Analysis of Relationship between Natural Standing Behavior of Elderly People and a Class of Standing Aids in a Living Space
Abstract
:1. Introduction
2. Materials and Methods
2.1. Standing Behavior Recorded in the Elderly Behavior Library
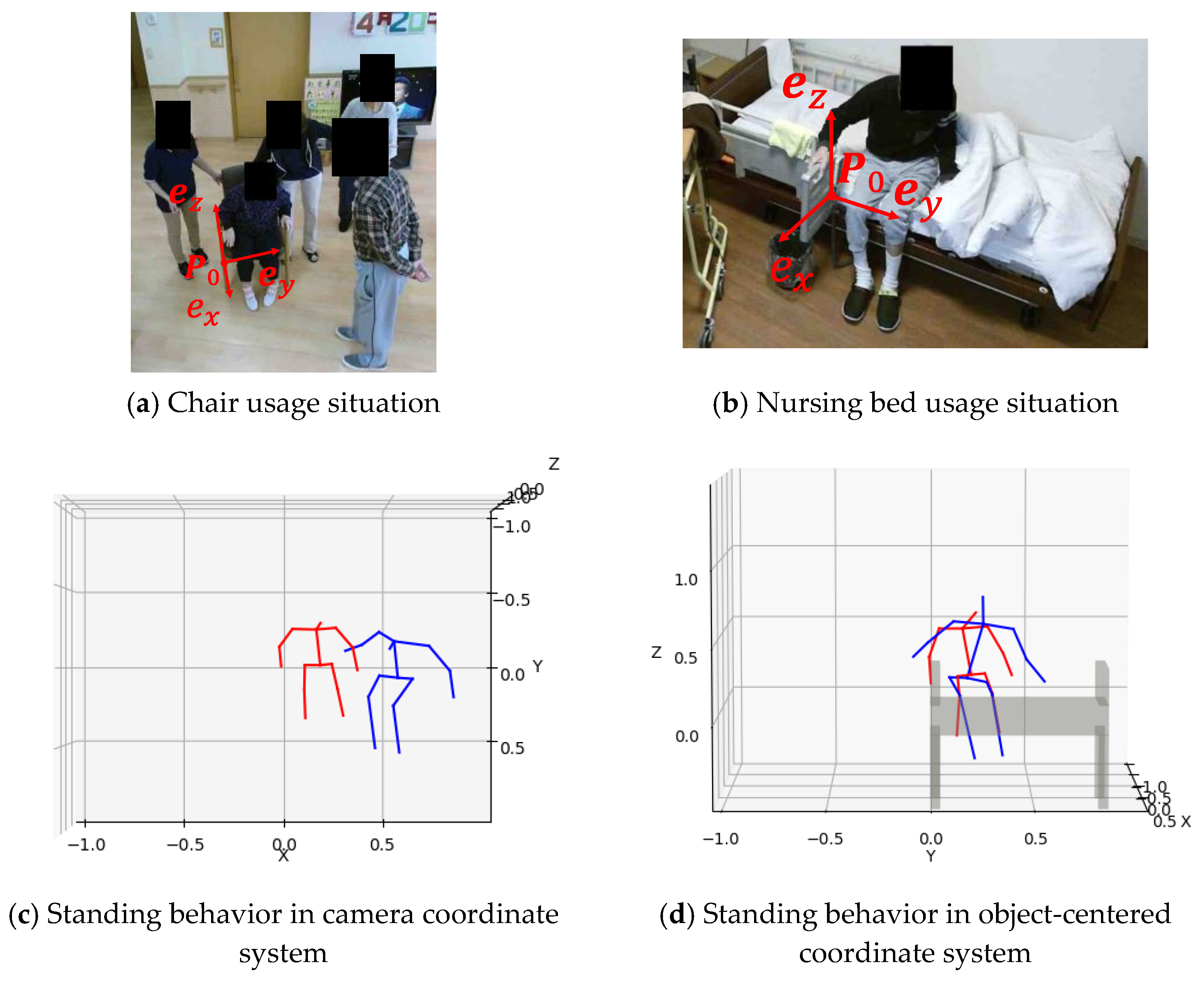
2.2. Method for Analyzing Product Use Behavior Stored in the Elderly Behavior Library
3. Results
3.1. Cluster Analysis and the Representative Behaviors of Elderly Standing Behavior
3.2. Relationship between Standing Behavior and Product Use
3.3. Relationship between Standing Behavior and Physical Ability and Cognitive Ability
4. Discussion
4.1. Cluster Analysis and the Representative Standing Behaviors
4.2. Relationship between Product Use and Representative Standing Behaviors of Each Cluster
4.3. Relationship between Standing Behavior and Physical or Cognitive Ability Scores
4.4. Limitations and Future Scope
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Appendix B

References
- WHO. Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 31 October 2021).
