An Intraoperative Visualization System Using Hyperspectral Imaging to Aid in Brain Tumor Delineation
Abstract
:1. Introduction
2. Materials and Methods
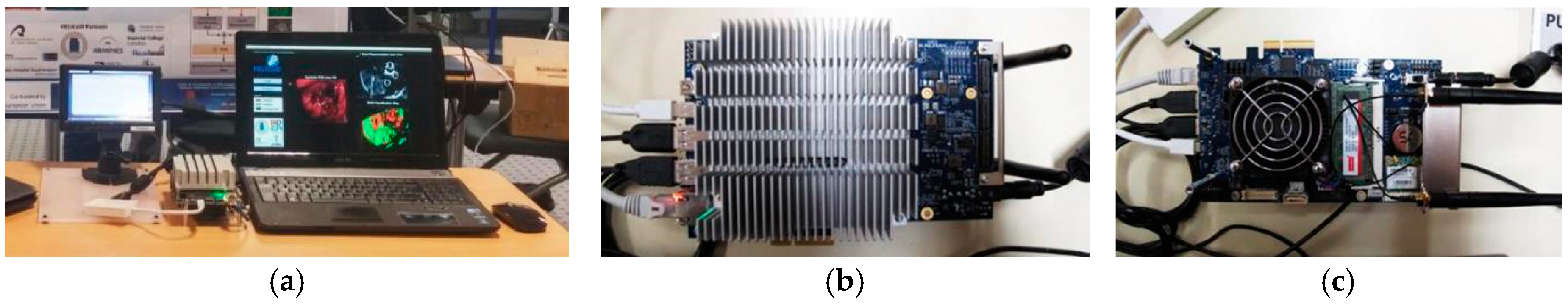
2.1. Acquisition Platform
2.1.1. Hyperspectral Cameras
- The Hyperspec® VNIR A-Series model covers spectral range from 400 to 1000 nm. It has a dispersion per pixel of 0.74 nm and a spectral resolution of 2–3 nm (with a 25-μm slit), and is able to capture 826 spectral bands and 1004 spatial pixels. This device integrates a silicon CCD detector array (Adimec 1000-m, Adimec Electronic Imaging, Inc., Woburn, MA, USA) with a minimum frame rate of 90 fps. This sensor is a monochromatic camera connected to the control unit using a PIXCI® Camera Link Interface (EPIX, Inc., Buffalo Grove, IL), which provides a data transmission rate up to 255 MB/s. The lens used in this camera is a Xenoplan 1.4 (Schneider Optics, Hauppauge, NY, USA) with a focal length of 22.5 mm and a broadband coating for the spectral range of 400 to 1000 nm.
- The Hyperspec® NIR 100/U model covers the spectral range from 900 to 1700 nm. It has a dispersion per pixel of 4.8 nm and a spectral resolution of 5 nm (with a 25-μm slit), being able to capture 172 spectral channels and 320 spatial pixels. This system incorporates an indium gallium arsenide (InGaAs) detector array (Xeneth XEVA 5052, Xenics nv, Leuven, Belgium), which provides a fast response, high quantum efficiency, and low dark current for the sensor area. This system has a frame rate of up to 100 fps. This camera is connected to the control unit by a USB 2.0 interface with a transfer rate up to 60 MB/s. The lens used with this camera is a Kowa LM25HC-SW 1.4 (Kowa Optimed Deutschland GmbH, Düsseldorf, Germany) with 25 mm of focal length and a broadband coating for the spectral range of 800–2000 nm.
