Three-Dimensional Quantitative Evaluation of the Scapular Skin Marker Movements in the Upright Posture
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
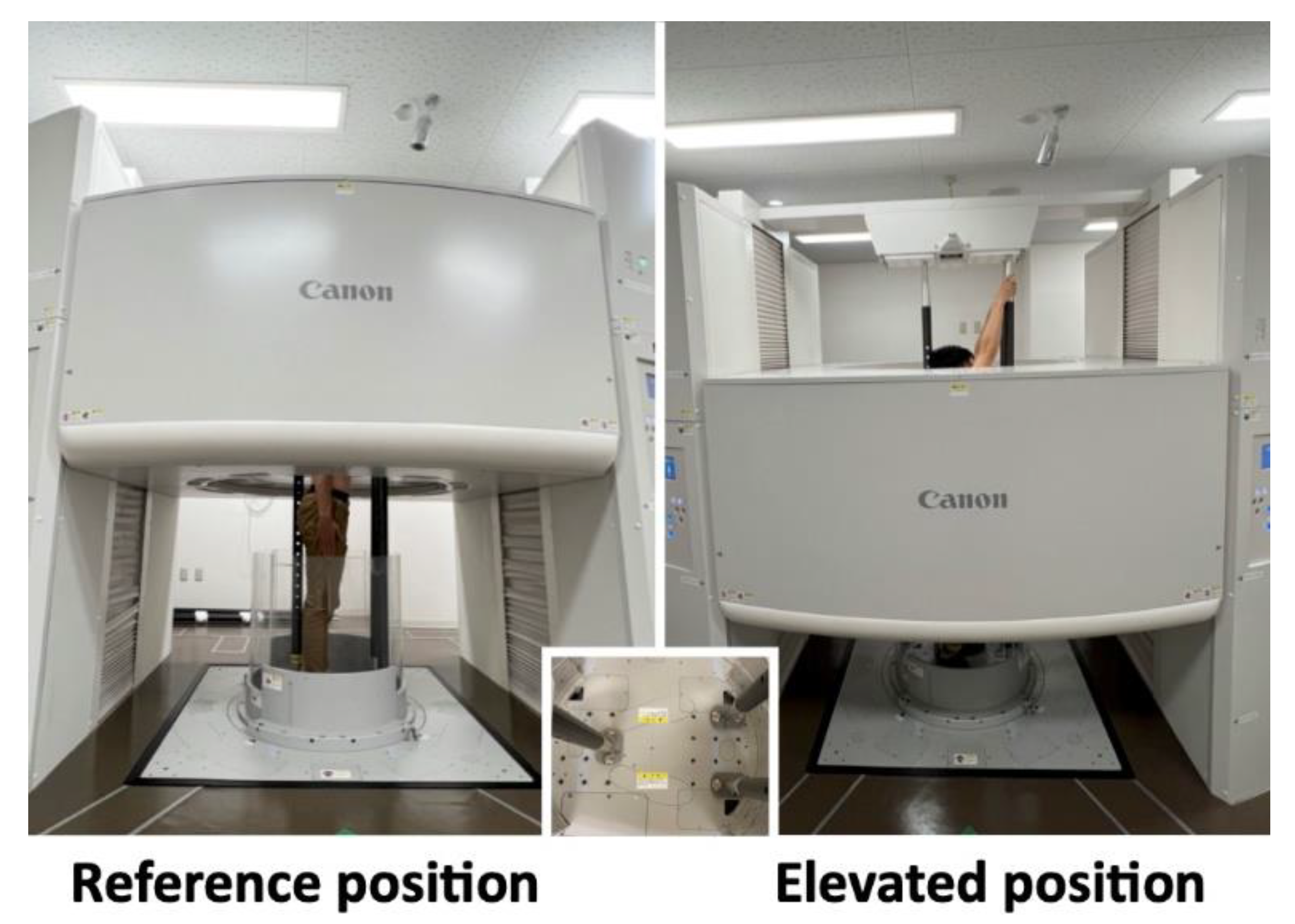
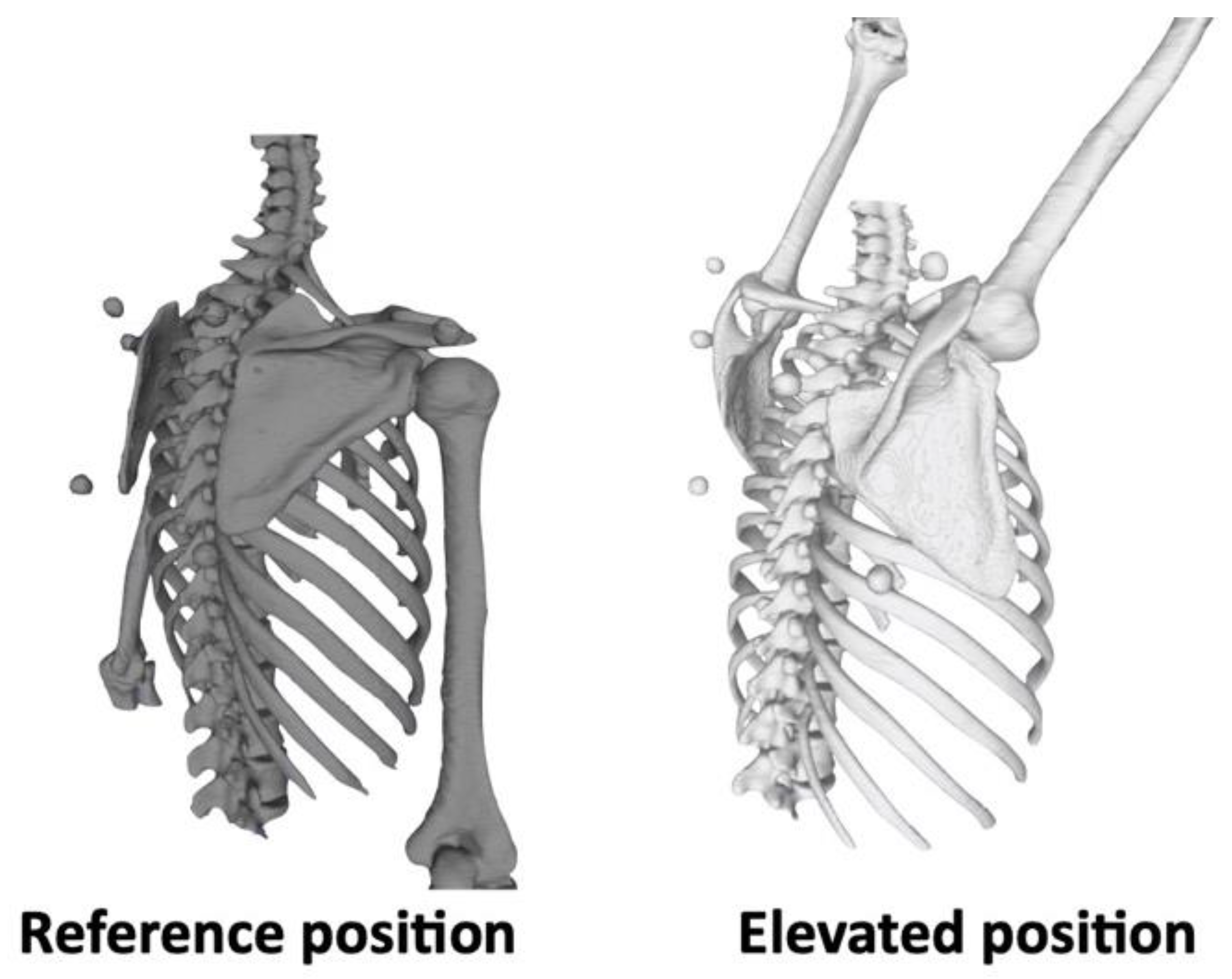
2.2. Image Acquisition
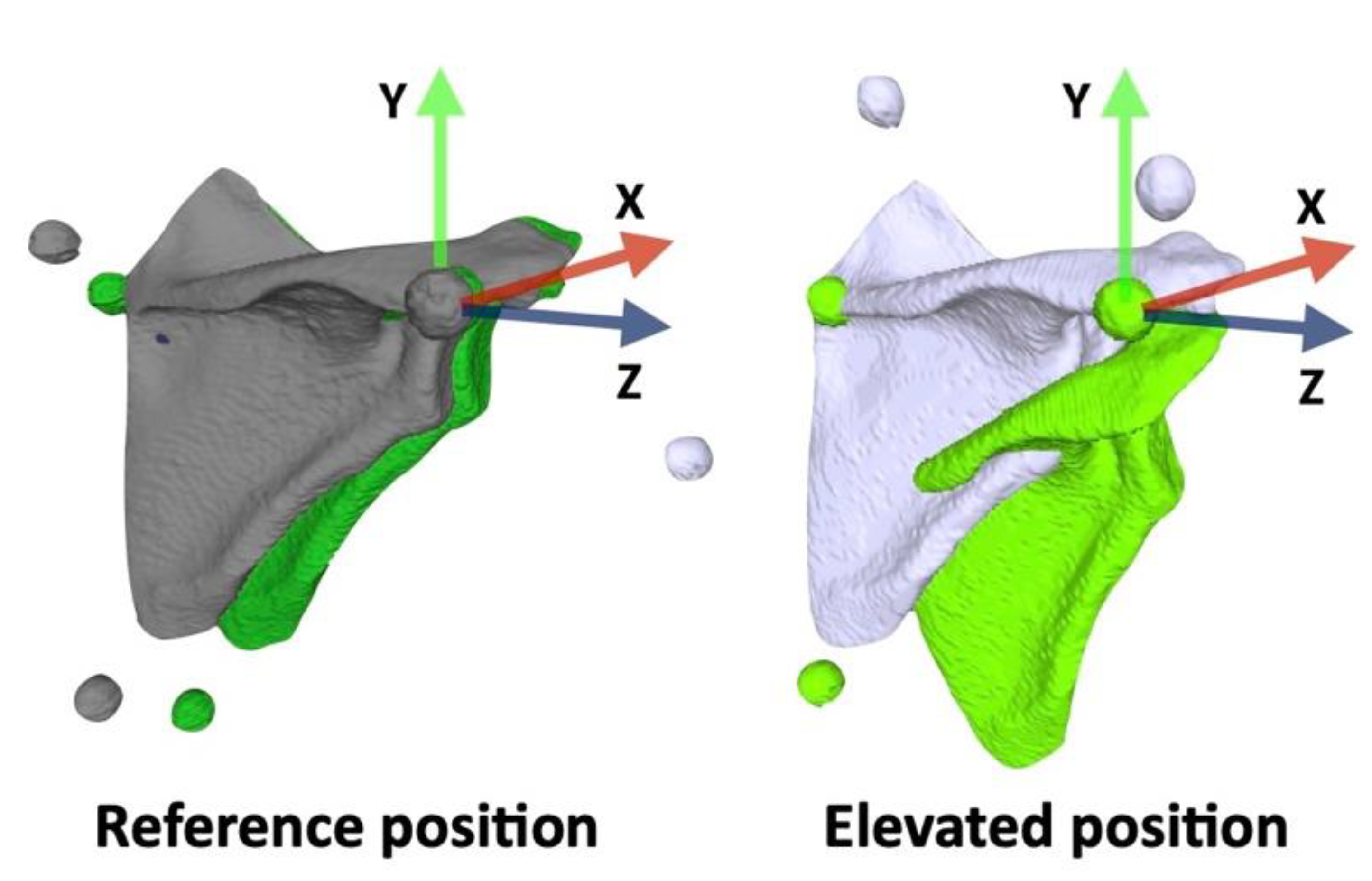
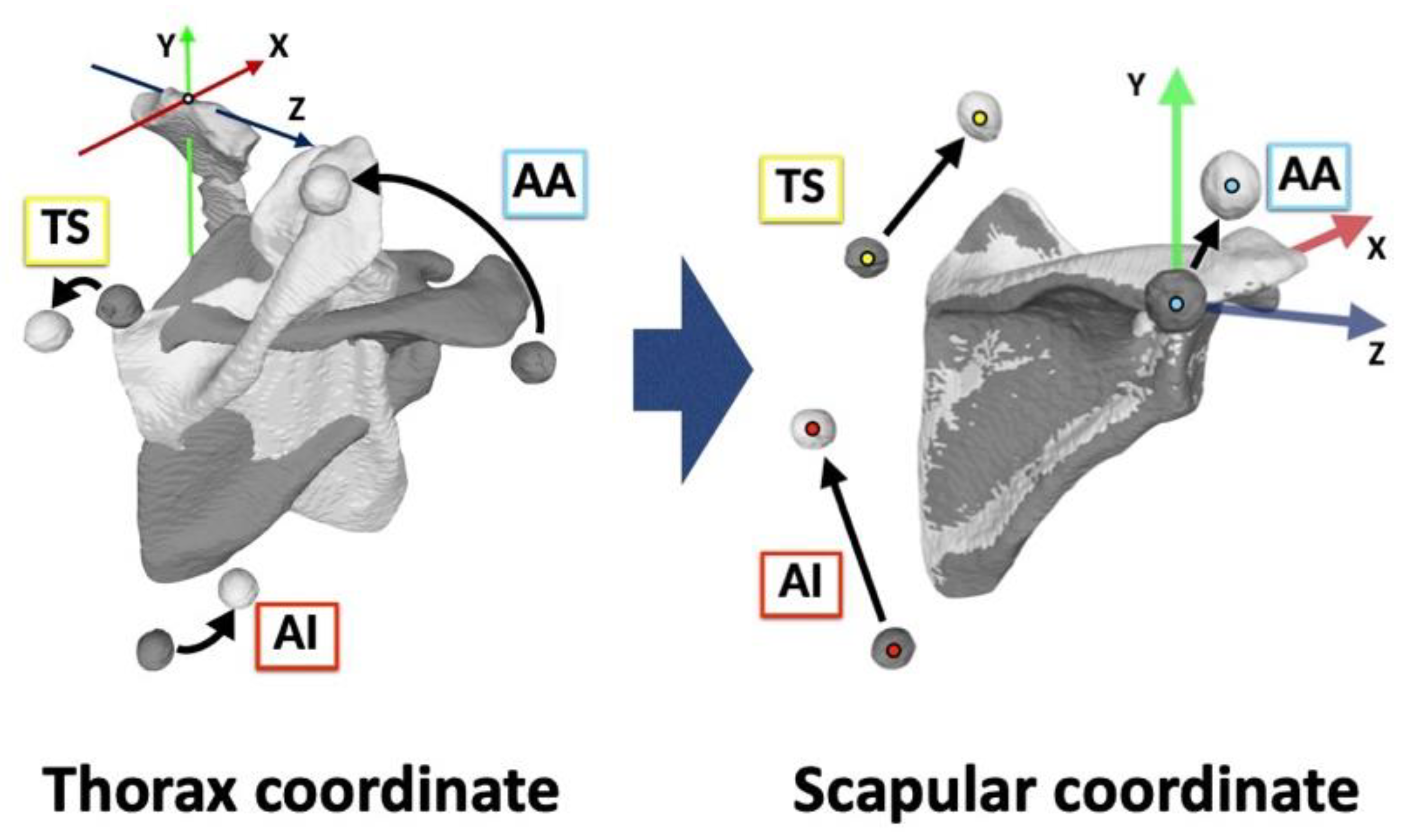
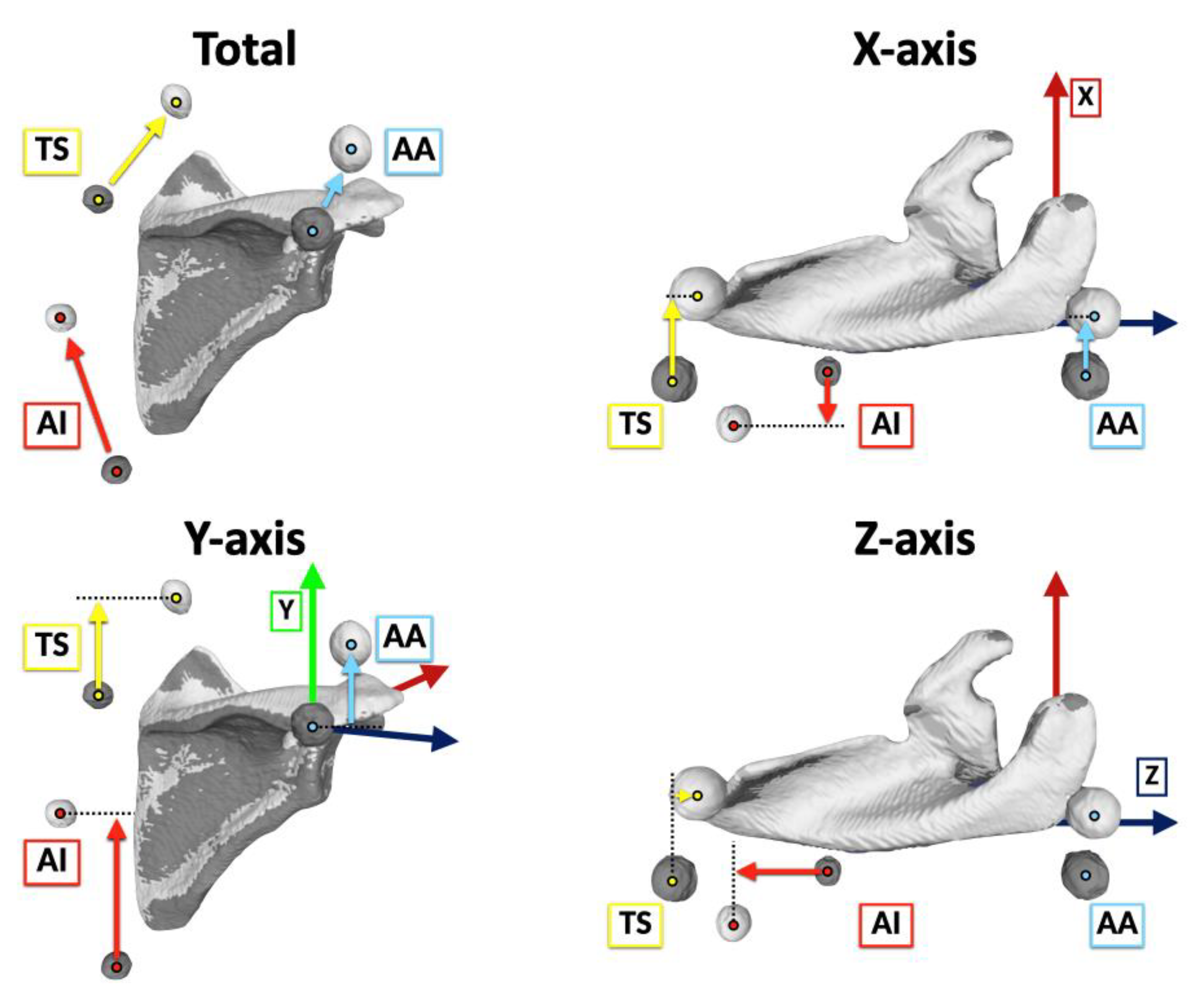
2.3. Coordinate Systems
2.4. Marker Movements
2.5. Rotation Angles
2.6. Statistical Analysis
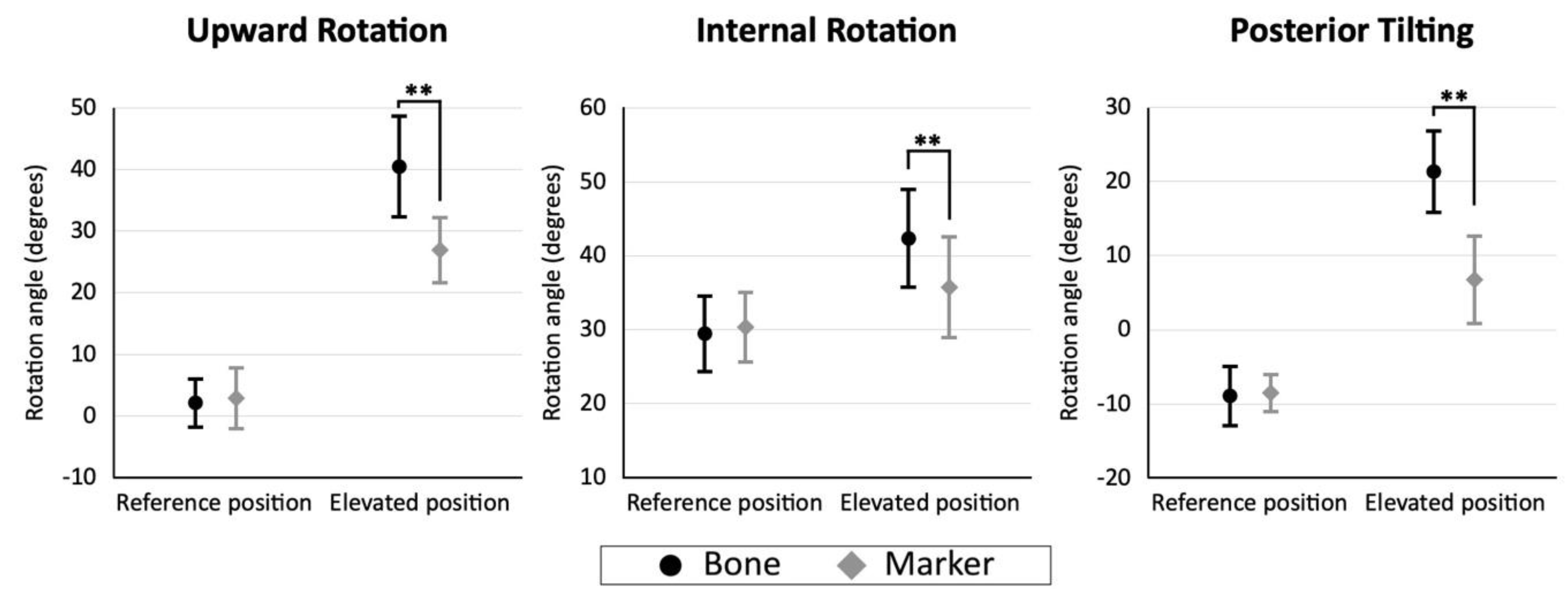
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AA | acromial angle (angulus acromialis); |
| AI | inferior angle (angulus inferior) |
| BMI | body mass index |
| CI | confidence interval |
| CT | computed tomography |
| DICOM | Digital Imaging and Communication in Medicine |
| ICC | intraclass correlation coefficient |
| IQR | interquartile range |
| ISB | International Society of Biomechanics |
| MRI | magnetic resonance imaging |
| STL | Standard Triangulated Language |
| STA | soft-tissue artifact |
| TS | root of the scapular spine (trigonum spinae scapulae) |
| 3D | three-dimensional |
References
- Sahara, W.; Sugamoto, K.; Murai, M.; Tanaka, H.; Yoshikawa, H. The three-dimensional motions of glenohumeral joint under semi-loaded condition during arm abduction using vertically open MRI. Clin. Biomech. 2007, 22, 304–312. [Google Scholar] [CrossRef] [PubMed]
