Wearable Contactless Respiration Sensor Based on Multi-Material Fibers Integrated into Textile
Abstract
:1. Introduction
2. Sensor Design
3. Results and Discussion
3.1. Antenna Characterization
3.1.1. Return Loss
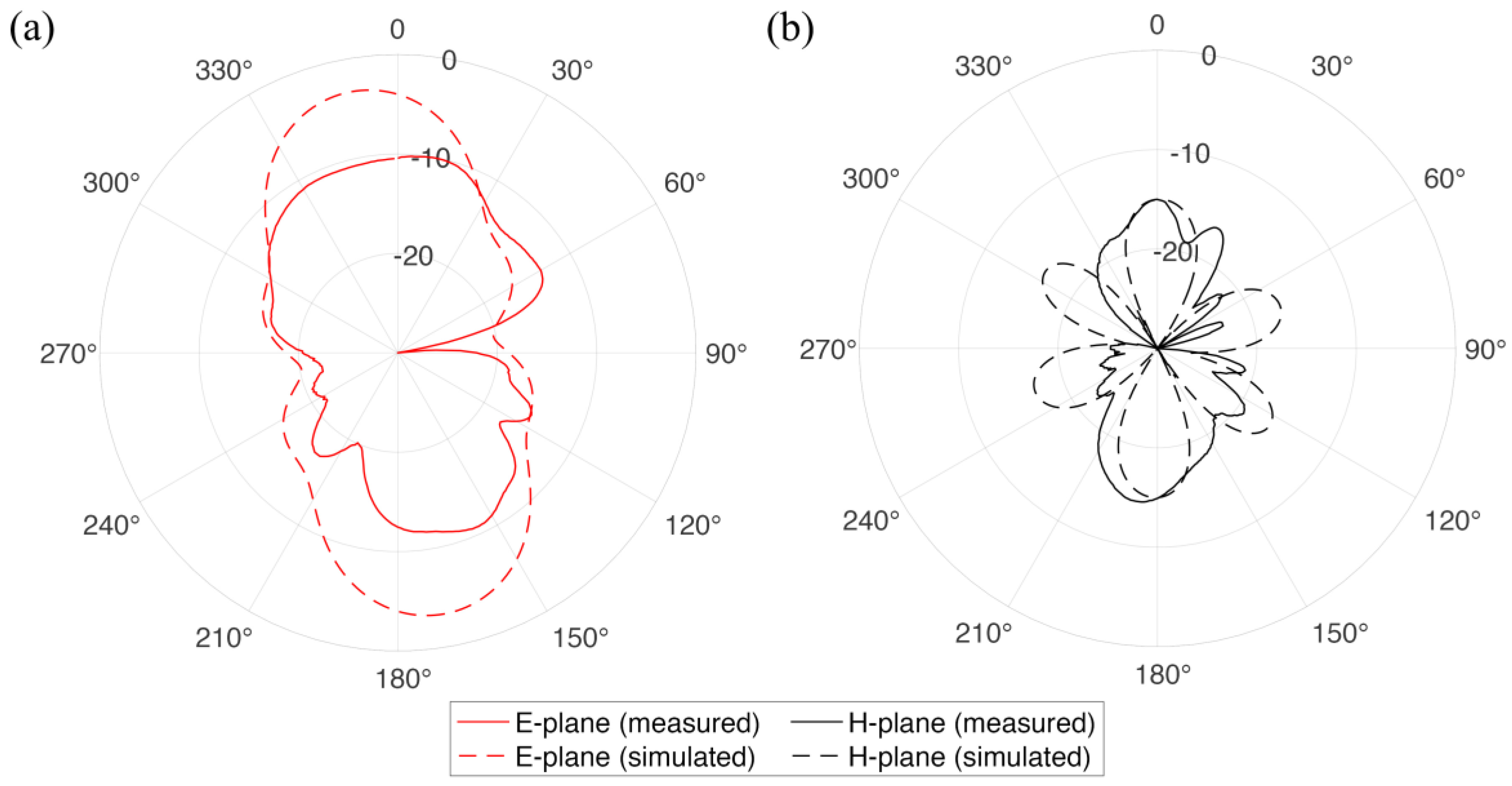
3.1.2. Radiation Pattern
3.1.3. Gain
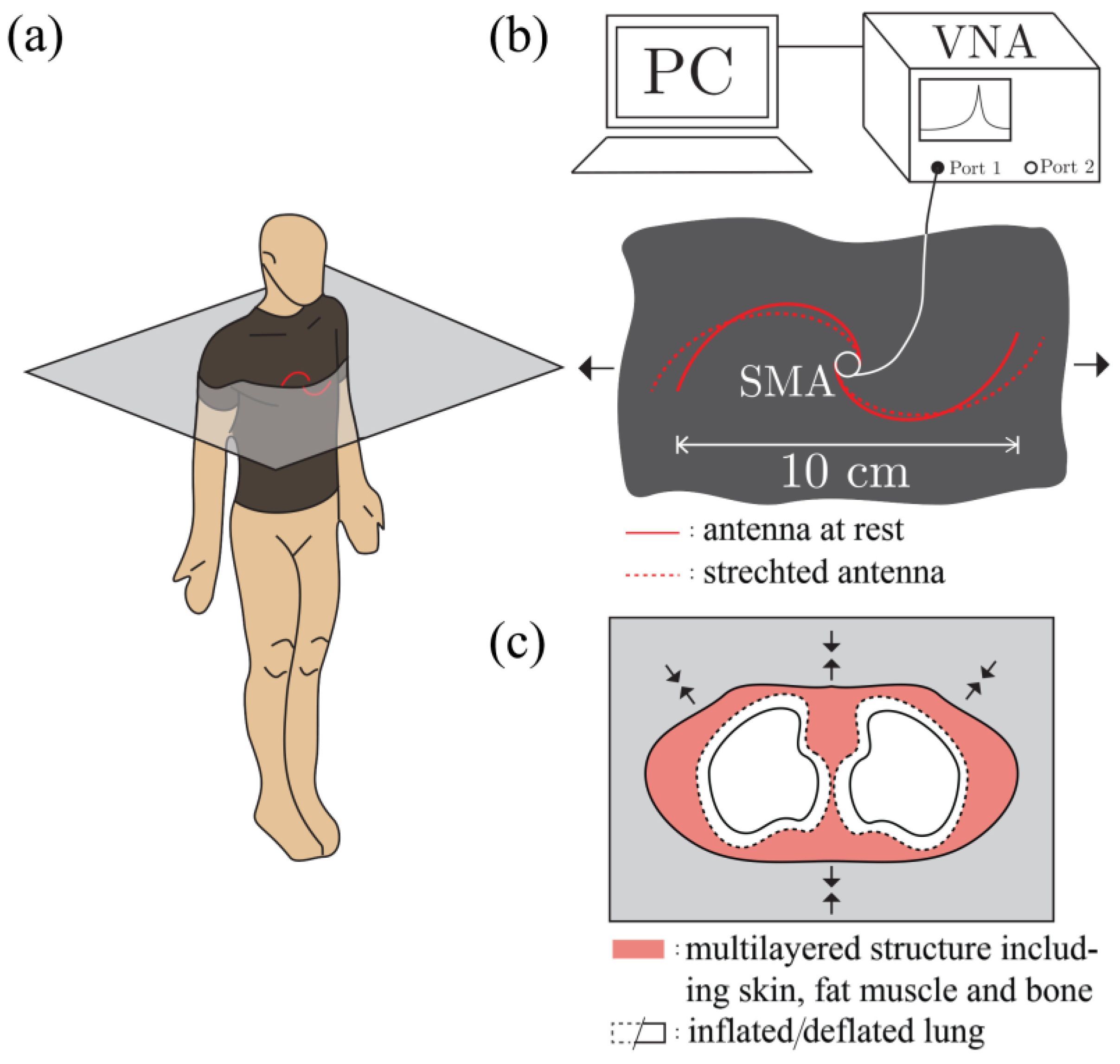
3.2. Breathing Detection
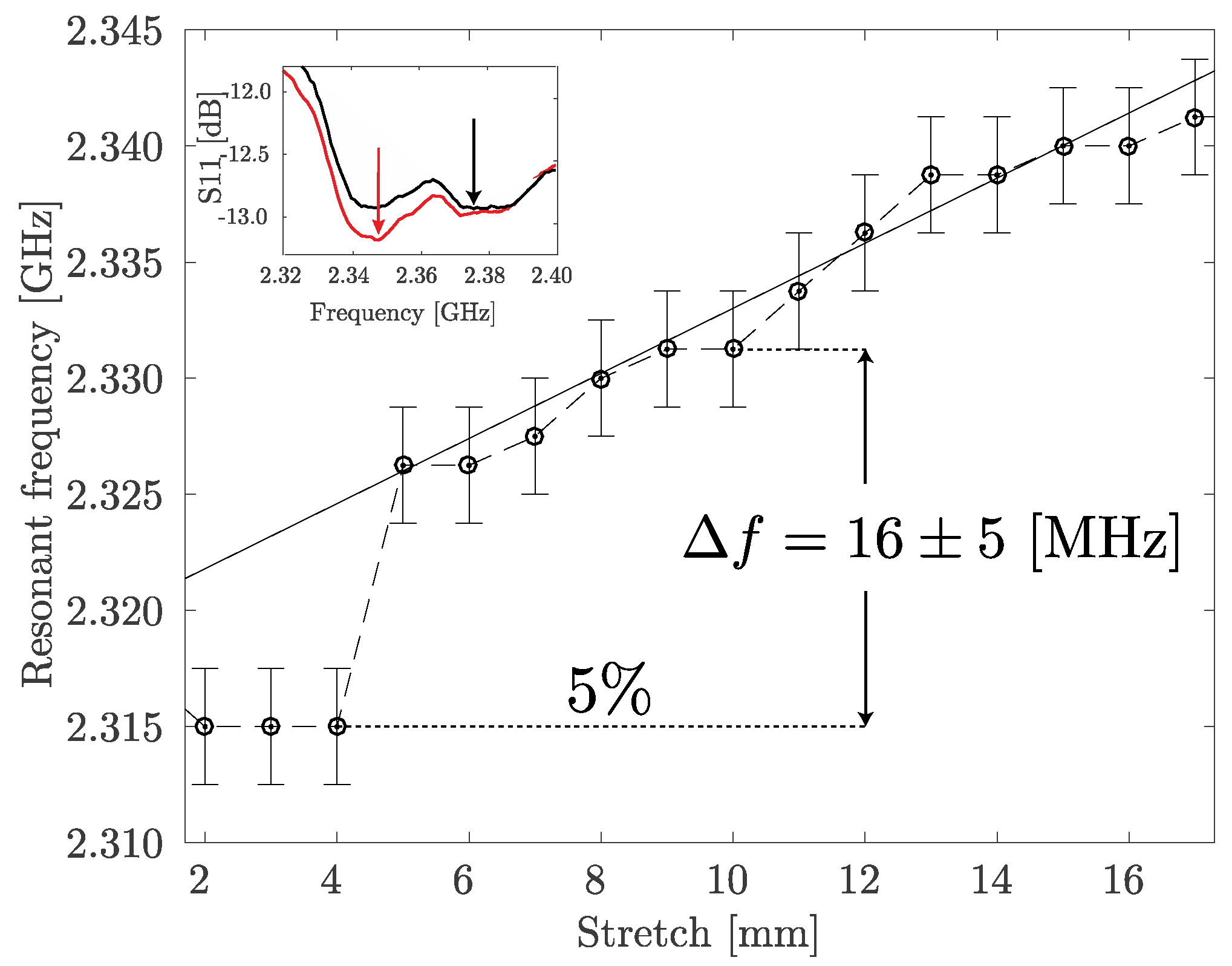
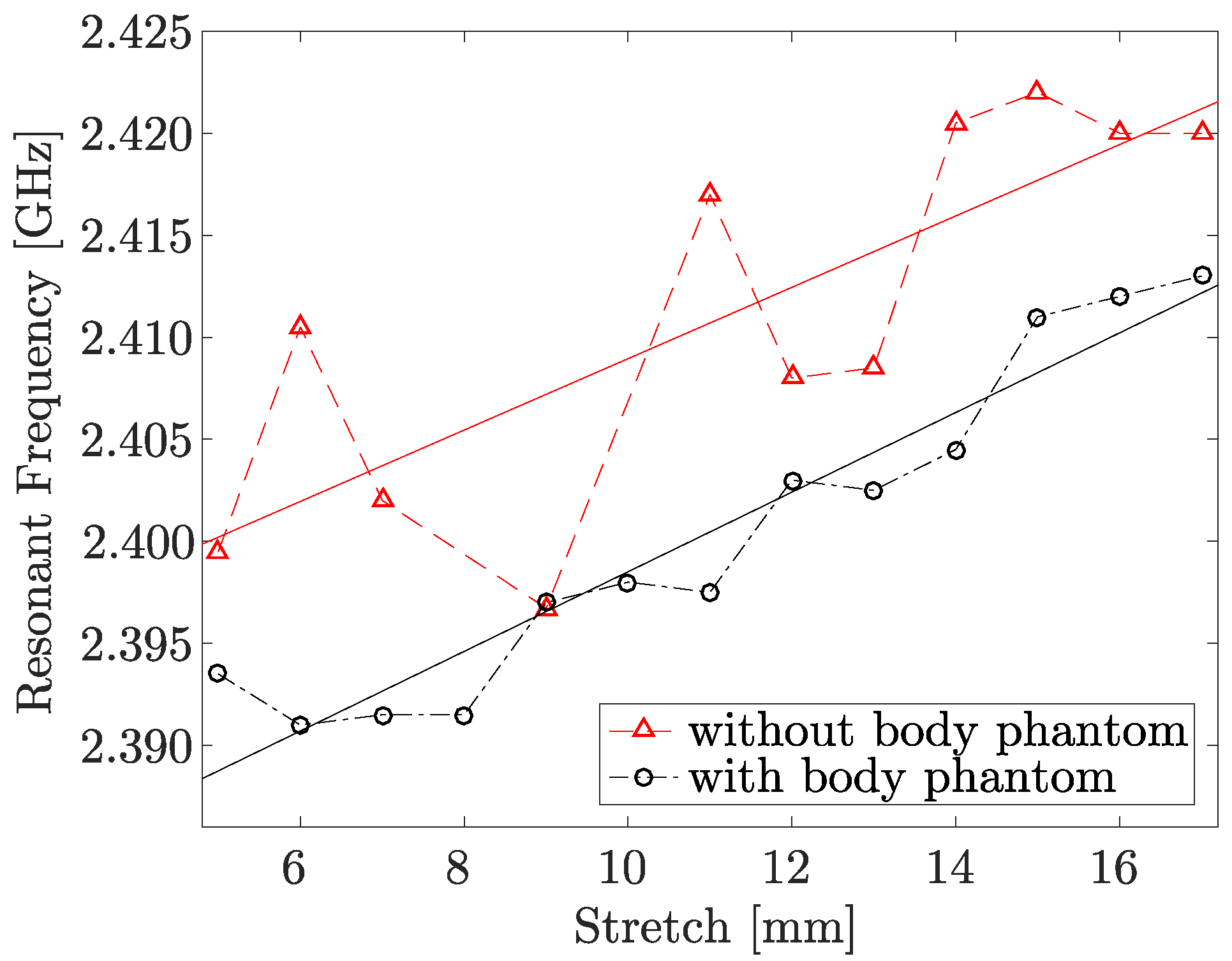
3.2.1. Antenna Configuration Change Due to Stretching
Off-Body
On body phantom
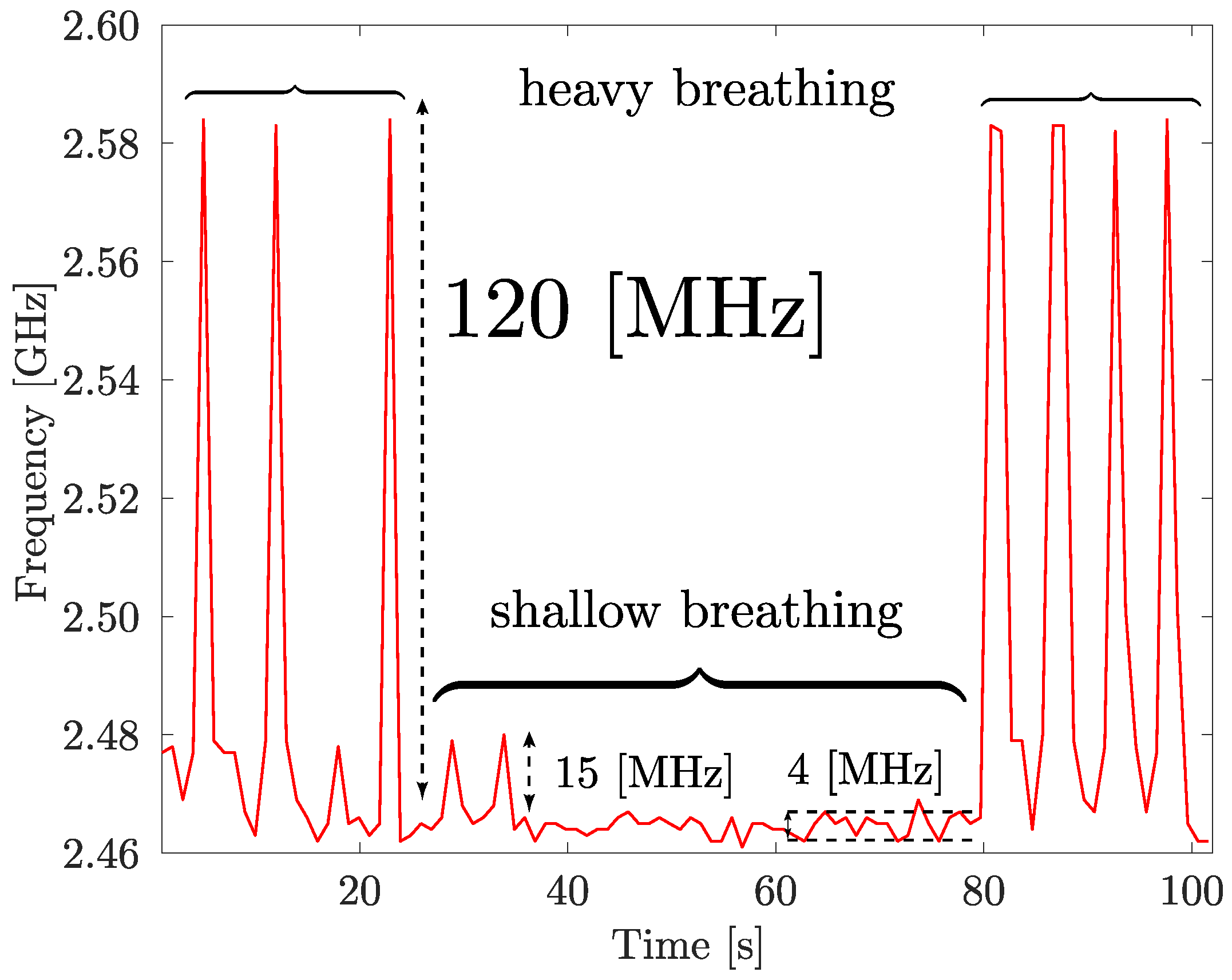
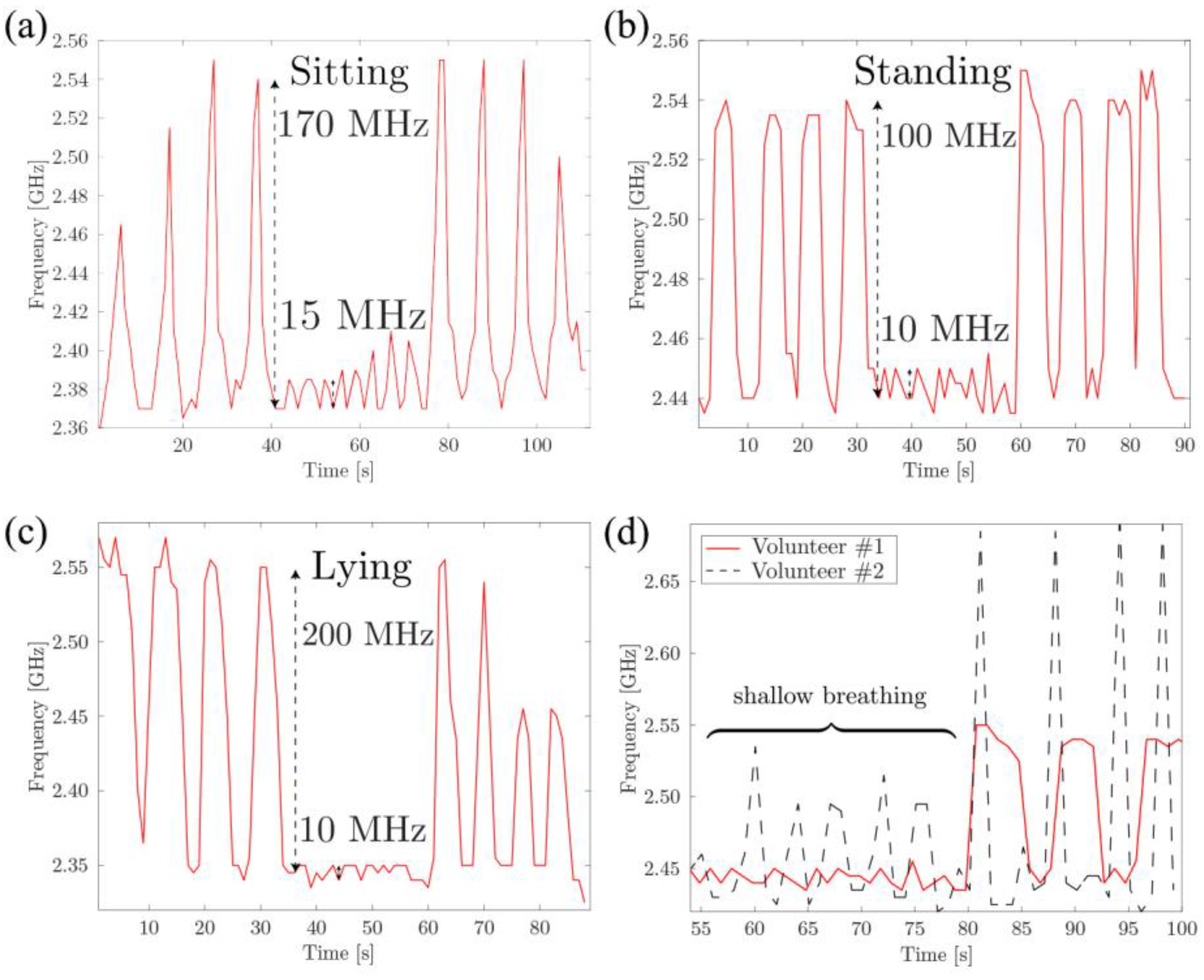
3.2.2. Respiration Sensing Based on the Torso Volume Change
3.2.3. On-Body Measurements
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Hung, K.; Lee, C.C.; Choy, S.-O. Ubiquitous Health Monitoring: Integration of Wearable Sensors, Novel Sensing Techniques, and Body Sensor Networks. In Mobile Health; Sasan, A., Ed.; Springer International Publishing: Cham, Switzerland, 2015; pp. 319–342. [Google Scholar]
- Shyamal, P.; Hyung, P.; Paolo, B.; Leighton, C.; Mary, R. A Review of Wearable Sensors and Systems with Application in Rehabilitation. J. NeuroEng. Rehabil. 2012, 9, 1–17. [Google Scholar]
