Design of a Novel Compact MICS Band PIFA Antenna for Implantable Biotelemetry Applications
Abstract
:1. Introduction
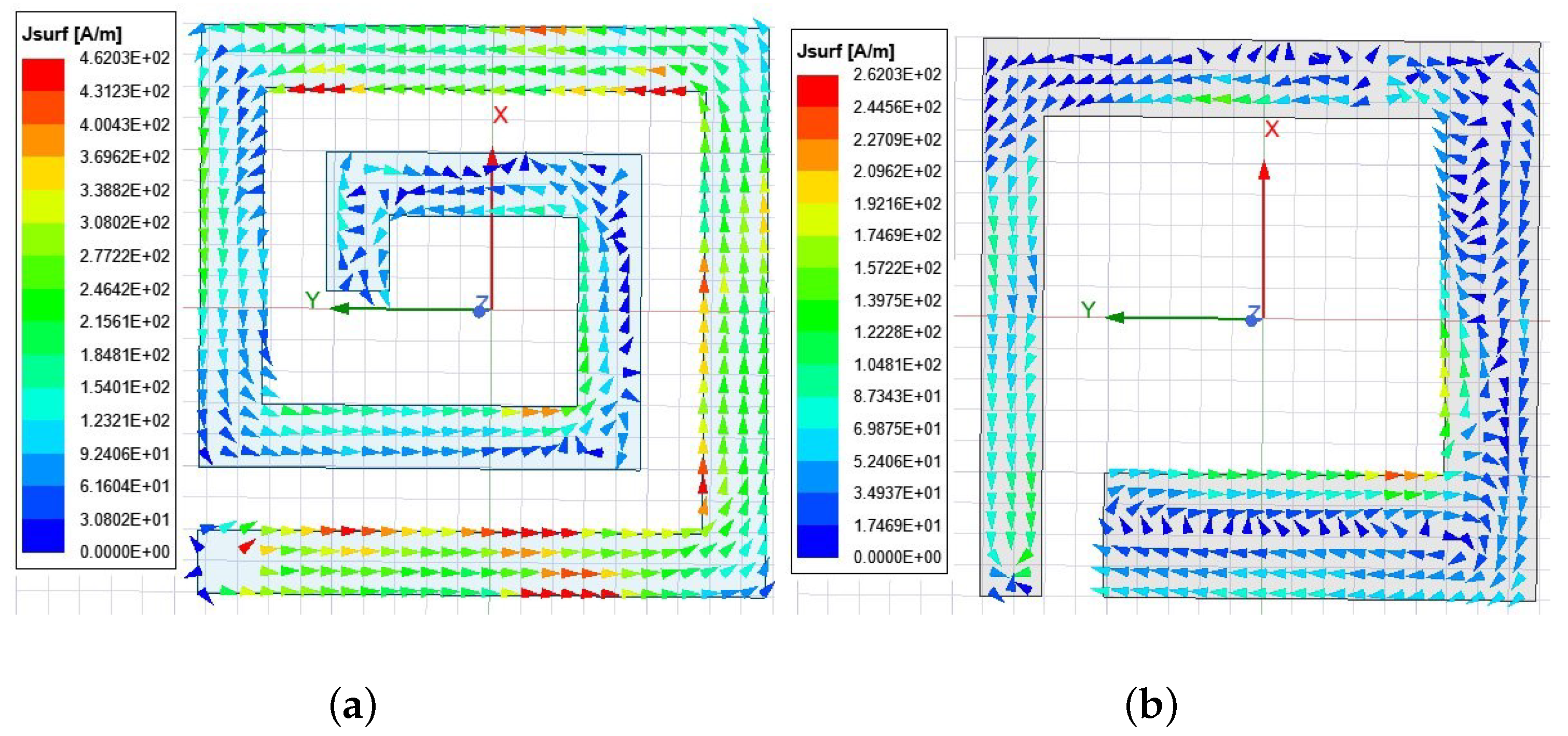
2. Antenna Design
3. Parametric Study and Simulation Results
3.1. Position of Shorting Pin
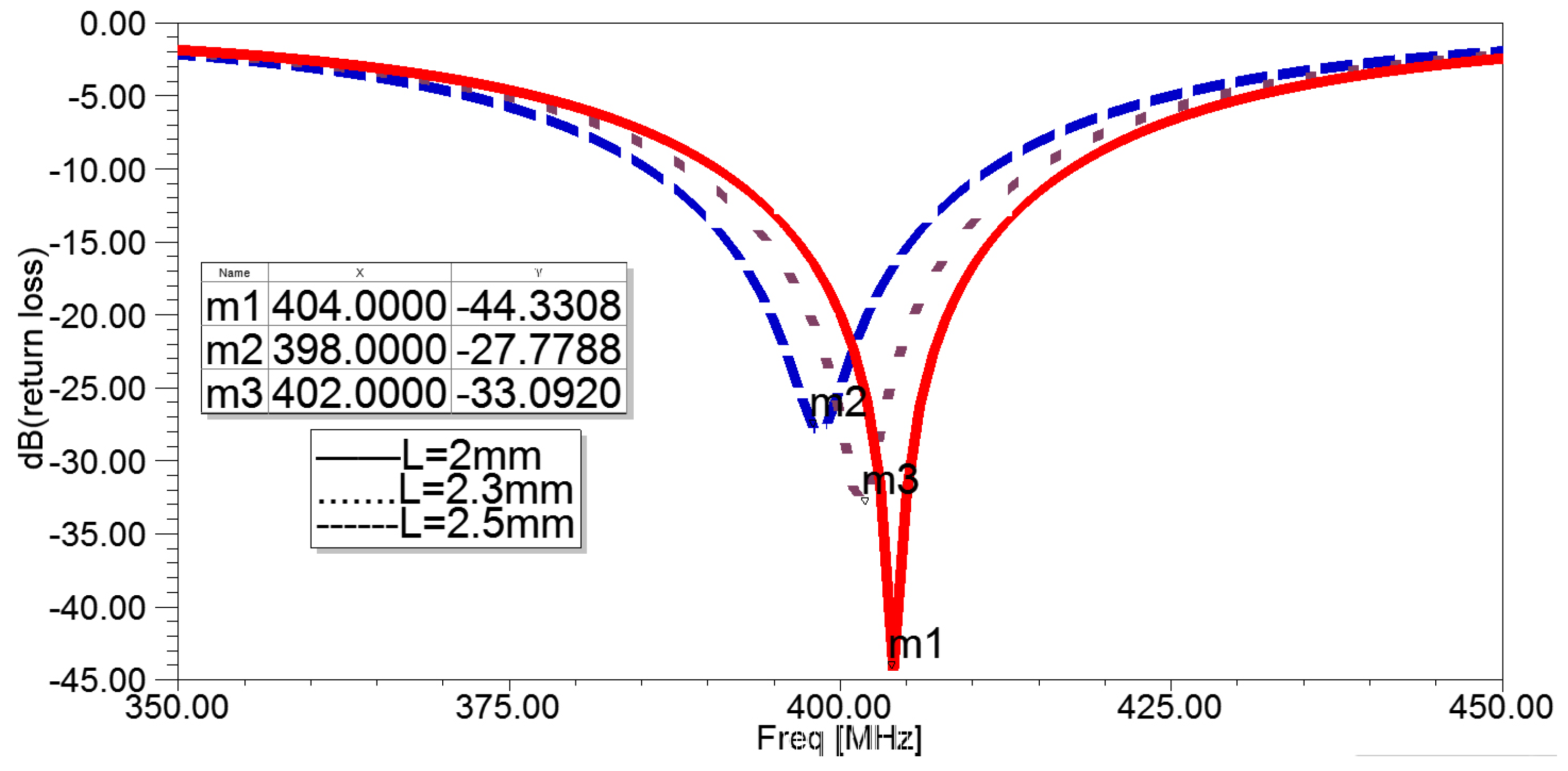
3.2. Length of Top Spiral Line
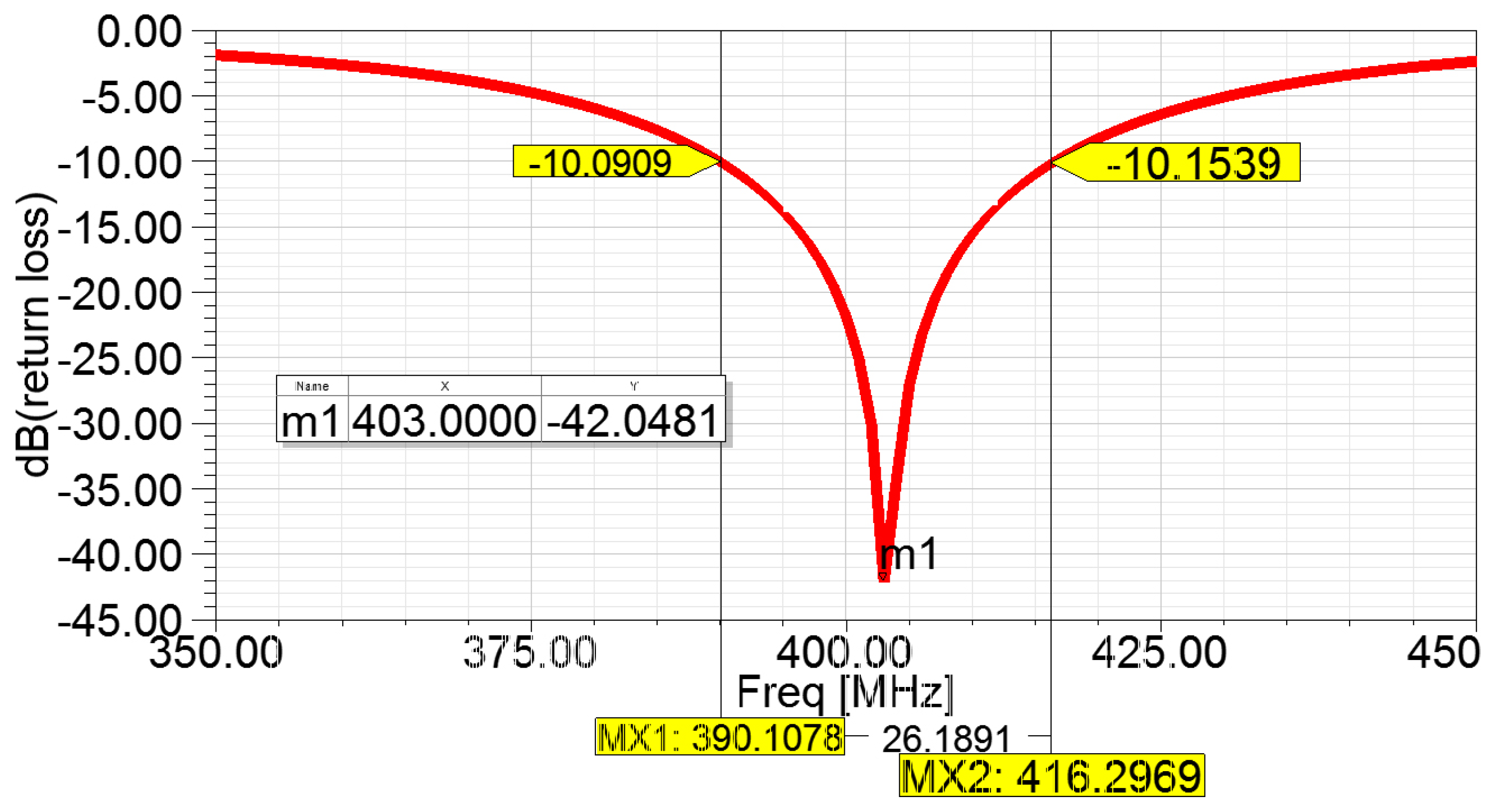
3.3. Optimal Simulation Results
4. Measurement Results and Discussion
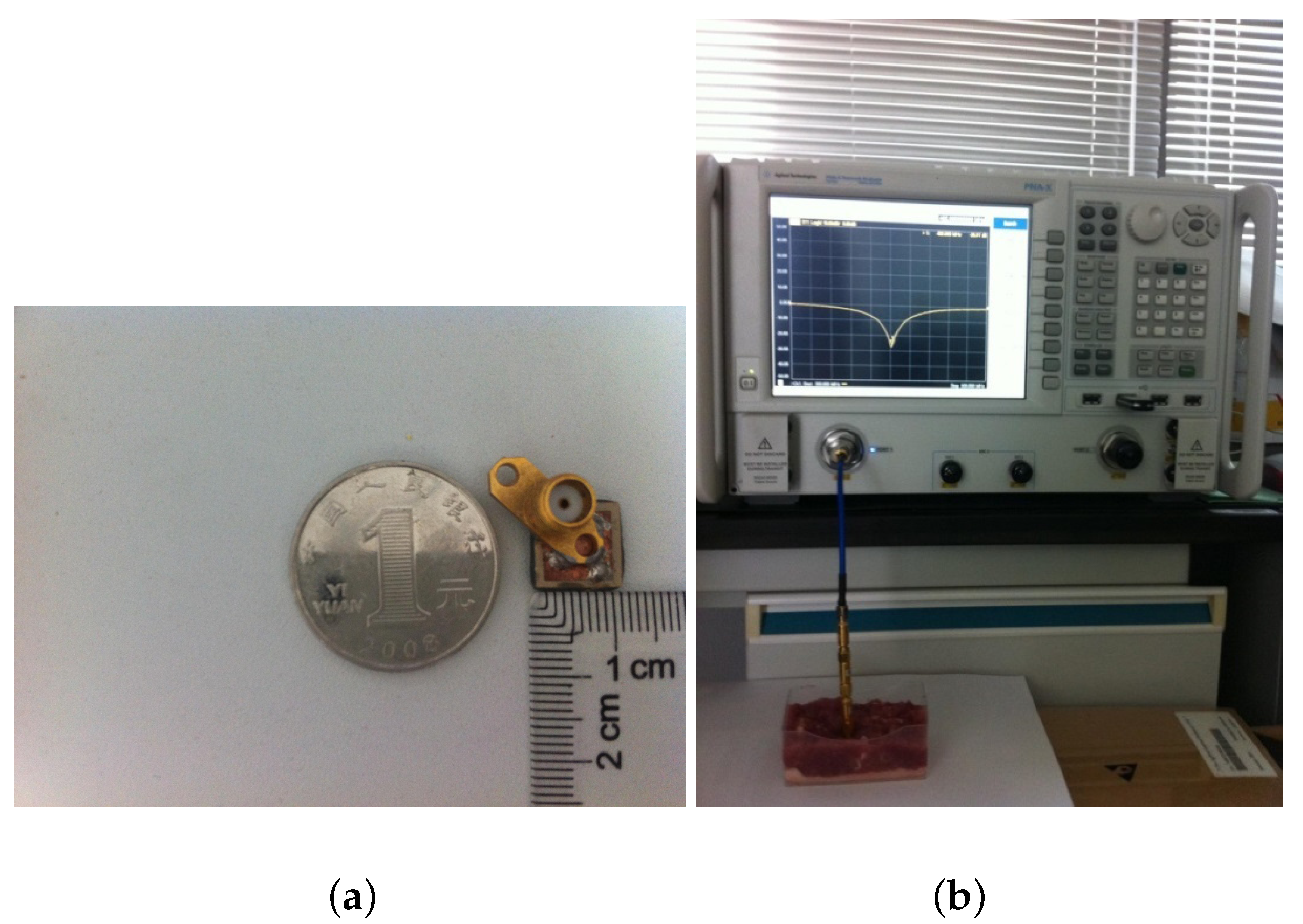
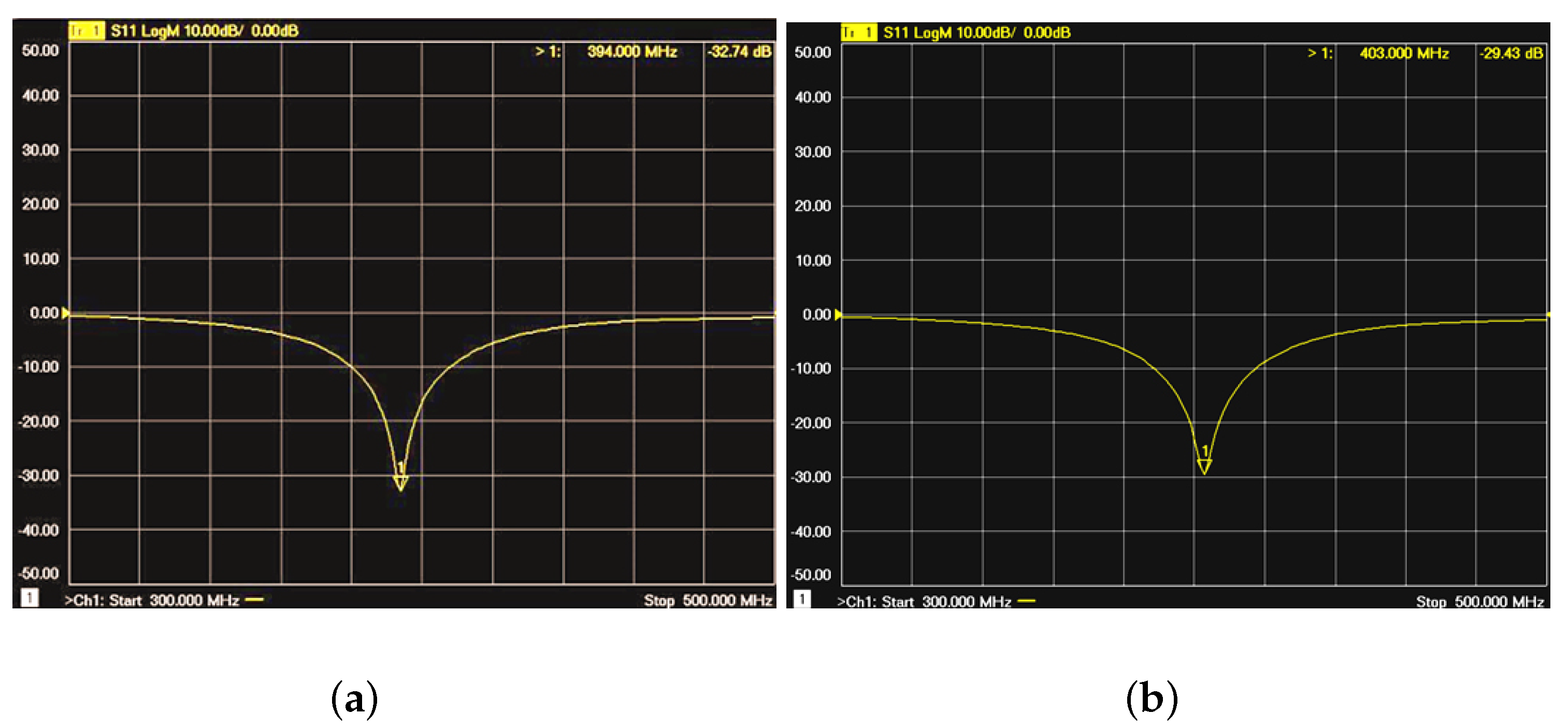
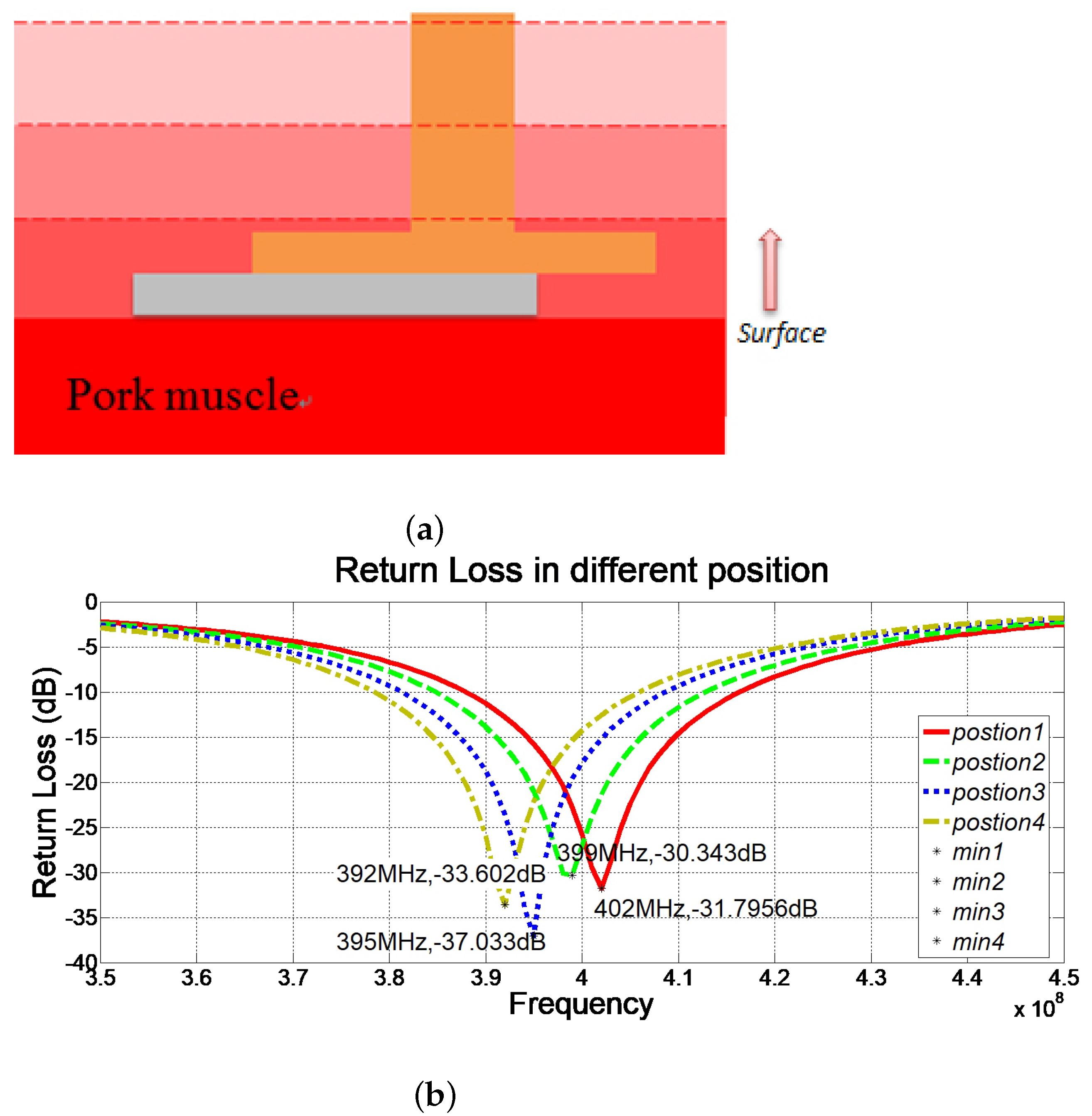
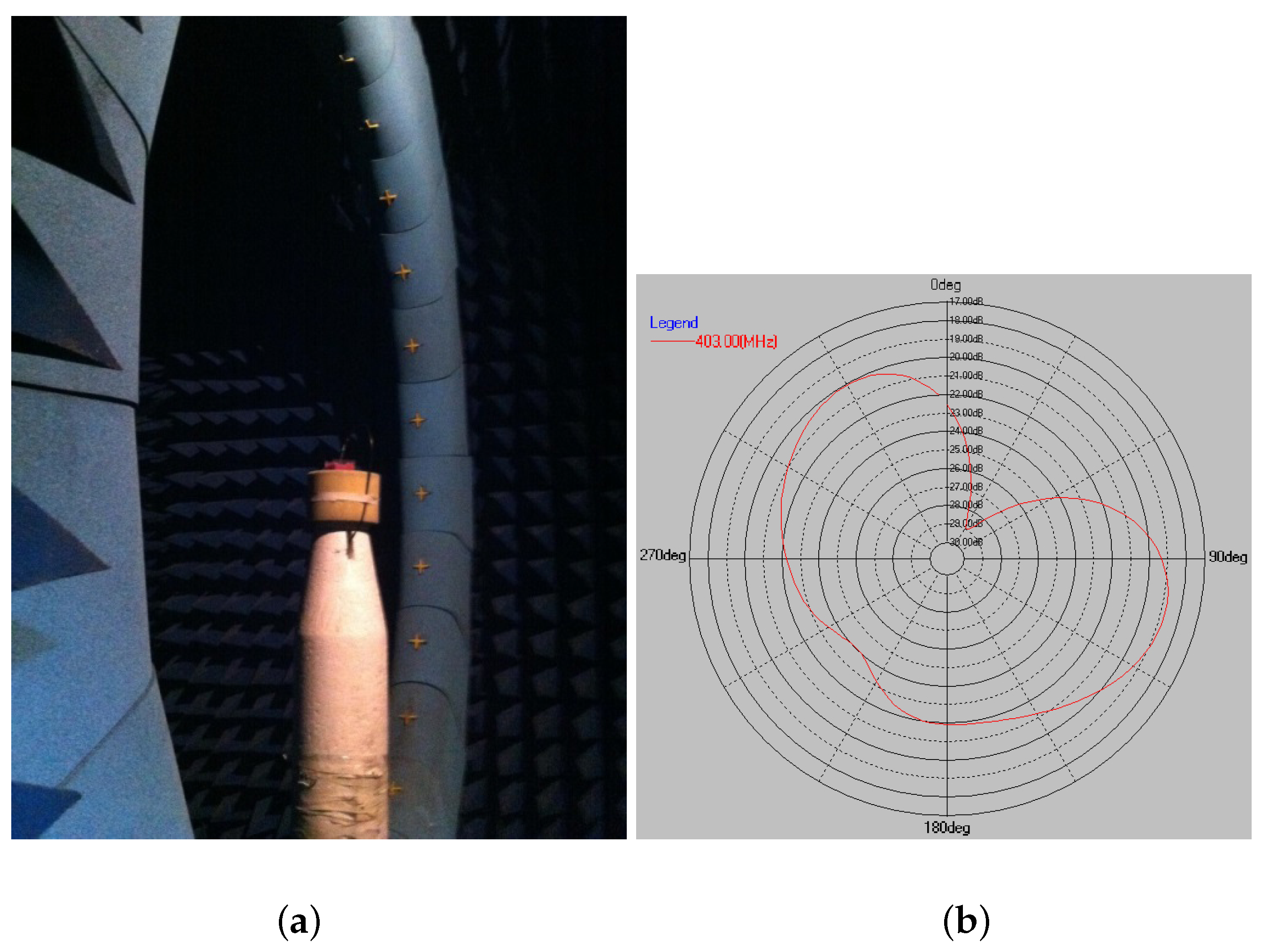
4.1. In Vitro Experiment
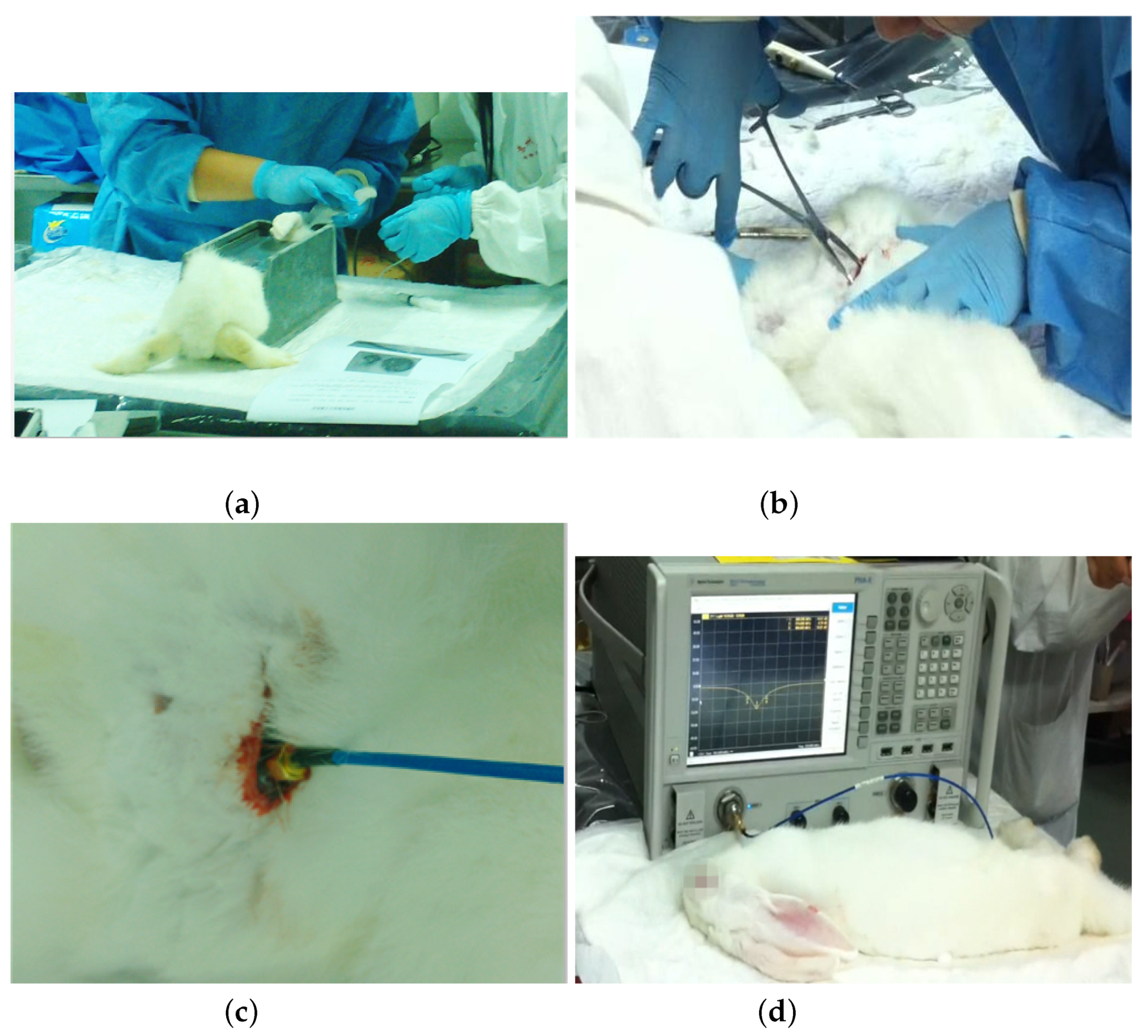
4.2. In Vivo Experiment
4.3. Comparative Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PIFA | Planar inverted-F antenna |
