The Development and Concurrent Validity of a Multi-Sensor-Based Frailty Toolkit for In-Home Frailty Assessment
Abstract
:1. Introduction
- FT consists of a unique and new collection of heterogeneous customized sensors that use off-the-shelf sensing modules. FT was tailored for home-based frailty assessment by measuring early behavioral signs of frailty under free-living conditions in older adults’ daily lives. The system does not require older adults to perform standardized physical tests, such as gait speed tests or chair stand tests, which could need extra supervision and compliance to perform correctly. FT consists of a unique and new collection of heterogeneous off-the-shelf sensors tailored for home-based frailty assessment. The sensors measure early behavioral signs of frailty in older adults’ daily lives.
- FT uses state-of-the-art cloud services from major commercial cloud service providers. The cloud technologies enable real-time telecommunication and the use of advanced data analytics. The use of cloud services can benefit research data analysis for this study and future real-world deployment of similar systems in terms of implementation process and lessons learned.
- FT makes no use of cameras or wearable sensors. Such devices are perceived to have privacy and obtrusiveness concerns, undermining user acceptance. Instead, ambient sensors require minimal effort from end-users to monitor frailty. Users are not required to carry any device.
- The design of FT involves older adults’ perspectives from the beginning to enhance its usability.
2. Materials and Methods
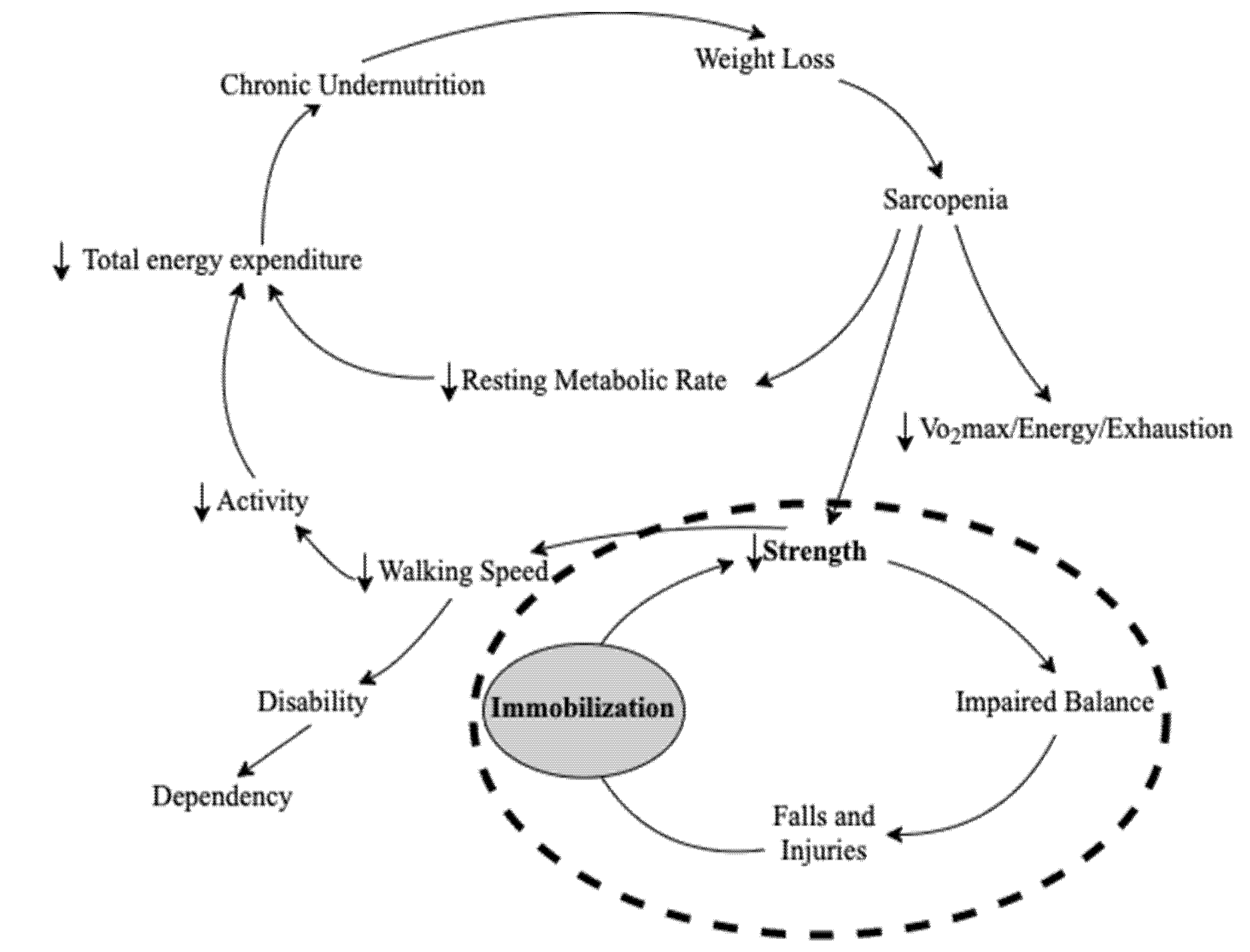
2.1. Frailty Criteria and Sensor Selection
2.1.1. Strength
- tunoccupied = the time when a mat sensor detects an unoccupied seat
- tpre_occupied = the time when a mat sensor detects a previously occupied seat
- tdistance_sensor1 = the time when the first distance sensor detects a person’s proximity
- tdistance_sensor2 = the time when the second distance sensor detects a person’s proximity
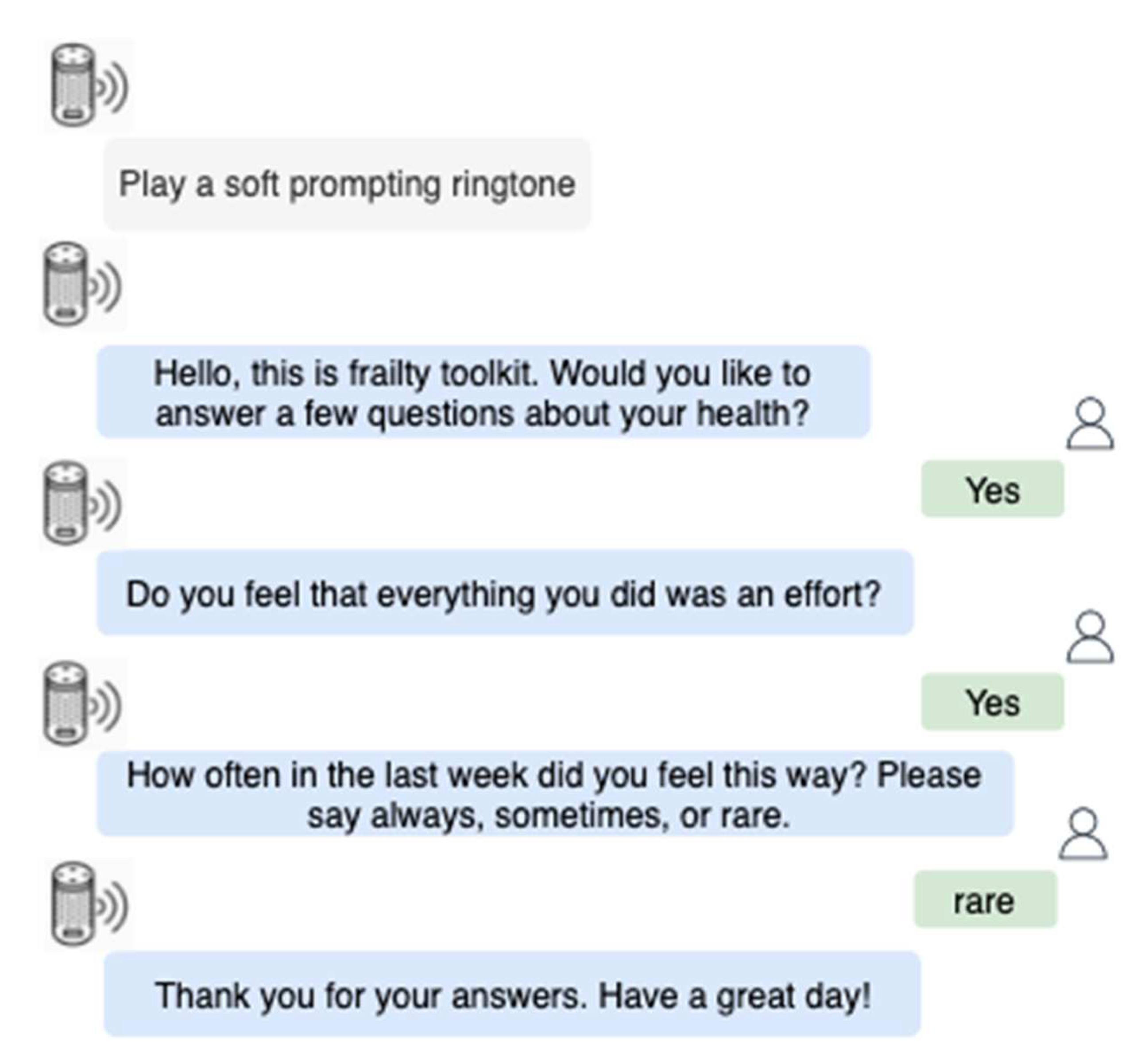
2.1.2. Self-Report Exhaustion
2.1.3. Physical Activity
- tnext_motion_sensor = the first confirmed time when the next motion sensor detects a person
- tpre_motion_sensor = the first confirmed time when the previous motion sensor detects a person.
2.1.4. Weight
2.1.5. Life Space Mobility
