactoferrin structure and functions. Adv. Exp. Med. Biol 2008, 606, 163–194. [Google Scholar]
- Suzuki, Y.A.; Lopez, V.; Lonnerdal, B. Mammalian lactoferrin receptors: Structure and function. Cell. Mol. Life Sci 2005, 62, 2560–2575. [Google Scholar]
- Kong, F.; Zhou, F.; Ge, L.; Liu, X.; Wang, Y. Mannosylated liposomes for targeted gene delivery. Int. J. Nanomed 2012, 7, 1079–1089. [Google Scholar]
- Tomko, R.P.; Xu, R.; Philipson, L. HCAR and MCAR: The human and mouse cellular receptors for subgroup C adenoviruses and group B coxsackieviruses. Proc. Natl. Acad. Sci. USA 1997, 94, 3352–3356. [Google Scholar]
- Ahn, C.H.; Chae, S.Y.; Bae, Y.H.; Kim, S.W. Biodegradable poly(ethylenimine) for plasmid DNA delivery. J. Control. Release 2002, 80, 273–282. [Google Scholar]
- Densmore, C.L. Advances in noninvasive pulmonary gene therapy. Curr. Drug Deliv 2006, 3, 55–63. [Google Scholar]
- Eastman, S.J.; Lukason, M.J.; Tousignant, J.D.; Murray, H.; Lane, M.D.; St George, J.A.; Akita, G.Y.; Cherry, M.; Cheng, S.H.; Scheule, R.K. A concentrated and stable aerosol formulation of cationic lipid: DNA complexes giving high-level gene expression in mouse lung. Hum. Gene Ther 1997, 8, 765–773. [Google Scholar]
- Eastman, S.J.; Tousignant, J.D.; Lukason, M.J.; Murray, H.; Siegel, C.S.; Constantino, P.; Harris, D.J.; Cheng, S.H.; Scheule, R.K. Optimization of formulations and conditions for the aerosol delivery of functional cationic lipid: DNA complexes. Hum. Gene Ther 1997, 8, 313–322. [Google Scholar]
- Eastman, S.J.; Tousignant, J.D.; Lukason, M.J.; Chu, Q.; Cheng, S.H.; Scheule, R.K. Aerosolization of cationic lipid: pDNA complexes—In vitro optimization of nebulizer parameters for human clinical studies. Hum. Gene Ther 1998, 9, 43–52. [Google Scholar]
- Beck, S.E.; Laube, B.L.; Barberena, C.I.; Fischer, A.C.; Adams, R.J.; Chesnut, K.; Flotte, T.R.; Guggino, W.B. Deposition and expression of aerosolized rAAV vectors in the lungs of Rhesus macaques. Mol. Ther 2002, 6, 546–554. [Google Scholar]
- Dunlap, D.D.; Maggi, A.; Soria, M.R.; Monaco, L. Nanoscopic structure of DNA condensed for gene delivery. Nucleic Acids Res 1997, 25, 3095–3101. [Google Scholar]
- Rudolph, C.; Lausier, J.; Naundorf, S.; Muller, R.H.; Rosenecker, J. In vivo gene delivery to the lung using polyethylenimine and fractured polyamidoamine dendrimers. J. Gene Med 2000, 2, 269–278. [Google Scholar]
- Rudolph, C.; Ortiz, A.; Schillinger, U.; Jauernig, J.; Plank, C.; Rosenecker, J. Methodological optimization of polyethylenimine (PEI)-based gene delivery to the lungs of mice via aerosol application. J. Gene Med 2005, 7, 59–66. [Google Scholar]
- Kooijmans, S.A.; Vader, P.; van Dommelen, S.M.; van Solinge, W.W.; Schiffelers, R.M. Exosome mimetics: A novel class of drug delivery systems. Int. J. Nanomed 2012, 7, 1525–1541. [Google Scholar]
- Ma, Y.; Zhao, X.; Li, J.; Shen, Q. The comparison of different daidzein-PLGA nanoparticles in increasing its oral bioavailability. Int. J. Nanomed 2012, 7, 559–570. [Google Scholar]
- Kanwar, J.R.; Palmano, K.P.; Sun, X.; Kanwar, R.K.; Gupta, R.; Haggarty, N.; Rowan, A.; Ram, S.; Krissansen, G.W. “Iron-saturated” lactoferrin is a potent natural adjuvant for augmenting cancer chemotherapy. Immunol. Cell Biol 2008, 86, 277–288. [Google Scholar]
- Mack, C.A.; Song, W.R.; Carpenter, H.; Wickham, T.J.; Kovesdi, I.; Harvey, B.G.; Magovern, C.J.; Isom, O.W.; Rosengart, T.; Falck-Pedersen, E.; et al. Circumvention of anti-adenovirus neutralizing immunity by administration of an adenoviral vector of an alternate serotype. Hum. Gene Ther 1997, 8, 99–109. [Google Scholar]