| MICS | Medical implant communications service |
| IMDs | Implantable medical devices |
| RF | Radio frequency |
| SAR | Specific absorption rate |
| HFSS | High-frequency structure simulator |
| AUT | Antenna under test |
References
- Tang, Z.; Smith, B.; Schild, J.H.; Peckham, P.H. Data transmission from an implantable biotelemeter by load-shift keying using circuit configuration modulator. IEEE Trans. Biomed. Eng. 1995, 42, 524–528. [Google Scholar] [CrossRef] [Green Version]
- Valdastri, P.; Menciassi, A.; Arena, A.; Caccamo, C.; Dario, P. An implantable telemetry platform system for in vivo monitoring of physiological parameters. IEEE Trans. Inf. Technol. Biomed. 2004, 8, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Manjulatha, V.; Korada, K. Implantable antennas for biomedical applications. IEEE J. Electromagn. Microwaves Med. Biol. 2016, 11, 5632–5636. [Google Scholar]
- Savci, H.S.; Sula, A.; Wang, Z.; Dogan, N.S.; Arvas, E. MICS transceivers: Regulatory standards and applications [medical implant communications service]. In Proceedings of the IEEE SoutheastCon, Ft. Lauderdale, FL, USA, 8–10 April 2005; pp. 179–182. [Google Scholar] [CrossRef]
- Soliman, M.M.; Chowdhury, M.E.H.; Khandakar, A.; Islam, M.T.; Qiblawey, Y.; Musharavati, F.; Zal Nezhad, E. Review on Medical Implantable Antenna Technology and Imminent Research Challenges. Sensors 2021, 21, 3163. [Google Scholar] [CrossRef] [PubMed]
