A Miniature Bio-Photonics Companion Diagnostics Platform for Reliable Cancer Treatment Monitoring in Blood Fluids
Abstract
1. Introduction
2. Materials and Methods
2.1. Integrated Optical Sensing Chips
2.2. Bio-Modification of the Photonic Chips
2.3. Microfluidic Cartridge
2.4. Optical Measurement Experimental Setups
2.5. Integrated Photonic Biosensor Device for Cancer Treatment Monitoring
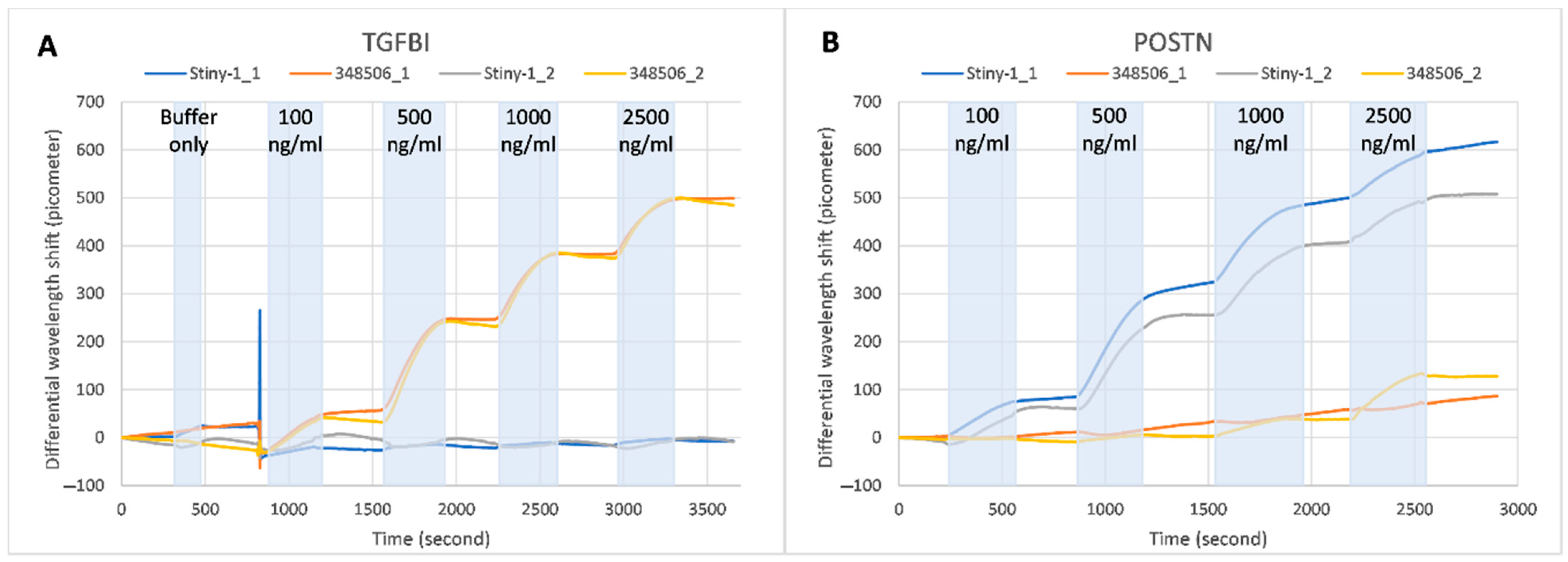
3. Results and Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Use of ‘-Omics’ Technologies in the Development of Personalised Medicine. 2013. Available online: https://ec.europa.eu/research/health/pdf/2013-10_personalised_medicine_en.pdf (accessed on 25 October 2013).
- Paving the Way for Personalized Medicine, FDA’s Role in a New Era of Medical Product Development. Available online: https://www.fdanews.com/ext/resources/files/10/10-28-13-Personalized-Medicine.pdf (accessed on 30 October 2013).
- The Global Cancer Observatory (GCO). Available online: http://globocan.iarc.fr/Default.aspx (accessed on 3 February 2021).