- Kay, M.; Santos, J.; Takane, M. Mhealth: New Horizons for Health through Mobile Technologies; World Health Organization: Geneva, Switzerland, 2011; Volume 64, p. 66. [Google Scholar]
- Dziuda, L.; Skibniewski, F.W.; Krej, M.; Lewandowski, J. Monitoring Respiration and Cardiac Activity Using Fiber Bragg Grating-Based Sensor. IEEE Trans. Biomed. Eng. 2012, 59, 1934–1942. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.; Berglin, L.; Li, Y.J.; Mattila, H.; Mehrjerdi, A.K.; Skrifvars, M. Disappearing Sensor'-Textile Based Sensor for Monitoring Breathing. In Proceedings of the 2011 International Conference on Control, Automation and Systems Engineering (CASE), Singapore, 30–31 July 2011. [Google Scholar]
- Grenvik, A.; Ballou, S.; McGinley, E.; Millen, J.E.; Cooley, W.L.; Safar, P. Impedance Pneumography: Comparison between Chest Impedance Changes and Respiratory Volumes in 11 Healthy Volunteers. Chest 1972, 62, 439–443. [Google Scholar] [CrossRef] [PubMed]
- Leonard, P.; Beattie, T.; Addison, P.; Watson, J. Standard Pulse Oximeters Can Be Used to Monitor Respiratory Rate. Emerg. Med. J. 2003, 20, 524–525. [Google Scholar] [CrossRef] [PubMed]
