A Detailed Algorithm for Vital Sign Monitoring of a Stationary/Non-Stationary Human through IR-UWB Radar
Abstract
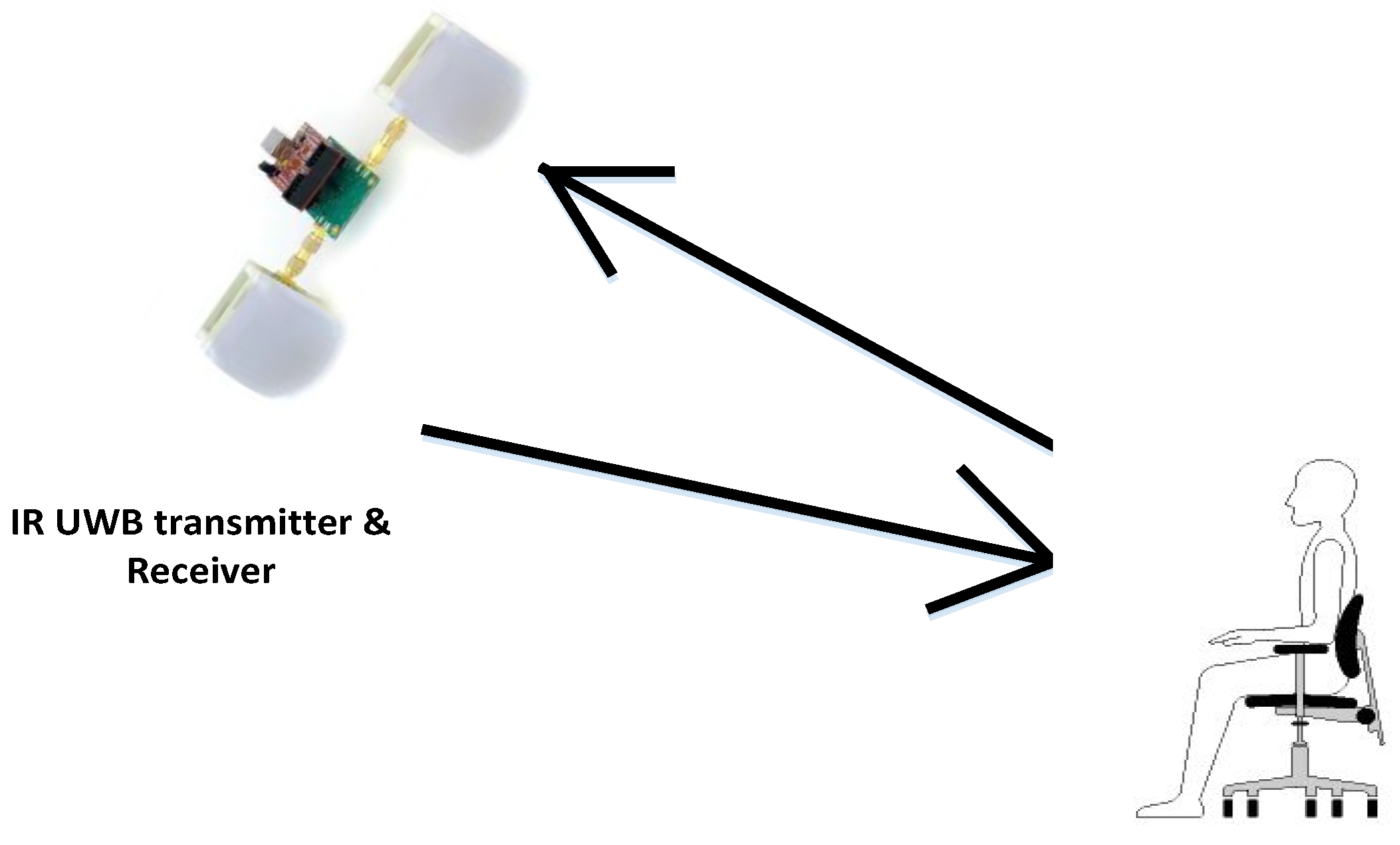
:1. Introduction
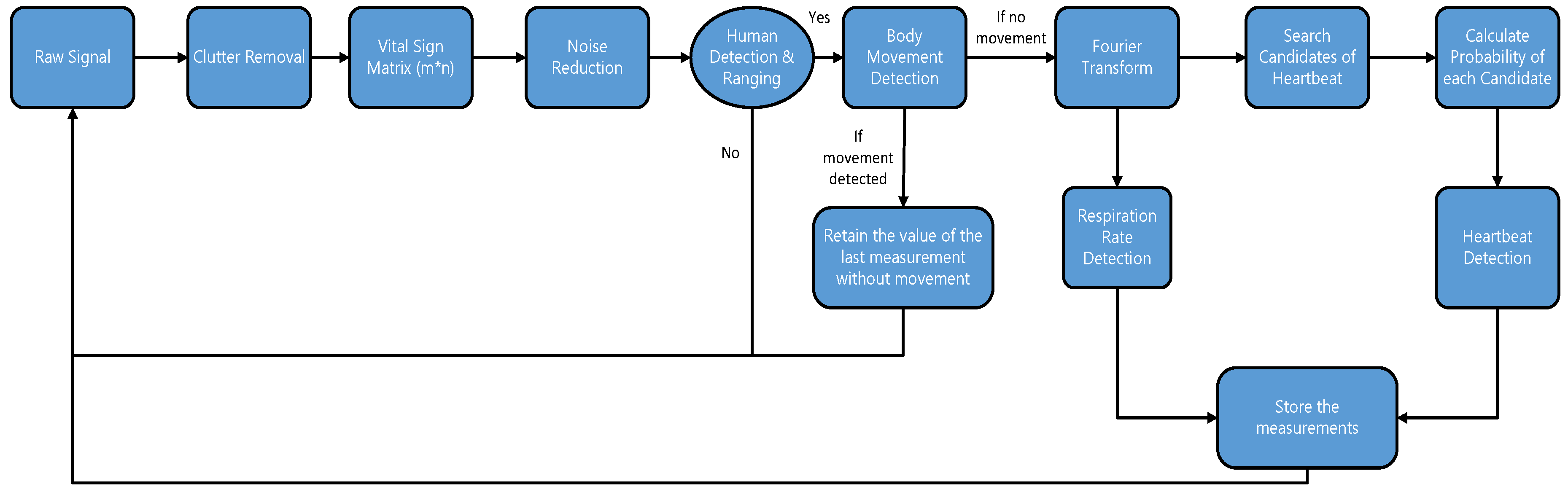
2. Motion Detection
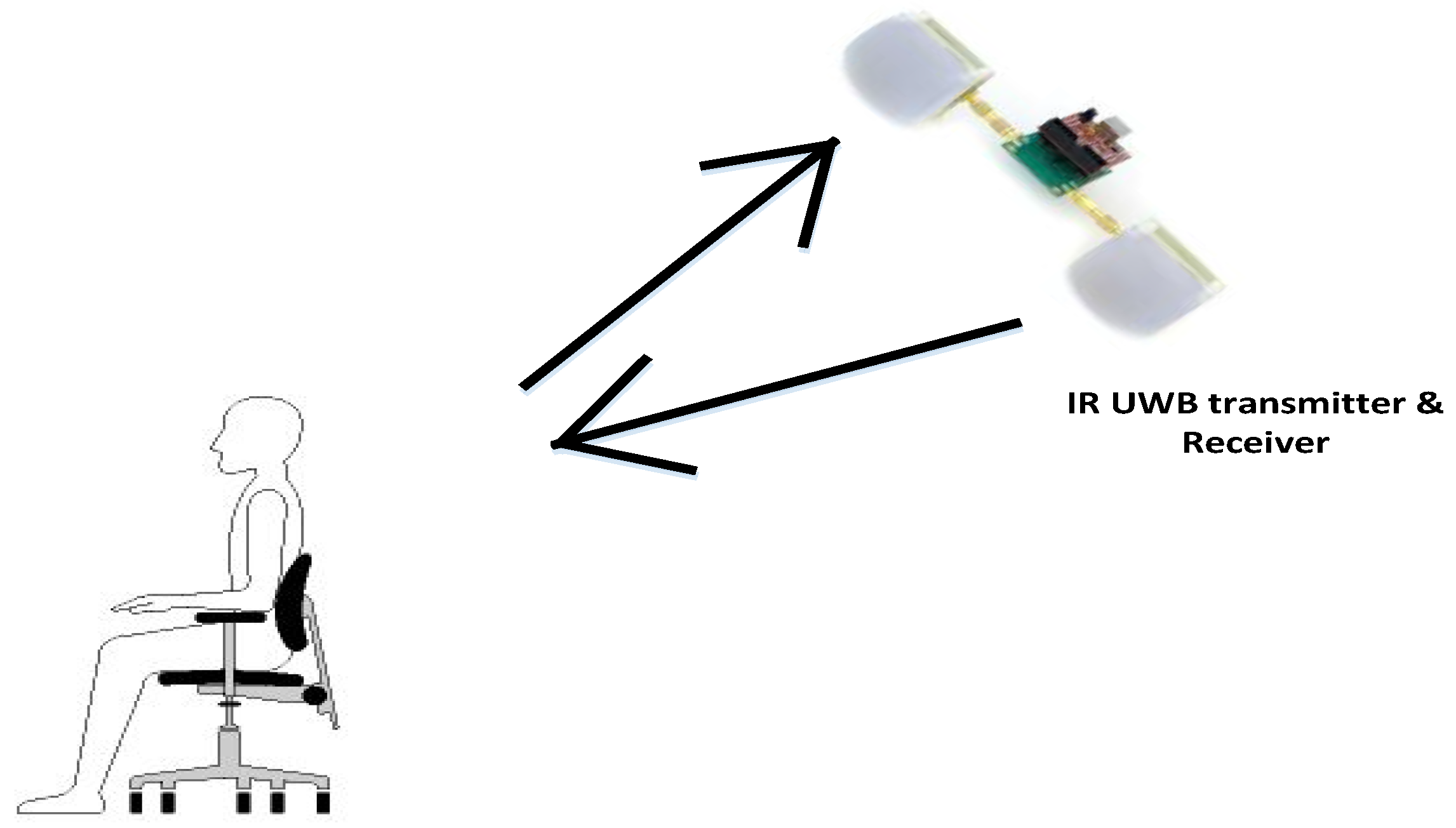
3. Respiration and Heart Rate Measurement
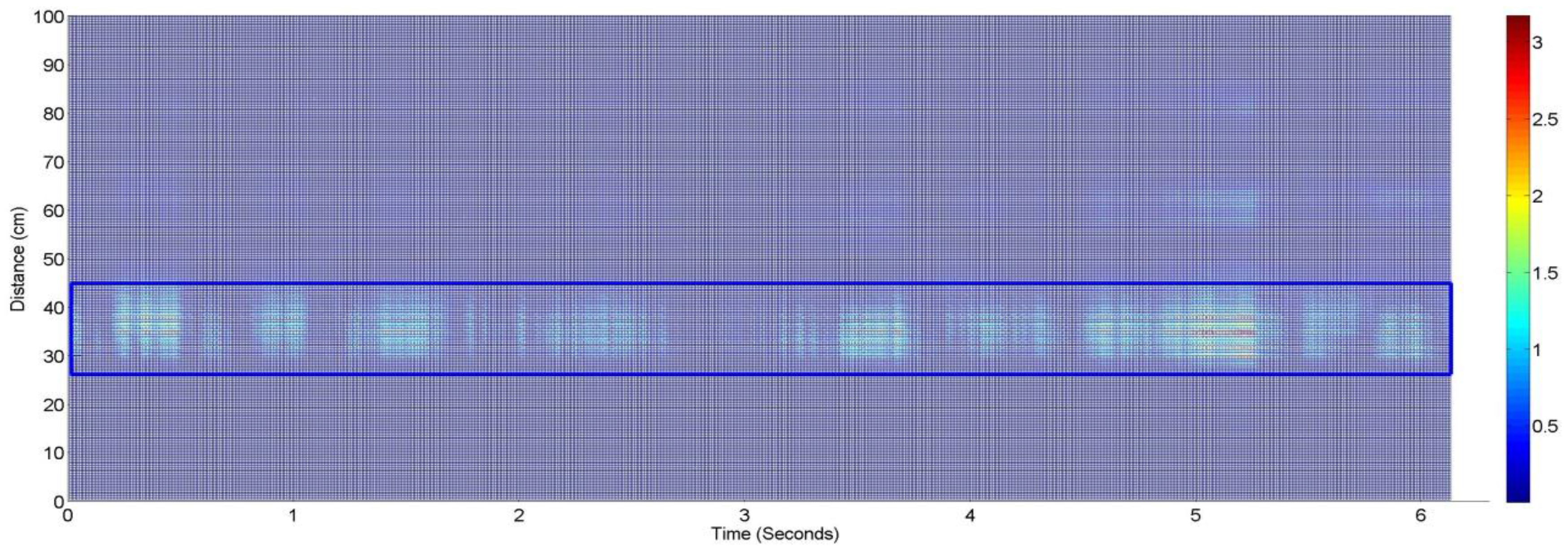