- tdoor_event = the time when a door sensor detects a door opening event
- tpre_door_event = the time of a previous door opening event
2.2. User-Centred Design
2.3. Protocol
- Minimum 18 years old;
- Able to understand and speak English;
- Able to give informed consent;
- Able to attend at least one experiment session.
- Have trouble getting in and out of bed without assistance;
- Have trouble walking or always use a wheelchair;
- Cannot speak due to speech impairment;
- Cannot hear due to hearing impairment.
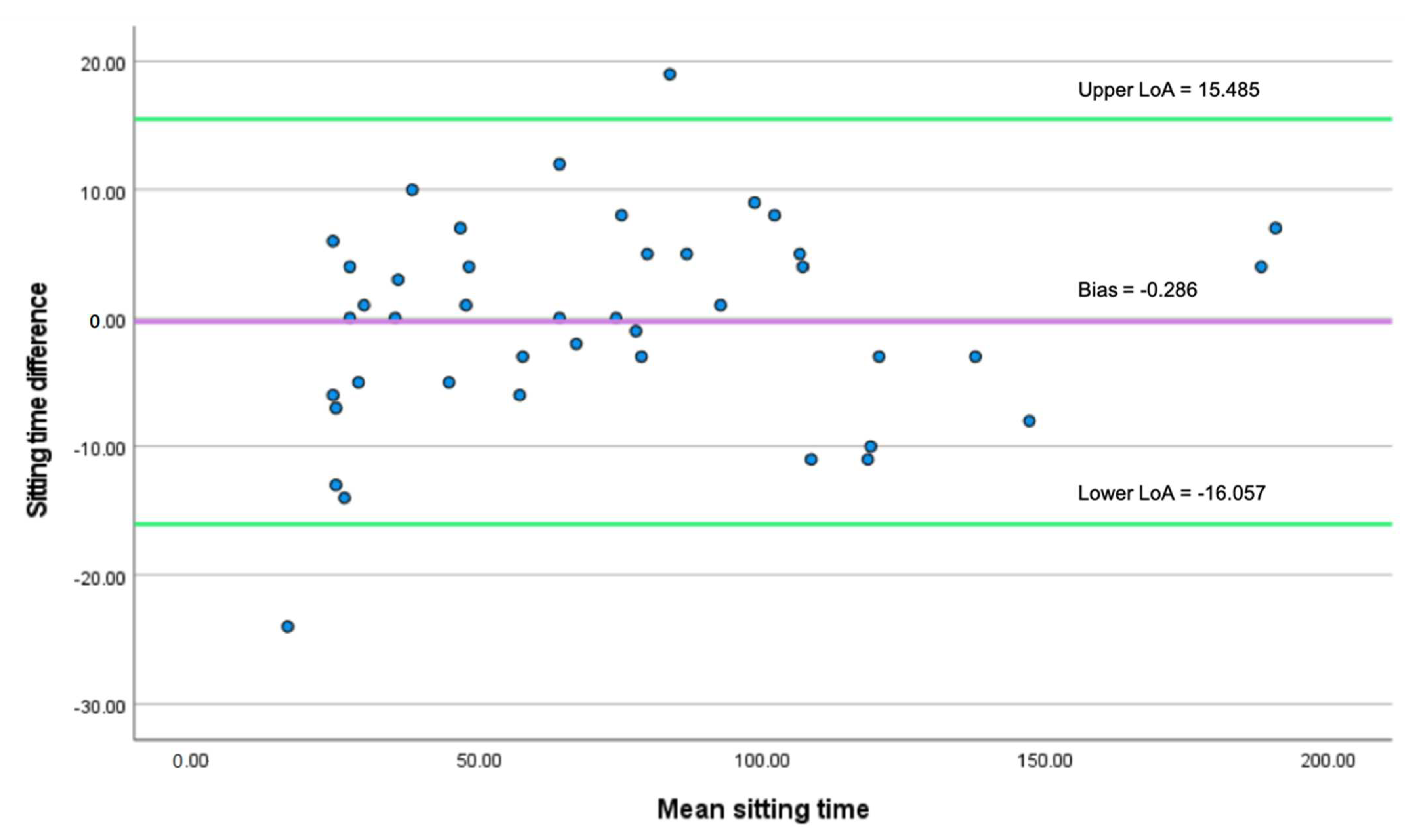
2.4. Data Processing
- po = the relative observed agreement between the sensor and ground truth measurement
- pe = the hypothetical probability of chance agreement
3. Results
3.1. The Smart Speaker for Self-Report Exhaustion
3.2. The Motion Sensor for Room-Level Physical Activity
3.3. The Door Sensor for Life-Space Mobility
3.4. The Mat Sensors for Sedentary Behavior
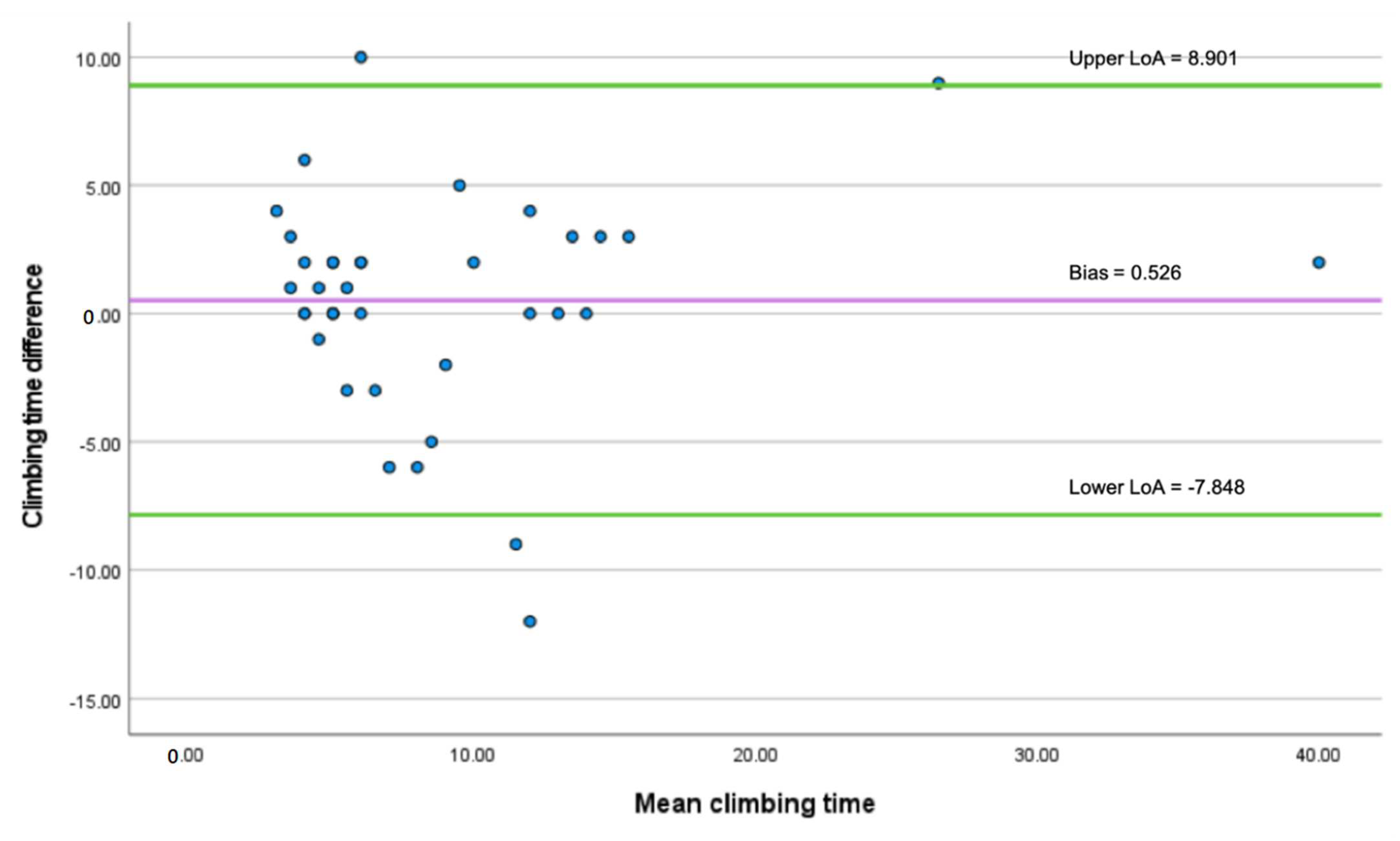
3.5. The Distance Sensors for Stair Climbing Time
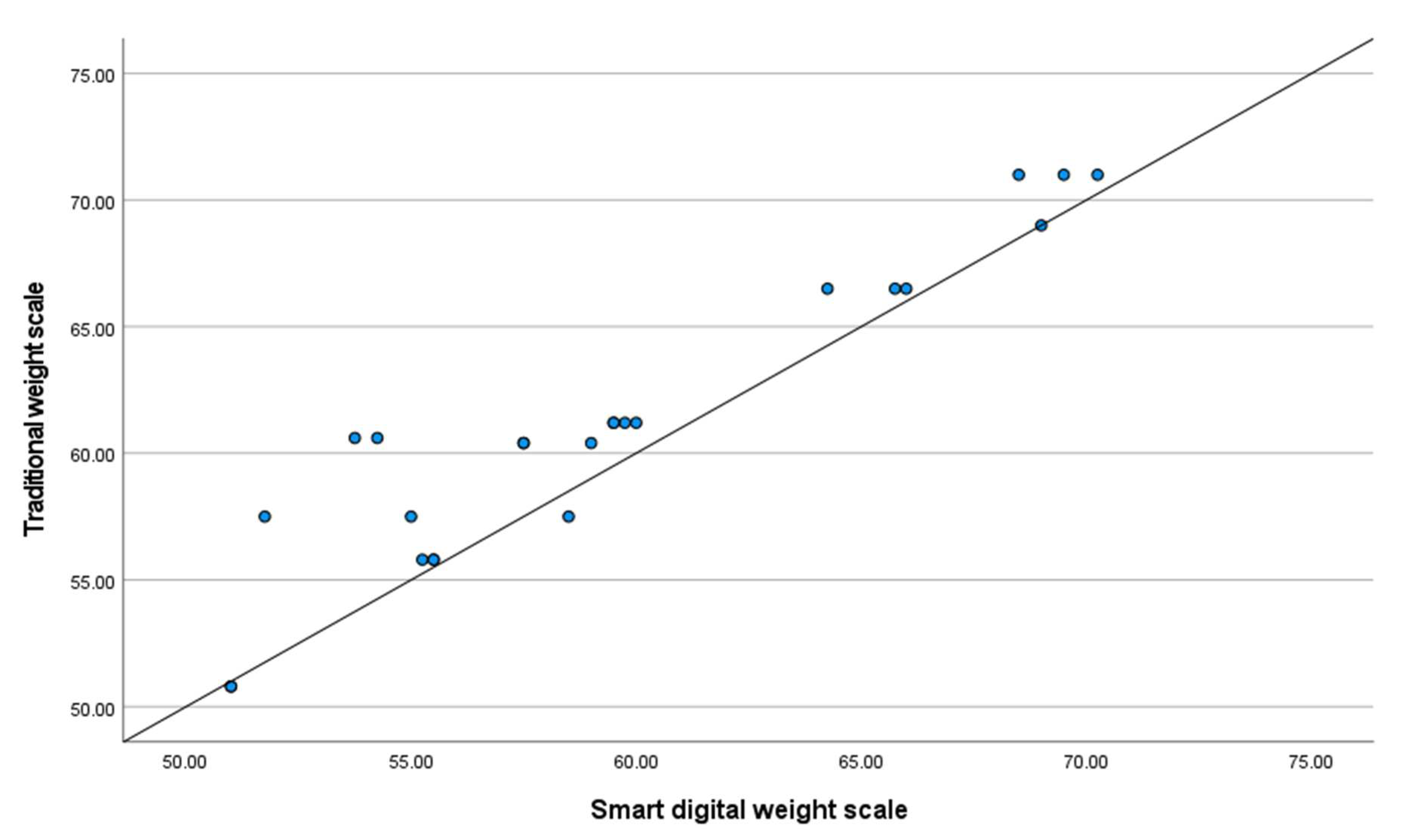
3.6. The Smart Weight Scale for Weight
4. Discussion
- Test the system in HomeLab with non-frail and frail participants to validate the effectiveness of the frailty assessment. The test would also allow more data collection for training a machine learning model for classifying non-frail and frail older adults.
- Move the system from the simulated home to an actual home of an older adult who lives alone. While older adults continue to live their own lives, the system will continuously run for a week to collect data. The data will be compared with the older adult’s frailty status measured by a reference clinical frailty scale.
- Develop sensors to measure new frailty criteria or phenotypes in different domains and identify other persons living in the same household.
- Compare sensors in FT with wearable sensors to validate the effectiveness of measuring certain frailty signs such as physical activity using ambient sensors.
- Consult with clinicians to investigate how the data provided by FT would be made palatable and useful for them.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- United Nations, Department of Economic and Social Affairs, P.D. World Population Prospects 2019: Highlights (ST/ESA/SER.A/423). 2019. Available online: https://population.un.org/wpp/Publications/Files/WPP2019_Highlights.pdf (accessed on 26 April 2022).