- Boyle, J.; Bidargaddi, N.; Sarela, A.; Karunanithi, M. Automatic Detection of Respiration Rate from Ambulatory Single-Lead Ecg. IEEE Trans. Inf. Technol. Biomed. 2009, 13, 890–896. [Google Scholar] [CrossRef] [PubMed]
- Lazaro, A.; Girbau, D.; Villarino, R. Analysis of Vital Signs Monitoring Using an Ir-Uwb Radar. Prog. Electromagn. Res. B 2010, 100, 265–284. [Google Scholar] [CrossRef]
- Lorussi, F.; Scilingo, E.P.; Tesconi, M.; Tognetti, A.; De Rossi, D. Strain Sensing Fabric for Hand Posture and Gesture Monitoring. IEEE Trans. Inf. Technol. Biomed. 2005, 9, 372–381. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.M.; Wu, C.C.; Chou, C.M.; Yang, T.L. Vehicle Driver’s Ecg and Sitting Posture Monitoring System. In Proceedings of the 9th International Conference on Information Technology and Applications in Biomedicine, Larnaca, Cyprus, 4–7 November 2009. [Google Scholar]
- Cheng, J.; Amft, O.; Lukowicz, P. Active Capacitive Sensing: Exploring a New Wearable Sensing Modality for Activity Recognition. In Proceedings of the 8th International Conference on Pervasive Computing; Springer: Berlin, Germany, 2010; pp. 319–336. [Google Scholar]
