Smartphone- and Paper-Based Delivery of Balance Intervention for Older Adults Are Equally Effective, Enjoyable, and of High Fidelity: A Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample Size
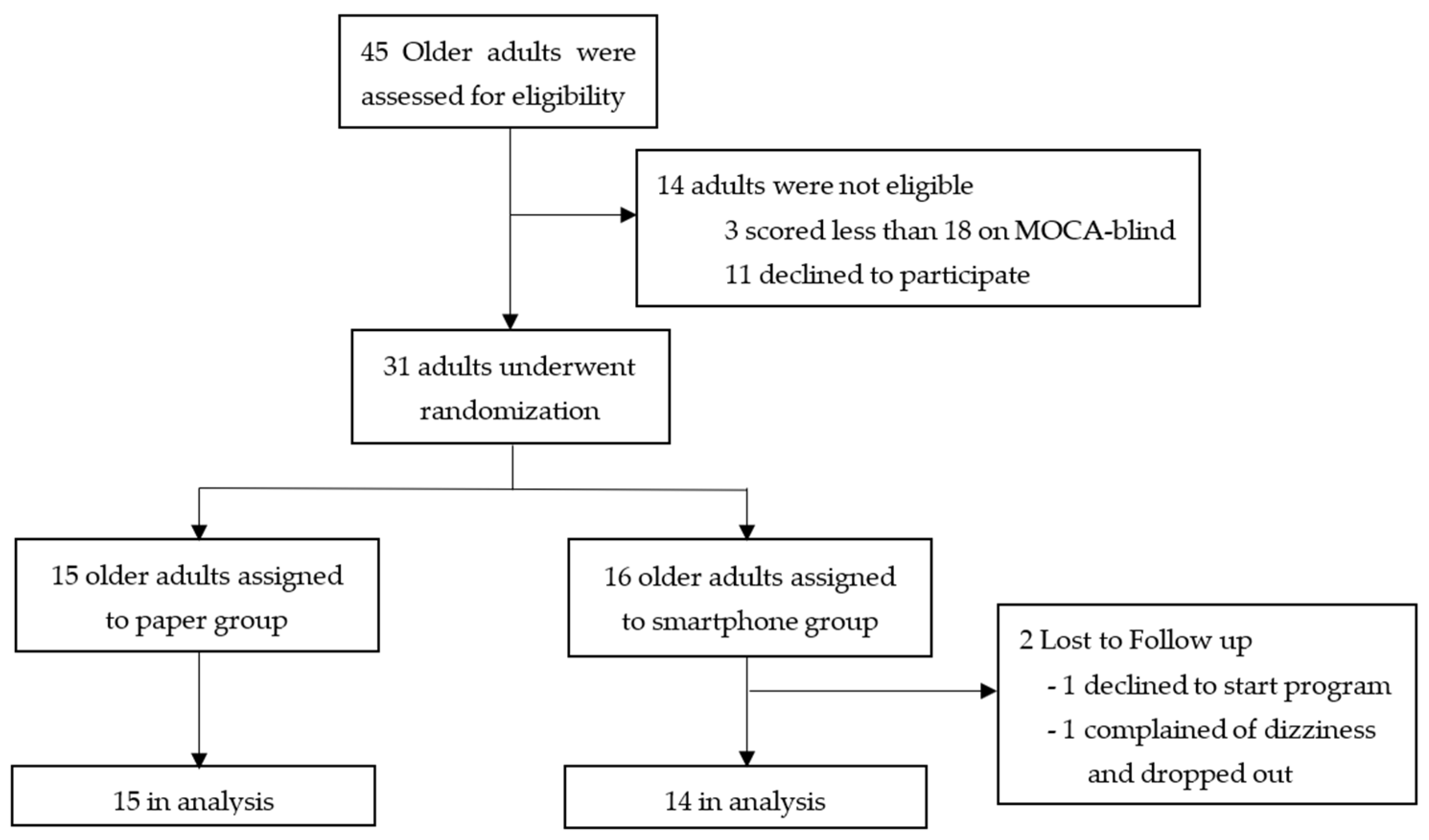
2.2. Procedures
2.3. Intervention
3. Statistical Analysis
4. Results
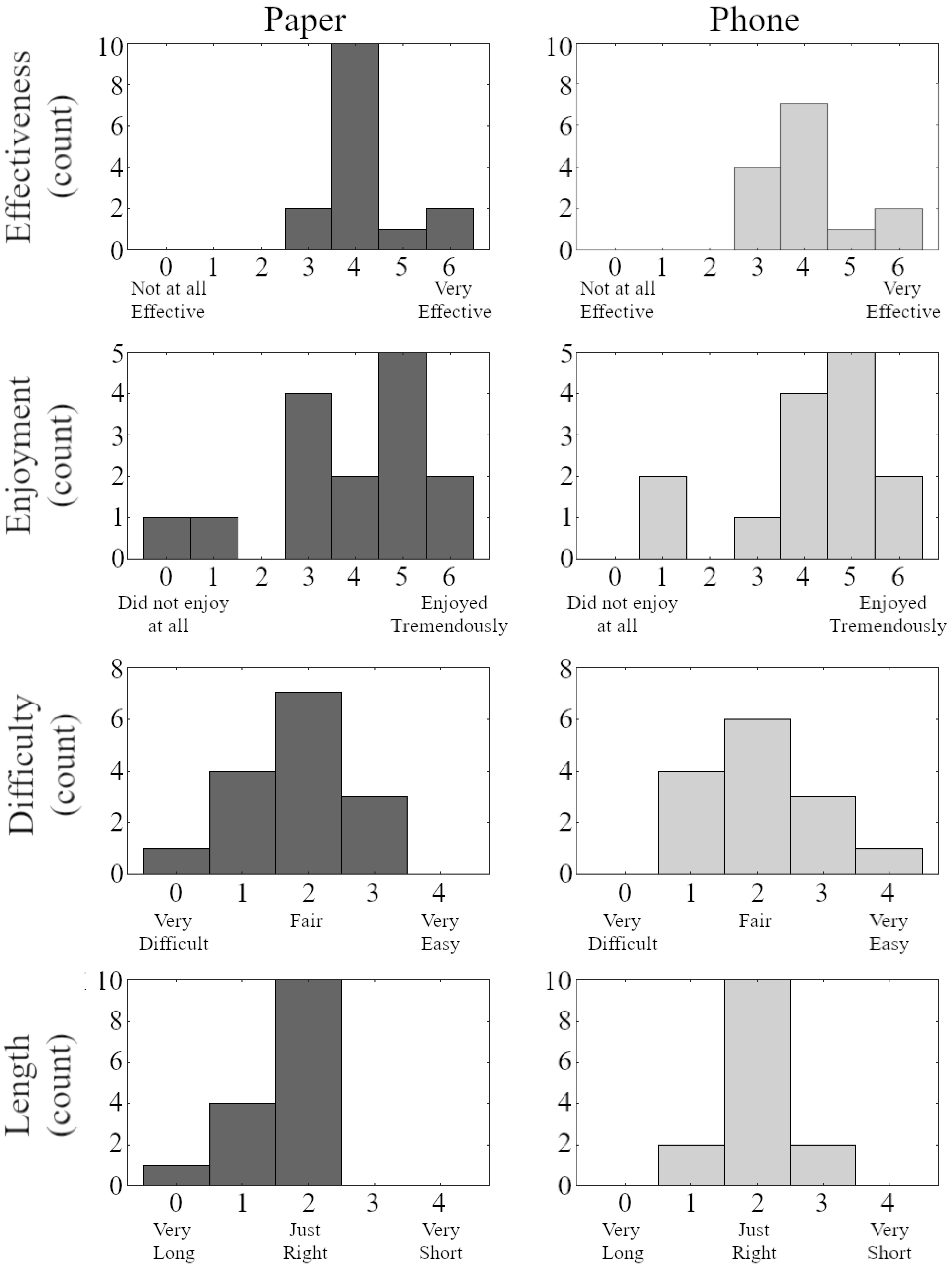
4.1. Exercise Response
4.2. Clinical Measures
4.3. Gait and Balance Measures
5. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Atella, V.; Piano Mortari, A.; Kopinska, J.; Belotti, F.; Lapi, F.; Cricelli, C.; Fontana, L. Trends in age-related disease burden and healthcare utilization. Aging Cell 2019, 18, e12861. [Google Scholar] [CrossRef]
- Gurwitz, J.H.; Pearson, S.D. Novel Therapies for an Aging Population: Grappling with Price, Value, and Affordability. JAMA 2019, 321, 1567–1568. [Google Scholar] [CrossRef] [PubMed]
- Campbell, A.J.; Borrie, M.J.; Spears, G.F.; Jackson, S.L.; Brown, J.S.; Fitzgerald, J.L. Circumstances and Consequences of Falls Experienced by a Community Population 70 Years and over during a Prospective Study. Age Ageing 1990, 19, 136–141. [Google Scholar] [CrossRef]
- Sattin, R.W.; Huber, D.A.L.; Devito, C.A.; Rodriguez, J.G.; Ros, A.; Bacchelli, S.; Stevens, J.A.; Waxweiler, R.J. The Incidence of Fall Injury Events among the Elderly in a Defined Population. Am. J. Epidemiol. 1990, 131, 1028–1037. [Google Scholar] [CrossRef] [PubMed]
- Administration for Community Living. 2021 Profile of Older Americans; Administration for Community Living: Washington, DC, USA, 2022. [Google Scholar]
- Silsupadol, P.; Lugade, V.; Shumway-Cook, A.; van Donkelaar, P.; Chou, L.-S.; Mayr, U.; Woollacott, M.H. Training-related changes in dual-task walking performance of elderly persons with balance impairment: A double-blind, randomized controlled trial. Gait Posture 2009, 29, 634–639. [Google Scholar] [CrossRef]
- Silsupadol, P.; Shumway-Cook, A.; Lugade, V.; van Donkelaar, P.; Chou, L.-S.; Mayr, U.; Woollacott, M.H. Effects of Single-Task Versus Dual-Task Training on Balance Performance in Older Adults: A Double-Blind, Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2009, 90, 381–387. [Google Scholar] [CrossRef] [PubMed]
