An Overview of Recent Application of Medical Infrared Thermography in Sports Medicine in Austria
Abstract
:1. Introduction
2. International Status of Medical Infrared Imaging
3. Principles and Technique of Infrared Thermography
3.1. Electromagnetic Spectrum
- H (Planck’s constant) = 6.6256 × 10−34 Js
- K (Boltzmann’s constant) = 1.38054 × 10−23 WsK−1
- C (velocity of light in vacuum) = 2.9979 × 108 ms−1
- μ = wavelength in μm
- T = temperature in K
4. Infrared Radiation
- Conduction: the transfer of heat energy via tissue layer by contact between two bodies of different temperatures;
- Convection: the heat change between the skin and the surroundings; and
- Radiation: a transfer of heat that does not require a medium. The energy is transferred between two separate objects at different temperatures via electromagnetic waves (photons)
- Sweat Evaporation: which is the main mechanism for heat dissipation during exercise? The conversion of liquid into vapor allows the body to regulate its temperature. Evaporation results in a decrease of surface temperature.
4.1. The 21st Century Technique
4.2. Recommended Requirements for Human Medicine
- High Spatial resolution which reflects the separation between two nearby spots. A resolution of 320 (horizontal) × 240 (vertical) pixel is the minimum requirement. The spatial resolution is very dependent on image focusing.
- High Thermal resolution as an expression of sensitivity, defined as the minimum temperature difference that can be measured at two distinct spots.
- Medical CE certification is recommended: As soon as a temperature value in degree celcius is stated, the device is classified as a medical modality with a measuring function and should be signed by a specific CE approval.
- Narrow Calibration range accustomed to the human temperature range (i.e., 20–40 °C) assures more detailed temperature readings.
- Medical examination software including an export function, for medical analysis report and well-designed software tools for data analysis and image fusion (Figure 2).
5. Reliability Study
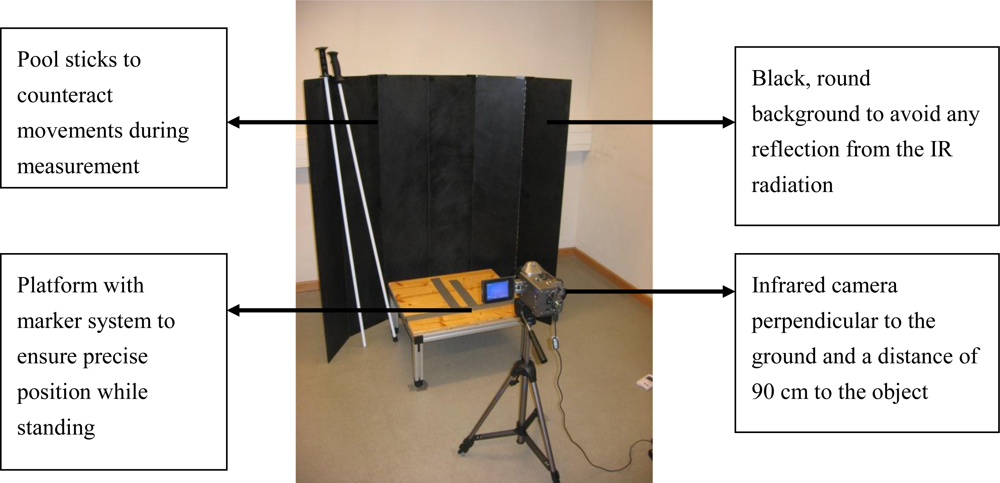
5.1. Methods of Reliability Study
5.2. Results
6. Clinical Application in Alpine Skiing
6.1. Methods
- Patient communication
- Patient preparation
- Patient assessment
- Examination guidelines
- Review of the imaging examination
- Presentation of the findings
- Exam time recommendation continuing professional education
- Name, age, sex
- Sport history including information about training performed in the previous 7 days
- Health status
- Nutritional status
- Menstrual cycle
6.2. Case Studies
6.2.1. Overuse Injuries
6.2.2. Traumatic Injuries
7. Limitations and Advantages of Infrared Imaging
8. Conclusions
References