- Torsten, L.; Lena, G.; Geert, L. Contactless Emg Sensors Embroidered onto Textile. In 4th International Workshop on Wearable and Implantable Body Sensor Networks (Bsn 2007); Steffen, L., Thomas, F., Petri, M., Eds.; Springer: Berlin, Germany, 2007; pp. 29–34. [Google Scholar]
- Chi, Y.M.; Cauwenberghs, G. Wireless Non-Contact Eeg/Ecg Electrodes for Body Sensor Networks. In Proceedings of the 2010 International Conference on Body Sensor Networks (BSN), Singapore, 7–9 June 2010. [Google Scholar]
- Singh, N.; Singh, A.K.; Singh, V.K. Design and Performance of Wearable Ultrawide Band Textile Antenna for Medical Applications. Microwav. Opt. Technol. Lett. 2015, 57, 1553–1557. [Google Scholar] [CrossRef]
- Kumar, G.; Ray, K.P. Broadband Microstrip Antennas; Artech House: London, UK, 2003. [Google Scholar]
- Huang, C.T.; Tang, C.F.; Shen, C. A Wearable Textile for Monitoring Respiration, Using a Yarn-Based Sensor. In Proceedings of the 2006 10th IEEE International Symposium on Wearable Computers, Montreux, Switzerland, 11–14 October 2006. [Google Scholar]
