Variation within Variation: Comparison of 24-h Rhythm in Rodent Infarct Size between Ischemia Reperfusion and Permanent Ligation
Abstract
:1. Introduction
2. Results
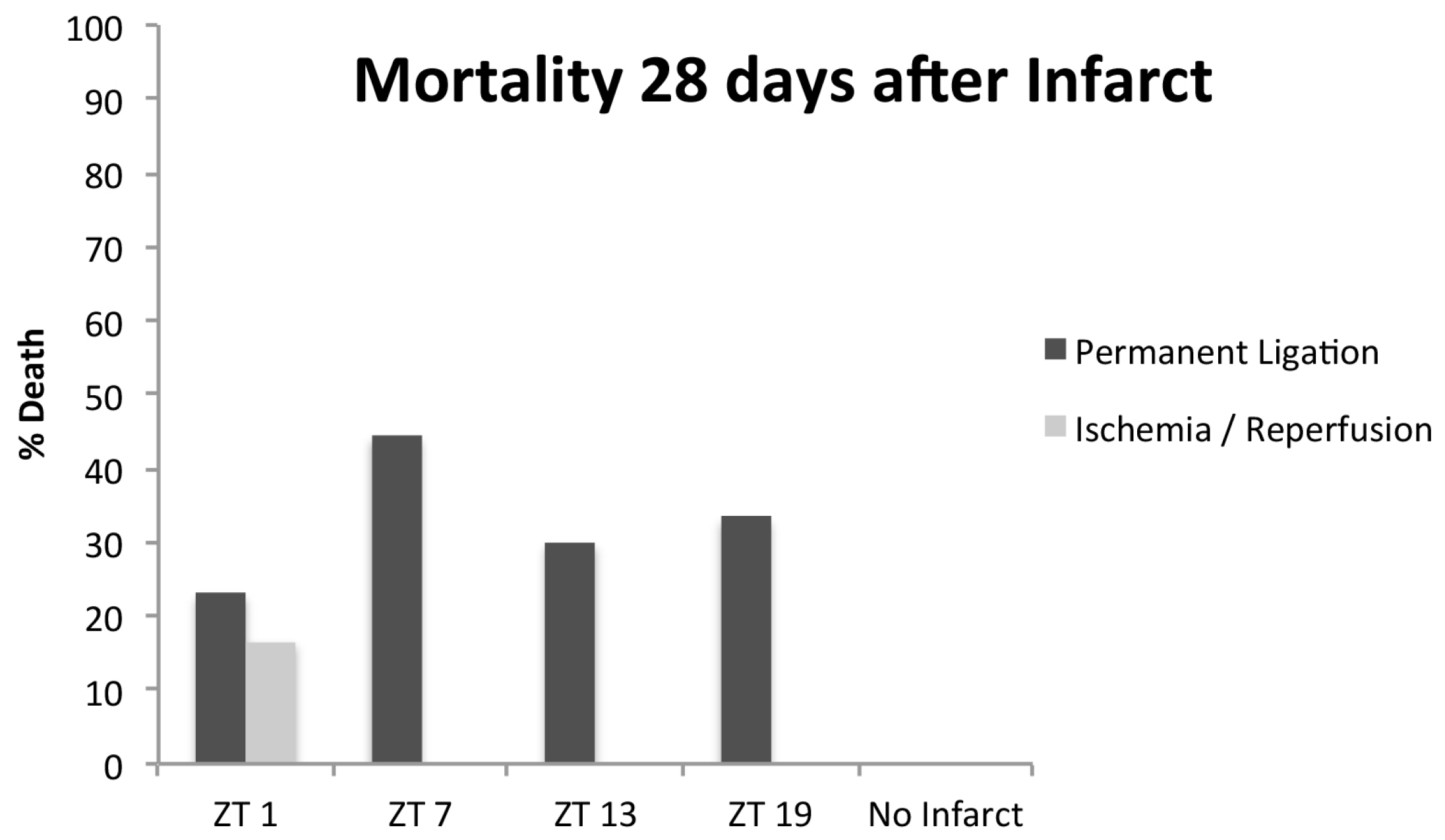
2.1. Operations
2.2. Body and Cardiac Weight
2.3. Echocardiography
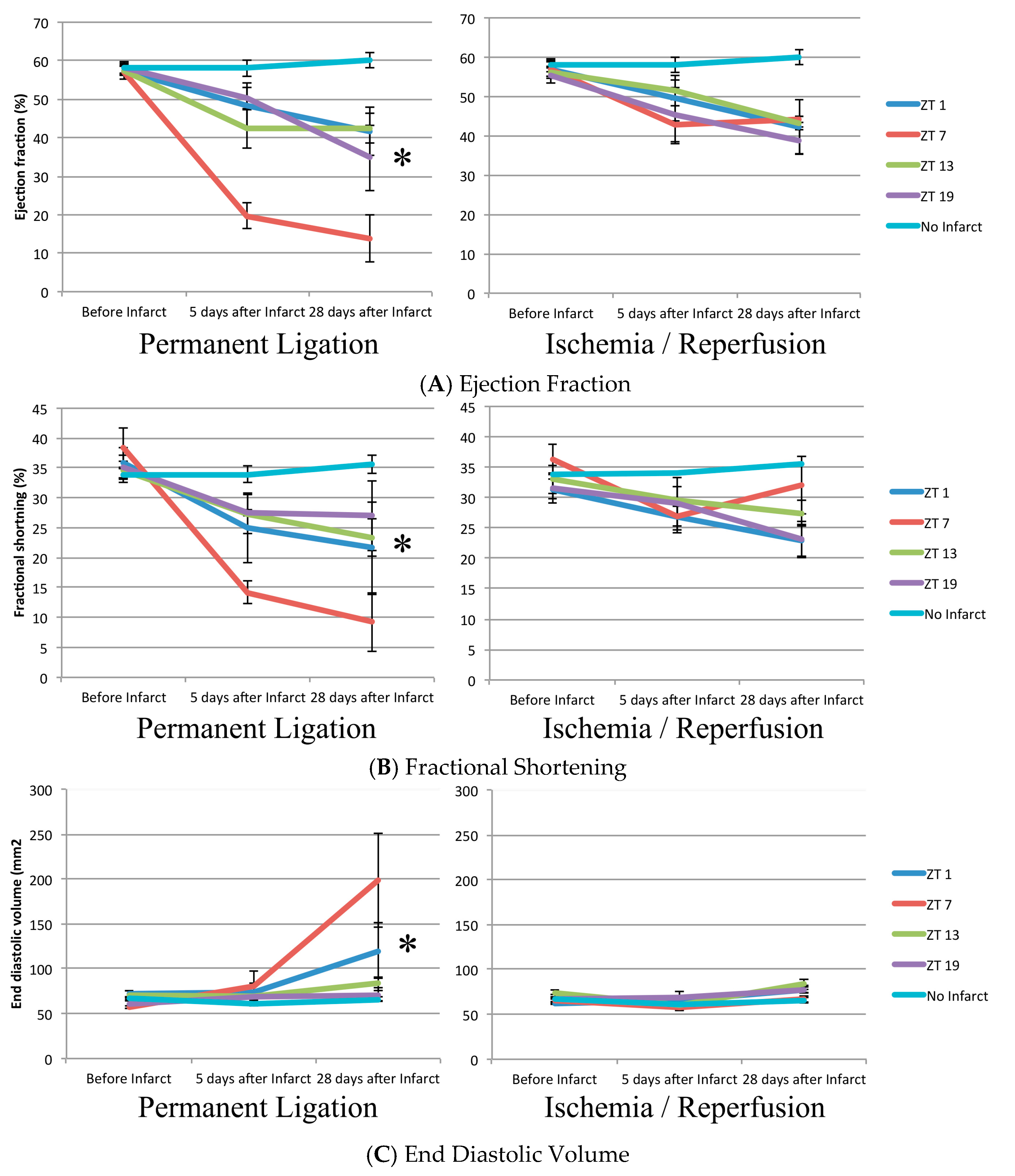
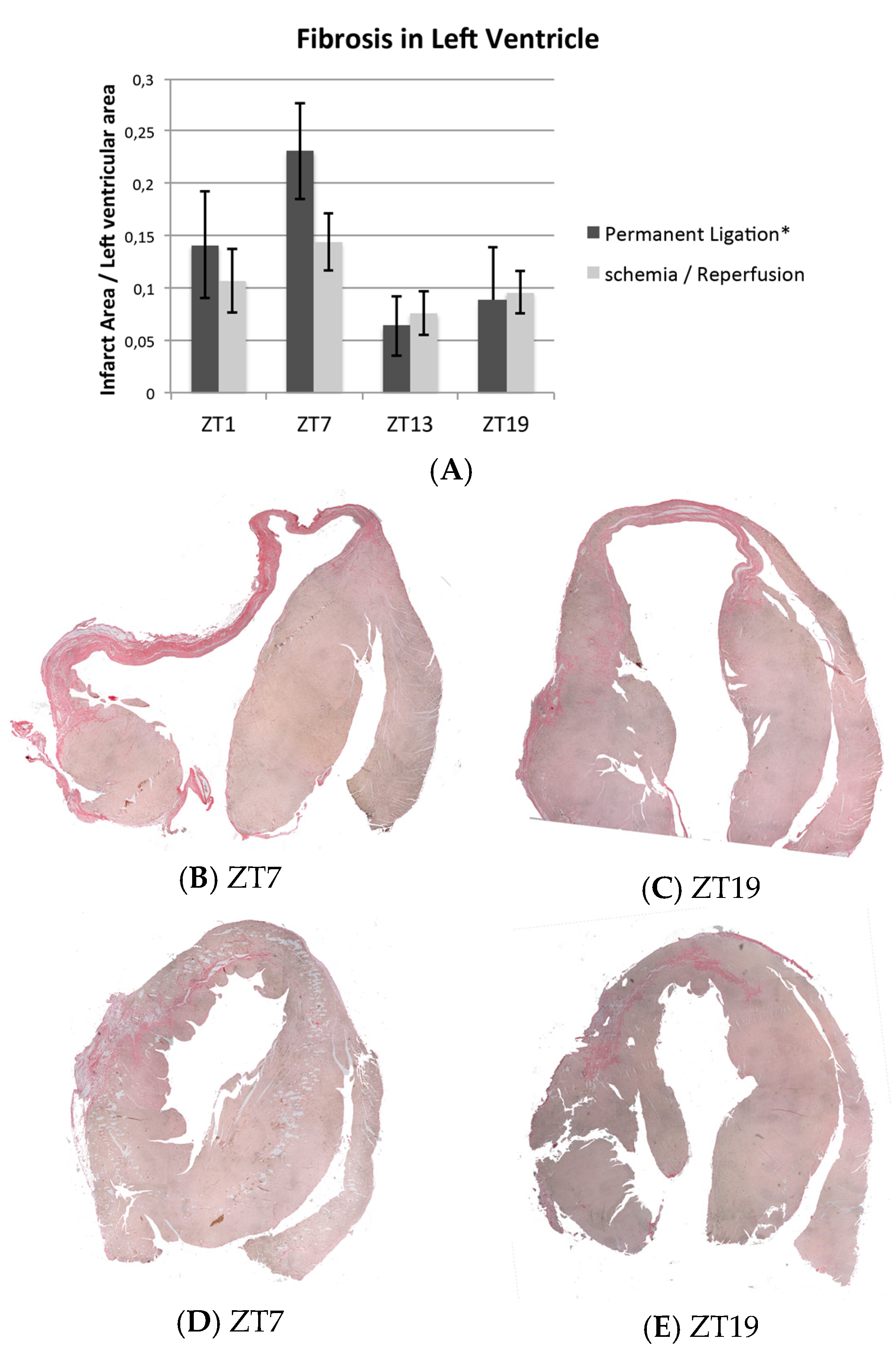
2.4. Histology
3. Discussion
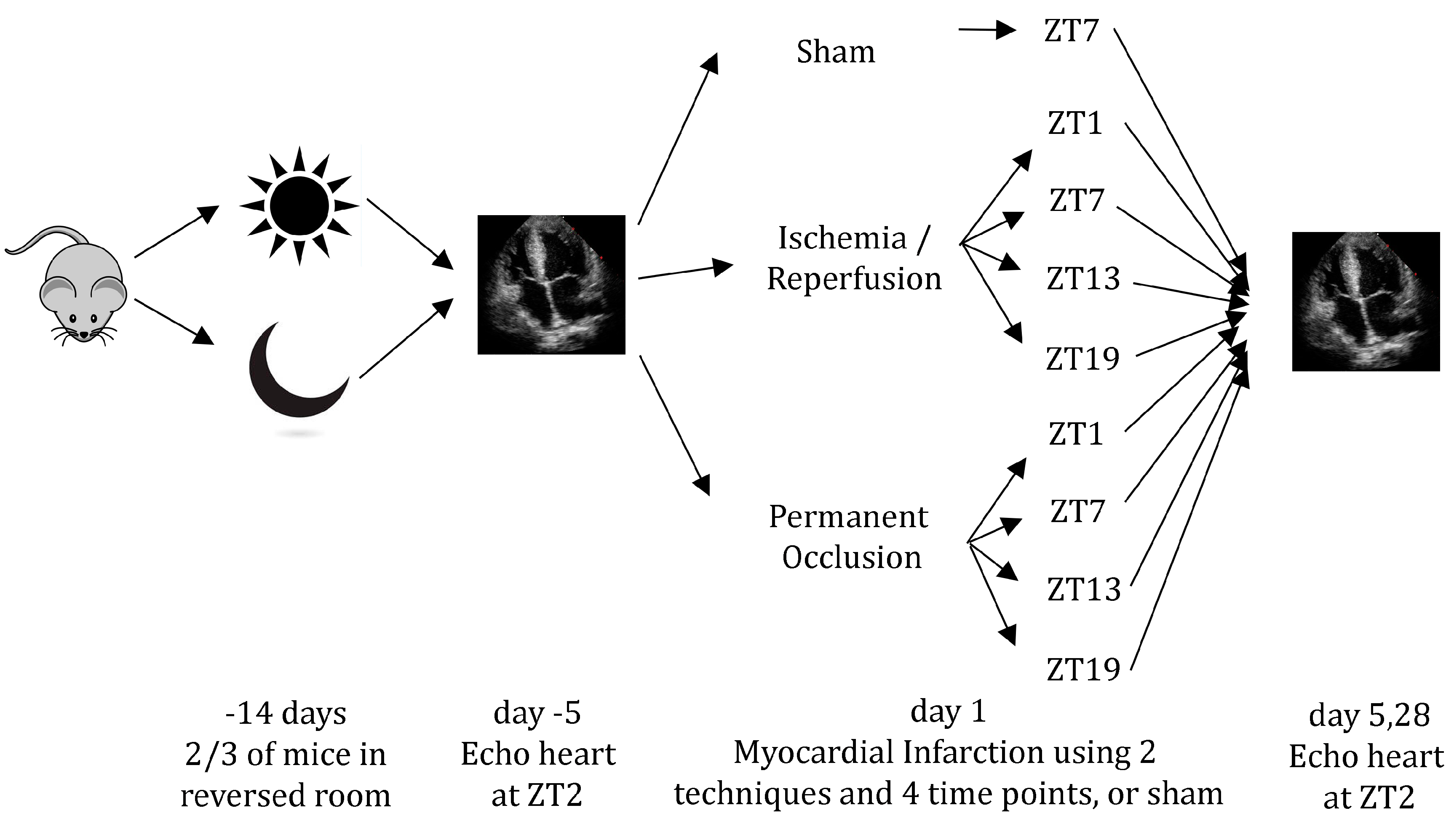
4. Materials and Methods
4.1. Animals
4.2. Myocardial Infarction
4.3. Echocardiography
4.4. Histology
4.5. Statistical Analysis
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| CVD | Cardiovascular disease |
| EDD | End Diastolic Diameter |
| EDV | End Diastolic Volume |
| ESD | End Systolic DIameter |
| ESV | End Systolic Volume |
| EF | Ejection Fraction |
| FS | Fractional Shortening |
| MI | Myocardial Infarction |
| IR | Ischemia/Reperfusion |
| PL | Permanent Ligation |
| ZT | Zeitgeber Time |
References
- Durgan, D.J.; Young, M.E. The cardiomyocyte circadian clock: Emerging roles in health and disease. Circ. Res. 2010, 106, 647–658. [Google Scholar] [CrossRef] [PubMed]