- Melnizky, P.; Schartelmüller, T.; Ammer, K. Prüfung der intra- und interindividuellen Verlässlichkeit der Auswertung von Infrarot-Thermogrammen. Eur. J. Thermol 1997, 7, 224–226. [Google Scholar]
- Garagiola, U.; Giani, E. The use of telethermography in the management of sport injuries. Spo. Med 1990, 10, 267–272. [Google Scholar]
- Ishigaki, T.; Ikeda, M.; Asai, H.; Sakuma, S. Forehead back thermal ratio for the interpretation of infrared imaging of spinal cord lesions and other neurological disorders. Thermol. Int 1989, 3, 101–107. [Google Scholar]
- Kaczmarek, M.; Nowakowski, A.; Siebert, J.; Rogowski, J. Infrared thermography: applications in heart surgery. Proc. SPIE 1999, 3730, 184–188. [Google Scholar]
- Ammer, K. Diagnosis of raynaud's phenomenon by thermography. Skin Res. Tech 2006, 2, 182–185. [Google Scholar]
- Gulevich, S.J.; Conwell, T.D.; Lane, J.M.D.; Lockwood, B.M.D.; Schwettmann, R.S.; Rosenberg, N.; Goldman, L.B. Stress Infrared telethermography is useful in the diagnosis of complex regional pain syndrome. Clin. J. Pain 1997, 13, 50–59. [Google Scholar]
- Ng, W.K.; Eng, M.; Ng, E.Y.K.; Tan, Y.T. Qualitative study of sexual functioning in couples with erectile dysfunction: Prospective evaluation of the thermography diagnostic system. J. Reprod. Med 2009, 54, 698–705. [Google Scholar]
- Ng, E.Y.K.; Acharya, R. Remote-sensing infrared thermography. IEEE Eng. Med. Biol 2009, 28, 76–83. [Google Scholar]
- Head, J.F.; Elliot, R.L. Breast thermography. Cancer 1995, 79, 186–187. [Google Scholar]
- Ng, E.Y.K. A review of thermography as promising non-invasive detection modality for breast tumor. Int. J. Therm. Sci 2009, 48, 849–859. [Google Scholar]
- Head, J.F.; Wang, F.; Elliott, R. Breast thermography is a non-invasive prognostic procedure that predicts tumor growth rate in breast cancer patients. Ann. NY Acad. Sci 1993, 698, 153–158. [Google Scholar]
- Eliyahu, B. Infrared thermography and the sports injury practice. Dyn. Chiropr. 1992, 10, 27–28. [Google Scholar]
- Purohit, R.C.; McCoy, M.D. Thermography in the diagnosis of inflammatory processes in the horse. Am. J. Vet. Res 1980, 41, 1167–1168. [Google Scholar]
- Turner, T.A. Diagnostic thermography. Vet. Clin. North. Am. Equine Pract 2000, 17, 95–113. [Google Scholar]
- Eddy, A.L.; Van Hoogmoed, L.M.; Snyder, J.R. The role of Thermography in the Management of Equine Lameness. Vet. J 2001, 162, 172–181. [Google Scholar]
- Holmes, L.C.; Gaughan, E.M.; Gorondy, D.A.; Hogge, S.; Spire, M.F. The effect of perineural anesthesia on infrared thermographic images of the forelimb digits of normal horses. Can. Vet. J 2003, 44, 392–396. [Google Scholar]
- Davidson, T.M.; Laliotis, A.T. Alpine skiing injuries. A nine year study. West. J. Med 1996, 164, 310–314. [Google Scholar]
