A Low-Power and Portable Biomedical Device for Respiratory Monitoring with a Stable Power Source
Abstract
:1. Introduction

2. Innovative Respiratory Monitoring System
2.1. Design of the Biomedical Module


2.2. Gas Flow Measurement Module

2.3. CO Concentration Measurement Module



3. Methods
3.1. Power Analysis of the Circuits

3.2. Fluctuation Analysis of Sensors

4. Results and Discussion
4.1. Analysis of Stable Power

4.2. Analysis of the Drive of the Pressure Sensor
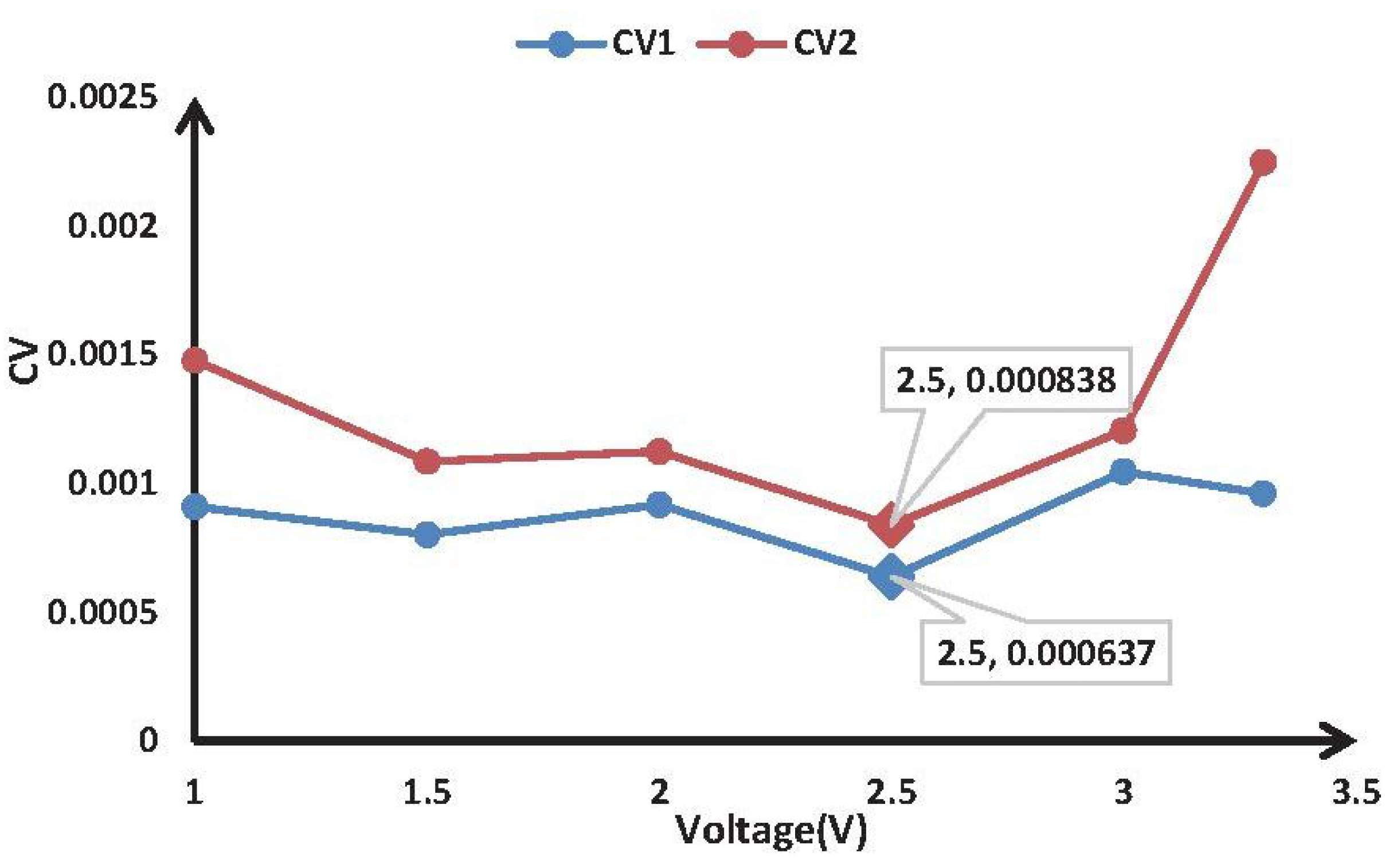
| Voltage (V) | 1 V | 1.5 V | 2 V | 2.5 V | 3 V | 3.3 V |
|---|---|---|---|---|---|---|
| CV 1 | 0.00091 | 0.000802 | 0.000918 | 0.000637 | 0.001046 | 0.000961 |
| CV 2 | 0.001479 | 0.001086 | 0.001124 | 0.000838 | 0.001206 | 0.002249 |
4.3. Analysis of Power Consumption
4.4. Analysis of Stability of Device