2.1.2. Illumination System
2.1.3. Scanning Platform
2.1.4. Positioning Camera
2.1.5. Electromechanical Elements
2.2. Control Unit
HS Image Acquisition Software
2.3. Hardware Accelerator
2.4. HS Training Database
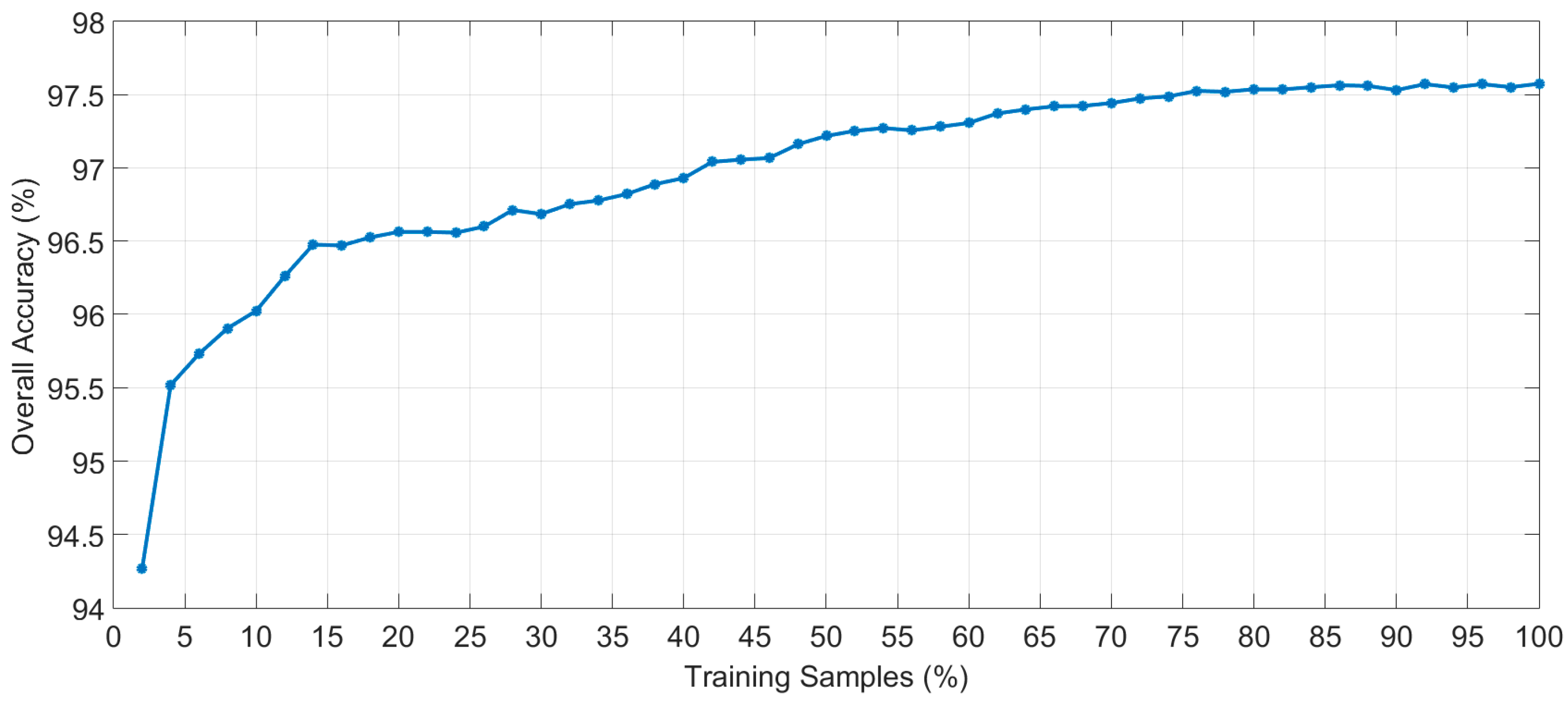
2.5. Brain Cancer Detection Algorithm Implementation
3. Experimental Results and Discussion
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Ethical Statements
References
- Improving Outcomes for People with Brain and Other CNS Tumours. Available online: https://www.nice.org.uk/guidance/csg10 (accessed on 30 January 2018).