- Harish, A.; Hidayat, M.R.; Nur, L.O.; Nugroho, B.S.; Munir, A. Spiral-shaped printed planar inverted-F antenna for body wearable application. In Proceedings of the 2017 11th International Conference on Telecommunication Systems Services and Applications (TSSA), Lombok, Indonesia, 26–27 October 2017; pp. 1–4. [Google Scholar] [CrossRef]
- Hosain, M.K.; Kouzani, A.Z.; Tye, S.J.; Samad, M.F.; Kale, R.P.; Bennet, K.E.; Manciu, F.S.; Berk, M. Radio frequency energy harvesting from a feeding source in a passive deep brain stimulation device for murine preclinical research. Med. Eng. Phys. 2015, 37, 1020–1026. [Google Scholar] [CrossRef]
- Bakogianni, S.; Koulouridis, S. A Dual-Band Implantable Rectenna for Wireless Data and Power Support at Sub-GHz Region. IEEE Trans. Antennas. Propag. 2019, 67, 6800–6810. [Google Scholar] [CrossRef]
- Li, R.; Li, B.; Du, G.; Sun, X.; Sun, H. A compact broadband antenna with dual-resonance for implantable devices. Micromachines 2019, 10, 59. [Google Scholar] [CrossRef] [Green Version]
- Kawdungta, S.; Boonpoonga, A.; Phongcharoenpanich, C. Mics/ism meander-line microstrip antenna encapsulated in oblong-shaped pod for gastrointestinal tract diagnosis. Sensors 2021, 21, 3897. [Google Scholar] [CrossRef]
- Yang, Z.J.; Zhu, L.; Xiao, S. An Implantable Circularly Polarized Patch Antenna Design for Pacemaker Monitoring Based on Quality Factor Analysis. IEEE Trans. Antennas Propag. 2018, 66, 5180–5192. [Google Scholar] [CrossRef]
- Soontornpipit, P.; Furse, C.M.; Chung, Y.C. Design of implantable microstrip antenna for communication with medical implants. IEEE Trans. Microw. Theory Tech. 2004, 52, 1944–1951. [Google Scholar] [CrossRef]
