A Label-Free Immunosensor for Ultrasensitive Detection of Ketamine Based on Quartz Crystal Microbalance
Abstract
:1. Introduction
2. Experimental Section
2.1. Reagents and Materials
2.2. Apparatus
2.3. Fabrication of the Immunosensor
2.4. The Electrochemical Measurements
2.5. Detection of Ketamine in Urine Matrix
3. Results and Discussion
3.1. To Verify the Immunosensor Preparation

3.2. Effects of Immobilized KT-Ab Quantity on Sensing Performance

3.3. Responses of the Developed Immunosensor toward KT

| Concentration (pg/mL) | 1 | 5 | 10 | 15 | 20 | 30 | 40 |
| RSD (%) | 8.83 | 5.12 | 2.32 | 2.17 | 2.45 | 4.47 | 4.74 |
| Detection Method | LOD | Sample | The Linear Range | Reference |
|---|---|---|---|---|
| GC/MS | 10 ng/mL | Urine | 30–1000 ng/mL | [8] |
| LC-MS-MS | 5 ng/mL | Urine | 5–1000 ng/mL | [12] |
| electrochemistry | 5 ng/mL | Beverage | 50–2000 ng/mL | [16] |
| EIS | 0.1 pg/mL | Serum | 1–100 pmol/L | [17] |
| QCM | 0.86pg/mL | Urine | 1–40 pg/mL | Present work |
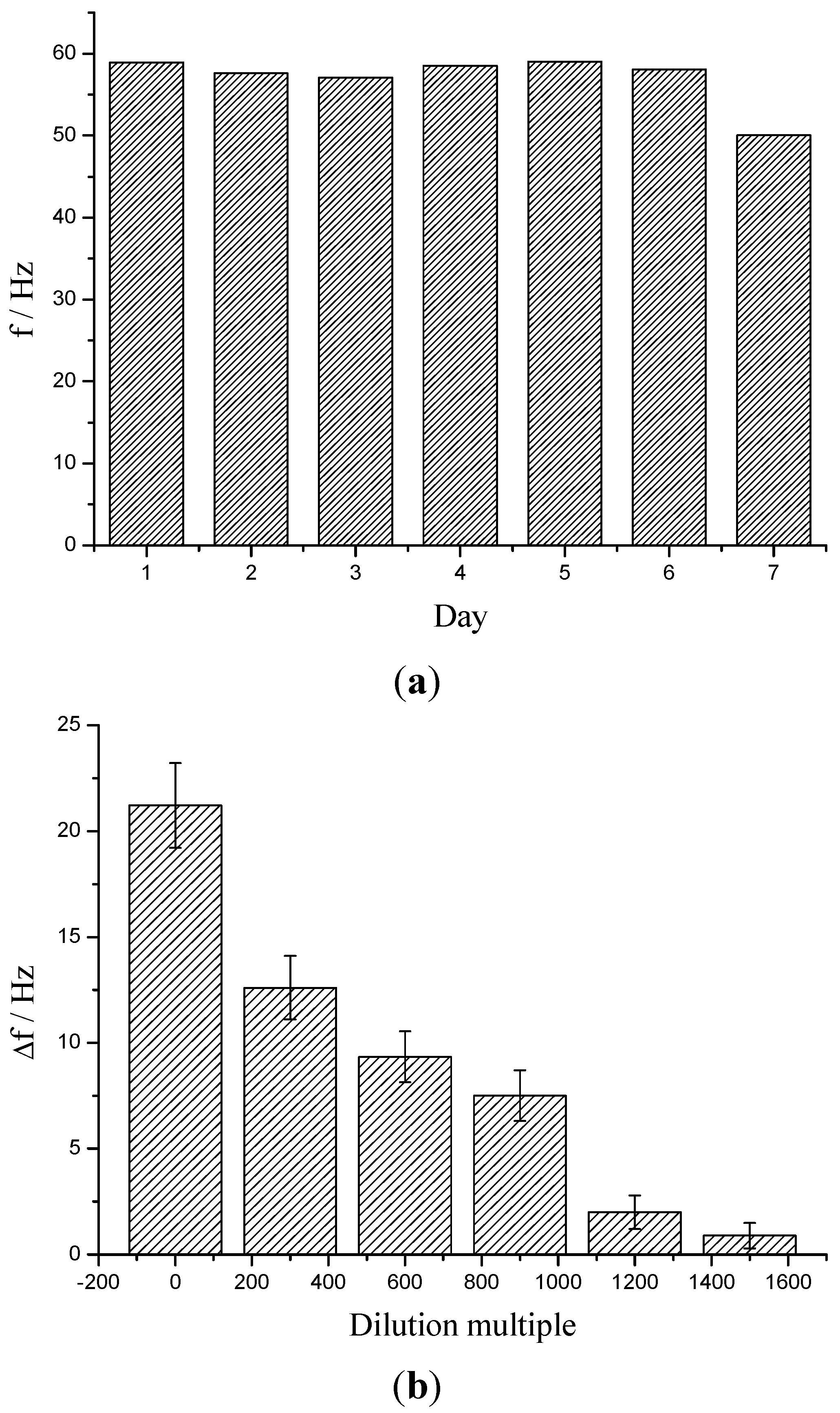
3.4. The Anti-Interference Ability and Stability of the Resulted Immunosensor
| Compound | Concentration (ng/mL) | Δf (Hz) | Influence (Relative Error) |
|---|---|---|---|
| urea | 50 | 0.04 | 0.14% |
| urea | 500 | 2.49 | 8.5% |
| uric acid | 50 | 1.02 | 3.5% |
| uric acid | 500 | 2.83 | 9.6% |
| ammonia | 50 | 0.32 | 1.1% |
| ammonia | 500 | 2.39 | 8.1% |
3.5. Determination of KT in Spiked Urine Sample
| In Spiked Sample (pg/mL) | After Dilution (pg/mL) | Δf (Hz) | Detected Concentration (pg/mL) | Recovery |
|---|---|---|---|---|
| 3,000 | 2.0 | 15.9 | 2.14 | 107% |
| 6,000 | 4.0 | 17.1 | 3.67 | 91.8% |
| 12,000 | 8.0 | 20.9 | 8.66 | 108% |
| 24,000 | 16.0 | 26.1 | 15.5 | 96.9% |
| 48,000 | 32.0 | 36.7 | 29.5 | 92.2% |
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Domino, E.F.; Chodoff, P.; Corssen, G. Pharmacologic Effects of Ci-581, a New Dissociative Anesthetic, in Man. Clin. Pharmacol. Ther. 1965, 6, 279–291. [Google Scholar] [PubMed]
- Hirota, K.; Lambert, D.G. Ketamine: Its mechanism(s) of action and unusual clinical uses. Br. J. Anaesth. 1996, 77, 441–444. [Google Scholar] [CrossRef] [PubMed]
- Fisher, K.; Coderre, T.J.; Hagen, N.A. Targeting the N-methyl-d-aspartate receptor for chronic pain management. Preclinical animal studies, recent clinical experience and future research directions. J. Pain Symptom Manag. 2000, 20, 358–373. [Google Scholar] [CrossRef]
- Jansen, K.L. A review of the nonmedical use of ketamine: Use, users and consequences. J. Psychoact. Drugs 2000, 32, 419–433. [Google Scholar] [CrossRef]