- Matsumura, N.; Oki, S.; Fukasawa, N.; Matsumoto, M.; Nakamura, M.; Nagura, T.; Yamada, Y.; Jinzaki, M. Glenohumeral translation during active external rotation with the shoulder abducted in cases with glenohumeral instability: A 4-dimensional computed tomography analysis. J. Shoulder Elb. Surg. 2019, 28, 1903–1910. [Google Scholar] [CrossRef] [PubMed]
- Matsuki, K.; Matsuki, K.O.; Mu, S.; Yamaguchi, S.; Ochiai, N.; Sasho, T.; Sugaya, H.; Toyone, T.; Wada, Y.; Takahashi, K.; et al. In vivo 3-dimensional analysis of scapular kinematics: Comparison of dominant and nondominant shoulders. J. Shoulder Elb. Surg. 2011, 20, 659–665. [Google Scholar] [CrossRef]
- Ludewig, P.M.; Phadke, V.; Braman, J.P.; Hassett, D.R.; Cieminski, C.J.; LaPrade, R.F. Motion of the shoulder complex during multiplanar humeral elevation. J. Bone Jt. Surg. Am. 2009, 91, 378–389. [Google Scholar] [CrossRef] [PubMed]
- Mackey, A.H.; Walt, S.E.; Lobb, G.A.; Stott, N.S. Reliability of upper and lower limb three-dimensional kinematics in children with hemiplegia. Gait Posture 2005, 22, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Cereatti, A.; Bonci, T.; Akbarshahi, M.; Aminian, K.; Barré, A.; Begon, M.; Benoit, D.L.; Charbonnier, C.; Dal Maso, F.; Fantozzi, S.; et al. Standardization proposal of soft tissue artefact description for data sharing in human motion measurements. J. Biomech. 2017, 62, 5–13. [Google Scholar] [CrossRef]
- Matsui, K.; Shimada, K.; Andrew, P.D. Deviation of skin marker from bone target during movement of the scapula. J. Orthop. Sci. 2006, 11, 180–184. [Google Scholar] [CrossRef]
- Blache, Y.; Dumas, R.; Lundberg, A.; Begon, M. Main component of soft tissue artifact of the upper-limbs with respect to different functional, daily life and sports movements. J. Biomech. 2017, 62, 39–46. [Google Scholar] [CrossRef]