- Permana, H. Hermetic Implantable Antenna Inside Vitreous Humor Simulating Fluid. Prog. Electromagn. Res. 2013, 133, 571–590. [Google Scholar] [CrossRef] [Green Version]
- Soontornpipit, P.; Furse, C.M.; Chung, Y.C. Miniaturized biocompatible microstrip antenna using genetic algorithm. IEEE Trans. Antennas Propag. 2005, 53, 1939–1945. [Google Scholar] [CrossRef]
- Liu, W.C.; Chen, S.H.; Wu, C.M. Implantable Broadband Circular Stacked Pifa Antenna for Biotelemetry Communication. J. Electromagn. Waves Appl. 2008, 22, 1791–1800. [Google Scholar] [CrossRef]
- Karacolak, T.; Hood, A.Z.; Topsakal, E. Design of a Dual-Band Implantable Antenna and Development of Skin Mimicking Gels for Continuous Glucose Monitoring. IEEE Trans. Microw. Theory Tech. 2008, 56, 1001–1008. [Google Scholar] [CrossRef]
- Permana, H.; Fang, Q.; Lee, S.Y. Comparison study on specific absorption rate of three implantable antennas designed for retinal prosthesi systems. Microw. Antennas Propag. IET 2013, 7, 886–893. [Google Scholar] [CrossRef]
- Permana, H.; Fang, Q.; Lee, S.Y. A microstrip antenna designed for implantable body sensor network. In Proceedings of the 2013 1st International Conference on Orange Technologies, Tainan, Taiwan, 12–16 March 2013; pp. 103–106. [Google Scholar] [CrossRef]
- Andreuccetti, D.; Fossi, R.; Petrucci, C. An Internet Resource for the Calculation of the Dielectric Properties of Body Tissues in the Frequency Range 10 Hz–100 GHz. Available online: http://niremf.ifac.cnr.it/tissprop/ (accessed on 1 June 2022).