- Tecklenburg, K.; Smekal, V.; Hoser, C.; Raschner, C.; El, A.R.; Fink, C. Incidence and injury mechanism of anterior cruciate ligament injury in professional junior alpine skiers in Austria. In Abstract-Book of the 12th European Society of Sports Traumatology Knee Surgery and Arthroscopy; ESSKA: Innsbruck, Austria, May 23–27 2006; p. 159. [Google Scholar]
- Jiang, L.J.; Ng, E.Y.K.; Yeo, A.C.B.; Wu, S.; Pan, F.; Yau, W.Y.; Chen, J.H.; Yang, Y. A perspective on medical infrared imaging. J. Med. Eng. Tech 2005, 29, 257–267. [Google Scholar]
- Gold, J.E.; Cherniack, M.; Buchholz, B. Infrared thermography for examination of skin temperature in the dorsal hand of office workers. Eur. J. Appl. Physiol 2004, 93, 245–251. [Google Scholar]
- Kakuta, N.; Yokoyama, S.; Mabuchi, K. Human thermal models for evaluating infrared images. Eng. Med. Biol. Mag. IEEE 2002, 21, 65–72. [Google Scholar]
- Mercer, J.B. Infrared Thermal Imaging in Modern Medical Research- A Technique with Extensive Possibilities; The Kastelli Symposium: Oulu, Finland, 2000. [Google Scholar]
- Ammer, K. The Glamorgan Protocol for recording and evaluation of thermal images of the human body. Thermol. Int 2008, 18, 125–129. [Google Scholar]
- Buchlin, J.M. Convective heat transfer and infrared thermography. J. Appl. Fluid Mech 2010, 3, 55–62. [Google Scholar]
- Steketee, J. Spectral emissivity of skin and pericardium. Phys. Med. Biol 1973, 18, 686–694. [Google Scholar]
- Planck, M. On the law of distribution of energy in the normal spectrum. Ann. Phys 1901, 4, 553. [Google Scholar]
- Maldague, X.P.V.; Jones, T.S.; Kaplan, H.; Marinetti, S; Prystay, M. Fundamentals of Infrared and Thermal Testing. In Nondestructive Handbook, Infrared and Thermal Testing; ASNT Press: Columbus, OH, USA, 2001; p. 718. [Google Scholar]
- Xiaojiang, X.; Werner, J. A dynamic model of the human clothing environment system. Appl. Human Sci 1997, 16, 61–75. [Google Scholar]
- Elliott, R.L.; Head, J.F. Medical infrared imaging in the twenty-first century. Thermol. Int 1999, 9, 111. [Google Scholar]
- Diakides, N.A.; Diakides, M.; Lupo, J.C.; Paul, J.L.; Balcerak, R. Medical Infrared Imaging. In Advances in Medical Infrared Imaging; Diakides, N.A., Bronzino, J.D., Eds.; CRC Press: Boca Raton, FL, USA, 2008; pp. 1–13. [Google Scholar]
- Ring, E.F.J.; Ammer, K. The technique of infrared imaging in medicine. Thermol. Int 2000, 10, 7–14. [Google Scholar]
- Thomas, R.A. Reliability of Medical Thermography. Proceedings of Thermal Solutions Conference, Sarasota, FL, USA, January 23–26, 2006.
- Plassmann, P.; Murawski, P. CTHERM for standardized thermography. Proceedings of Abstracts, the 9th Congress of Thermology Poland, Krakow, Poland, May 29–June 1, 2003; pp. 27–29.