- Louis, D.N.; Perry, A.; Reifenberger, G.; von Deimling, A.; Figarella-Branger, D.; Cavenee, W.K.; Ohgaki, H.; Wiestler, O.D.; Kleihues, P.; Ellison, D.W. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: A summary. Acta Neuropathol. 2016, 131, 803–820. [Google Scholar] [CrossRef] [PubMed]
- Robson, D.K. Pathology & Genetics. Tumours of the Nervous System. World Health Organisation ClassificationofTumours. J. Pathol. 2001, 193, 276. [Google Scholar] [CrossRef]
- Stummer, W.; Tonn, J.C.; Mehdorn, H.M.; Nestler, U.; Franz, K.; Goetz, C.; Bink, A.; Pichlmeier, U. Counterbalancing risks and gains from extended resections in malignant glioma surgery: A supplemental analysis from the randomized 5-aminolevulinic acid glioma resection study: Clinical article. J. Neurosurg. 2011, 114, 613–623. [Google Scholar] [CrossRef] [PubMed]
- Sanai, N.; Berger, M.S. Glioma extent of resection and its impact on patient outcome. Neurosurgery 2008, 62, 753–764. [Google Scholar] [CrossRef] [PubMed]
- Sanai, N.; Berger, M.S. Operative Techniques for Gliomas and the Value of Extent of Resection. Neurotherapeutics 2009, 6, 478–486. [Google Scholar] [CrossRef] [PubMed]
- Petrecca, K.; Guiot, M.; Panet-Raymond, V.; Souhami, L. Failure pattern following complete resection plus radiotherapy and temozolomide is at the resection margin in patients with glioblastoma. J. Neurooncol. 2013, 111, 19–23. [Google Scholar] [CrossRef] [PubMed]
- Gerard, I.J.; Kersten-Oertel, M.; Petrecca, K.; Sirhan, D.; Hall, J.A.; Collins, D.L. Brain shift in neuronavigation of brain tumors: A review. Med. Image Anal. 2017, 35, 403–420. [Google Scholar] [CrossRef] [PubMed]
- Kast, R.E.; Auner, G.W.; Rosenblum, M.L.; Mikkelsen, T.; Yurgelevic, S.M.; Raghunathan, A.; Poisson, L.M.; Kalkanis, S.N. Raman molecular imaging of brain frozen tissue sections. J. Neurooncol. 2014, 120, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Reinges, M.H.T.; Nguyen, H.H.; Krings, T.; Hütter, B.O.; Rohde, V.; Gilsbach, J.M.; Black, P.M.; Takakura, K.; Roberts, D.W. Course of brain shift during microsurgical resection of supratentorial cerebral lesions: Limits of conventional neuronavigation. Acta Neurochir. (Wien) 2004, 146, 369–377. [Google Scholar] [CrossRef] [PubMed]
- Nimsky, C.; Ganslandt, O.; Hastreiter, P.; Fahlbusch, R. Intraoperative compensation for brain shift. Surg. Neurol. 2001, 56, 357–364. [Google Scholar] [CrossRef]
- Ganser, K.A.; Dickhaus, H.; Staubert, A.; Bonsanto, M.M.; Wirtz, C.R.; Tronnier, V.M.; Kunze, S. Quantification of brain shift effects in MRI images. Biomed. Tech. (Berl.) 1997, 42, 247–248. [Google Scholar] [CrossRef] [PubMed]
- Stummer, W.; Pichlmeier, U.; Meinel, T.; Wiestler, O.D.; Zanella, F.; Reulen, H.J. Fluorescence-guided surgery with 5-aminolevulinic acid for resection of malignant glioma: a randomised controlled multicentre phase III trial. Lancet Oncol. 2006, 7, 392–401. [Google Scholar] [CrossRef]