- Charbonnier, C.; Chagué, S.; Kolo, F.C.; Chow, J.C.; Lädermann, A. A patient-specific measurement technique to model shoulder joint kinematics. Orthop. Traumatol. Surg. Res. 2014, 100, 715–719. [Google Scholar] [CrossRef]
- Duprey, S.; Billuart, F.; Sah, S.; Ohl, X.; Robert, T.; Skalli, W.; Wang, X. Three-Dimensional Rotations of the Scapula during Arm Abduction: Evaluation of the Acromion Marker Cluster Method in Comparison with a Model-Based Approach Using Biplanar Radiograph Images. J. Appl. Biomech. 2015, 31, 396–402. [Google Scholar] [CrossRef]
- Karduna, A.R.; McClure, P.W.; Michener, L.A.; Sennett, B. Dynamic measurements of three-dimensional scapular kinematics: A validation study. J. Biomech. Eng. 2001, 123, 184–190. [Google Scholar] [CrossRef] [PubMed]
- Lempereur, M.; Brochard, S.; Leboeuf, F.; Remy-Neris, O. Validity and reliability of 3D marker based scapular motion analysis: A systematic review. J. Biomech. 2014, 47, 2219–2230. [Google Scholar] [CrossRef] [PubMed]
- Hamming, D.; Braman, J.P.; Phadke, V.; LaPrade, R.F.; Ludewig, P.M. The accuracy of measuring glenohumeral motion with a surface humeral cuff. J. Biomech. 2012, 45, 1161–1168. [Google Scholar] [CrossRef] [PubMed]
- Meskers, C.G.; van de Sande, M.A.; de Groot, J.H. Comparison between tripod and skin-fixed recording of scapular motion. J. Biomech. 2007, 40, 941–946. [Google Scholar] [CrossRef]