- Borel, L.; Alescio-Lautier, B. Posture and cognition in the elderly: Interaction and contribution to the rehabilitation strategies. Neurophysiol. Clin. Clin. Neurophysiol. 2014, 44, 95–107. [Google Scholar] [CrossRef] [PubMed]
- Lord, S.R.; Rogers, M.W.; Howland, A.; Fitzpatrick, R. Lateral stability, sensorimotor function and falls in older people. J. Am. Geriatr. Soc. 1999, 47, 1077–1081. [Google Scholar] [CrossRef] [PubMed]
- Vuong, N.; Chan, S.; Lau, C. Automated detection of wandering patterns in people with dementia. Gerontechnology 2014, 12, 127–147. [Google Scholar] [CrossRef]
- Su, C.; Fu, L.; Chien, Y.; Li, T. Activity Recognition System for Dementia in Smart Homes based on Wearable Sensor Data. In Proceedings of the 2018 IEEE Symposium Series on Computational Intelligence (SSCI), Bangalore, India, 18–21 November 2018; pp. 463–469. [Google Scholar]
- Enshaeifar, S.; Zoha, A.; Markides, A.; Skillman, S.; Acton, S.T.; Elsaleh, T.; Hassanpour, M.; Ahrabian, A.; Kenny, M.; Klein, S.; et al. Health management and pattern analysis of daily living activities of people with dementia using in-home sensors and machine learning techniques. PLoS ONE 2018, 13, e0195605. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Enshaeifar, S.; Zoha, A.; Skillman, S.; Markides, A.; Acton, S.T.; Elsaleh, T.; Kenny, M.; Rostill, H.; Nilforooshan, R.; Barnaghi, P. Machine learning methods for detecting urinary tract infection and analysing daily living activities in people with dementia. PLoS ONE 2019, 14, e0209909. [Google Scholar] [CrossRef] [Green Version]
- Ahamed, F.; Shahrestani, S.; Cheung, H. Internet of Things and Machine Learning for Healthy Ageing: Identifying the Early Signs of Dementia. Sensors 2020, 20, 6031. [Google Scholar] [CrossRef] [PubMed]
- Wilmink, G.; Dupey, K.; Alkire, S.; Grote, J.; Zobel, G.; Fillit, H.M.; Movva, S. Artificial Intelligence–Powered Digital Health Platform and Wearable Devices Improve Outcomes for Older Adults in Assisted Living Communities: Pilot Intervention Study. JMIR Aging 2020, 3, e19554. [Google Scholar] [CrossRef]
- Kayama, H.; Okamoto, K.; Nishiguchi, S.; Yamada, M.; Kuroda, T.; Aoyama, T. Effect of a Kinect-based exercise game on improving executive cognitive performance in community-dwelling elderly: Case control study. J. Med. Internet Res. 2014, 16, e61. [Google Scholar] [CrossRef] [Green Version]
- Parajuli, M.; Dat, T.; Wanli, M.; Sharma, D. Senior health monitoring using Kinect. In Proceedings of the 2012 Fourth International Conference on Communications and Electronics (ICCE), Hue, Vietnam, 1–3 August 2012; pp. 309–312. [Google Scholar]
- Cao, W.; Zhong, J.; Cao, G.; He, Z. Physiological Function Assessment Based on Kinect V2. IEEE Access 2019, 7, 105638–105651. [Google Scholar] [CrossRef]
- Burle, A.d.Q.; Lafayette, T.B.d.G.; Fonseca, J.R.; Teichrieb, V.; Gama, A.E.F.D. Real-time approach for gait analysis using the Kinect v2 sensor for clinical assessment purpose. In Proceedings of the 2020 22nd Symposium on Virtual and Augmented Reality (SVR), Porto de Galinhas, Brazil, 7–10 November 2020; pp. 144–153. [Google Scholar]
- Jang, J.; Kim, D.; Park, C.; Jang, M.; Lee, J.; Kim, J. ETRI-Activity3D: A Large-Scale RGB-D Dataset for Robots to Recognize Daily Activities of the Elderly. In Proceedings of the 2020 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), Las Vegas, NV, USA, 24 October–24 January 2020; pp. 10990–10997. [Google Scholar]
- Alexander, N.B.; Koester, D.J.; Grunawalt, J.A. Chair design affects how older adults rise from a chair. J. Am. Geriatr. Soc. 1996, 44, 356–362. [Google Scholar] [CrossRef] [Green Version]
- Kuo, Y.L.; Tully, E.A.; Galea, M.P. Kinematics of sagittal spine and lower limb movement in healthy older adults during sit-to-stand from two seat heights. Spine 2010, 35, E1-7. [Google Scholar] [CrossRef] [PubMed]
- Kinoshita, S.; Kiyama, R.; Yoshimoto, Y. Effect of Handrail Height on Sit-To-Stand Movement. PLoS ONE 2015, 10, e0133747. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murata, E.; Kitamura, K.; Oono, M.; Shirato, Y.; Nishida, Y. Behavior Monitoring with Non-wearable Sensors for Precision Nursing. In Proceedings of the Advances in Safety Management and Human Factors, Los Angeles, CA, USA, 17–21 July 2017; pp. 384–392. [Google Scholar]
- Nishida, Y.; Kitamura, K. Living Function-Resilient Society in the Centenarian Era: Living Safety Technology Based on Connective, Artificial Intelligence. In IoT and Smart Applications; IntechOpen: London, UK, 2019. [Google Scholar]
- AIST. Elderly Behavior Library. Available online: https://www.behavior-library-meti.com/behaviorLib/homes/about (accessed on 29 October 2021).