- Floeth, F.W.; Sabel, M.; Ewelt, C.; Stummer, W.; Felsberg, J.; Reifenberger, G.; Steiger, H.J.; Stoffels, G.; Coenen, H.H.; Langen, K.J. Comparison of 18F-FET PET and 5-ALA fluorescence in cerebral gliomas. Eur. J. Nucl. Med. Mol. Imaging 2011, 38, 731–741. [Google Scholar] [CrossRef] [PubMed]
- Lu, G.; Fei, B. Medical hyperspectral imaging: A review. J. Biomed. Opt. 2014, 19, 10901. [Google Scholar] [CrossRef] [PubMed]
- Calin, M.A.; Parasca, S.V.; Savastru, D.; Manea, D. Hyperspectral imaging in the medical field: Present and future. Appl. Spectrosc. Rev. 2014, 49, 435–447. [Google Scholar] [CrossRef]
- Akbari, H.; Uto, K.; Kosugi, Y.; Kojima, K.; Tanaka, N. Cancer detection using infrared hyperspectral imaging. Cancer Sci. 2011, 102, 852–857. [Google Scholar] [CrossRef] [PubMed]
- Regeling, B.; Thies, B.; Gerstner, A.O.H.; Westermann, S.; Müller, N.A.; Bendix, J.; Laffers, W. Hyperspectral Imaging Using Flexible Endoscopy for Laryngeal Cancer Detection. Sensors 2016, 16, 1288. [Google Scholar] [CrossRef] [PubMed]
- Kester, R.T.; Bedard, N.; Gao, L.; Tkaczyk, T.S. Real-time snapshot hyperspectral imaging endoscope. J. Biomed. Opt. 2011, 16, 56005. [Google Scholar] [CrossRef] [PubMed]
- Akbari, H.; Halig, L.V.; Schuster, D.M.; Osunkoya, A.; Master, V.; Nieh, P.T.; Chen, G.Z.; Fei, B. Hyperspectral imaging and quantitative analysis for prostate cancer detection. J. Biomed. Opt. 2012, 17, 760051. [Google Scholar] [CrossRef] [PubMed]
- Hou, Y.; Ren, Z.; Liu, G.; Zeng, L.; Huang, Z. Design of a novel LD-induced hyper-spectral imager for breast cancer diagnosis based on VHT grating. In Proceedings of the 2011 Symposium on Photonics and Optoelectronics, Wuhan, China, 16–18 May 2011. [Google Scholar]
- Kim, B.; Kehtarnavaz, N.; LeBoulluec, P.; Liu, H.; Peng, Y.; Euhus, D. Automation of ROI extraction in hyperspectral breast images. In Proceedings of the 2013 35th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Osaka, Japan, 3–7 July 2013; Volume 2013, pp. 3658–3661. [Google Scholar] [CrossRef]
- Pourreza-Shahri, R.; Saki, F.; Kehtarnavaz, N.; Leboulluec, P.; Liu, H. Classification of ex-vivo breast cancer positive margins measured by hyperspectral imaging. In Proceedings of the 2013 IEEE International Conference on Image Processing, ICIP 2013—Proceedings, Melbourne, VIC, Australia, 15–18 September 2013; pp. 1408–1412. [Google Scholar]
- Han, Z.; Zhang, A.; Wang, X.; Sun, Z.; Wang, M.D.; Xie, T. In vivo use of hyperspectral imaging to develop a noncontact endoscopic diagnosis support system for malignant colorectal tumors. J. Biomed. Opt. 2016, 21, 16001. [Google Scholar] [CrossRef] [PubMed]
- Masood, K.; Rajpoot, N.M. Texture based classification of hyperspectral colon biopsy samples using CLBP. In Proceedings of the IEEE International Symposium on Biomedical Imaging: From Nano to Macro, 2009, ISBI 09, Boston, MA, USA, 28 June–1 July 2009; pp. 1011–1014. [Google Scholar] [CrossRef]