- Gupta, G.P.; Massague, J. Cancer Metastasis: Building a Framework. Cell 2006, 127, 679–695. [Google Scholar] [CrossRef] [PubMed]
- Prabhakar, B.; Shende, P.; Augustine, S. Current trends and emerging diagnostic techniques for lung cancer. Biomed. Pharmacother. 2018, 106, 1586. [Google Scholar] [CrossRef] [PubMed]
- Altintas, Z.; Tothill, I. Biomarkers and biosensors for the early diagnosis of lung cancer. Sens. Actuators B Chem. 2013, 188, 988–998. [Google Scholar] [CrossRef]
- Mittal, S.; Kaur, H.; Gautam, N.; Mantha, A.K. Biosensors for breast cancer diagnosis: A review of bioreceptors, biotransducers and signal amplification strategies. Biosens. Bioelectron. 2017, 88, 217–231. [Google Scholar] [CrossRef] [PubMed]
- Jayanthi, S.; Das, A.B.; Saxena, U. Recent advances in biosensor development for the detection of cancer biomarkers. Biosens. Bioelectron. 2017, 91, 15–23. [Google Scholar] [CrossRef]
- Chikkaveeraiah, B.V.; Bhirde, A.A.; Morgan, N.Y.; Eden, H.S.; Chen, X. Electrochemical immunosensors for detection of cancer protein biomarkers. ACS Nano 2012, 6, 6546–6561. [Google Scholar] [CrossRef]
- Jeronimo, P.C.; Araujo, A.N.; Montenegro, M.C.B. Optical sensors and biosensors based on sol-gel films. Talanta 2007, 72, 13–27. [Google Scholar] [CrossRef]
- Hoß, S.G.; Bendas, G. Mass-Sensitive Biosensor Systems to Determine the Membrane Interaction of Analytes. Methods Mol. Biol. 2017, 1520, 145–157. [Google Scholar]
- Mahato, K.; Kumar, A.; Maurya, P.K.; Chandra, P. Shifting paradigm of cancer diagnoses in clinically relevant samples based on miniaturized electrochemical nanobiosensors and microfluidic devices. Biosens. Bioelectron. 2018, 100, 411–428. [Google Scholar] [CrossRef]
- Freitas, M.; Nouws, H.P.A.; Delerue-Matos, C. Electrochemical Biosensing in Cancer Diagnostics and Follow-up. Electroanalysis 2018, 30, 1576–1603. [Google Scholar] [CrossRef]
- Fan, X.; White, I.M.; Shopova, S.I.; Zhu, H.; Suter, J.D.; Sun, Y. Sensitive optical biosensors for unlabeled targets: A review. Anal. Chim. Acta 2008, 620, 8–26. [Google Scholar] [CrossRef] [PubMed]
- Heideman, R.G.; Leinse, A.; Geuzebroek, D.H.; Schreuder, F.; Falke, F.; Zergioti, I.; van der Meer, A.; Schuetz-Trilling, A.; Scheres, L.; Vestering-Stenger, R. Ultra-sensitive photonic integrated circuit-based biosensors for healthcare applications. In Proceedings of the Integrated Optics: Devices, Materials, and Technologies XXIV, San Francisco, CA, USA, 3–6 February 2020; p. 112830Q. [Google Scholar]
- Besselink, G.A.J.; Heideman, R.G.; Schreuder, E.; Wevers, L.S.; Falke, F. Performance of Arrayed Microring Resonator Sensors with the TriPleX Platform. J. Biosens. Bioelectron. 2016, 7, 1000209. [Google Scholar]
- Wörhoff, K.; Heideman, R.G.; Leinse, A.; Hoekman, M. TriPleX: A versatile dielectric photonic platform. Adv. Opt. Technol. 2015, 4, 189–207. [Google Scholar] [CrossRef]
- Gounaridis, L.; Groumas, P.; Schreuder, E.; Heideman, R.; Avramopoulos, H.; Kouloumentas, C. New set of design rules for resonant refractive index sensors enabled by FFT based processing of the measurement data. Opt. Express 2016, 24, 7611–7632. [Google Scholar] [CrossRef]
- Gounaridis, L.; Groumas, P.; Schreuder, E.; Tsekenis, G.; Marousis, A.; Heideman, R.; Avramopoulos, H.; Kouloumentas, C. High performance refractive index sensor based on low Q-factor ring resonators and FFT processing of wavelength scanning data. Opt. Express 2017, 25, 7483–7495. [Google Scholar] [CrossRef]
- Rosso, M.; Giesbers, M.; Arafat, A.; Schroën, K.; Zuilhof, H. Covalently Attached Organic Monolayers on SiC and SixN4 Surfaces: Formation Using UV Light at Room Temperature. Langmuir 2009, 25, 2172–2180. [Google Scholar] [CrossRef]