- Campbell, A.J.; Robertson, M.C.; Gardner, M.M.; Norton, R.N.; Tilyard, M.W.; Buchner, D.M. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ 1997, 315, 1065–1069. [Google Scholar] [CrossRef]
- Seguin, R.; Nelson, M.E. The benefits of strength training for older adults. Am. J. Prev. Med. 2003, 25, 141–149. [Google Scholar] [CrossRef]
- Wadley, V.G.; Benz, R.L.; Ball, K.K.; Roenker, D.L.; Edwards, J.D.; Vance, D.E. Development and Evaluation of Home-Based Speed-of-Processing Training for Older Adults. Arch. Phys. Med. Rehabil. 2006, 87, 757–763. [Google Scholar] [CrossRef]
- Wongcharoen, S.; Sungkarat, S.; Munkhetvit, P.; Lugade, V.; Silsupadol, P. Home-based interventions improve trained, but not novel, dual-task balance performance in older adults: A randomized controlled trial. Gait Posture 2017, 52, 147–152. [Google Scholar] [CrossRef]
- Nasreddine, Z.S.; Phillips, N.A.; Bédirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A Brief Screening Tool for Mild Cognitive Impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Sheikh, J.I.; Yesavage, J.A. Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version. J. Aging Ment. Health 1986, 5, 165–173. [Google Scholar]
- Powell, L.E.; Myers, A.M. The Activities-specific Balance Confidence (ABC) Scale. J. Gerontol. Ser. A 1995, 50A, M28–M34. [Google Scholar] [CrossRef] [PubMed]
- Podsiadlo, D.; Richardson, S. The Timed “Up & Go”: A Test of Basic Functional Mobility for Frail Elderly Persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef]
- Vanicek, N.; King, S.A.; Gohil, R.; Chetter, I.C.; Coughlin, P.A. Computerized Dynamic Posturography for Postural Control Assessment in Patients with Intermittent Claudication. J. Vis. Exp. 2013, 82, e51077. [Google Scholar] [CrossRef]
- Prieto, T.; Myklebust, J.; Hoffmann, R.; Lovett, E.; Myklebust, B. Measures of postural steadiness: Differences between healthy young and elderly adults. IEEE Trans. Biomed. Eng. 1996, 43, 956–966. [Google Scholar] [CrossRef]
- Brown, L.A.; Shumway-Cook, A.; Woollacott, M.H. Attentional Demands and Postural Recovery: The Effects of Aging. J. Gerontol. Ser. A 1999, 54, M165–M171. [Google Scholar] [CrossRef]