- Du Pre, B.C.; van Veen, T.A.; Young, M.E.; Vos, M.A.; Doevendans, P.A.; van Laake, L.W. Circadian rhythms in cell maturation. Physiology 2014, 29, 72–83. [Google Scholar] [CrossRef] [PubMed]
- Scheer, F.A.; Michelson, A.D.; Frelinger, A.L., 3rd; Evoniuk, H.; Kelly, E.E.; McCarthy, M.; Doamekpor, L.A.; Barnard, M.R.; Shea, S.A. The human endogenous circadian system causes greatest platelet activation during the biological morning independent of behaviors. PLoS ONE 2011, 6, e24549. [Google Scholar] [CrossRef] [PubMed]
- Reppert, S.M.; Weaver, D.R. Coordination of circadian timing in mammals. Nature 2002, 418, 935–941. [Google Scholar] [CrossRef] [PubMed]
- Vyas, M.V.; Garg, A.X.; Iansavichus, A.V.; Costella, J.; Donner, A.; Laugsand, L.E.; Janszky, I.; Mrkobrada, M.; Parraga, G.; Hackam, D.G. Shift work and vascular events: Systematic review and meta-analysis. BMJ 2012, 345, e4800. [Google Scholar] [CrossRef] [PubMed]
- Muller, J.E.; Tofler, G.H.; Stone, P.H. Circadian variation and triggers of onset of acute cardiovascular disease. Circulation 1989, 79, 733–743. [Google Scholar] [CrossRef] [PubMed]