- Masood, K.; Rajpoot, N.; Rajpoot, K.; Qureshi, H. Hyperspectral Colon Tissue Classification using Morphological Analysis. In Proceedings of the International Conference on Emerging Technologies, Peshawar, Pakistan, 13–14 Novrmber 2006; pp. 735–741. [Google Scholar]
- Rajpoot, K.M.; Rajpoot, N.M. Wavelet based segmentation of hyperspectral colon tissue imagery. In Proceedings of the INMIC 2003: IEEE 7th International Multi Topic Conference, Islamabad, Pakistan, 8–9 December 2003; pp. 38–43. [Google Scholar]
- Dicker, D.T.; Lerner, J.; Van Belle, P.; Barth, S.F.; Guerry, D., 4th; Herlyn, M.; Elder, D.E.; El-Deiry, W.S. Differentiation of normal skin and melanoma using high resolution hyperspectral imaging. Cancer Biol. Ther. 2006, 5, 1033–1038. [Google Scholar] [CrossRef] [PubMed]
- Gaudi, S.; Meyer, R.; Ranka, J.; Granahan, J.C.; Israel, S.A.; Yachik, T.R.; Jukic, D.M. Hyperspectral Imaging of Melanocytic Lesions. Am. J. Dermatopathol. 2014, 36, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Akbari, H.; Halig, L.V.; Zhang, H.; Wang, D.; Chen, Z.G.; Fei, B. Detection of Cancer Metastasis Using a Novel Macroscopic Hyperspectral Method. Proc. SPIE 2012, 8317, 831711. [Google Scholar] [CrossRef]
- Laffers, W.; Westermann, S.; Regeling, B.; Martin, R.; Thies, B.; Gerstner, A.O.H.; Bootz, F.; Müller, N.A. Early recognition of cancerous lesions in the mouth and oropharynx: Automated evaluation of hyperspectral image stacks. HNO 2015. [Google Scholar] [CrossRef]
- Zhi, L.; Zhang, D.; Yan, J.Q.; Li, Q.L.; Tang, Q.L. Classification of hyperspectral medical tongue images for tongue diagnosis. Comput. Med. Imaging Graph. 2007, 31, 672–678. [Google Scholar]
- Liu, Z.; Wang, H.; Li, Q. Tongue tumor detection in medical hyperspectral images. Sensors 2012, 12, 162–174. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Yan, J.; Zhang, D.; Li, Q.-L. Automated tongue segmentation in hyperspectral images for medicine. Appl. Opt. 2007, 46, 8328–8334. [Google Scholar] [CrossRef] [PubMed]
- Akbari, H.; Kosugi, Y.; Kojima, K.; Tanaka, N. Blood vessel detection and artery-vein differentiation using hyperspectral imaging. In Proceedings of the 31st Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Minneapolis, MN, USA, 3–6 September 2009; pp. 1461–1464. [Google Scholar] [CrossRef]
- Akbari, H.; Kosugi, Y.; Kojima, K.; Tanaka, N. Detection and Analysis of the Intestinal Ischemia Using Visible and Invisible Hyperspectral Imaging. IEEE Trans. Biomed. Eng. 2010, 57, 2011–2017. [Google Scholar] [CrossRef] [PubMed]
- Jayanthi, J.L.; Nisha, G.U.; Manju, S.; Philip, E.K.; Jeemon, P.; Baiju, K.V.; Beena, V.T.; Subhash, N. Diffuse reflectance spectroscopy: diagnostic accuracy of a non-invasive screening technique for early detection of malignant changes in the oral cavity. BMJ Open 2011, 1, e000071. [Google Scholar] [CrossRef] [PubMed]