- Mahoney, F.I.; Barthel, D.W. Functional Evaluation: The Barthel Index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar] [PubMed]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Hirano, K.; Shoda, K.; Kitamura, K.; Miyazaki, Y.; Nishida, Y. Method for Behavior Normalization to Enable Comparative Understanding of Interactions of Elderly Persons with Consumer Products using a Behavior Video Database. Procedia Comput. Sci. 2019, 160, 409–416. [Google Scholar] [CrossRef]
- Najafi, B.; Aminian, K.; Loew, F.; Blanc, Y.; Robert, P.A. Measurement of stand-sit and sit-stand transitions using a miniature gyroscope and its application in fall risk evaluation in the elderly. IEEE Trans. Biomed. Eng. 2002, 49, 843–851. [Google Scholar] [CrossRef]
- Chorin, F.; Cornu, C.; Beaune, B.; Frère, J.; Rahmani, A. Sit to stand in elderly fallers vs non-fallers: New insights from force platform and electromyography data. Aging Clin. Exp. Res. 2016, 28, 871–879. [Google Scholar] [CrossRef]
- Riley, P.O.; Schenkman, M.L.; Mann, R.W.; Hodge, W.A. Mechanics of a constrained chair-rise. J. Biomech. 1991, 24, 77–85. [Google Scholar] [CrossRef]
- Schultz, A.B.; Alexander, N.B.; Ashton-Miller, J.A. Biomechanical analyses of rising from a chair. J. Biomech. 1992, 25, 1383–1391. [Google Scholar] [CrossRef] [Green Version]
- Hughes, M.A.; Weiner, D.K.; Schenkman, M.L.; Long, R.M.; Studenski, S.A. Chair rise strategies in the elderly. Clin. Biomech. 1994, 9, 187–192. [Google Scholar] [CrossRef]
- Fotoohabadi, M.R.; Tully, E.A.; Galea, M.P. Kinematics of rising from a chair: Image-based analysis of the sagittal hip-spine movement pattern in elderly people who are healthy. Phys. Ther. Rehabil. J. 2010, 90, 561–571. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anan, M.; Hattori, H.; Tanimoto, K.; Wakimoto, Y.; Ibara, T.; Kito, N.; Shinkoda, K. The coordination of joint movements during sit-to-stand motion in old adults: The uncontrolled manifold analysis. Phys. Ther. Res. 2017, 20, 44–50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walgaard, S.; Faber, G.S.; van Lummel, R.C.; van Dieën, J.H.; Kingma, I. The validity of assessing temporal events, sub-phases and trunk kinematics of the sit-to-walk movement in older adults using a single inertial sensor. J. Biomech. 2016, 49, 1933–1937. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Atrsaei, A.; Dadashi, F.; Hansen, C.; Warmerdam, E.; Mariani, B.; Maetzler, W.; Aminian, K. Postural transitions detection and characterization in healthy and patient populations using a single waist sensor. J. NeuroEng. Rehabil. 2020, 17, 70. [Google Scholar] [CrossRef] [PubMed]
- Nose, T.; Kitamura, K.; Oono, M.; Nishida, Y.; Ohkura, M. Automatic Learning of Climbing Configuration Space for Digital Human Children Model. In Advances in Human Factors in Simulation and Modeling; Springer: Berlin/Heidelberg, Germany, 2019; pp. 483–490. [Google Scholar]
- Sokal, R.R.; Michener, C.D.; Kansas, U.O. A Statistical Method for Evaluating Systematic Relationships; University of Kansas: Lawrence, KS, USA, 1958. [Google Scholar]