- Durgan, D.J.; Pulinilkunnil, T.; Villegas-Montoya, C.; Garvey, M.E.; Frangogiannis, N.G.; Michael, L.H.; Chow, C.W.; Dyck, J.R.; Young, M.E. Short communication: Ischemia/reperfusion tolerance is time-of-day-dependent: Mediation by the cardiomyocyte circadian clock. Circ. Res. 2010, 106, 546–550. [Google Scholar] [CrossRef] [PubMed]
- Eckle, T.; Hartmann, K.; Bonney, S.; Reithel, S.; Mittelbronn, M.; Walker, L.A.; Lowes, B.D.; Han, J.; Borchers, C.H.; Buttrick, P.M.; et al. Adora2b-elicited Per2 stabilization promotes a HIF-dependent metabolic switch crucial for myocardial adaptation to ischemia. Nat. Med. 2012, 18, 774–782. [Google Scholar] [CrossRef] [PubMed]
- Schloss, M.J.; Horckmans, M.; Nitz, K.; Duchene, J.; Drechsler, M.; Bidzhekov, K.; Scheiermann, C.; Weber, C.; Soehnlein, O.; Steffens, S. The time-of-day of myocardial infarction onset affects healing through oscillations in cardiac neutrophil recruitment. EMBO Mol. Med. 2016, 8, 937–948. [Google Scholar] [CrossRef] [PubMed]