- Kabwama, S.; Bulters, D.; Bulstrode, H.; Fabelo, H.; Ortega, S.; Callico, G.M.; Stanciulescu, B.; Kiran, R.; Ravi, D.; Szolna, A.; et al. Intra-operative hyperspectral imaging for brain tumour detection and delineation: Current progress on the HELICoid project. Int. J. Surg. 2016, 36, S140. [Google Scholar] [CrossRef]
- Salvador, R.; Ortega, S.; Madroñal, D.; Fabelo, H.; Lazcano, R.; Marrero, G.; Juárez, E.; Sarmiento, R.; Sanz, C. HELICoiD: Interdisciplinary and collaborative project for real-time brain cancer detection. In Proceedings of the ACM International Conference on Computing Frontiers 2017, CF 2017, Siena, Italy, 15–17 May 2017. [Google Scholar]
- Szolna, A.; Morera, J.; Piñeiro, J.F.; Callicó, G.M.; Fabelo, H.; Ortega, S. Hyperspectral Imaging as A Novel Instrument for Intraoperative Brain Tumor Detection. Neurocirugia 2016, 27, 166. [Google Scholar]
- Fabelo, H.; Ortega, S.; Kabwama, S.; Callico, G.M.; Bulters, D.; Szolna, A.; Pineiro, J.F.; Sarmiento, R. HELICoiD project: A new use of hyperspectral imaging for brain cancer detection in real-time during neurosurgical operations. In Proceedings of the SPIE 9860, Hyperspectral Imaging Sensors: Innovative Applications and Sensor Standards 2016; SPIE- Commercial + Scientific Sensing and Imaging, Baltimore, MD, USA, 17–21 April 2016. [Google Scholar]
- Salvador, R.; Fabelo, H.; Lazcano, R.; Ortega, S.; Madroñal, D.; Callicó, G.M.; Juárez, E.; Sanz, C. Demo: HELICoiD tool demonstrator for real-time brain cancer detection. In Proceedings of the Conference on Design and Architectures for Signal and Image Processing, DASIP, Rennes, France, 12–14 October 2016. [Google Scholar]
- Fabelo, H.; Ortega, S.; Guerra, R.; Callicó, G.; Szolna, A.; Piñeiro, J.F.; Tejedor, M.; López, S.; Sarmiento, R. A novel use of hyperspectral images for human brain cancer detection using in-vivo samples. In Proceedings of the BIOSIGNALS 2016–9th International Conference on Bio-Inspired Systems and Signal Processing; Part of 9th International Joint Conference on Biomedical Engineering Systems and Technologies, BIOSTEC 2016, Rome, Italy, 21–23 February 2016. [Google Scholar]
- Madroñal, D.; Fabelo, H.; Lazcano, R.; Callicó, G.M.; Juárez, E.; Sanz, C. Parallel implementation of a hyperspectral image linear SVM classifier using RVC-CAL. In Proceedings of the SPIE–The International Society for Optical Engineering, Edinburgh, UK, 26–29 September 2016; Volume 10007. [Google Scholar]
- Lazcano, R.; Madroñal, D.; Salvador, R.; Desnos, K.; Pelcat, M.; Guerra, R.; Fabelo, H.; Ortega, S.; Lopez, S.; Callico, G.M.; Juarez, E.; Sanz, C. Porting a PCA-based hyperspectral image dimensionality reduction algorithm for brain cancer detection on a manycore architecture. J. Syst. Archit. 2017, 77, 101–111. [Google Scholar] [CrossRef]
- Wu, D.; Sun, D.-W. Advanced applications of hyperspectral imaging technology for food quality and safety analysis and assessment: A review—Part I: Fundamentals. Innov. Food Sci. Emerg. Technol. 2013, 19, 1–14. [Google Scholar] [CrossRef]