- Lanlin, Z.; Zheyu, W.; Volakis, J.L. Textile Antennas and Sensors for Body-Worn Applications. Antennas Wirel. Propag. Lett. IEEE 2012, 11, 1690–1693. [Google Scholar]
- Sorin, F.; Abouraddy, A.F.; Orf, N.; Shapira, O.; Viens, J.; Arnold, J.; Joannopoulos, J.D.; Fink, Y. Multimaterial Photodetecting Fibers: A Geometric and Structural Study. Adv. Mater. 2007, 19, 3872–3877. [Google Scholar] [CrossRef]
- Egusa, S.; Wang, Z.; Chocat, N.; Ruff, Z.M.; Stolyarov, A.M.; Shemuly, D.; Sorin, F.; Rakich, P.T.; Joannopoulos, J.D.; Fink, Y. Multimaterial Piezoelectric Fibres. Nat. Mater. 2010, 9, 643–648. [Google Scholar] [CrossRef] [PubMed]
- Gorgutsa, S.; Blais-Roberge, M.; Viens, J.; LaRochelle, S.; Messaddeq, Y. User-Interactive and Wireless-Communicating RF Textiles. Adv. Mater. Technol. 2016, 1, 1600032. [Google Scholar] [CrossRef]
- Gorgutsa, S.; Khalil, M.; Belanger-Garnier, V.; Viens, J.; Gosselin, B.; LaRochelle, S.; Messaddeq, Y. Emissive Properties of Wearable Wireless-Communicating Textiles Made from Multimaterial Fibers. IEEE Trans. Antennas Propag. 2016, 64, 2457–2464. [Google Scholar] [CrossRef]