- Polanczyk, C.A.; Marcantonio, E.; Goldman, L.; Rohde, L.E.P.; Orav, J.; Mangione, C.M.; Lee, T.H. Impact of Age on Perioperative Complications and Length of Stay in Patients Undergoing Noncardiac Surgery. Ann. Intern. Med. 2001, 134, 637. [Google Scholar] [CrossRef] [PubMed]
- Davenport, D.L.; Bowe, E.A.; Henderson, W.G.; Khuri, S.F.; Mentzer, R.M. National Surgical Quality Improvement Program (NSQIP) Risk Factors Can Be Used to Validate American Society of Anesthesiologists Physical Status Classification (ASA PS) Levels. Ann. Surg. 2006, 243, 636–644. [Google Scholar] [CrossRef] [PubMed]
- Makary, M.A.; Segev, D.L.; Pronovost, P.J.; Syin, D.; Bandeen-Roche, K.; Patel, P.; Takenaga, R.; Devgan, L.; Holzmueller, C.G.; Tian, J.; et al. Frailty as a Predictor of Surgical Outcomes in Older Patients. J. Am. Coll. Surg. 2010, 210, 901–908. [Google Scholar] [CrossRef] [PubMed]
- Rockwood, K.; Andrew, M.; Mitnitski, A. A Comparison of Two Approaches to Measuring Frailty in Elderly People. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2007, 62, 738–743. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in Older Adults: Evidence for a Phenotype. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M146–M157. [Google Scholar] [CrossRef]
- Hoogendijk, E.O.; Afilalo, J.; Ensrud, K.E.; Kowal, P.; Onder, G.; Fried, L.P. Frailty: Implications for Clinical Practice and Public Health. Lancet 2019, 394, 1365–1375. [Google Scholar] [CrossRef]
- Maresova, P.; Javanmardi, E.; Barakovic, S.; Barakovic Husic, J.; Tomsone, S.; Krejcar, O.; Kuca, K. Consequences of Chronic Diseases and Other Limitations Associated with Old Age—A Scoping Review. BMC Public Health 2019, 19, 1431. [Google Scholar] [CrossRef]
- Mondor, L.; Maxwell, C.J.; Hogan, D.B.; Bronskill, S.E.; Campitelli, M.A.; Seitz, D.P.; Wodchis, W.P. The Incremental Health Care Costs of Frailty Among Home Care Recipients With and Without Dementia in Ontario, Canada. Med. Care 2019, 57, 512–520. [Google Scholar] [CrossRef]
- Hajek, A.; Bock, J.-O.; Saum, K.-U.; Matschinger, H.; Brenner, H.; Holleczek, B.; Haefeli, W.E.; Heider, D.; König, H.-H. Frailty and Healthcare Costs—Longitudinal Results of a Prospective Cohort Study. Age Ageing 2018, 47, 233–241. [Google Scholar] [CrossRef] [Green Version]
- Gill, T.M.; Gahbauer, E.A.; Allore, H.G.; Han, L. Transitions Between Frailty States Among Community-Living Older Persons. Arch. Intern. Med. 2006, 166, 418. [Google Scholar] [CrossRef]
- Fallah, N.; Mitnitski, A.; Searle, S.D.; Gahbauer, E.A.; Gill, T.M.; Rockwood, K. Transitions in Frailty Status in Older Adults in Relation to Mobility: A Multistate Modeling Approach Employing a Deficit Count. J. Am. Geriatr. Soc. 2011, 59, 524–529. [Google Scholar] [CrossRef]
- Xue, Q.L. The Frailty Syndrome: Definition and Natural History. Clin. Geriatr. Med. 2011, 27, 1–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Toosizadeh, N.; Mohler, J.; Najafi, B. Assessing Upper Extremity Motion: An Innovative Method to Identify Frailty. J. Am. Geriatr. Soc. 2015, 63, 1181–1186. [Google Scholar] [CrossRef] [PubMed]
- Soaz, C.; Diepold, K. Step Detection and Parameterization for Diagnosis and Monitoring of Functional Decline Using a Single Waist-Worn Accelerometer. IEEE Trans. Biomed. Eng. 2015, 63, 933–942. [Google Scholar] [CrossRef] [PubMed]
- Schwenk, M.; Mohler, J.; Wendel, C.; D’’Huyvetter, K.; Fain, M.; Taylor-Piliae, R.; Najafi, B. Wearable Sensor-Based in-Home Assessment of Gait, Balance, and Physical Activity for Discrimination of Frailty Status: Baseline Results of the Arizona Frailty Cohort Study. Gerontology 2015, 61, 258–267. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Greene, B.R.; Doheny, E.P.; O’Halloran, A.; Kenny, R.A. Frailty Status Can Be Accurately Assessed Using Inertial Sensors and the TUG Test. Age Ageing 2014, 43, 406–411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gianaria, E.; Grangetto, M.; Roppolo, M.; Mulasso, A.; Rabaglietti, E. Kinect-Based Gait Analysis for Automatic Frailty Syndrome Assessment. In Proceedings of the 2016 IEEE International Conference on Image Processing (ICIP), Phoenix, AZ, USA, 25–28 September 2016; pp. 1314–1318. [Google Scholar] [CrossRef] [Green Version]
- Jaber, R.; Chkeir, A.; Hewson, D.J.; Duchene, J. A New Device to Assess Gait Velocity at Home. IFMBE Proc. 2014, 41, 670–673. [Google Scholar] [CrossRef] [Green Version]