5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Zhu, Z.; Liu, T.; Li, G.; Li, T.; Inoue, Y. Wearable sensor systems for infants. Sensors 2015, 15, 3721–3749. [Google Scholar] [CrossRef] [PubMed]
- Heines, S.J.; Strauch, U.; Roekaerts, P.M.; Winkens, B.; Bergmans, D.C. Accuracy of End-Tidal CO2 Capnometers in Post-Cardiac Surgery Patients During Controlled Mechanical Ventilation. J. Emerg. Med. 2013, 45, 130–135. [Google Scholar] [CrossRef] [PubMed]
- Jaffe, M.B.; Orr, J. Continuous Monitoring of Respiratory Flow and CO2. IEEE Eng. Med. Biol. Mag. 2010, 29, 44–52. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Wang, B.; Xu, R.; Wang, L. A new real-time and precision capnography for human respiration carbon dioxide concentration. Perfusion 2010, 25, 399–408. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Wang, B.; Fan, C.; Wang, L. A new single-end mainstream CO2 capnograph. Comput. Methods Biomechan. Biomed. Eng. 2011, 14, 1033–1039. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Wang, H.; Wang, B.; Wang, L. Accurate and stable continuous monitoring module by mainstream capnography. J. Clin. Monit. Comput. 2014, 28, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Wang, H.; Chen, B.; Wang, B.; Wang, L. Use of signal decomposition to compensate for respiratory disturbance in mainstream capnometer. Appl. Opt. 2014, 53, 2145–2151. [Google Scholar] [CrossRef] [PubMed]
- Yasuda, T.; Yonemura, S.; Tani, A. Comparison of the characteristics of small commercial NDIR CO2 sensor models and development of a portable CO2 measurement device. Sensors 2012, 12, 3641–3655. [Google Scholar] [CrossRef] [PubMed]
- Howe, T.A.; Jaalam, K.; Ahmad, R.; Sheng, C.K.; Ab Rahman, N.H.N. The use of end-tidal capnography to monitor non-intubated patients presenting with acute exacerbation of asthma in the emergency department. J. Emerg. Med. 2011, 41, 581–589. [Google Scholar] [CrossRef] [PubMed]
- Schranz, C.; Becher, T.; Schädler, D.; Weiler, N.; Möller, K. Model-based setting of inspiratory pressure and respiratory rate in pressure-controlled ventilation. Physiol. Meas. 2014, 35, 383. [Google Scholar] [CrossRef] [PubMed]
- Sivaramakrishnan, S.; Rajamani, R.; Johnson, B.D. Dynamic model inversion techniques for breath-by-breath measurement of carbon dioxide from low bandwidth sensors. IEEE Sens. J. 2010, 10, 1637–1646. [Google Scholar] [CrossRef]
- Lovett, P.B.; Buchwald, J.M.; Stürmann, K.; Bijur, P. The vexatious vital: Neither clinical measurements by nurses nor an electronic monitor provides accurate measurements of respiratory rate in triage. Ann. Emerg. Med. 2005, 45, 68–76. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, N. Micromachined flow sensors—A review. Flow Meas. Instrum. 1997, 8, 7–16. [Google Scholar] [CrossRef]
- Silvestri, S.; Schena, E. Micromachined flow sensors in biomedical applications. Micromachines 2012, 3, 225–243. [Google Scholar] [CrossRef]
- Schena, E.; Massaroni, C.; Saccomandi, P.; Cecchini, S. Flow measurement in mechanical ventilation: A review. Med. Eng. Phys. 2015, 37, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Nakayama, M.; Yagi, M.; Nishikawa, M.; Fukunaga, M.; Watanabe, K. The NDIR CO2 monitor with smart interface for global networking. IEEE Trans. Instrum. Meas. 2005, 54, 1634–1639. [Google Scholar] [CrossRef]