- Plassmann, P.; Ring, E.J.F.; Jones, C.D. Quality assurance of thermal imaging systems in medicine. Thermol. Int 2006, 16, 10–15. [Google Scholar]
- Mayr, H. Korrelation durchschnittlicher und maximaler Temperatur am Kniegelenk bei Auswertung unterschiedlicher Messareale. Thermol. Int 1995, 5, 89–91. [Google Scholar]
- Selfe, J.; Hardaker, N.; Thewlis, D.; Karki, A. An accurate and reliable method of thermal data analysis in thermal imaging of the anterior knee for use in cryotherapy research. Arch. Phys. Med. Rehabil 2006, 87, 1630–1635. [Google Scholar]
- Akata, T.; Kanna, T.; Yoshino, J.; Higashi, M.; Fukui, K.; Takahashi, S. Reliability of fingertip skin-surface temperature and its related thermal measures as indices of peripheral perfusion in the clinical setting of the operating theatre. Anaest. Intensive Care 2004, 32, 519–529. [Google Scholar]
- Kattapong, K.R.; Fogg, L.F.; Eastmann, C.I. Effect of Sex, Menstrual cycle phase and oral contraceptive use on circadian temperature rhythms. Chronobiol. Int 1995, 12, 257–266. [Google Scholar]
- Zaproudina, N.; Varmavuo, V.; Airaksinen, O.; Närhi, M. Reproducibility of infrared thermography measurements in healthy individuals. Physiol. Meas 2008, 29, 515–524. [Google Scholar]
- Hildebrandt, C.; Raschner, C. An intra-examiner reliability study of knee temperature patterns with medical infrared thermal imaging. Therm. Int 2009, 19, 73–77. [Google Scholar]
- Owens, E.F.; Hart, J.F.; Donofrio, J.J.; Haralambous, J.; Mierzejewski, E. Paraspinal skin temperature patterns: an inter-examiner and intra-examiner reliability study. J. Manipulative Physiol. Ther 2004, 27, 155–159. [Google Scholar]
- Vardasca, R. Symmetry of temperature distribution in the upper and lower extremities. Thermol. Int 2008, 18, 154–155. [Google Scholar]
- Selfe, J.; Whitaker, J.; Hardaker, N. A narrative literature review identifying the minimum clinically important difference for skin temperature asymmetry at the knee. Thermol. Int 2008, 18, 41–44. [Google Scholar]
- Koehle, M.S.; Lloyd-Smith, R.; Taunton, J.E. Alpine Ski Injuries and their prevention. Sports Med 2002, 32, 785–793. [Google Scholar]
- Bergstrom, K. Activity related knee injuries and pain in athletic adolescents. Knee Surgery, Sport Traumat. Arthros 2001, 9, 146–150. [Google Scholar]
- Ammer, K. Thermal Evaluation of Tennis Elbow. In The Thermal Image in Medicine and Biology; Ammer, K., Ring, E.J.F., Eds.; Uhlen Verlag Wien: Vienna, Austria, 1995; pp. 214–219. [Google Scholar]
- De Loes, M.; Dahlstedt, L.J.; Thomee, R. A 7-year on risks and costs of knee injuries in male and female youth participants in 12 sports. Scand J. Med. Sci. Sports 2000, 10, 90–97. [Google Scholar]
- Randall, W.V.; Steadman, J.R.; Mair, S.D.; Briggs, K.K.; Sterett, W.I. Anterior Cruciate Ligament Injury Incidence Among Male and Female Professional Alpine Skiers. Am. J. Sports Med 1999, 27, 792–795. [Google Scholar]
- Fisher, G.; Hoyt, G.L., III; Lamberth, J.G.; Joe, L.A.; Chromiak, J.A.; Chromiak, A.B.; Willard, S.T.; Ryan, P.L. Determination of the typical digital infrared thermographic profile of the knee of distance runners. Med. Sci. Sports Exer 2007, 39, 318. [Google Scholar]
- Ring, E.F.J.; Ammer, K. Thermal Imaging in sports medicine. Sport Med. Today 1998, 1, 108–109. [Google Scholar]
- Deng, Z.; Liu, J. Mathematical modelling of temperature mapping over skin surface and its implementation in thermal disease diagnostics. Comput. Bio. Med 2009, 34, 495–521. [Google Scholar]