- Lobodzinski, S.S. Ecg Patch Monitors for Assessment of Cardiac Rhythm Abnormalities. Prog. Cardiovasc. Dis. 2013, 56, 224–229. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.-D.; Chung, W.-Y. Wireless Sensor Network Based Wearable Smart Shirt for Ubiquitous Health and Activity Monitoring. Sens. Actuators B Chem. 2009, 140, 390–395. [Google Scholar] [CrossRef]
- Warren, J.B.; Anderson, J.M. Newborn Respiratory Disorders. Pediatr. Rev. 2010, 31, 487. [Google Scholar] [CrossRef] [PubMed]
- Beardsell, I.; Bell, S.; Robinson, S.; Rumbold, H. Get through Mcem Part A: Mcqs; Hulbert, D., Ed.; CRC Press: Boca Raton, FL, USA, 2009. [Google Scholar]
- Moll, J.M.; Wright, V. An Objective Clinical Study of Chest Expansion. Ann. Rheum. Dis. 1972, 31, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Benet, W.E. The Mechanism of the Reaction of the Tollen Reagent. J. Chem. Res. 2011, 35, 675–677. [Google Scholar] [CrossRef]
- Dicke, R.H. A Computational Method Applicable to Microwave Networks. J. Appl. Phys. 1947, 18, 873–878. [Google Scholar] [CrossRef]
- Shaw, J.A. Radiometry and the Friis Transmission Equation. Am. J. Phys. 2013, 81, 33–37. [Google Scholar] [CrossRef]