- Elvidge, C.D.; Keith, D.M.; Tuttle, B.T.; Baugh, K.E. Spectral identification of lighting type and character. Sensors 2010, 10, 3961–3988. [Google Scholar] [CrossRef] [PubMed]
- Quinn, P.J. Effects of temperature on cell membranes. Symp. Soc. Exp. Biol. 1988, 42, 237–258. [Google Scholar] [PubMed]
- Akbari, H.; Kosugi, Y. Hyperspectral imaging: A new modality in surgery. In Recent Advances in Biomedical Engineering; InTech: London, UK, 2009. [Google Scholar]
- De Dinechin, B.D.; Ayrignac, R.; Beaucamps, P.E.; Couvert, P.; Ganne, B.; De Massas, P.G.; Jacquet, F.; Jones, S.; Chaisemartin, N.M.; Riss, F.; et al. A clustered manycore processor architecture for embedded and accelerated applications. In Proceedings of the 2013 IEEE High Performance Extreme Computing Conference, HPEC 2013, Waltham, MA, USA, 10–12 September 2013. [Google Scholar]
- Madroñal, D.; Lazcano, R.; Fabelo, H.; Ortega, S.; Salvador, R.; Callicó, G.M.; Juarez, E.; Sanz, C. Energy consumption characterization of a Massively Parallel Processor Array (MPPA) platform running a hyperspectral SVM classifier. In Proceedings of the 2017 Conference on Design and Architectures for Signal and Image Processing, DASIP, Dresden, Germany, 27–29 September 2017. [Google Scholar]
- Chang, C.-I. New hyperspectral discrimination measure for spectral characterization. Opt. Eng. 2004, 43, 1777. [Google Scholar] [CrossRef]
- Madroñal, D.; Lazcano, R.; Salvador, R.; Fabelo, H.; Ortega, S.; Callico, G.M.; Juarez, E.; Sanz, C. SVM-based real-time hyperspectral image classifier on a manycore architecture. J. Syst. Archit. 2017, 80. [Google Scholar] [CrossRef]








| Class | #Patients | #Labelled Pixels | ||
|---|---|---|---|---|
| Normal | 21 | 117,242 | ||
| Tumor | Primary (G-IV) | GBM | 8 | 12,641 |
| Primary (G-III) | Anaplastic Oligodendroglioma | 2 | 1844 | |
| Secondary | Lung | 2 | 1936 | |
| Renal | 1 | 21 | ||
| Breast | 1 | 325 | ||
| Blood Vessel/Hypervascularized Tissue | 22 | 57,429 | ||
| Background | 21 | 186,118 | ||
| Total (22 Patients, 36 Captures): | 377,556 | |||
| Image ID | Size (MB) | #Pixels | Dimension (Width × Height × Bands) | Pathological Diagnosis |
|---|---|---|---|---|
| P1C1 | 362.62 | 224,770 | 495 × 456 × 826 | Normal Brain |
| P1C2 | 197.90 | 122,670 | 471 × 262 × 826 | Primary Grade II Oligodendroglioma |
| P2C1 | 225.35 | 139,682 | 332 × 423 × 826 | Normal Brain |
| P2C2 | 276.99 | 171,699 | 364 × 474 × 826 | Primary GBM |
| P3C1 | 402.26 | 249,344 | 513 × 488 × 826 | Normal Brain |
| P3C2 | 230.34 | 143,560 | 485 × 296 × 826 | Primary GBM |
| P4C1 | 372.47 | 230,878 | 480 × 483 × 826 | Primary Grade I Meningioma |
| Image ID | Processing Type | Acquisition Time (s) | Pre-Processing (s) | Transmission (s) | PCA + SVM (s) | KNN (s) | HKM (s) | MV (s) | Total Processing Time (s) |