- Ferre, X.; Villalba-Mora, E.; Caballero-Mora, M.-A.; Sanchez, A.; Aguilera, W.; Garcia-Grossocordon, N.; Nuñez-Jimenez, L.; Rodríguez-Mañas, L.; Liu, Q.; del Pozo-Guerrero, F. Gait Speed Measurement for Elderly Patients with Risk of Frailty. Mob. Inf. Syst. 2017, 2017, 1310345. [Google Scholar] [CrossRef]
- Chang, Y.C.; Lin, C.C.; Lin, P.H.; Chen, C.C.; Lee, R.G.; Huang, J.S.; Tsai, T.H. EFurniture for Home-Based Frailty Detection Using Artificial Neural Networks and Wireless Sensors. Med. Eng. Phys. 2013, 35, 263–268. [Google Scholar] [CrossRef]
- del Pozo-Cruz, B.; Mañas, A.; Martín-García, M.; Marín-Puyalto, J.; García-García, F.J.; Rodriguez-Mañas, L.; Guadalupe-Grau, A.; Ara, I. Frailty Is Associated with Objectively Assessed Sedentary Behaviour Patterns in Older Adults: Evidence from the Toledo Study for Healthy Aging (TSHA). PLoS ONE 2017, 12, e0183911. [Google Scholar] [CrossRef]
- Tuttle, L.J.; Bittel, D.C.; Bittel, A.J.; Sinacore, D.R. Early-Onset Physical Frailty in Adults With Diabesity and Peripheral Neuropathy. Can. J. Diabetes 2018, 42, 478–483. [Google Scholar] [CrossRef] [PubMed]
- Merry, K.J.; Macdonald, E.; MacPherson, M.; Aziz, O.; Park, E.; Ryan, M.; Sparrey, C.J. Classifying Sitting, Standing, and Walking Using Plantar Force Data. Med. Biol. Eng. Comput. 2021, 59, 257–270. [Google Scholar] [CrossRef] [PubMed]
- Zijlstra, W.; Giannouli, E. Mobility in Community-Dwelling Older Adults; What Are Its Determinants? BMC Geriatr. 2021, 21, 228. [Google Scholar] [CrossRef]
- Ganea, R.; Paraschiv-Ionescu, A.; Büla, C.; Rochat, S.; Aminian, K. Multi-Parametric Evaluation of Sit-to-Stand and Stand-to-Sit Transitions in Elderly People. Med. Eng. Phys. 2011, 33, 1086–1093. [Google Scholar] [CrossRef] [PubMed]
- Millor, N.; Lecumberri, P.; Gómez, M.; Martínez-Ramírez, A.; Izquierdo, M. An Evaluation of the 30-s Chair Stand Test in Older Adults: Frailty Detection Based on Kinematic Parameters from a Single Inertial Unit. J. NeuroEngineering Rehabil. 2013, 10, 86. [Google Scholar] [CrossRef] [Green Version]
- Hellmers, S.; Kromke, T.; Dasenbrock, L.; Heinks, A.; Bauer, J.M.; Hein, A.; Fudickar, S. Stair Climb Power Measurements via Inertial Measurement Units—Towards an Unsupervised Assessment of Strength in Domestic Environments. In Proceedings of the 11th International Conference on Health Informatics (HEALTHINF), Madeira, Portugal, 19–21 January 2018; Volume 5, pp. 39–47. [Google Scholar]
- Allin, S.; Mihailidis, A. Low-Cost, Automated Assessment of Sit-To-Stand Movement in “Natural” Environments. In Proceedings of the IFMBE; Springer: Berlin/Heidelberg, Germany, 2009. [Google Scholar]
- Bérubé, C.; Schachner, T.; Keller, R.; Fleisch, E.; v Wangenheim, F.; Barata, F.; Kowatsch, T. Voice-Based Conversational Agents for the Prevention and Management of Chronic and Mental Health Conditions: Systematic Literature Review. J. Med. Internet Res. 2021, 23, e25933. [Google Scholar] [CrossRef]
- Piau, A.; Charlon, Y.; Campo, E.; Vellas, B.; Nourhashemi, F. A Smart Insole to Promote Healthy Aging for Frail Elderly Individuals: Specifications, Design, and Preliminary Results. JMIR Rehabil. Assist. Technol. 2015, 2, e5. [Google Scholar] [CrossRef]
- Dasios, A.; Gavalas, D.; Pantziou, G.; Konstantopoulos, C. Hands-On Experiences in Deploying Cost-Effective Ambient-Assisted Living Systems. Sensors 2015, 15, 14487–14512. [Google Scholar] [CrossRef] [Green Version]
- Griebel, L.; Prokosch, H.-U.; Köpcke, F.; Toddenroth, D.; Christoph, J.; Leb, I.; Engel, I.; Sedlmayr, M. A Scoping Review of Cloud Computing in Healthcare. BMC Med. Inform. Decis. Mak. 2015, 15, 17. [Google Scholar] [CrossRef] [Green Version]
- Xue, Q.L.; Bandeen-Roche, K.; Varadhan, R.; Zhou, J.; Fried, L.P. Initial Manifestations of Frailty Criteria and the Development of Frailty Phenotype in the Women’s Health and Aging Study II. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2008, 63, 984–990. [Google Scholar] [CrossRef] [Green Version]
- Piau, A.; Mattek, N.; Crissey, R.; Beattie, Z.; Dodge, H.; Kaye, J. When Will My Patient Fall? Sensor-Based In-Home Walking Speed Identifies Future Falls in Older Adults. J. Gerontol. Ser. A 2020, 75, 968–973. [Google Scholar] [CrossRef] [PubMed]