- Camelia, G.; Sami, G. Compilation of the Dielectric Properties of Body Tissues at Rf and Microwave Frequencies; Brooks Air Force Base, Texas, Armstrong Laboratory (AFMC), Occupational and Environmental Health Directorate, Radiofrequency Radiation Division: San Antonio, TX, USA, 1998. [Google Scholar]
- Ida, N. Engineering Electromagnetics; Springer International Publishing: Cham, Switzerland, 2015. [Google Scholar]
- Moore, R.K. Effects of a Surrounding Conducting Medium on Antenna Analysis. Antennas Propag. IEEE Trans. 1963, 11, 216–225. [Google Scholar] [CrossRef]
- Jaehoon, K.; Rahmat-Samii, Y. Implanted Antennas inside a Human Body: Simulations, Designs, and Characterizations. Microw. Theory Tech. IEEE Trans. 2004, 52, 1934–1943. [Google Scholar]
- Ito, K. Human Body Phantoms for Evaluation of Wearable and Implantable Antennas. In Proceedings of the Second European Conference on Antennas and Propagation, EuCAP 2007, Edinburgh, UK, 11–16 November 2007. [Google Scholar]
- Karacolak, T.; Hood, A.Z.; Topsakal, E. Design of a Dual-Band Implantable Antenna and Development of Skin Mimicking Gels for Continuous Glucose Monitoring. Microw. Theory Tech. IEEE Trans. 2008, 56, 1001–1008. [Google Scholar] [CrossRef]