- Xu, S.; Chen, M. Design and modeling of non-linear infrared transducer for measuring methane using cross-correlation method. IMEKO 2012, 45, 325–332. [Google Scholar] [CrossRef]
- Park, I.-Y.; Park, H.-J.; Lee, J.-W.; Kang, S.-W.; Cho, J.-H. A proposal of effective compensation method for IR lamp deterioration in NDIR type capnograph systems. IEICE Trans. Fundam. Electron. Commun. Comput. Sci. 2003, 86, 1513–1516. [Google Scholar]
- Antón, J.C.M.; Silva-López, M. Optical cavity for auto-referenced gas detection. Opt. Express 2011, 19, 26079–26087. [Google Scholar] [CrossRef] [PubMed]
- Berggren, M. Improved response time with a new miniaturised main-stream multigas monitor. JCMC 2009, 23, 355–361. [Google Scholar] [CrossRef] [PubMed]
- Cinar, O.; Acar, Y.A.; Arziman, İ.; Kilic, E.; Eyi, Y.E.; Ocal, R. Can mainstream end-tidal carbon dioxide measurement accurately predict the arterial carbon dioxide level of patients with acute dyspnea in ED. Am. J. Emerg. Med. 2012, 30, 358–361. [Google Scholar]
- Pekdemir, M.; Cinar, O.; Yilmaz, S.; Yaka, E.; Yuksel, M. Disparity Between Mainstream and Sidestream End Tidal Carbon Dioxide Values and Arterial Carbon Dioxide Levels. Respir. Care 2013. [Google Scholar] [CrossRef] [PubMed]
- Haque, S.A.; Rahman, M.; Aziz, S.M. Sensor Anomaly Detection in Wireless Sensor Networks for Healthcare. Sensors 2015, 15, 8764–8786. [Google Scholar] [CrossRef] [PubMed]
- Chipara, O.; Lu, C.; Bailey, T.C.; Roman, G.C. Reliable clinical monitoring using wireless sensor networks: experiences in a step-down hospital unit. In Proceedings of the 8th ACM Conference on Embedded Networked Sensor Systems, Zurich, Switzerland, 3–5 November 2010; pp. 155–168.
- Xie, Q.; Li, J.; Gao, X.; Jia, J. Fourier domain local narrow-band signal extraction algorithm and its application to real-time infrared gas detection. Sens. Actuators B Chem. 2010, 146, 35–39. [Google Scholar] [CrossRef]
- Yang, Y.; Gao, Z.; Zhong, D.; Lin, W. Detection of nitrogen dioxide using an external modulation diode laser. Appl. Opt. 2013, 52, 3027–3030. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, K.; Pignanelli, E.; Schutze, A. Versatile Gas Detection System Based on Combined NDIR Transmission and Photoacoustic Absorption Measurements. IEEE Sens. J. 2013, 13, 934–940. [Google Scholar] [CrossRef]
- Zhu, Z.; Xu, Y.; Jiang, B. A One ppm NDIR Methane Gas Sensor with Single Frequency Filter Denoising Algorithm. Sensors 2012, 12, 12729–12740. [Google Scholar] [CrossRef]
- Sotnikova, G.Y.; Gavrilov, G.A.; Aleksandrov, S.E.; Kapralov, A.A.; Karandashev, S.A.; Matveev, B.A.; Remennyy, M.A. Low Voltage CO-Gas Sensor Based on III–V Mid-IR Immersion Lens Diode Optopairs: Where we Are and How Far we Can Go? IEEE Sens. J. 2010, 10, 225–234. [Google Scholar] [CrossRef]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, J.; Chen, B.; Zhou, J.; Lv, Z. A Low-Power and Portable Biomedical Device for Respiratory Monitoring with a Stable Power Source. Sensors 2015, 15, 19618-19632. https://doi.org/10.3390/s150819618
Yang J, Chen B, Zhou J, Lv Z. A Low-Power and Portable Biomedical Device for Respiratory Monitoring with a Stable Power Source. Sensors. 2015; 15(8):19618-19632. https://doi.org/10.3390/s150819618
Chicago/Turabian StyleYang, Jiachen, Bobo Chen, Jianxiong Zhou, and Zhihan Lv. 2015. "A Low-Power and Portable Biomedical Device for Respiratory Monitoring with a Stable Power Source" Sensors 15, no. 8: 19618-19632. https://doi.org/10.3390/s150819618