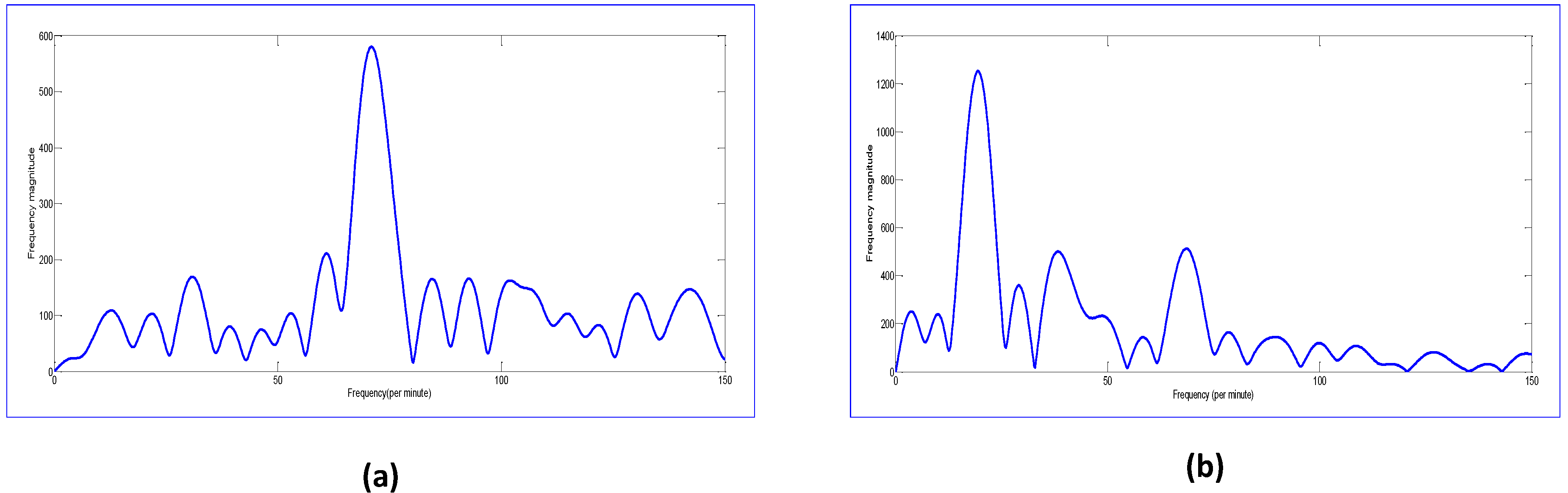
3.1. Frequency Domain Signal and Respiration Rate
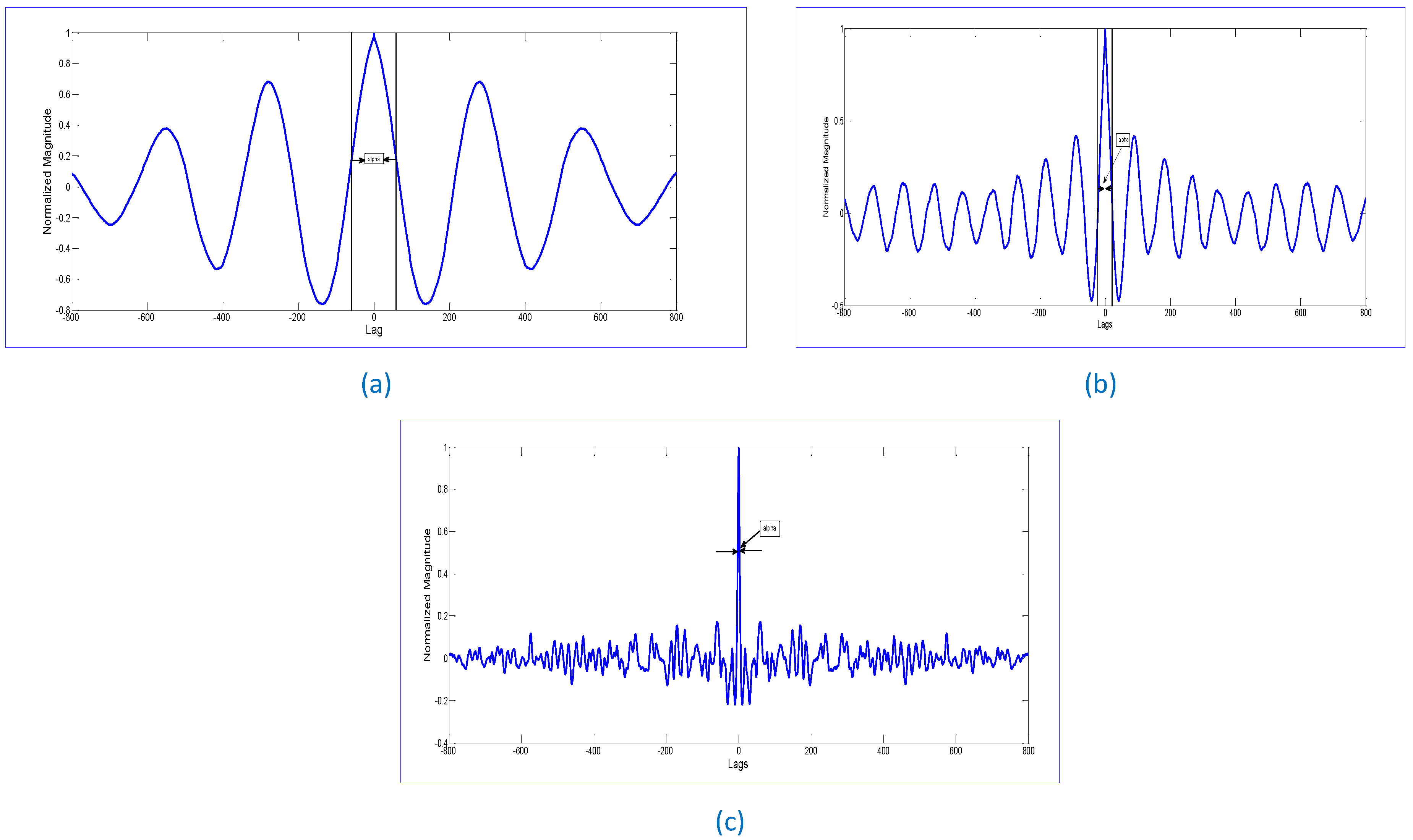
3.2. Heart Rate Detection Algorithm
| Algorithm 1: Selection of the Heart Rate |
|
4. Experimental Results
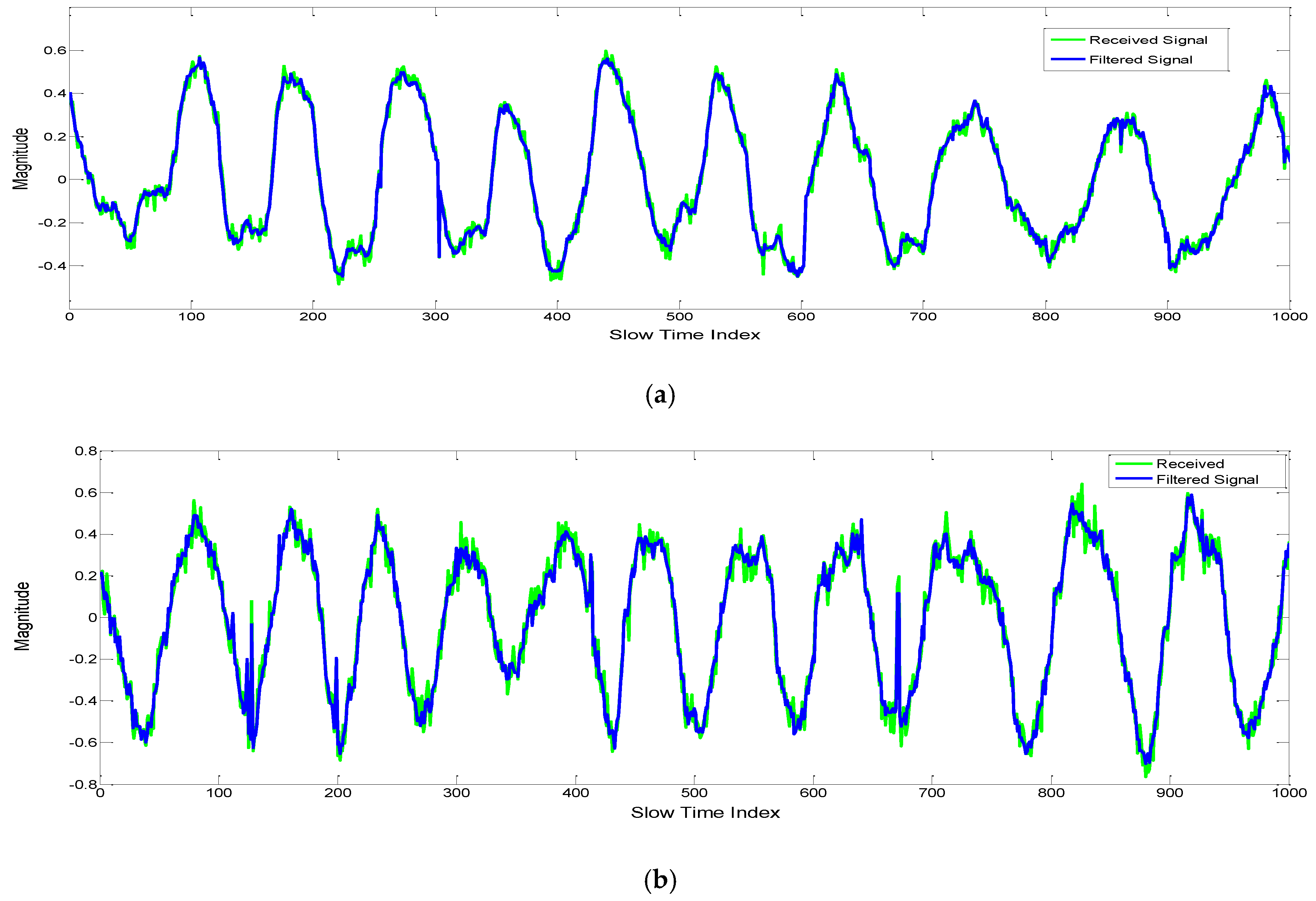
4.1. Noise Reduction by Kalman Filtering