- Arroyo Ucar, E.; Dominguez-Rodriguez, A.; Abreu-Gonzalez, P. Influence of diurnal variation in the size of acute myocardial infarction. Med. Intensiva 2012, 36, 11–14. [Google Scholar] [CrossRef] [PubMed]
- Ari, H.; Sonmez, O.; Koc, F.; Demir, K.; Alihanoglu, Y.; Ozdemir, K.; Vatankulu, M.A. Circadian rhythm of infarct size and left ventricular function evaluated with tissue doppler echocardiography in ST elevation myocardial infarction. Heart Lung Circ. 2016, 25, 250–256. [Google Scholar] [CrossRef] [PubMed]
- Suarez-Barrientos, A.; Lopez-Romero, P.; Vivas, D.; Castro-Ferreira, F.; Nunez-Gil, I.; Franco, E.; Ruiz-Mateos, B.; Garcia-Rubira, J.C.; Fernandez-Ortiz, A.; Macaya, C.; et al. Circadian variations of infarct size in acute myocardial infarction. Heart 2011, 97, 970–976. [Google Scholar] [CrossRef] [PubMed]
- Seneviratna, A.; Lim, G.H.; Devi, A.; Carvalho, L.P.; Chua, T.; Koh, T.H.; Tan, H.C.; Foo, D.; Tong, K.L.; Ong, H.Y.; et al. Circadian dependence of infarct size and acute heart failure in ST elevation myocardial infarction. PLoS ONE 2015, 10, e0128526. [Google Scholar] [CrossRef] [PubMed]