- Moreton, J.E.; Meisch, R.A.; Stark, L.; Thompson, T. Ketamine self-administration by the rhesus monkey. J. Pharmacol. Exp. Ther. 1977, 203, 303–309. [Google Scholar] [PubMed]
- Huang, M.H.; Wu, M.Y.; Wu, C.H.; Tsai, J.L.; Lee, H.H.; Liu, R.H. Performance characteristics of ELISAs for monitoring ketamine exposure. Clin. Chim. Acta Int. J. Clin. Chem. 2007, 379, 59–65. [Google Scholar] [CrossRef]
- Zhang, W.; Su, P.; Yang, Y.; Guo, Z. Development of a sensitive biotin-avidin amplified enzyme-linked immunosorbent assay for the determination of ketamine in biological samples. J. Immunoass. Immunochem. 2010, 31, 205–216. [Google Scholar] [CrossRef]
- Cheng, P.S.; Fu, C.Y.; Lee, C.H.; Liu, C.; Chien, C.S. GC-MS quantification of ketamine, norketamine, and dehydronorketamine in urine specimens and comparative study using ELISA as the preliminary test methodology. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2007, 852, 443–449. [Google Scholar] [CrossRef]
- Kim, E.M.; Lee, J.S.; Choi, S.K.; Lim, M.A.; Chung, H.S. Analysis of ketamine and norketamine in urine by automatic solid-phase extraction (SPE) and positive ion chemical ionization-gas chromatography-mass spectrometry (PCI-GC-MS). Forensic Sci. Int. 2008, 174, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Geisslinger, G.; Menzel-Soglowek, S.; Kamp, H.D.; Brune, K. Stereoselective high-performance liquid chromatographic determination of the enantiomers of ketamine and norketamine in plasma. J. Chromatogr. 1991, 568, 165–176. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.C.; Shih, T.S.; Cheng, S.G. Use of SPE and LC/TIS/MS/MS for rapid detection and quantitation of ketamine and its metabolite, norketamine, in urine. Forensic Sci. Int. 2005, 147, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.Y.; Mok, V.K. Rapid determination of ketamine in urine by liquid chromatography-tandem mass spectrometry for a high throughput laboratory. Forensic Sci. Int. 2004, 142, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Sergi, M.; Bafile, E.; Compagnone, D.; Curini, R.; D’Ascenzo, G.; Romolo, F.S. Multiclass analysis of illicit drugs in plasma and oral fluids by LC-MS/MS. Anal. Bioanal. Chem. 2009, 393, 709–718. [Google Scholar] [CrossRef] [PubMed]
- Gentili, S.; Cornetta, M.; Macchia, T. Rapid screening procedure based on headspace solid-phase microextraction and gas chromatography-mass spectrometry for the detection of many recreational drugs in hair. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2004, 801, 289–296. [Google Scholar] [CrossRef]
- Sporkert, F.; Pragst, F. Use of headspace solid-phase microextraction (HS-SPME) in hair analysis for organic compounds. Forensic Sci. Int. 2000, 107, 129–148. [Google Scholar] [CrossRef] [PubMed]