- Parks, R.J.; Bramson, J.L.; Wan, Y.; Addison, C.L.; Graham, F.L. Effects of stuffer DNA on transgene expression from helper-dependent adenovirus vectors. J. Virol 1999, 73, 8027–8034. [Google Scholar]
- Otake, K.; Ennist, D.L.; Harrod, K.; Trapnell, B.C. Nonspecific inflammation inhibits adenovirus-mediated pulmonary gene transfer and expression independent of specific acquired immune responses. Hum. Gene Ther 1998, 9, 2207–2222. [Google Scholar]
- Belur, L.R.; Frandsen, J.L.; Dupuy, A.J.; Ingbar, D.H.; Largaespada, D.A.; Hackett, P.B.; Scott McIvor, R. Gene insertion and long-term expression in lung mediated by the Sleeping Beauty transposon system. Mol. Ther 2003, 8, 501–507. [Google Scholar]
| Author | Gene | Evaluation | Toxicity | Protection | Inhalation Mode | Subjects | Reference |
|---|---|---|---|---|---|---|---|
| Hasenpusch et al. (2011) | PEI-BC-819 | Histologic Bioluminescence | - | Inhalation Chamber | Nebulizer (spacer) | In Vitro In Vivo | [82] |
| Xu et al. (2008) | PEI + PEG Akt1 siRNA | BALF, LDH, IHC, Histologic, RTPCR, Western Blot | No toxicity | Nose only chamber | Aerosol | In Vivo | [93] |
| Jin et al. (2006) | UAC-PDCD4 | Western Blot, IHC, TUNEL | Low toxicity | Nose only chamber | Patent Nebulizer No. 20304964 | In Vitro In Vivo | [104] |
| Zou et al. (2012) | AND –p53sm | Weight, RT-PCR, extrusion precipitation | Dose dependent peribronchial inflammation | Accurately aerosol administration | Nebulizer | In Vitro In Vivo | [42] |
| Densmore et al. (2001) | PEI-p53/p53-CD(1-366) | Weight, histological, ELISA, IHC | No acute inflammatory response | Inhalation Chamber HEPA | Nebulizer + 5% CO2 | In Vitro | [61] |
| Gautam et al. (2000) | PEI-p53 | Histological, ELISA, weight | Low toxicity | Inhalation Chamber | Nebulizer + 5% CO2 | In Vitro In Vivo | [37] |
| Okamoto et al. (2011) | Chitosan-Interferon-β | Scanning electron microscope, histological, weight | - | Intratracheal | Dry powder | In vivo | [107] |
| Tehrani et al. (2011) | GPEI-Akt1WT or KD | Western Blot, IHC, histopathological, CC10 marker | Low toxicity, correlated with naphthalene | Nose only chamber | Patent Nebulizer No. 20304964 | In Vivo | [74] |
| Gautam et al. (2002) | PEI-p53 | IHC, CAT IHV, vWF, VEGF-TSP-1 ELISA | - | Inhalation Chamber | Nebulizer + 5% CO2 | In Vitro In Vivo | [42] |
| Tehrani et al. (2007) | GPEI-Akt1WT or KD | Western blot, IHC, Luciferase | Low toxicity | Nose only chamber | Patent Nebulizer No. 20304964 | In Vivo | [90] |
| Kim et al.(2004) | GPEI-pcDNA3.0-PTEN | Western blot, IHC, Detection of Apoptosis, Immuno-precipitation and Kinase assays, TUNEL, GFP expression | Low toxicity | Nose only chamber | Patent Nebulizer No. 20304964 | In Vivo | [41] |
| Koshkina et al. (2003) | PEI-p53 | Southern Blot analysis, Andersen cascade impactor, RT-PCR, Genomic DNA isolation | Low toxicity | Inhalation Chamber | Nebulizer + 5% CO2 | In Vivo | [81] |
| Hwang et al.(2007) | GPEI-PDCD4 | Western Blot, IHC, TUNEL | Low toxicity | Nose only chamber | Patent Nebulizer No. 20304964 | In Vivo | [91] |
| Frederiksen et al. (2000) | EGF-DNA complex | Receptor binding studies, Transfection experiments | - | - | - | In Vitro | [40] |
| Zamora-Avila et al. (2009) | PEI-RNA WT-1,2 | RT-PCR, TUNEL, histology, weight | Low toxicity | Nose only chamber | Micro-mist Nebulizer | In Vivo | [38] |
| Jere et al. (2008) | PAE-shRNA (Akt1) | EFTEM, FACS, confocal Microscopy, Western Blot, RT-PCR | PAE Low toxicity vs. PEI | - | aerosol | In Vitro In Vivo | [92] |
| Densmore (2003) | Review | Review | Review | Review | Review | Review | [39] |