- Reiter, R.; Swingen, C.; Moore, L.; Henry, T.D.; Traverse, J.H. Circadian dependence of infarct size and left ventricular function after st elevation myocardial infarction. Circ. Res. 2012, 110, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Fournier, S.; Eeckhout, E.; Mangiacapra, F.; Trana, C.; Lauriers, N.; Beggah, A.T.; Monney, P.; Cook, S.; Bardy, D.; Vogt, P.; et al. Circadian variations of ischemic burden among patients with myocardial infarction undergoing primary percutaneous coronary intervention. Am. Heart J. 2012, 163, 208–213. [Google Scholar] [CrossRef] [PubMed]
- Ammirati, E.; Cristell, N.; Cianflone, D.; Vermi, A.C.; Marenzi, G.; de Metrio, M.; Uren, N.G.; Hu, D.; Ravasi, T.; Maseri, A.; et al. Questing for circadian dependence in ST-segment-elevation acute myocardial infarction: A multicentric and multiethnic study. Circ. Res. 2013, 112, e110–e114. [Google Scholar] [CrossRef] [PubMed]
- Ibanez, B.; Suarez-Barrientos, A.; Lopez-Romero, P. Circadian variations of infarct size in STEM1. Circ. Res. 2012, 110, e22. [Google Scholar] [CrossRef] [PubMed]