- IEEE Std C95.1-1991; IEEE Standard for Safety Levels with Respect to Human Exposure to Radio Frequency Electromagnetic Fields, 3 kHz to 300 GHz. IEEE: Piscataway, NJ, USA, 1992; pp. 1–76. [CrossRef]
- SMT Connector Datasheet. Available online: http://www.radiall.com (accessed on 1 July 2022).
- Nikolayev, D.; Joseph, W.; Skrivervik, A.; Zhadobov, M.; Martens, L.; Sauleau, R. Dielectric-Loaded Conformal Microstrip Antennas for Versatile In-Body Applications. IEEE Antennas Wirel. Propag. Lett. 2019, 18, 2686–2690. [Google Scholar] [CrossRef] [Green Version]
- Ramli, N.H.; Kamarudin, M.R.; Samsuri, N.A.; Ahyat, E.N. Investigation on a compact ring printed monopole antenna for wireless implantable body area network (WiBAN) applications. Microw. Opt. Technol. Lett. 2013, 55, 1053–1058. [Google Scholar] [CrossRef]
- Hout, S.; Chung, J.Y. Design and Characterization of a Miniaturized Implantable Antenna in a Seven-Layer Brain Phantom. IEEE Access 2019, 7, 162062–162069. [Google Scholar] [CrossRef]
- Lee, J.H.; Seo, D.W.; Lee, H.S. Design of Implantable Rectangular Spiral Antenna for Wireless Biotelemetry in MICS Band. ETRI J. 2015, 37, 204–211. [Google Scholar] [CrossRef] [Green Version]
- Liu, W.C.; Yeh, F.M.; Ghavami, M. Miniaturized implantable broadband antenna for biotelemetry communication. Microw. Opt. Technol. Lett. 2008, 50, 2407–2409. [Google Scholar] [CrossRef]
- Kim, U.; Choi, J. An Implantable Antenna for Wireless Body Area Network Application. J. Electromagn. Eng. Sci. 2010, 10, 206–210. [Google Scholar] [CrossRef]
- Palandoken, M. Compact bioimplantable MICS and ISM band antenna design for wireless biotelemetry applications. Radioengineering 2017, 26, 917–918. [Google Scholar] [CrossRef]
- Sulaiman, N.H.; Samsuri, N.A.; Rahim, M.K.A.; Seman, F.C.; Inam Abbasi, M. Compact meander line telemetry antenna for implantable pacemaker applications. Indones. J. Electr. Eng. Comput. Sci. 2018, 10, 883–889. [Google Scholar] [CrossRef]
- Fu, Y.; Lei, J.; Zou, X.; Guo, J. Flexible antenna design on PDMS substrate for implantable bioelectronics applications. Electrophoresis 2019, 40, 1186–1194. [Google Scholar] [CrossRef] [PubMed]
- Usluer, M.; Cetindere, B.; Basaran, S.C. Compact implantable antenna design for MICS and ISM band biotelemetry applications. Microw. Opt. Technol. Lett. 2020, 62, 1581–1587. [Google Scholar] [CrossRef]






| Tissue | Thickness (mm) | Relative Permittivity | Conductivity (S/m) | Mass Density (kg/m3) |
|---|---|---|---|---|
| Skin | 3 | 46.72 | 0.68 | 1100 |
| Fat | 10 | 5.58 | 0.04 | 916 |
| Muscle | 20 | 57.10 | 0.79 | 1041 |
| Reference Type | Frequency Band | Dimension (mm) | Gain (dB) |
|---|---|---|---|
| Palandoken 2017 [28] | MICS/ISM | 432 (15 × 15 × 1.92) | MICS: −14.4 ISM: −14.55 |
| Sulaiman 2018 [29] | MICS | 4103.1 (30.5 × 21.02 × 6.4) | - |
| Bakogianni 2019 [8] | MedRadio/ISM | 284.48 (16 × 14 × 1.27) | MedRadio: −35.9 ISM: −24.3 |
| Fu 2019 [30] | ISM | 242 (11 × 11 × 2) | −22.95 |
| Usluer 2020 [31] | MICS/ISM | 248.92 (14 × 14 × 1.27) | MICS: −48.15 ISM: −21.15 |
| Li 2019 [9] | MedRadio | 479 (23 × 16.4 × 1.27) | −37.05 |
| Kawdungta 2021 [10] | MICS/ISM | 213.36 (6 × 28 × 1.27) | MICS: −40.15 ISM: −15.15 |
| Proposed Antenna | MICS | 190.5 (10 × 10 × 1.905) | −18.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, Z.; Wu, H.; Mahmoud, S.S.; Fang, Q. Design of a Novel Compact MICS Band PIFA Antenna for Implantable Biotelemetry Applications. Sensors 2022, 22, 8182. https://doi.org/10.3390/s22218182
Huang Z, Wu H, Mahmoud SS, Fang Q. Design of a Novel Compact MICS Band PIFA Antenna for Implantable Biotelemetry Applications. Sensors. 2022; 22(21):8182. https://doi.org/10.3390/s22218182
Chicago/Turabian StyleHuang, Ziyang, Hao Wu, Seedahmed S. Mahmoud, and Qiang Fang. 2022. "Design of a Novel Compact MICS Band PIFA Antenna for Implantable Biotelemetry Applications" Sensors 22, no. 21: 8182. https://doi.org/10.3390/s22218182