- Warner, M.B.; Chappell, P.H.; Stokes, M.J. Measurement of dynamic scapular kinematics using an acromion marker cluster to minimize skin movement artifact. J. Vis. Exp. 2015, 96, e51717. [Google Scholar] [CrossRef]
- Begon, M.; Andersen, M.S.; Dumas, R. Multibody Kinematics Optimization for the Estimation of Upper and Lower Limb Human Joint Kinematics: A Systematized Methodological Review. J. Biomech. Eng. 2018, 140, 030801. [Google Scholar] [CrossRef]
- Seth, A.; Matias, R.; Veloso, A.P.; Delp, S.L. A Biomechanical Model of the Scapulothoracic Joint to Accurately Capture Scapular Kinematics during Shoulder Movements. PLoS ONE 2016, 11, e0141028. [Google Scholar] [CrossRef]
- Konda, S.; Sahara, W.; Sugamoto, K. Directional bias of soft-tissue artifacts on the acromion during recording of 3D scapular kinematics. J. Biomech. 2018, 73, 217–222. [Google Scholar] [CrossRef]
- Richardson, R.T. An individualized linear model approach for estimating scapular kinematics during baseball pitching. J. Biomech. 2021, 114, 110160. [Google Scholar] [CrossRef]
- Brochard, S.; Lempereur, M.; Rémy-Néris, O. Double calibration: An accurate, reliable and easy-to-use method for 3D scapular motion analysis. J. Biomech. 2011, 44, 751–754. [Google Scholar] [CrossRef]
- Lovern, B.; Stroud, L.A.; Evans, R.O.; Evans, S.L.; Holt, C.A. Dynamic tracking of the scapula using skin-mounted markers. Proc. Inst. Mech. Eng. H 2009, 223, 823–831. [Google Scholar] [CrossRef]