- Traverse, J.H. Of mice and men: The quest to determine a circadian basis for myocardial protection in ischemia/reperfusion injury. Circ. Res. 2013, 112, e115–e117. [Google Scholar] [CrossRef] [PubMed]
- Ammirati, E.; Maseri, A.; Cannistraci, C.V. Still need for compelling evidence to support the circadian dependence of infarct size after st-elevation myocardial infarction. Circ. Res. 2013, 113, e43–e44. [Google Scholar] [CrossRef] [PubMed]
- Fournier, S.; Taffe, P.; Muller, O. Ischemic burden in st elevation myocardial infarction and circadian rhythms. Circ. Res. 2013, 113, e42. [Google Scholar] [CrossRef] [PubMed]
- Mukamal, K.J.; Muller, J.E.; Maclure, M.; Sherwood, J.B.; Mittleman, M.A. Increased risk of congestive heart failure among infarctions with nighttime onset. Am. Heart J. 2000, 140, 438–442. [Google Scholar] [CrossRef] [PubMed]
- Virag, J.A.; Anderson, E.J.; Kent, S.D.; Blanton, H.D.; Johnson, T.L.; Moukdar, F.; DeAntonio, J.H.; Thayne, K.; Ding, J.M.; Lust, R.M. Cardioprotection via preserved mitochondrial structure and function in the mPer2-mutant mouse myocardium. Am. J. Physiol. Heart Circ. Physiol 2013, 305, H477–H483. [Google Scholar] [CrossRef] [PubMed]