- Stone, E.; Skubic, M.; Rantz, M.; Abbott, C.; Miller, S. Average In-Home Gait Speed: Investigation of a New Metric for Mobility and Fall Risk Assessment of Elders. Gait Posture 2015, 41, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Freire Junior, R.C.; Porto, J.M.; Rodrigues, N.C.; Brunelli, R.D.M.; Braga, L.F.P.; Abreu, D.C.C. Spatial and Temporal Gait Characteristics in Pre-Frail Community-Dwelling Older Adults. Geriatr. Gerontol. Int. 2016, 16, 1102–1108. [Google Scholar] [CrossRef]
- Klebbe, R.; Steinert, A.; Müller-Werdan, U. Wearables for Older Adults: Requirements, Design, and User Experience. In Perspectives on Wearable Enhanced Learning (WELL); Springer International Publishing: Cham, Switzerland, 2019; pp. 313–332. [Google Scholar]
- Schreier, G.; Eckmann, H.; Hayn, D.; Kreiner, K.; Kastner, P.; Lovell, N. Web versus App—Compliance of Patients in a Telehealth Diabetes Management Programme Using Two Different Technologies. J. Telemed. Telecare 2012, 18, 476–480. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Sandoval, D.; Favela, J.; Lopez-Nava, I.H.; Morales, A. Adoption of Wearable Devices by Persons with Dementia: Lessons from a Non-Pharmacological Intervention Enabled by a Social Robot. In IoT in Healthcare and Ambient Assisted Living; Springer: Singapore, 2021; pp. 145–163. [Google Scholar]
- Li, L.; Peng, W.; Kamp, K.; Bowen, M.; Cotten, S.R.; Rikard, R.V.; Kononova, A. Poster: Understanding Long-Term Adoption of Wearable Activity Trackers among Older Adults. In Proceedings of the 2017 Workshop on Wearable Systems and Applications, Niagara Falls, NY, USA, 19 June 2017; pp. 33–34. [Google Scholar]
- Jaber, R.; Chkeir, A.; Hewson, D.; Duchene, J. ARPEGE: Assessment of Frailty at Home. In Proceedings of the 2013 IEEE 15th International Conference on e-Health Networking, Applications and Services, Lisbon, Portugal, 9–12 October 2013; Healthcom: Sullivan, IL, USA; pp. 434–438. [Google Scholar] [CrossRef]
- Bautmans, I.; van Puyvelde, K.; Mets, T. Sarcopenia and Functional Decline: Pathophysiology, Prevention and Therapy. Acta Clin. Belg. 2009, 64, 303–316. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santilli, V.; Bernetti, A.; Mangone, M.; Paoloni, M. Clinical Definition of Sarcopenia. Clin. Cases Miner. Bone Metab. 2014, 11, 177–180. [Google Scholar] [CrossRef]
- Mohlberg, W.; Sieber, C. Sarcopenia and Frailty in Geriatric Patients: Implications for Training and Prevention. Z. Für Gerontol. Und Geriatr. 2004, 37, 2–8. [Google Scholar] [CrossRef]
- BELL, K.E.; von Allmen, M.T.; Devries, M.C.; Phillips, S.M. Muscle Disuse as a Pivotal Problem in Sarcopenia-related Muscle Loss and Dysfunction. J. Frailty Aging 2016, 1–9. [Google Scholar] [CrossRef]
- Charansonney, O.L.; Després, J.-P. Disease Prevention—Should We Target Obesity or Sedentary Lifestyle? Nat. Rev. Cardiol. 2010, 7, 468–472. [Google Scholar] [CrossRef]
- Nightingale, E.J.; Pourkazemi, F.; Hiller, C.E. Systematic Review of Timed Stair Tests. J. Rehabil. Res. Dev. 2014, 51, 335–350. [Google Scholar] [CrossRef]
- Orme, J.G.; Reis, J.; Herz, E.J. Factorial and Discriminant Validity of the Center for Epidemiological Studies Depression (CES-D) Scale. J. Clin. Psychol. 1986, 42, 28–33. [Google Scholar] [CrossRef]
- Fuller, D.; Colwell, E.; Low, J.; Orychock, K.; Tobin, M.A.; Simango, B.; Buote, R.; van Heerden, D.; Luan, H.; Cullen, K.; et al. Reliability and Validity of Commercially Available Wearable Devices for Measuring Steps, Energy Expenditure, and Heart Rate: Systematic Review. JMIR Mhealth Uhealth 2020, 8, e18694. [Google Scholar] [CrossRef]
- Myers, A.; Johnston, N.; Rathod, V.; Korattikara, A.; Gorban, A.; Silberman, N.; Guadarrama, S.; Papandreou, G.; Huang, J.; Murphy, K. Im2Calories: Towards an Automated Mobile Vision Food Diary. In Proceedings of the 2015 IEEE International Conference on Computer Vision (ICCV), Santiago, Chile, 7–13 December 2015; pp. 1233–1241. [Google Scholar]
- Tegou, T.; Kalamaras, I.; Tsipouras, M.; Giannakeas, N.; Votis, K. A Low-Cost Indoor Activity Monitoring System for Detecting Frailty in Older Adults. Sensors 2019, 19, 452. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doyle, J.; Bailey, C.; Ni Scanaill, C.; van den Berg, F. Lessons Learned in Deploying Independent Living Technologies to Older Adults’ Homes. Univers. Access Inf. Soc. 2013, 13, 191–204. [Google Scholar] [CrossRef] [Green Version]
- Bian, C.; Ye, B.; Hoonakker, A.; Mihailidis, A. Attitudes and Perspectives of Older Adults on Technologies for Assessing Frailty in Home Settings: A Focus Group Study. BMC Geriatr. 2021, 21, 298. [Google Scholar] [CrossRef]