- Woollacott, M.; Shumway-Cook, A. Attention and the control of posture and gait: A review of an emerging area of research. Gait Posture 2002, 16, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Lugade, V.; Lin, V.; Chou, L.-S. Center of mass and base of support interaction during gait. Gait Posture 2011, 33, 406–411. [Google Scholar] [CrossRef]
- Hof, A.L. The ‘extrapolated center of mass’ concept suggests a simple control of balance in walking. Hum. Mov. Sci. 2008, 27, 112–125. [Google Scholar] [CrossRef]
- Lugade, V.; Kaufman, K. Dynamic stability margin using a marker based system and Tekscan: A comparison of four gait conditions. Gait Posture 2013, 40, 252–254. [Google Scholar] [CrossRef] [PubMed]
- Curtze, C.; Buurke, T.J.; McCrum, C. Notes on the Margin of Stability; University of Groningen: Groningen, The Netherlands, 2023. [Google Scholar]
- Gentile, A. Movement Science: Foundations for Physical Therapy in Rehabilitation; Carr, J.S.R., Gordon, J., Eds.; Aspen Systems Inc.: Wheat Ridge, CO, USA, 1987; pp. 93–154. [Google Scholar]
- Geraedts, H.A.; Zijlstra, W.; Zhang, W.; Bulstra, S.; Stevens, M. Adherence to and effectiveness of an individually tailored home-based exercise program for frail older adults, driven by mobility monitoring: Design of a prospective cohort study. BMC Public Health 2014, 14, 570. [Google Scholar] [CrossRef]
- Geraedts, H.A.E.; Zijlstra, W.; Zhang, W.; Spoorenberg, S.L.W.; Báez, M.; Far, I.K.; Baldus, H.; Stevens, M. A Home-Based Exercise Program Driven by Tablet Application and Mobility Monitoring for Frail Older Adults: Feasibility and Practical Implications. Prev. Chronic Dis. 2017, 14, 160227. [Google Scholar] [CrossRef] [PubMed]
- Rivera-Torres, S.; Fahey, T.D.; Rivera, M.A. Adherence to Exercise Programs in Older Adults: Informative Report. Gerontol. Geriatr. Med. 2019, 5, 2333721418823604. [Google Scholar] [CrossRef]
- Anderson, M.; Perrin, A. Tech Adoption Climbs among Older Adults; Pew Research Center: Washington, DC, USA, 2017. [Google Scholar]
- Mitzner, T.L.; Savla, J.; Boot, W.R.; Sharit, J.; Charness, N.; Czaja, S.J.; Rogers, W.A. Technology Adoption by Older Adults: Findings from the PRISM Trial. Gerentologist 2018, 59, 34–44. [Google Scholar] [CrossRef]
- Wang, S.; Bolling, K.; Mao, W.; Reichstadt, J.; Jeste, D.; Kim, H.-C.; Nebeker, C. Technology to Support Aging in Place: Older Adults’ Perspectives. Healthcare 2019, 7, 60. [Google Scholar] [CrossRef] [PubMed]