- Burgoyne, J.R.; Mongue-Din, H.; Eaton, P.; Shah, A.M. Redox signaling in cardiac physiology and pathology. Circ. Res. 2012, 111, 1091–1106. [Google Scholar] [CrossRef] [PubMed]
- Eckle, T.; Grenz, A.; Kohler, D.; Redel, A.; Falk, M.; Rolauffs, B.; Osswald, H.; Kehl, F.; Eltzschig, H.K. Systematic evaluation of a novel model for cardiac ischemic preconditioning in mice. Am. J. Physiol. Heart Circ. Physiol. 2006, 291, H2533–H2540. [Google Scholar] [CrossRef] [PubMed]
- van Laake, L.W.; Passier, R.; Monshouwer-Kloots, J.; Nederhoff, M.G.; Ward-van Oostwaard, D.; Field, L.J.; van Echteld, C.J.; Doevendans, P.A.; Mummery, C.L. Monitoring of cell therapy and assessment of cardiac function using magnetic resonance imaging in a mouse model of myocardial infarction. Nat. Protoc. 2007, 2, 2551–2567. [Google Scholar] [CrossRef] [PubMed]
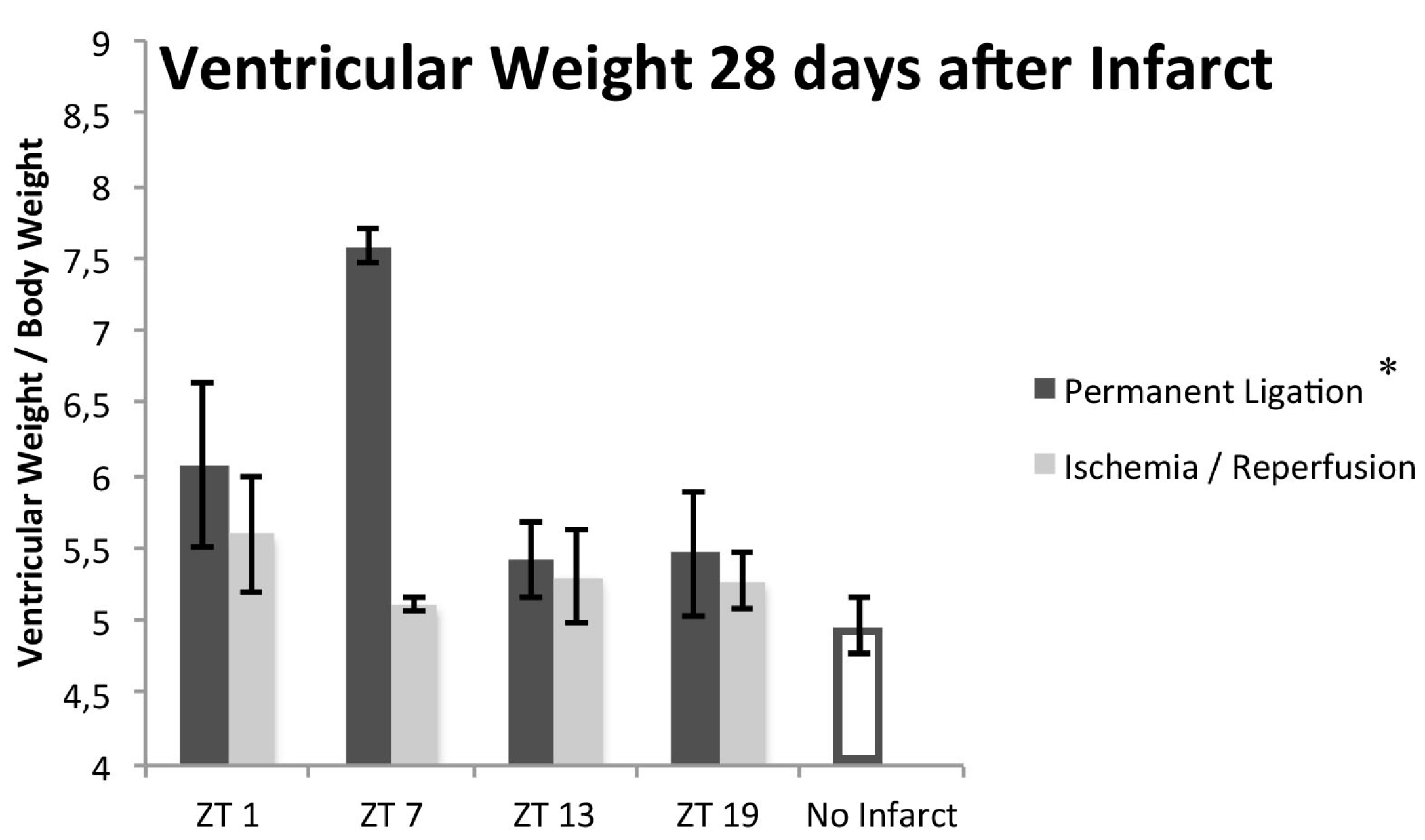
| Function | PL | IR | Sham | PL vs. Sham | IR vs. Sham |
|---|---|---|---|---|---|
| EF (%) | 31.8 ± 4.0 | 42.3 ± 1.6 | 60.4 ± 1.0 | p < 0.001 | p = 0.012 |
| FS (%) | 19.9 ± 2.6 | 26.5 ± 1.6 | 35.7 ± 1.4 | p < 0.001 | p = 0.014 |