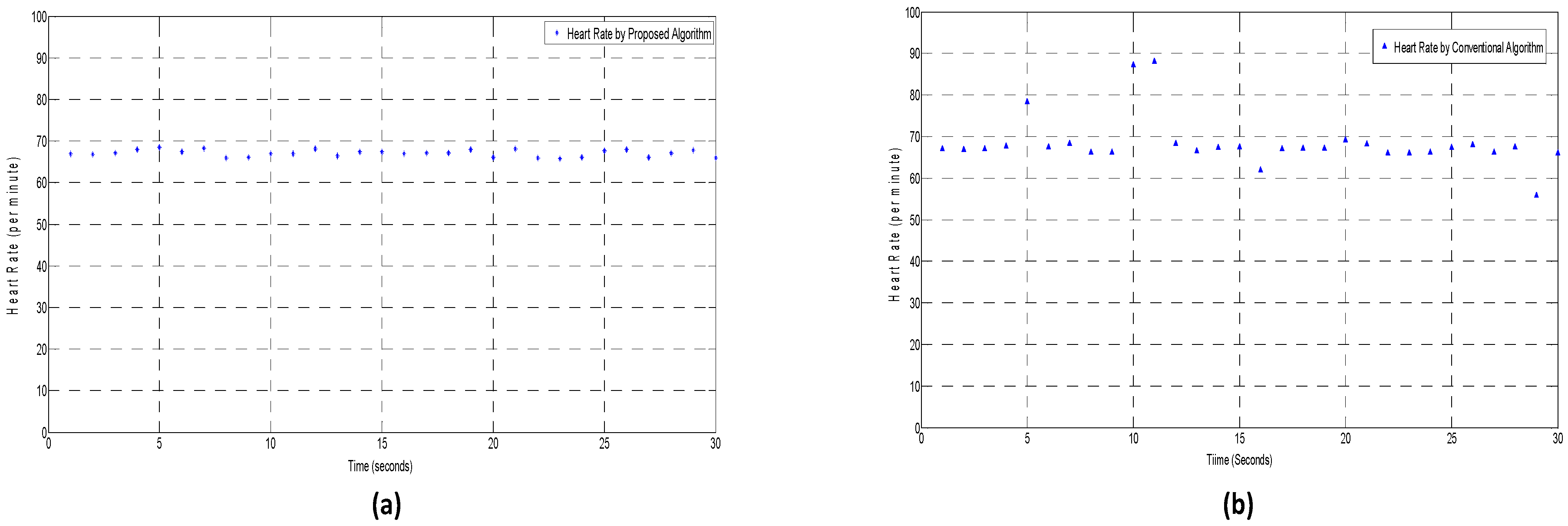
4.2. Heart Rate Detection by Conventional vs. Proposed Algorithm
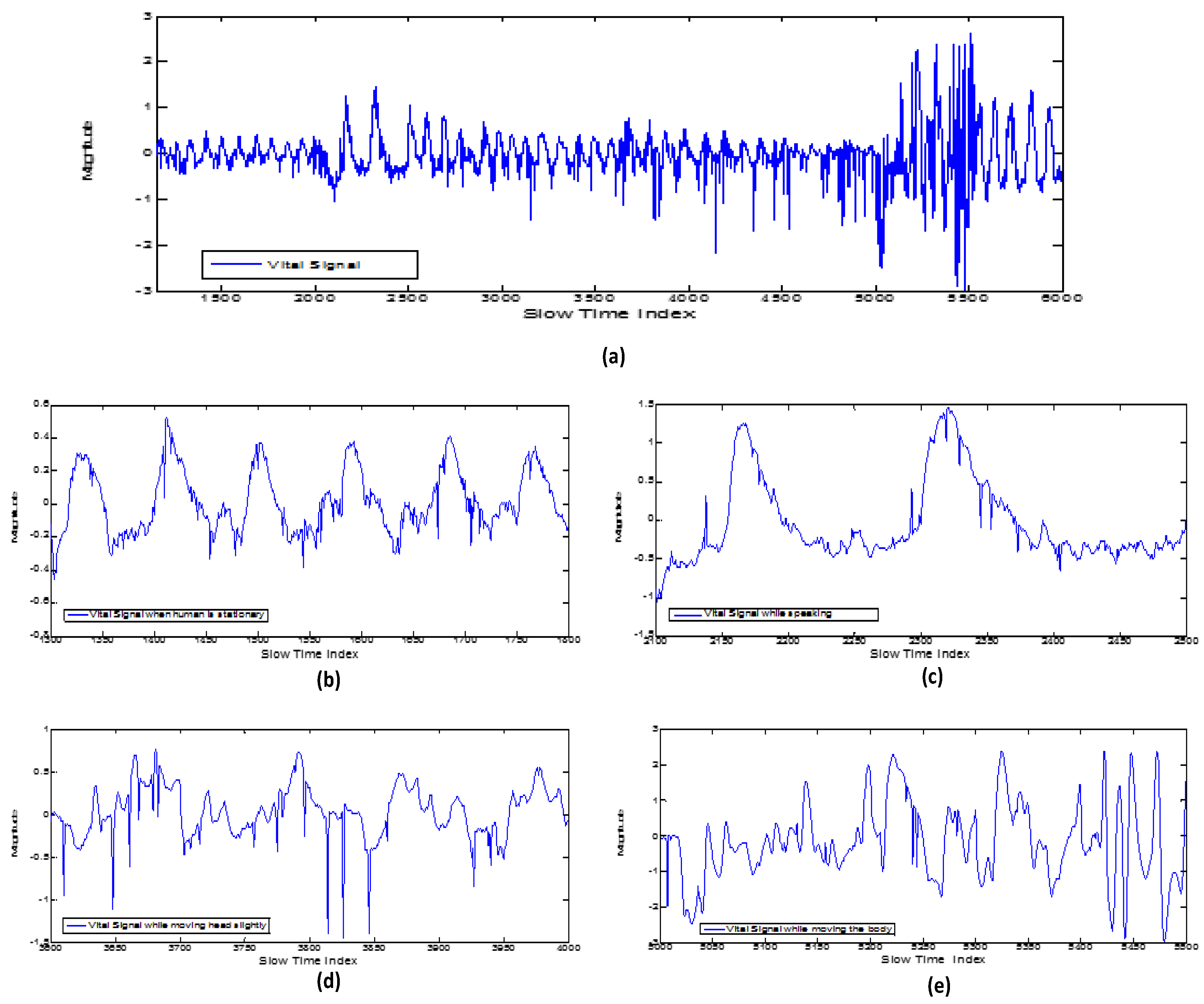
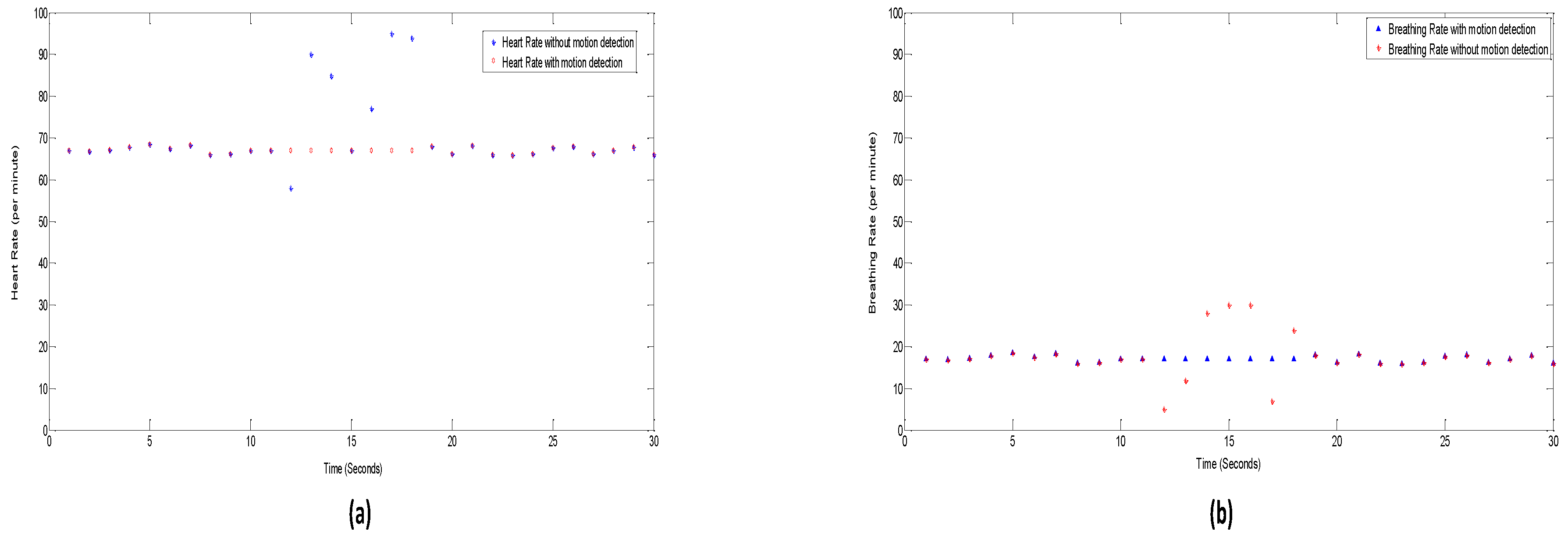
4.3. Vital Signs Measurement with and without Movement Detection Algorithm
4.4. Vital Signs Measurement with the Radar Pointed at the Backside of Body
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| IR UWB | Impulse Radio Ultra-Wideband |
| FCC | Federal Communications Commission |
| FIR | Finite Impulse Response |
| KF | Kalman Filter |
| RR | Respiration Rate |
| HR | Heart Rate |
| GHz | Giga Hertz |
| I/O | Input Output |
| RF | Radio Frequency |
| RBM | Random Body Movement |
| RMSE | Root Mean Squared Error |
| NA | Not Applicable |
| SNR | Signal to Noise ratio |
| Sec | Seconds |
| Bpm | Beats per minute |
References
- Fernandes, J.R.; Wentzloff, D. Recent advances in IR-UWB transceivers: An overview. In Proceedings of the 2010 IEEE International Symposium on Circuits and Systems, Paris, France, 30 May–2 June 2010.