|---|---|---|---|---|---|---|---|---|---|
| P1C1 | Seq. | 19.98 | 15.07 | 0.00 | 11.32 | 378.87 | 39.68 | 0.009 | 444.95 |
| Acc. | 14.00 | 6.02 | 8.16 | 68.76 * | |||||
| Speedup | N/A ¥ | N/A ¥ | 0.00 | 1.88 | 46.45 | N/A ¥ | N/A ¥ | 6.47 | |
| P1C2 | Seq. | 19.02 | 6.50 | 0.00 | 5.90 | 196.64 | 21.87 | 0.004 | 230.92 |
| Acc. | 7.15 | 4.35 | 4.23 | 35.53 * | |||||
| Speedup | N/A ¥ | N/A ¥ | 0.00 | 1.36 | 46.44 | N/A ¥ | N/A ¥ | 6.50 | |
| P2C1 | Seq. | 13.40 | 9.35 | 0.00 | 6.72 | 158.66 | 24.96 | 0.005 | 199.70 |
| Acc. | 8.07 | 4.48 | 3.48 | 42.38 * | |||||
| Speedup | N/A ¥ | N/A ¥ | 0.00 | 1.50 | 45.62 | N/A ¥ | N/A ¥ | 4.71 | |
| P2C2 | Seq. | 14.70 | 12.59 | 0.00 | 8.96 | 212.96 | 30.45 | 0.006 | 264.97 |
| Acc. | 9.56 | 5.02 | 4.66 | 52.61 * | |||||
| Speedup | N/A ¥ | N/A ¥ | 0.00 | 1.78 | 45.74 | N/A ¥ | N/A ¥ | 5.04 | |
| P3C1 | Seq. | 20.71 | 19.72 | 0.00 | 13.68 | 434.96 | 44.57 | 0.008 | 512.93 |
| Acc. | 13.34 | 6.72 | 9.44 | 77.63 * | |||||
| Speedup | N/A ¥ | N/A ¥ | 0.00 | 2.03 | 46.10 | N/A ¥ | N/A ¥ | 6.61 | |
| P3C2 | Seq. | 19.58 | 8.94 | 0.00 | 7.73 | 234.90 | 25.75 | 0.005 | 277.33 |
| Acc. | 9.45 | 4.66 | 5.08 | 44.15 * | |||||
| Speedup | N/A ¥ | N/A ¥ | 0.00 | 1.66 | 46.27 | N/A ¥ | N/A ¥ | 6.28 | |
| P4C1 | Seq. | 19.38 | 13.84 | 0.00 | 11.49 | 377.60 | 41.59 | 0.007 | 444.52 |
| Acc. | 12.36 | 6.29 | 8.15 | 67.79 * | |||||
| Speedup | N/A ¥ | N/A ¥ | 0.00 | 1.83 | 46.34 | N/A ¥ | N/A ¥ | 6.56 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fabelo, H.; Ortega, S.; Lazcano, R.; Madroñal, D.; M. Callicó, G.; Juárez, E.; Salvador, R.; Bulters, D.; Bulstrode, H.; Szolna, A.; et al. An Intraoperative Visualization System Using Hyperspectral Imaging to Aid in Brain Tumor Delineation. Sensors 2018, 18, 430. https://doi.org/10.3390/s18020430
Fabelo H, Ortega S, Lazcano R, Madroñal D, M. Callicó G, Juárez E, Salvador R, Bulters D, Bulstrode H, Szolna A, et al. An Intraoperative Visualization System Using Hyperspectral Imaging to Aid in Brain Tumor Delineation. Sensors. 2018; 18(2):430. https://doi.org/10.3390/s18020430
Chicago/Turabian StyleFabelo, Himar, Samuel Ortega, Raquel Lazcano, Daniel Madroñal, Gustavo M. Callicó, Eduardo Juárez, Rubén Salvador, Diederik Bulters, Harry Bulstrode, Adam Szolna, and et al. 2018. "An Intraoperative Visualization System Using Hyperspectral Imaging to Aid in Brain Tumor Delineation" Sensors 18, no. 2: 430. https://doi.org/10.3390/s18020430
APA StyleFabelo, H., Ortega, S., Lazcano, R., Madroñal, D., M. Callicó, G., Juárez, E., Salvador, R., Bulters, D., Bulstrode, H., Szolna, A., Piñeiro, J. F., Sosa, C., J. O’Shanahan, A., Bisshopp, S., Hernández, M., Morera, J., Ravi, D., Kiran, B. R., Vega, A., ... Sarmiento, R. (2018). An Intraoperative Visualization System Using Hyperspectral Imaging to Aid in Brain Tumor Delineation. Sensors, 18(2), 430. https://doi.org/10.3390/s18020430