- Lacroix, A.; Hortobágyi, T.; Beurskens, R.; Granacher, U. Effects of Supervised vs. Unsupervised Training Programs on Balance and Muscle Strength in Older Adults: A Systematic Review and Meta-Analysis. Sports Med. 2017, 47, 2341–2361. [Google Scholar] [CrossRef]
- Lesinski, M.; Hortobágyi, T.; Muehlbauer, T.; Gollhofer, A.; Granacher, U. Effects of Balance Training on Balance Performance in Healthy Older Adults: A Systematic Review and Meta-analysis. Sports Med. 2015, 45, 1721–1738. [Google Scholar] [CrossRef]
- Perera, S.; Mody, S.H.; Woodman, R.C.; Studenski, S.A. Meaningful Change and Responsiveness in Common Physical Performance Measures in Older Adults. J. Am. Geriatr. Soc. 2006, 54, 743–749. [Google Scholar] [CrossRef]
- Faulkner, K.A.; Redfern, M.S.; Cauley, J.A.; Landsittel, D.P.; Studenski, S.A.; Rosano, C.; Simonsick, E.M.; Harris, T.B.; Shorr, R.I.; Ayonayon, H.N.; et al. Multitasking: Association Between Poorer Performance and a History of Recurrent Falls. J. Am. Geriatr. Soc. 2007, 55, 570–576. [Google Scholar] [CrossRef]
- Seidler, R.D.; Martin, P.E. The effects of short term balance training on the postural control of older adults. Gait Posture 1997, 6, 224–236. [Google Scholar] [CrossRef]
- Hillel, I.; Gazit, E.; Nieuwboer, A.; Avanzino, L.; Rochester, L.; Cereatti, A.; Croce, U.D.; Rikkert, M.O.; Bloem, B.R.; Pelosin, E. Is every-day walking in older adults more analogous to dual-task walking or to usual walking? Elucidating the gaps between gait performance in the lab and during 24/7 monitoring. Eur. Rev. Aging Phys. Act. 2019, 16, 6. [Google Scholar] [CrossRef] [PubMed]


| Tasks | Week 1 | Week 2 | Week 3 | Week 4 |
|---|---|---|---|---|
| Stance Activities No manipulation | 1. Feet together stance 2. Knee marching 3. Stepping in different directions 4. Standing with forwards and backwards straight leg swings 5. Standing with sideways straight leg swings | 1. Semi-tandem stance 2. Draw number with left foot 3. Draw number with right foot | 1. Tightrope standing | |