- Fontana, R.J. Recent system applications of short-pulse ultra-wideband (UWB) technology. IEEE Trans. Microw. Theory Tech. 2004, 52, 2087–2104. [Google Scholar] [CrossRef]
- Li, B.; Zhou, Z.; Zou, W.; Li, D.; Zhao, C. Optimal waveforms design for ultra-wideband impulse radio sensors. Sensors 2010, 10, 11038–11063. [Google Scholar] [CrossRef] [PubMed]
- Chóliz, J.; Hernández, Á.; Valdovinos, A. A framework for UWB-based communication and location tracking systems for wireless sensor networks. Sensors 2011, 11, 9045–9068. [Google Scholar] [CrossRef] [PubMed]
- Fear, E.C.; Li, X.; Hagness, S.C.; Stuchly, M.A. Confocal microwave imaging for breast cancer detection: Localization of tumors in three dimensions. IEEE Trans. Biomed. Eng. 2002, 49, 812–822. [Google Scholar] [CrossRef] [PubMed]
- Buehrer, R.M.; Davis, W.A.; Safaai-Jazi, A.; Sweeney, D. Characterization of the ultra-wideband channel. In Proceedings of 2003 IEEE Conference on Ultra Wideband Systems and Technologies, Reston, VA, USA, 16–19 November 2003; pp. 26–31.
- Lazaro, A.; Girbau, D.; Villarino, R. Wavelet-based breast tumor localization technique using a UWB radar. Prog. Electromagn. Res. 2009, 98, 75–95. [Google Scholar] [CrossRef]
- Thiel, F.; Kosch, O.; Seifert, F. Ultra-wideband sensors for improved magnetic resonance imaging, cardiovascular monitoring and tumour diagnostics. Sensors 2010, 10, 10778–10802. [Google Scholar] [CrossRef] [PubMed]
- Staderini, E.M. UWB radars in medicine. IEEE Aerosp. Electron. Syst. Mag. 2002, 17, 13–18. [Google Scholar] [CrossRef]
- Kocur, D.; Švecová, M.; Rovňáková, J. Through-the-wall localization of a moving target by two independent ultra wideband (UWB) radar systems. Sensors 2013, 13, 11969–11997. [Google Scholar] [CrossRef] [PubMed]
- Lazaro, A.; Girbau, D.; Villarino, R. Analysis of vital signs monitoring using an ir-UWB radar. Prog. Electromagn. Res. 2010, 100, 265–284. [Google Scholar] [CrossRef]
- Xu, Y.; Dai, S.; Wu, S.; Chen, J.; Fang, G. Vital sign detection method based on multiple higher order cumulant for ultrawideband radar. IEEE Trans. Geosci. Remote Sens. 2012, 50, 1254–1265. [Google Scholar] [CrossRef]
- Yan, J.; Zhao, H.; Li, Y.; Sun, L.; Hong, H.; Zhu, X. Through-the-wall human respiration detection using impulse ultra-wide-band radar. In Proceedings of the 2016 IEEE Topical Conference on Biomedical Wireless Technologies, Networks, and Sensing Systems (BioWireleSS), Austin, TX, USA, 24–27 January 2016.
- McEwan, T.E. Body Monitoring and Imaging Apparatus and Method. U.S. Patent No. 5,573,012, 12 November 1996. [Google Scholar]
- Droitcour, A.D.; Boric-Lubecke, O.; Lubecke, V.M.; Lin, J. 0.25/spl mu/m CMOS and BiCMOS single-chip direct-conversion Doppler radars for remote sensing of vital signs. In Proceedings of the 2002 IEEE International Solid-State Circuits Conference (ISSCC), Digest of Technical Papers, San Francisco, CA, USA, 3–7 February 2002.
- Lubecke, O.B.; Ong, P.-W.; Lubecke, V.M. 10 GHz Doppler radar sensing of respiration and heart movement. In Proceedings of the IEEE 28th Annual Northeast Bioengineering Conference, Philadelphia, PA, USA, 20–21 April 2002.
- Ivashov, S.I.; Razevig, V.V.; Sheyko, A.P.; Vasilyev, I.A. Detection of human breathing and heartbeat by remote radar. In Proceedings of the Progress in Electromagnetic Research Symposium, Pisa, Italy, 28–31 March 2004.
- Zito, D.; Pepe, D.; Mincica, M.; Zito, F.; Tognetti, A.; Lanata, A.; De Rossi, D. SoC CMOS UWB pulse radar sensor for contactless respiratory rate monitoring. IEEE Trans. Biomed. Circuits Syst. 2011, 5, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Ossberger, G.; Buchegger, T.; Schimback, E.; Stelzer, A.; Weigel, R. Non-invasive respiratory movement detection and monitoring of hidden humans using ultra wideband pulse radar. In Proceedings of the 2004 International Workshop on Ultra Wideband Systems, Joint with Conference on Ultrawideband Systems and Technologies, Joint UWBST & IWUWBS, Kyoto, Japan, 18–21 May 2004.
- Zetik, R.; Crabbe, S.; Krajnak, J.; Peyerl, P.; Sachs, J.; Thomä, R. Detection and localization of persons behind obstacles using M-sequence through-the-wall radar. Proc. SPIE 2006, 6201. [Google Scholar] [CrossRef]
- Yarovoy, A.G.; Ligthart, L.P.; Matuzas, J.; Levitas, B. UWB radar for human being detection. IEEE Aerosp. Electron. Syst. Mag. 2006, 21, 10–14. [Google Scholar] [CrossRef]
- Zito, D.; Pepe, D.; Neri, B.; De Rossi, D.; Lanatà, A.; Tognetti, A.; Scilingo, E.P. Wearable system-on-a-chip UWB radar for health care and its application to the safety improvement of emergency operators. In Proceedings of the 2007 29th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Lyon, France, 23–26 August 2007.
- Immoreev, I.; Tao, T.-H. UWB radar for patient monitoring. IEEE Aerosp. Electron. Syst. Mag. 2008, 23, 11–18. [Google Scholar] [CrossRef]
- Chu, T.-S.; Roderick, J.; Chang, S.; Mercer, T.; Du, C.; Hashemi, H. A short-range UWB impulse-radio CMOS sensor for human feature detection. In Proceedings of the 2011 IEEE International Solid-State Circuits Conference Digest of Technical Papers (ISSCC), San Francisco, CA, USA, 20–24 February 2011.
- Zetik, R.; Jovanoska, S.; Thomä, R. Simple method for localisation of multiple tag-free targets using UWB sensor network. In Proceedings of the 2011 IEEE International Conference on Ultra-Wideband (ICUWB), Bologna, Italy, 14–16 September 2011.
- Zito, D.; Pepe, D.; Mincica, M.; Zito, F. A 90 nm CMOS SoC UWB pulse radar for respiratory rate monitoring. In Proceedings of the 2011 IEEE International Solid-State Circuits Conference, San Francisco, CA, USA, 20–24 February 2011.
- Van, N.; Javaid, A.Q.; Weitnauer, M.A. Harmonic Path (HAPA) algorithm for non-contact vital signs monitoring with IR-UWB radar. In Proceedings of the 2013 IEEE Biomedical Circuits and Systems Conference (BioCAS), Rotterdam, The Netherlands, 31 October–2 November 2013.