- Jinzaki, M.; Yamada, Y.; Nagura, T.; Nakahara, T.; Yokoyama, Y.; Narita, K.; Ogihara, N.; Yamada, M. Development of Upright Computed Tomography With Area Detector for Whole-Body Scans: Phantom Study, Efficacy on Workflow, Effect of Gravity on Human Body, and Potential Clinical Impact. Investig. Radiol. 2020, 55, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Yamada, Y.; Yamada, M.; Chubachi, S.; Yokoyama, Y.; Matsuoka, S.; Tanabe, A.; Niijima, Y.; Murata, M.; Fukunaga, K.; Jinzaki, M. Comparison of inspiratory and expiratory lung and lobe volumes among supine, standing, and sitting positions using conventional and upright CT. Sci. Rep. 2020, 10, 16203. [Google Scholar] [CrossRef]
- Yamada, Y.; Yamada, M.; Yokoyama, Y.; Tanabe, A.; Matsuoka, S.; Niijima, Y.; Narita, K.; Nakahara, T.; Murata, M.; Fukunaga, K.; et al. Differences in Lung and Lobe Volumes between Supine and Standing Positions Scanned with Conventional and Newly Developed 320-Detector-Row Upright CT: Intra-Individual Comparison. Respiration 2020, 99, 598–605. [Google Scholar] [CrossRef]
- Wu, G.; van der Helm, F.C.T.; Veeger, H.E.J.; Makhsous, M.; Van Roy, P.; Anglin, C.; Nagels, J.; Karduna, A.R.; McQuade, K.; Wang, X.; et al. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion—Part II: Shoulder, elbow, wrist and hand. J. Biomech. 2005, 38, 981–992. [Google Scholar] [CrossRef]
- Yamada, Y.; Jinzaki, M.; Hosokawa, T.; Tanami, Y.; Sugiura, H.; Abe, T.; Kuribayashi, S. Dose reduction in chest CT: Comparison of the adaptive iterative dose reduction 3D, adaptive iterative dose reduction, and filtered back projection reconstruction techniques. Eur. J. Radiol. 2012, 81, 4185–4195. [Google Scholar] [CrossRef]