| Hand manipulation | 6. Standing with feet together and reach as far and as safely as you can in different directions | 4. Semi-tandem stance with arm alternation 5. Knee marching with arm alternation 6. Standing knee lifts to each hand | 2. Tightrope standing with reaching as far and as safely as you can in different directions 3. Knee marching with clap hand under knee | 1. Tightrope standing with reaching as far and as safely as you can in different direction 2. Standing on toes with arms lift overhead 3. Knee lifts while standing with raise the opposite arm overhead |
| Transitional Activities | 7. Sit to stand and walk in a circle 8. Sit to stand and walk in a figure eight | 7. Sit to stand and cross-legged walk 8. Sit to stand and walk with high step | 4. Sit to stand and walking while knee marching in a figure eight | 4. Stand up and cross leg walk in a figure of eight |
| Gait Activities No manipulation | 9. Narrow walking 10. Walking with knee marching in a figure eight 11. Toe walking | 9. Narrow walking 10. Cross leg walking in a figure eight 11. Walk around obstacles–place two items on floor | 5 Narrow walking 6.Tightrope walking 7. Backward long-step walking 8. Backward tightrope walking 9. Sideways walking with step across in front of other leg 10. Sideways walking with step across and behind other leg | 5. Narrow walking 6. Sideways walking with step across in front of/behind other leg 7. Walk up and down stairs |
| Hand manipulation | 12. Toe walking with arm alternation | 12. Walk around obstacles with arm alternation | 11. Tightrope walking while carrying bag 12. High step walking with clap hand under knee | 8. Tightrope walking with arm alternation 9. Backward tightrope walking with arm alternation 10. Backward long-step walking with arm alternation 11. Backward toe walking with arm alternation 12. Backward high step walking with hand clap under knee |
| Smartphone Group (n = 14) | Paper Group (n = 15) | p-Value | |
|---|---|---|---|
| Female | 9 | 10 | |
| Reported a fall in past year | 6 | 9 | |
| Age (years) | 75.6 (8.9) | 78.2 (8.4) | 0.420 |
| Height (m) | 1.64 (0.06) | 1.61 (0.11) | 0.175 |
| Weight (kg) | 69.4 (14.9) | 68.5 (16.6) | 0.443 |
| Number of medications | 6.0 (3.4) | 5.1 (3.4) | 0.238 |
| Years of smartphone use | 7.1 (5.1) | 9.7 (5.6) | 0.106 |
| Education level (years) | 16.4 (2.3) | 16.5 (2.3) | 0.898 |
| Smartphone (n = 14) | Paper (n = 15) | |||||
|---|---|---|---|---|---|---|