- Van, N.; Javaid, A.Q.; Weitnauer, M.A. Spectrum-averaged Harmonic Path (SHAPA) algorithm for non-contact vital sign monitoring with ultra-wideband (UWB) radar. In Proceedings of the 2014 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Chicago, IL, USA, 27–31 August 2014.
- Khan, F.; Choi, J.W.; Cho, S.H. Design issues in vital sign monitoring through IR UWB radar. In Proceedings of the 18th IEEE International Symposium on Consumer Electronics (ISCE 2014), JeJu, Korea, 22–25 June 2014.
- Fletcher, R.; Han, J. Low-cost differential front-end for Doppler radar vital sign monitoring. In Proceedings of the IEEE MTT-S International Microwave Symposium Digest (MTT’09), Boston, MA, USA, 7–12 June 2009.
- Ascione, M.; Buonanno, A.; D'Urso, M.; Angrisani, L.; Moriello, R.S.L. A new measurement method based on music algorithm for through-the-wall detection of life signs. IEEE Trans. Instrum. Meas. 2013, 62, 13–26. [Google Scholar] [CrossRef]
- Levitas, B.; Matuzas, J. UWB radar for human being detection behind the wall. In Proceedings of the 2006 International Radar Symposium, Krakow, Poland, 24–26 May 2006.
- Greneker, E.F. RADAR flashlight for through-the-wall detection of humans. Proc. SPIE 1998, 3375. [Google Scholar] [CrossRef]
- Lazaro, A.; Girbau, D.; Villarino, R. Techniques for clutter suppression in the presence of body movements during the detection of respiratory activity through UWB radars. Sensors 2014, 14, 2595–2618. [Google Scholar] [CrossRef] [PubMed]
- Yan, J.; Hong, H.; Zhao, H.; Li, Y.; Gu, C.; Zhu, X. Through-Wall Multiple Targets Vital Signs Tracking Based on VMD Algorithm. Sensors 2016, 16, 1293. [Google Scholar] [CrossRef] [PubMed]
- Li, W.Z.; Li, Z.; Lv, H.; Lu, G.; Zhang, Y.; Jing, X.; Li, S.; Wang, J. A new method for non-line-of-sight vital sign monitoring based on developed adaptive line enhancer using low centre frequency UWB radar. Prog. Electromagn. Res. 2013, 133, 535–554. [Google Scholar] [CrossRef]
- Leib, M.; Menzel, W.; Schleicher, B.; Schumacher, H. Vital signs monitoring with a UWB radar based on a correlation receiver. In Proceedings of the IEEE Fourth European Conference on Antennas and Propagation (EuCAP), Barcelona, Spain, 12–16 April 2010.
- Rivera, N.V.; Venkatesh, S.; Anderson, C.; Buehrer, R.M. Multi-target estimation of heart and respiration rates using ultra wideband sensors. In Proceedings of the IEEE 2006 14th European Signal Processing Conference, Florence, Italy, 4–8 September 2006.
- Baldi, M.; Chiaraluce, F.; Zanaj, B.; Moretti, M. Analysis and simulation of algorithms for vital signs detection using UWB radars. In Proceedings of the 2011 IEEE International Conference on Ultra-Wideband (ICUWB), Bologna, Italy, 14–16 September 2011.
- Van, N.; Javaid, A.Q.; Weitnauer, M.A. Detection of motion and posture change using an IR-UWB radar. In Proceedings of the 2016 IEEE 38th Annual International Conference of the Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016.
- Khan, F.; Choi, J.W.; Cho, S.H. Vital sign monitoring of a non-stationary human through IR-UWB radar. In Proceedings of the 2014 4th IEEE International Conference on Network Infrastructure and Digital Content (IC-NIDC), Beijing, China, 19–21 September 2014; pp. 511–514.
- Chia, M.Y.W.; Leong, S.W.; Sim, C.K.; Chan, K.M. Through-wall UWB radar operating within FCC’s mask for sensing heart beat and breathing rate. In Proceedings of the European Radar Conference, 2005 (EURAD 2005), Piscataway, NJ, USA, 3–4 October 2005.
- Baboli, M.; Ghorashi, S.A.; Saniei, N.; Ahmadian, A. A new wavelet based algorithm for estimating respiratory motion rate using UWB radar. In Proceedings of the 2009 International Conference on Biomedical and Pharmaceutical Engineering, Singapore, 2–4 December 2009.
- Schleicher, B.; Nasr, I.; Trasser, A.; Schumacher, H. IR-UWB radar demonstrator for ultra-fine movement detection and vital-sign monitoring. IEEE Trans. Microw. Theory Tech. 2013, 61, 2076–2085. [Google Scholar] [CrossRef]
- Richards, J.L.; Fullerton, L.W.; Kelly, D.A.; Meigs, D.C.; Payment, T.T.; Finn, J.S.; Tucker, W.J.; Welch, W.D., Jr. System and Method Using Impulse Radio Technology to Track and Monitor People Needing Health Care. U.S. Patent 6,466,125, 15 October 2002. [Google Scholar]
- Li, C.; Lin, J.; Xiao, Y. Robust overnight monitoring of human vital signs by a non-contact respiration and heartbeat detector. In Proceedings of the 28th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBS’06), New York City, NY, USA, 31 August–3 September 2006.
- Yilmaz, T.; Foster, R.; Hao, Y. Detecting vital signs with wearable wireless sensors. Sensors 2010, 10, 10837–10862. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Lin, J. Random body movement cancellation in Doppler radar vital sign detection. IEEE Trans. Microw. Theory Tech. 2008, 56, 3143–3152. [Google Scholar]
- Hu, X.; Jin, T. Short-Range Vital Signs Sensing Based on EEMD and CWT Using IR-UWB Radar. Sensors 2016, 16, 2025. [Google Scholar] [CrossRef] [PubMed]
- Venkatesh, S.; Anderson, C.R.; Rivera, N.V.; Buehrer, R.M. Implementation and analysis of respiration-rate estimation using impulse-based UWB. In Proceedings of the MILCOM 2005—IEEE Military Communications Conference, Atlantic City, NJ, USA, 17–20 October 2005.
- Javaid, A.Q.; Noble, C.M.; Rosenberg, R.; Weitnauer, M.A. Towards Sleep Apnea Screening with an Under-the-Mattress IR-UWB Radar Using Machine Learning. In Proceedings of the 2015 IEEE 14th International Conference on Machine Learning and Applications (ICMLA), Miami, FL, USA, 9–11 December 2015.
- Ota, K.; Ota, Y.; Otsu, M.; Kajiwara, A. Elderly-care motion sensor using UWB-IR. In Proceedings of the 2011 IEEE Sensors Applications Symposium (SAS), San Antonio, TX, USA, 22–24 February 2011.
- Li, X.; Qiao, D.; Li, Y. Macro-motion detection using ultra-wideband impulse radar. In Proceedings of the 2014 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Chicago, IL, USA, 27–31 August 2014.