| EDV (mL) | 118.1 ± 18.1 | 77.3 ± 2.9 | 64.1 ± 2.8 | 0.011 | 1.000 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Du Pré, B.; Van Veen, T.; Crnko, S.; Vos, M.; Deddens, J.; Doevendans, P.; Van Laake, L. Variation within Variation: Comparison of 24-h Rhythm in Rodent Infarct Size between Ischemia Reperfusion and Permanent Ligation. Int. J. Mol. Sci. 2017, 18, 1670. https://doi.org/10.3390/ijms18081670
Du Pré B, Van Veen T, Crnko S, Vos M, Deddens J, Doevendans P, Van Laake L. Variation within Variation: Comparison of 24-h Rhythm in Rodent Infarct Size between Ischemia Reperfusion and Permanent Ligation. International Journal of Molecular Sciences. 2017; 18(8):1670. https://doi.org/10.3390/ijms18081670
Chicago/Turabian StyleDu Pré, Bastiaan, Toon Van Veen, Sandra Crnko, Marc Vos, Janine Deddens, Pieter Doevendans, and Linda Van Laake. 2017. "Variation within Variation: Comparison of 24-h Rhythm in Rodent Infarct Size between Ischemia Reperfusion and Permanent Ligation" International Journal of Molecular Sciences 18, no. 8: 1670. https://doi.org/10.3390/ijms18081670