- Yoshida, Y.; Matsumura, N.; Yamada, Y.; Yamada, M.; Yokoyama, Y.; Matsumoto, M.; Nakamura, M.; Nagura, T.; Jinzaki, M. Evaluation of three-dimensional acromiohumeral distance in the standing position and comparison with its conventional measuring methods. J. Orthop. Surg. Res. 2020, 15, 436. [Google Scholar] [CrossRef]
- Drew, A.J.; Tashjian, R.Z.; Henninger, H.B.; Bachus, K.N. Sex and Laterality Differences in Medullary Humerus Morphology. Anat. Rec. 2019, 302, 1709–1717. [Google Scholar] [CrossRef]
- Yoshida, Y.; Matsumura, N.; Miyamoto, A.; Oki, S.; Yokoyama, Y.; Yamada, M.; Yamada, Y.; Nakamura, M.; Nagura, T.; Jinzaki, M. Three-dimensional shoulder kinematics: Upright four-dimensional computed tomography in comparison with an optical three-dimensional motion capture system. J. Orthop. Res. 2022. [Google Scholar] [CrossRef]
- Matsumura, N.; Yamada, Y.; Oki, S.; Yoshida, Y.; Yokoyama, Y.; Yamada, M.; Nagura, T.; Jinzaki, M. Three-dimensional alignment changes of the shoulder girdle between the supine and standing positions. J. Orthop. Surg. Res. 2020, 15, 411. [Google Scholar] [CrossRef]
- Shaheen, A.F.; Alexander, C.M.; Bull, A.M. Effects of attachment position and shoulder orientation during calibration on the accuracy of the acromial tracker. J. Biomech. 2011, 44, 1410–1413. [Google Scholar] [CrossRef]
- Prinold, J.A.; Shaheen, A.F.; Bull, A.M. Skin-fixed scapula trackers: A comparison of two dynamic methods across a range of calibration positions. J. Biomech. 2011, 44, 2004–2007. [Google Scholar] [CrossRef]