| Topical Gautam et al. (2003) | PEI-CAT | CAT, Luciferase, Histological, IHC, MPO, BALF | Toxicity concerns Presented for personnel and mice | Inhalation Chamber | Nebulizer + 5% CO2 | In Vivo | [64] |
| Gautam et al. (2003) | PEI-p53CD(1-366) | IHC, ELISA, Tumor growth | - | Inhalation Chamber | Nebulizer + 5% CO2 | In Vivo | [63] |
| Davies et al. (2008) | pCIKLux/PEI (cPEI) | BALF, Histological, Luciferase, GFP expression, Electron microscopy | Hunching, Pronounced piloerection, Weight loss 5-10%, Foci of interstitial inflammation, Hemorrhage, Necrosis | Inhalation Chamber | Nebulizer + 5% CO2/Instillation | In Vivo | [62] |
| Gautam et al. (2001) | PEI-DNA BGTC:DOPE-DNA DOTAP-Chol:DNA | TNF-a, IL-1β, MPO, PMN, Histology, Elisa, Weight, Luciferase, MPO, BALF | No Toxicity | Inhalation Chamber | Nebulizer + 5% CO2 | In Vivo | [34] |
| Dong et al. (2007) | siRNA IGF-IR PEI | RT-PCR, Western Blot, Flow Cytometry, Cell Proliferation, Apoptotic Detection, TUNEL | - | Intratumoral | Intratumoral | In Vivo | [70] |
| Xing et al. (1996) | Human type 5 adenovirus with a CMV promoter | Northern hybridization analysis, RT-PCR, BALF,, Cytology, Histology, Elisa | Severe fibrotic reactions infiltrates of mono-nuclear cells, neutrophils and eosinophils | None | Instillation | In Vivo | [97] |
| Duan et al. (2005) | PEI:IL-12 ± IFX | Elisa, Fas/FasL, IHC, CD31, bFGF, PCNA, weight | - | - | Intranasal | In Vivo | [83] |
| Yu et al. (2010) | shOPN (recombinant lentivirus) | Western blot, IHC, Wound healing assay, VEGF, MMP-2, MMP-9, CD44v6, PCNA | - | Nose only chamber | Intranasal | In Vivo | [21] |
| Kawabata et al. (2012) | dTAT, PEI- AT2R, TRAIL | RT-PCR, TUNEL, Ki-67, IHC, Histology | PEI toxicity, but not for dTAT vector | - | Intratracheally | In Vitro In Vivo | [71] |
| Richard-Fiardo et al. (2011) | Amphiphilic Copolymer 704/Fraktalkine (CS3CL1) | IHC,CAT, IL-6, BALF, Histology, Western blot, IL-12, NK cells | No histological abnormalities, increased IL-6 after 6 hours, Mononuclear infiltration In perivascularly and Peribronchial zones | - | Instillation, Microsprayer | In Vitro In Vivo | [96] |
| Jia et al. (2002) | PEI:IL-12 | Northern blot analysis, RT-PCR | Low toxicity | - | Intranasal instillation | In Vitro In Vivo | [88] |
| Jia et al. (2003) | PEI:IL-12 | RT-PCR, IHC | Low toxicity | Plastic cage, HEPA | Nebulizer + 5% CO2 | In Vitro In Vivo | [87] |
© 2012 by the authors; licensee Molecular Diversity Preservation International, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Zarogouldis, P.; Karamanos, N.K.; Porpodis, K.; Domvri, K.; Huang, H.; Hohenforst-Schimdt, W.; Goldberg, E.P.; Zarogoulidis, K. Vectors for Inhaled Gene Therapy in Lung Cancer. Application for Nano Oncology and Safety of Bio Nanotechnology. Int. J. Mol. Sci. 2012, 13, 10828-10862. https://doi.org/10.3390/ijms130910828
Zarogouldis P, Karamanos NK, Porpodis K, Domvri K, Huang H, Hohenforst-Schimdt W, Goldberg EP, Zarogoulidis K. Vectors for Inhaled Gene Therapy in Lung Cancer. Application for Nano Oncology and Safety of Bio Nanotechnology. International Journal of Molecular Sciences. 2012; 13(9):10828-10862. https://doi.org/10.3390/ijms130910828
Chicago/Turabian StyleZarogouldis, Paul, Nikos K. Karamanos, Konstantinos Porpodis, Kalliopi Domvri, Haidong Huang, Wolfgang Hohenforst-Schimdt, Eugene P. Goldberg, and Konstantinos Zarogoulidis. 2012. "Vectors for Inhaled Gene Therapy in Lung Cancer. Application for Nano Oncology and Safety of Bio Nanotechnology" International Journal of Molecular Sciences 13, no. 9: 10828-10862. https://doi.org/10.3390/ijms130910828