- Yim, D.H.; Cho, S.H. An Equidistance Multi-human Detection Algorithm Based on Noise Level Using Mono-static IR-UWB Radar System. In Proceedings of the 2014 International Conference on Future Communication, Information and Computer Science (FCICS 2014), Beijing, China, 22–23 May 2014.
- Khan, N.; Khattak, M.I.; Khan, M.N.; Khan, F.; Khan, L.U.; Salam, S.A.; Gu, D.-W. Implementation of linear prediction techniques in state estimation. In Proceedings of the 2013 10th International Bhurban Conference on Applied Sciences and Technology (IBCAST), Islamabad, Pakistan, 15–19 January 2013.
- Khan, F.; Khattak, M.I.; Shafi, M.; Saleem, M.; Khan, F.; Khan, N. A case study of variable window size in linear prediction techniques. World Appl. Sci. J. 2013, 23, 71–80. [Google Scholar]
- Goodwin, G.C.; Sin, K.S. Adaptive Filtering Prediction and Control; Courier Corporation: North Chelmsford, MA, USA, 2014. [Google Scholar]


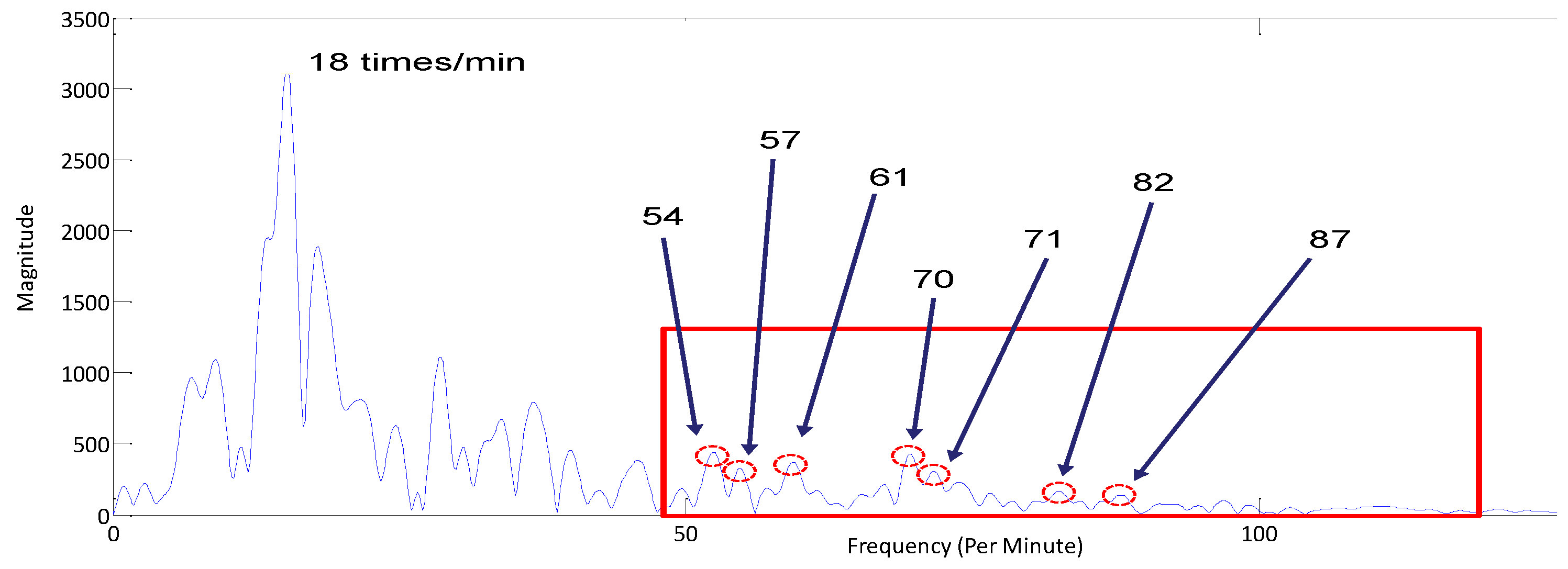
| Frequency (per Minute) Location | Total No. of Repetitions in M = 20 Iterations |
|---|---|
| 57 | 12 |
| 62 | 8 |
| 70 | 19 |
| 82 | 13 |
| Distance b/w Human & Radar | SNR before Filtering (dB) | SNR after Filtering (dB) | RMSE Breathing Rate/Heart Rate (Unfiltered Signal) | RMSE Breathing Rate/Heart Rate (Filtered Signal) |
|---|---|---|---|---|
| 1 m | 12.3 | 18.2 | 0.012/0.840 | 0.006/0.372 |
| 2 m | 8.6 | 14.9 | 0.042/1.831 | 0.029/0.487 |
| Human Subject No. | Breathing Frequency | Heart Rate | Total Estimates | Invalid Estimates by Filter Suppression | Invalid Estimate by Proposed Algorithm |
|---|---|---|---|---|---|
| 01 | 16 | 68 | 30 | 1 | 0 |
| 02 | 18 | 54 | 30 | 5 | 0 |
| 03 | 20 | 59 | 30 | 6 | 2 |
| 04 | 15 | 72 | 30 | 1 | 1 |
| 05 | 17 | 81 | 30 | 0 | 0 |
| Body State | Normalized Autocorrelation Width | Time Required for Motion Detection | Estimated Breathing Rate/Heart Rate | Original Breathing Rate/Heart Rate |
|---|---|---|---|---|
| Stationary | 1 | NA | 13/74 | 13/74 |
| Speaking | 0.73 | 3.2 s | 8/82 | 7.5/74 |
| Shaking head slightly (1–3 cm) | 0.46 | 1.8 s | 19/60 | 13/74 |
| Moving the body slightly (1–2 cm) | 0.24 | 0.46 s | 17/55 | 13/74 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khan, F.; Cho, S.H. A Detailed Algorithm for Vital Sign Monitoring of a Stationary/Non-Stationary Human through IR-UWB Radar. Sensors 2017, 17, 290. https://doi.org/10.3390/s17020290
Khan F, Cho SH. A Detailed Algorithm for Vital Sign Monitoring of a Stationary/Non-Stationary Human through IR-UWB Radar. Sensors. 2017; 17(2):290. https://doi.org/10.3390/s17020290
Chicago/Turabian StyleKhan, Faheem, and Sung Ho Cho. 2017. "A Detailed Algorithm for Vital Sign Monitoring of a Stationary/Non-Stationary Human through IR-UWB Radar" Sensors 17, no. 2: 290. https://doi.org/10.3390/s17020290
APA StyleKhan, F., & Cho, S. H. (2017). A Detailed Algorithm for Vital Sign Monitoring of a Stationary/Non-Stationary Human through IR-UWB Radar. Sensors, 17(2), 290. https://doi.org/10.3390/s17020290