- An, Z.; Wang, X.; Li, B.; Xiang, Z.; Zhang, B. Robust visual tracking for UAVs with dynamic feature weight selection. Appl. Intell. 2022. [Google Scholar] [CrossRef]
- Chen, H.; Miao, F.; Chen, Y.; Xiong, Y.; Chen, T. A Hyperspectral Image Classification Method Using Multifeature Vectors and Optimized KELM. IEEE J. Sel. Top. Appl. Earth Obs. Remote Sens. 2021, 14, 2781–2795. [Google Scholar] [CrossRef]
- Wu, D.; Wu, C. Research on the Time-Dependent Split Delivery Green Vehicle Routing Problem for Fresh Agricultural Products with Multiple Time Windows. Agriculture 2022, 12, 793. [Google Scholar] [CrossRef]
- Zhou, X.; Ma, H.; Gu, J.; Chen, H.; Deng, W. Parameter adaptation-based ant colony optimization with dynamic hybrid mechanism. Eng. Appl. Artif. Intell. 2022, 114, 105139. [Google Scholar] [CrossRef]
- Bahl, J.S.; Zhang, J.; Killen, B.A.; Taylor, M.; Solomon, L.B.; Arnold, J.B.; Lloyd, D.G.; Besier, T.F.; Thewlis, D. Statistical shape modelling versus linear scaling: Effects on predictions of hip joint centre location and muscle moment arms in people with hip osteoarthritis. J. Biomech. 2019, 85, 164–172. [Google Scholar] [CrossRef]
- Camomilla, V.; Bonci, T. A joint kinematics driven model of the pelvic soft tissue artefact. J. Biomech. 2020, 111, 109998. [Google Scholar] [CrossRef]
- Hasegawa, K.; Okamoto, M.; Hatsushikano, S.; Shimoda, H.; Ono, M.; Homma, T.; Watanabe, K. Standing sagittal alignment of the whole axial skeleton with reference to the gravity line in humans. J. Anat 2017, 230, 619–630. [Google Scholar] [CrossRef]