- Keogh, A.; Dorn, J.F.; Walsh, L.; Calvo, F.; Caulfield, B. Comparing the Usability and Acceptability of Wearable Sensors Among Older Irish Adults in a Real-World Context: Observational Study. JMIR Mhealth Uhealth 2020, 8, e15704. [Google Scholar] [CrossRef]
- Kovacshazy, T.; Fodor, G. New Approach to Passive Infrared Motion Sensors Signal Processing for Ambient Assisted Living Applications. In Proceedings of the 2012 IEEE International Instrumentation and Measurement Technology Conference Proceedings, Graz, Austria, 13–16 May 2012; pp. 2521–2525. [Google Scholar]
- Galán-Mercant, A.; Cuesta-Vargas, A.I. Clinical Frailty Syndrome Assessment Using Inertial Sensors Embedded in Smartphones. Physiol. Meas. 2015, 36, 1929–1942. [Google Scholar] [CrossRef]
- Fontecha, J.; Navarro, F.J.; Hervás, R.; Bravo, J. Elderly Frailty Detection by Using Accelerometer-Enabled Smartphones and Clinical Information Records. Pers. Ubiquitous Comput. 2013, 17, 1073–1083. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The Measurement of Observer Agreement for Categorical Data. Biometrics 1977, 33, 159. [Google Scholar] [CrossRef] [Green Version]
- Krakowiak, P.; Walker, C.K.; Tancredi, D.J.; Hertz-Picciotto, I. Maternal Recall Versus Medical Records of Metabolic Conditions from the Prenatal Period: A Validation Study. Matern. Child Health J. 2015, 19, 1925–1935. [Google Scholar] [CrossRef] [Green Version]
- Pursey, K.; Burrows, T.L.; Stanwell, P.; Collins, C.E. How Accurate Is Web-Based Self-Reported Height, Weight, and Body Mass Index in Young Adults? J. Med. Internet Res. 2014, 16, e4. [Google Scholar] [CrossRef] [PubMed]
- Muscedere, J.; Andrew, M.K.; Bagshaw, S.M.; Estabrooks, C.; Hogan, D.; Holroyd-Leduc, J.; Howlett, S.; Lahey, W.; Maxwell, C.; McNally, M.; et al. Screening for Frailty in Canada’s Health Care System: A Time for Action. Can. J. Aging/La Rev. Can. Du Vieil. 2016, 35, 281–297. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bian, C.; Ye, B.; Chu, C.H.; McGilton, K.S.; Mihailidis, A. Technology for Home-Based Frailty Assessment and Prediction: A Systematic Review. Gerontechnology 2020, 19, 3. [Google Scholar] [CrossRef]
- Chkeir, A.; Novella, J.L.; Dramé, M.; Bera, D.; Collart, M.; Duchêne, J. In-Home Physical Frailty Monitoring: Relevance with Respect to Clinical Tests. BMC Geriatr. 2019, 19, 34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
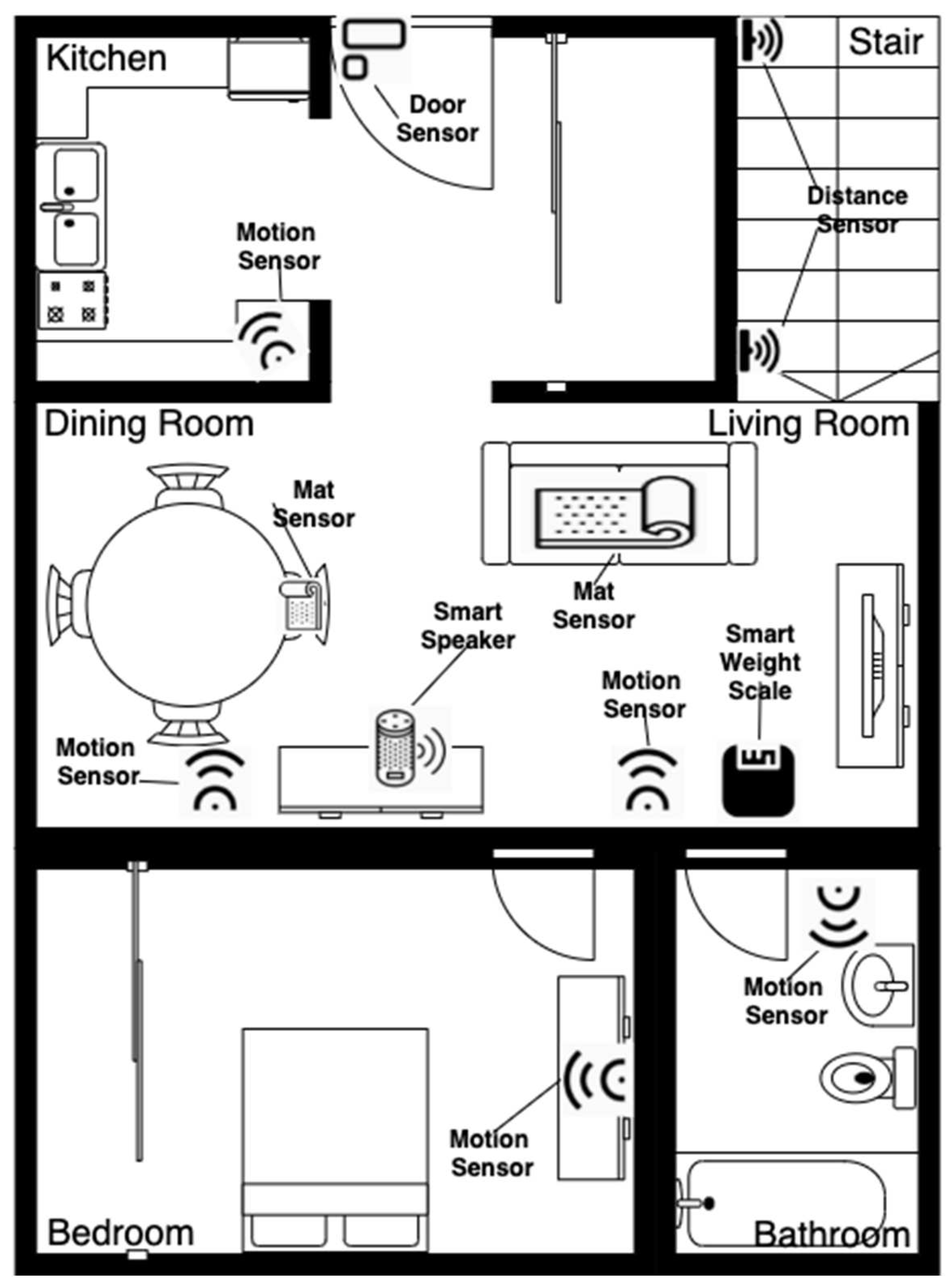

| Sensor | Frailty Criteria |
|---|---|
| Mat sensor | Strength through sedentary behavior |
| Distance sensor | Strength through stair climbing performance (ADL) |
| Smart speaker | Self-report exhaustion |
| Motion sensor | Physical activity, life-space mobility (indoor) |
| Door sensor | Life space mobility (outdoor) |
| Smart weight scale | Weight |
| Run | Run #1 | Run #2 | Run #3 |
|---|---|---|---|
| Run Type | Guided, normal pace | Self-paced, normal | Self-paced, slow (mimicking frail older adults) |
| Activity Type | Activities | ||
| Physical activity | Go to a room (e.g., living room) in HomeLab and do whatever activities in the room for 2 min. | ||
| Sedentary behavior | Sit on a chair that has a mat sensor. | ||
| Weight measuring | Measure weight using the smart weight scale. | ||
| Stair climbing | Climb a flight of stairs. | ||
| Self-report exhaustion | Have a conversation with the smart speaker. | ||
| Life space | Enter or exit HomeLab through the main entrance door. | ||
| Frequency | Percentage | |
|---|---|---|
| Detected | 35 | 87.5 |
| Undetected | 5 | 12.5 |
| Total | 40 | 100 |
| Frequency | Percentage | |
|---|---|---|
| Detected | 38 | 50 |
| Undetected | 38 | 50 |
| Total | 76 | 100 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bian, C.; Ye, B.; Mihailidis, A. The Development and Concurrent Validity of a Multi-Sensor-Based Frailty Toolkit for In-Home Frailty Assessment. Sensors 2022, 22, 3532. https://doi.org/10.3390/s22093532
Bian C, Ye B, Mihailidis A. The Development and Concurrent Validity of a Multi-Sensor-Based Frailty Toolkit for In-Home Frailty Assessment. Sensors. 2022; 22(9):3532. https://doi.org/10.3390/s22093532
Chicago/Turabian StyleBian, Chao, Bing Ye, and Alex Mihailidis. 2022. "The Development and Concurrent Validity of a Multi-Sensor-Based Frailty Toolkit for In-Home Frailty Assessment" Sensors 22, no. 9: 3532. https://doi.org/10.3390/s22093532