- Ward, J.H. Hierarchical Grouping to Optimize an Objective Function. J. Am. Stat. Assoc. 1963, 58, 236–244. [Google Scholar] [CrossRef]
- Rousseeuw, P.J. Silhouettes: A graphical aid to the interpretation and validation of cluster analysis. J. Comput. Appl. Math. 1987, 20, 53–65. [Google Scholar] [CrossRef] [Green Version]
- Alexander, N.B.; Galecki, A.T.; Nyquist, L.V.; Hofmeyer, M.R.; Grunawalt, J.C.; Grenier, M.L.; Medell, J.L. Chair and bed rise performance in ADL-impaired congregate housing residents. J. Am. Geriatr. Soc. 2000, 48, 526–533. [Google Scholar] [CrossRef] [Green Version]
- Shia, V.; Moore, T.Y.; Holmes, P.; Bajcsy, R.; Vasudevan, R. Stability basin estimates fall risk from observed kinematics, demonstrated on the Sit-to-Stand task. J. Biomech. 2018, 72, 37–45. [Google Scholar] [CrossRef]
- Norman-Gerum, V.; McPhee, J. Comprehensive description of sit-to-stand motions using force and angle data. J. Biomech. 2020, 112, 110046. [Google Scholar] [CrossRef]
- Das, S.; Dai, R.; Koperski, M.; Minciullo, L.; Garattoni, L.; Bremond, F.; Francesca, G. Toyota Smarthome: Real-World Activities of Daily Living. In Proceedings of the 2019 IEEE/CVF International Conference on Computer Vision (ICCV), Seoul, Korea, 27 October–2 November 2019; pp. 833–842. [Google Scholar]
- Liu, J.; Shahroudy, A.; Perez, M.; Wang, G.; Duan, L.Y.; Kot, A.C. NTU RGB+D 120: A Large-Scale Benchmark for 3D Human Activity Understanding. IEEE Trans. Pattern Anal. Mach. Intell. 2020, 42, 2684–2701. [Google Scholar] [CrossRef] [Green Version]









| ID | Sex | BI | MMSE | Product |
|---|---|---|---|---|
| no9_1 | M | 55 | 22 | Nursing bed |
| no9_2 | M | 55 | 22 | Nursing bed |
| no9_3 | M | 55 | 22 | Nursing bed |
| no9_4 | M | 55 | 22 | Nursing bed |
| no9_5 | M | 55 | 22 | Nursing bed |
| no29_1 | F | 85 | 19 | Chair |
| no29_2 | F | 85 | 19 | Chair |
| no29_3 | F | 85 | 19 | Chair |
| no29_4 | F | 85 | 19 | Chair |
| no30_1 | M | 80 | 24 | Sofa |
| no30_2 | M | 80 | 24 | Sofa |
| no30_3 | M | 80 | 24 | Chair |
| no30_4 | M | 80 | 24 | Sofa |
| no31_1 | F | 55 | 6 | Chair |
| no31_2 | F | 55 | 6 | Sofa |
| no31_3 | F | 55 | 6 | Chair |
| no31_4 | F | 55 | 6 | Sofa |
| no32_1 | M | 55 | 17 | Sofa |
| no32_2 | M | 55 | 17 | Sofa |
| no32_3 | M | 55 | 17 | Sofa |
| no33_1 | F | 55 | 15 | Sofa |
| no33_2 | F | 55 | 15 | Chair |
| no33_3 | F | 55 | 15 | Sofa |
| no33_4 | F | 55 | 15 | Sofa |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miyazaki, Y.; Hirano, K.; Kitamura, K.; Nishida, Y. Analysis of Relationship between Natural Standing Behavior of Elderly People and a Class of Standing Aids in a Living Space. Sensors 2022, 22, 1178. https://doi.org/10.3390/s22031178
Miyazaki Y, Hirano K, Kitamura K, Nishida Y. Analysis of Relationship between Natural Standing Behavior of Elderly People and a Class of Standing Aids in a Living Space. Sensors. 2022; 22(3):1178. https://doi.org/10.3390/s22031178
Chicago/Turabian StyleMiyazaki, Yusuke, Kei Hirano, Koji Kitamura, and Yoshifumi Nishida. 2022. "Analysis of Relationship between Natural Standing Behavior of Elderly People and a Class of Standing Aids in a Living Space" Sensors 22, no. 3: 1178. https://doi.org/10.3390/s22031178