- Zou, Y.; Song, E.; Jin, R. Age-dependent changes in skin surface assessed by a novel two-dimensional image analysis. Ski Res. Technol. 2009, 15, 399–406. [Google Scholar] [CrossRef]



| Spearman’s Rank Correlation Coefficient | Upward Rotation | Internal Rotation | Posterior Tilting | |
|---|---|---|---|---|
| Acromial angle (angulus acromialis [AA]) | ρ (p-value) | 0.281 (0.231) | 0.017 (0.945) | 0.535 (0.015 *) |
| Root of the scapular spine (trigonum spinae scapulae [TS]) | ρ (p-value) | 0.350 (0.131) | 0.449 (0.047 *) | 0.184 (0.439) |
| Inferior angle (angulus inferior [AI]) | ρ (p-value) | 0.453 (0.045 *) | 0.280 (0.232) | 0.117 (0.622) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoshida, Y.; Matsumura, N.; Yamada, Y.; Yamada, M.; Yokoyama, Y.; Miyamoto, A.; Nakamura, M.; Nagura, T.; Jinzaki, M. Three-Dimensional Quantitative Evaluation of the Scapular Skin Marker Movements in the Upright Posture. Sensors 2022, 22, 6502. https://doi.org/10.3390/s22176502
Yoshida Y, Matsumura N, Yamada Y, Yamada M, Yokoyama Y, Miyamoto A, Nakamura M, Nagura T, Jinzaki M. Three-Dimensional Quantitative Evaluation of the Scapular Skin Marker Movements in the Upright Posture. Sensors. 2022; 22(17):6502. https://doi.org/10.3390/s22176502
Chicago/Turabian StyleYoshida, Yuki, Noboru Matsumura, Yoshitake Yamada, Minoru Yamada, Yoichi Yokoyama, Azusa Miyamoto, Masaya Nakamura, Takeo Nagura, and Masahiro Jinzaki. 2022. "Three-Dimensional Quantitative Evaluation of the Scapular Skin Marker Movements in the Upright Posture" Sensors 22, no. 17: 6502. https://doi.org/10.3390/s22176502