- Lledo-Fernandez, C.; Pollard, P.; Kruanetr, S. Electroanalytical Sensing of Ketamine Using Electrogenerated Chemiluminescence. J. Electrochem. Soc. 2014, 161, H36–H40. [Google Scholar] [CrossRef]
- Chen, Y.; Yang, Y.; Tu, Y.F. An electrochemical impedimetric immunosensor for ultrasensitive determination of ketamine hydrochloride. Sens. Actuators B Chem. 2013, 183, 150–156. [Google Scholar] [CrossRef]
- Zhou, J.; Xu, Y.; Wang, L.; Liu, J.; Li, Y.M.; Ye, B.X. Electrochemical Behavior and Voltammetric Determination of Ketamine at Pulse Plating Gold Film Modified Platinum Electrode. J. Chin. Chem. Soc. Taip. 2012, 59, 879–883. [Google Scholar] [CrossRef]
- Ionescu, R.E.; Jaffrezic-Renault, N.; Bouffier, L.; Gondran, C.; Cosnier, S.; Pinacho, D.G.; Marco, M.P.; Sanchez-Baeza, F.J.; Healy, T.; Martelet, C. Impedimetric immunosensor for the specific label free detection of ciprofloxacin antibiotic. Biosens. Bioelectron. 2007, 23, 549–555. [Google Scholar] [CrossRef] [PubMed]
- Paddle, B.M. Biosensors for chemical and biological agents of defence interest. Biosens. Bioelectron. 1996, 11, 1079–1113. [Google Scholar] [CrossRef]
- Kim, J.H.; Cho, S.; Bae, T.S.; Lee, Y.S. Enzyme biosensor based on an N-doped activated carbon fiber electrode prepared by a thermal solid-state reaction. Sens. Actuators B Chem. 2014, 197, 20–27. [Google Scholar] [CrossRef]
- Chen, X.J.; Zhang, K.; Zhou, J.J.; Xuan, J.; Yan, W.; Jiang, L.P.; Zhu, J.J. Electrochemical immunosensor based on colloidal carbon sphere array. Biosens. Bioelectron. 2010, 25, 1130–1136. [Google Scholar] [CrossRef] [PubMed]
- Tang, D.P.; Tang, J.; Su, B.L.; Ren, J.J.; Chen, G.N. Simultaneous determination of five-type hepatitis virus antigens in 5 min using an integrated automatic electrochemical immunosensor array. Biosens. Bioelectron. 2010, 25, 1658–1662. [Google Scholar] [CrossRef] [PubMed]
- Arya, S.K.; Prusty, A.K.; Singh, S.P.; Solanki, P.R.; Pandey, M.K.; Datta, M.; Malhotra, B.D. Cholesterol biosensor based on N-(2-aminoethyl)-3-aminopropyl-trimethoxysilane self-assembled monolayer. Anal. Biochem. 2007, 363, 210–218. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.; Zhang, Y.M.; Chen, H.; Chen, Z.C.; Lin, X.F. Amperometric immunosensor for carcinoembryonic antigen detection with carbon nanotube-based film decorated with gold nanoclusters. Anal. Biochem. 2011, 414, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Sauerbrey, G. Verwendung Von Schwingquarzen Zur Wagung Dunner Schichten Und Zur Mikrowagung. Zeitschrift für Physik 1959, 155, 206–222. (In German) [Google Scholar] [CrossRef]