- Zontak, A.; Sideman, S.; Verbitsky, O.; Beyar, R. Dynamic thermography: analysis of hand temperature during exercise. Ann. Biomed. Eng 1998, 26, 988–993. [Google Scholar]
- Ferreira, J.J.A.; Mendonc, L.C.S.; Nunes, A.C.C.; Andrade, F.; Rebelatto, J.R.; Salvini, T.F. Exercise associated thermographic changes in young and elderly subjects. Ann. Biomed. Eng 2008, 36, 1420–1427. [Google Scholar]
- Merla, A.; Romani, G.L. Functional infrared imaging in clinical applications. In The Biomedical Engineering Handbook; Bronzino, J.D., Ed.; CRC Press: New York, NY, USA, 2005; pp. 32.1–32.13. [Google Scholar]
- Merla, A.; Mattei, P.A.; Di Donato, L.; Romani, G.L. Thermal Imaging of cutaneous temperature modifications in runners during graded exercise. Ann. Biomed. Eng 2010, 38, 158–163. [Google Scholar]
- Schaefer, G.; Tait, R.; Zhu, S.Y. Overlay of thermal and visual image using skin detection and image registration. Eng. Med. Biol. Soc. (EMBS) 2006, 3, 965–967. [Google Scholar]
- Tait, R.J.; Schaefer, G.; Howell, K.; Hopgood, A.A.; Woo, P.; Harper, J. Automated overlay of visual and thermal medical image. Proceedings of the 18th International EURASIP Conference Biosignal, Brno, Czech Republic, June 28–30, 2006; pp. 260–262.





| OLD TECHNIQUE | NEW TECHNIQUE |
|---|---|
| Liquid detector cooling | Uncooled camera technology |
| Single element detector | Focal plane array detector |
| Slow mechanical scan mechanism | Real time, high-speed imaging with multi elements arrays |
| Low resolution camera | High-resolution camera |
| Analogue conversion and computing | Digital conversion and computing, electronic transfer of images from camera to PC in real time |
| No sufficient knowledge about standardization methods | Standardization protocols and recommendations for medical use |
| Gray shade images | Color visible images |
| Expensive, big in size, not mobile | Affordable, smaller and fully mobile |
| Predominantly low sensitivity | Improved sensitivity (0.02 degrees celcius) |
| Insufficient software and tools | User-friendly image processing software |
| Intra-examiner reliability of the mean Temperature (n = 15) | ||
|---|---|---|
| ICC | Rangea | |
| Right leg | 0.85 | 0.61–0.94 |
| Left leg | 0.75 | 0.41–0.90 |
| Affected knee | Non-affected knee | Temperature differences | |
|---|---|---|---|
| Mean | 32.8 (± 0.48) | 31.1 (± 0.32) | 1.4 (± 0.58) |
| Minimum | 31.4 (± 0.43) | 30.3 (± 0.41) | 0.8 (± 0.31) |
| Maximum | 33.4 (± 0.39) | 32.1 (± 0.60) | 1.3 (± 0.64) |
© 2010 by the authors; licensee MDPI, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license ( http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Hildebrandt, C.; Raschner, C.; Ammer, K. An Overview of Recent Application of Medical Infrared Thermography in Sports Medicine in Austria. Sensors 2010, 10, 4700-4715. https://doi.org/10.3390/s100504700
Hildebrandt C, Raschner C, Ammer K. An Overview of Recent Application of Medical Infrared Thermography in Sports Medicine in Austria. Sensors. 2010; 10(5):4700-4715. https://doi.org/10.3390/s100504700
Chicago/Turabian StyleHildebrandt, Carolin, Christian Raschner, and Kurt Ammer. 2010. "An Overview of Recent Application of Medical Infrared Thermography in Sports Medicine in Austria" Sensors 10, no. 5: 4700-4715. https://doi.org/10.3390/s100504700
APA StyleHildebrandt, C., Raschner, C., & Ammer, K. (2010). An Overview of Recent Application of Medical Infrared Thermography in Sports Medicine in Austria. Sensors, 10(5), 4700-4715. https://doi.org/10.3390/s100504700