- To, T.D.; Le, H.T.; Dinh, M.N.; Nguyen, A.T.; Doan, T.C.; Dang, C.M. Chemical modification of silicon nitride microsieves for capture of MCF-7 circulating tumor cells of breast cancer. Adv. Nat. Sci. Nanosci. Nanotechnol. 2015, 6, 025006. [Google Scholar] [CrossRef]
- Chatzipetrou, M.; Massaouti, M.; Tsekenis, G.; Trilling, A.K.; van Andel, E.; Scheres, L.; Smulders, M.M.J.; Zuilhof, H.; Zergioti, I. Direct Creation of Biopatterns via a Combination of Laser-Based Techniques and Click Chemistry. Langmuir 2017, 33, 848–853. [Google Scholar] [CrossRef]
- Then, W.L.; Aguilar, M.I.; Garnier, G. Quantitative Detection of Weak D Antigen Variants in Blood Typing using SPR. Sci. Rep. 2017, 7, 1616. [Google Scholar] [CrossRef] [PubMed]
- Crauste, C.; Willand, N.; Villemagne, B.; Flipo, M.; Willery, E.; Carette, X.; Dimala, M.M.; Drucbert, A.S.; Danze, P.M.; Deprez, B.; et al. Unconventional surface plasmon resonance signals reveal quantitative inhibition of transcriptional repressor EthR by synthetic ligands. Anal. Biochem. 2014, 452, 54–66. [Google Scholar] [CrossRef]
- Fraire, J.C.; Motrich, R.D.; Coronado, E.A. Design of a novel plasmonic nanoconjugated analytical tool for ultrasensitive antigen quantification. Nanoscale 2016, 8, 17169–17180. [Google Scholar] [CrossRef] [PubMed]
- Gounaridis, L.; Groumas, P.; Schreuder, E.; Tsokos, C.; Mylonas, E.; Raptakis, A.; Heideman, R.; Avramopoulos, H.; Kouloumentas, C. Design of ultra-compact multimode interference (MMI) couplers and high efficiency grating couplers in TriPleX platform as part of a photonic-based sensor. In Proceedings of the Integrated Optics: Devices, Materials, and Technologies XXIII, San Francisco, CA, USA, 29 January–1 February 2018; Volume 10921, p. 1092127. [Google Scholar]
- Gounaridis, L.; Groumas, P.; Schreuder, E.; Heideman, R.; Katopodis, V.; Kouloumentas, C.; Avramopoulos, H. Design of grating couplers and MMI couplers on the TriPleX platform enabling ultra-compact photonic-based biosensors. Sens. Actuators B Chem. 2015, 209, 1057–1063. [Google Scholar] [CrossRef]









Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chatzipetrou, M.; Gounaridis, L.; Tsekenis, G.; Dimadi, M.; Vestering-Stenger, R.; F. Schreuder, E.; Trilling, A.; Besselink, G.; Scheres, L.; van der Meer, A.; et al. A Miniature Bio-Photonics Companion Diagnostics Platform for Reliable Cancer Treatment Monitoring in Blood Fluids. Sensors 2021, 21, 2230. https://doi.org/10.3390/s21062230
Chatzipetrou M, Gounaridis L, Tsekenis G, Dimadi M, Vestering-Stenger R, F. Schreuder E, Trilling A, Besselink G, Scheres L, van der Meer A, et al. A Miniature Bio-Photonics Companion Diagnostics Platform for Reliable Cancer Treatment Monitoring in Blood Fluids. Sensors. 2021; 21(6):2230. https://doi.org/10.3390/s21062230
Chicago/Turabian StyleChatzipetrou, Marianneza, Lefteris Gounaridis, George Tsekenis, Maria Dimadi, Rachel Vestering-Stenger, Erik F. Schreuder, Anke Trilling, Geert Besselink, Luc Scheres, Adriaan van der Meer, and et al. 2021. "A Miniature Bio-Photonics Companion Diagnostics Platform for Reliable Cancer Treatment Monitoring in Blood Fluids" Sensors 21, no. 6: 2230. https://doi.org/10.3390/s21062230
APA StyleChatzipetrou, M., Gounaridis, L., Tsekenis, G., Dimadi, M., Vestering-Stenger, R., F. Schreuder, E., Trilling, A., Besselink, G., Scheres, L., van der Meer, A., Lindhout, E., G. Heideman, R., Leeuwis, H., Graf, S., Volden, T., Ningler, M., Kouloumentas, C., Strehle, C., Revol, V., ... Zergioti, I. (2021). A Miniature Bio-Photonics Companion Diagnostics Platform for Reliable Cancer Treatment Monitoring in Blood Fluids. Sensors, 21(6), 2230. https://doi.org/10.3390/s21062230