- Mannelli, I.; Minunni, M.; Tombelli, S.; Mascini, M. Quartz crystal microbalance (QCM) affinity biosensor for genetically modified organisms (GMOs) detection. Biosens. Bioelectron. 2003, 18, 129–140. [Google Scholar] [CrossRef] [PubMed]
- Michalzik, M.; Wendler, J.; Rabe, J.; Buttgenbach, S.; Bilitewski, U.B. Development and application of a miniaturised quartz crystal microbalance (QCM) as immunosensor for bone morphogenetic protein-2. Sens. Actuators B Chem. 2005, 105, 508–515. [Google Scholar] [CrossRef]
- Park, I.S.; Kim, W.Y.; Kim, N. Operational characteristics of an antibody-immobilized QCM system detecting Salmonella spp. Biosens. Bioelectron. 2000, 15, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Mao, Q.G.; Zhang, X.; Jiang, T.L.; Chen, M.; Yu, F.; Fu, W.L. A novel piezoelectric quartz micro-array immunosensor based on self-assembled monolayer for determination of human chorionic gonadotropin. Biosens. Bioelectron. 2004, 19, 711–720. [Google Scholar] [CrossRef]
- De Oliveira, F.C.M.; Serrano, S.H.P. Electrochemically Active L-Cysteine Gold Modified Electrodes. Electrochim. Acta 2014, 125, 566–572. [Google Scholar] [CrossRef]
- Rajesh; Sharma, V.; Mishra, S.K.; Biradar, A.M. Synthesis and electrochemical characterization of myoglobin-antibody protein immobilized self-assembled gold nanoparticles on ITO-glass plate. Mater. Chem. Phys. 2012, 132, 22–28. [Google Scholar] [CrossRef]
- Rajesh; Sharma, V.; Tanwar, V.K.; Mishra, S.K.; Biradar, A.M. Electrochemical impedance immunosensor for the detection of cardiac biomarker Myogobin (Mb) in aqueous solution. Thin Solid Films 2010, 519, 1167–1170. [Google Scholar]
- Limbut, W.; Kanatharana, P.; Mattiasson, B.; Asawatreratanakul, P.; Thavarungkul, P. A comparative study of capacitive immunosensors based on self-assembled monolayers formed from thiourea, thioctic acid, and 3-mercaptopropionic acid. Biosens. Bioelectron. 2006, 22, 233–240. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, Y.; Tu, Y.; Wang, X.; Pan, J.; Ding, Y. A Label-Free Immunosensor for Ultrasensitive Detection of Ketamine Based on Quartz Crystal Microbalance. Sensors 2015, 15, 8540-8549. https://doi.org/10.3390/s150408540
Yang Y, Tu Y, Wang X, Pan J, Ding Y. A Label-Free Immunosensor for Ultrasensitive Detection of Ketamine Based on Quartz Crystal Microbalance. Sensors. 2015; 15(4):8540-8549. https://doi.org/10.3390/s150408540
Chicago/Turabian StyleYang, Ya, Yifeng Tu, Xiaoshu Wang, Jinyin Pan, and Yun Ding. 2015. "A Label-Free Immunosensor for Ultrasensitive Detection of Ketamine Based on Quartz Crystal Microbalance" Sensors 15, no. 4: 8540-8549. https://doi.org/10.3390/s150408540