- Kramer, G.H.; Capello, K.; Bearrs, B.; Lauzon, A.; Normandeau, L. Linear Dimensions and Volumes of Human Lungs Obtained from Ct Images. Health Phys. 2012, 102, 378–383. [Google Scholar] [CrossRef] [PubMed]



© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guay, P.; Gorgutsa, S.; LaRochelle, S.; Messaddeq, Y. Wearable Contactless Respiration Sensor Based on Multi-Material Fibers Integrated into Textile. Sensors 2017, 17, 1050. https://doi.org/10.3390/s17051050
Guay P, Gorgutsa S, LaRochelle S, Messaddeq Y. Wearable Contactless Respiration Sensor Based on Multi-Material Fibers Integrated into Textile. Sensors. 2017; 17(5):1050. https://doi.org/10.3390/s17051050
Chicago/Turabian StyleGuay, Philippe, Stepan Gorgutsa, Sophie LaRochelle, and Younes Messaddeq. 2017. "Wearable Contactless Respiration Sensor Based on Multi-Material Fibers Integrated into Textile" Sensors 17, no. 5: 1050. https://doi.org/10.3390/s17051050
APA StyleGuay, P., Gorgutsa, S., LaRochelle, S., & Messaddeq, Y. (2017). Wearable Contactless Respiration Sensor Based on Multi-Material Fibers Integrated into Textile. Sensors, 17(5), 1050. https://doi.org/10.3390/s17051050