| Visit 1 | Visit 2 | Visit 3 | Visit 1 | Visit 2 | Visit 3 | |
| ABC (%) | 88.3 (7.8) | 89.5 (7.4) | 89.0 (9.2) | 87.9 (10.8) | 84.0 (15.8) | 88.4 (10.7) |
| GDS (n/14) | 1.07 (1.38) | 1.00 (1.57) | 1.21 (1.72) | 1.20 (1.57) | 1.27 (1.91) | 0.80 (1.42) |
| TUG (sec) | 10.7 (2.0) | 10.6 (1.7) | 10.8 (2.0) | 12.7 (3.5) | 12.3 (3.8) | 12.2 (3.5) |
| Smartphone (n = 14) | Paper (n = 15) | |||||
|---|---|---|---|---|---|---|
| Visit 1 | Visit 2 | Visit 3 | Visit 1 | Visit 2 | Visit 3 | |
| Gait Velocity (m/s) †‡ | ||||||
| Single-Task | 1.02 (0.19) | 1.06 (0.20) | 1.05 (0.18) | 0.97 (0.22) | 0.95 (0.24) | 0.98 (0.23) |
| Dual-Task | 0.77 (0.18) | 0.77 (0.27) | 0.81 (0.25) | 0.72 (0.18) | 0.75 (0.20) | 0.81 (0.21) |
| Step Width (cm) * | ||||||
| Single-Task | 9.2 (4.6) a | 9.9 (3.8) | 9.4 (4.0) | 10.7 (2.0) | 10.1 (3.3) | 10.5 (3.6) |
| Dual-Task | 11.9 (3.5) a,b | 9.8 (3.9) b | 10.4 (3.5) | 11.1 (3.7) | 10.9 (4.1) | 12.3 (3.9) |
| XcoM-BOS at TO—Anteroposterior (cm) ‡ | ||||||
| Single-Task | 19.1 (5.9) | 19.7 (5.4) | 19.4 (5.1) | 16.4 (7.9) | 16.8 (8.6) | 17.8 (8.7) |
| Dual-Task | 10.2 (5.7) | 10.4 (7.6) | 11.6 (7.3) | 9.6 (6.9) | 10.1 (7.6) | 11.8 (7.3) |
| XcoM-BOS at TO—Mediolateral (cm) § ‡ | ||||||
| Single-Task | 19.1 (3.2) | 18.4 (3.0) | 18.3 (2.6) | 16.9 (5.0) | 17.2 (5.3) | 17.7 (5.4) |
| Dual-Task | 17.9 (2.7) | 17.3 (2.9) | 17.5 (2.7) | 16.4 (4.4) | 16.4 (4.9) | 17.3 (5.0) |
| Smartphone (n = 14) | Paper (n = 15) | |||||
|---|---|---|---|---|---|---|
| Visit 1 | Visit 2 | Visit 3 | Visit 1 | Visit 2 | Visit 3 | |
| Equilibrium Score (%) ‡ | ||||||
| EO | 92.7 (2.3) | 93.1 (2.3) | 92.0 (2.8) | 92.2 (2.3) | 91.4 (2.6) | 91.9 (2.8) |
| EC | 91.9 (3.1) | 91.2 (3.4) | 91.0 (3.8) | 90.9 (3.2) | 89.9 (4.1) | 88.7 (5.7) |
| VS | 89.6 (6.3) | 90.0 (4.4) | 91.5 (3.7) | 89.2 (6.8) | 88.6 (5.2) | 89.0 (5.0) |
| EO Sway | 71.5 (13.3) | 72.5 (11.8) | 75.0 (9.5) | 70.9 (15.4) | 73.1 (11.5) | 74.3 (10.1) |
| EC Sway | 60.5 (24.6) | 54.5 (22.2) | 68.3 (17.7) | 56.3 (20.6) | 58.6 (22.6) | 60.1 (21.8) |
| VS Sway | 53.1 (26.9) | 54.0 (18.0) | 62.4 (11.4) | 48.7 (19.8) | 54.9 (20.6) | 55.3 (21.7) |
| Total Excursion * | ||||||
| EO | 2.29 (0.52) | 2.29 (0.50) | 2.32 (0.48) | 2.30 (0.48) | 2.33 (0.50) | 2.38 (0.49) |
| EC | 2.32 (0.48) | 2.33 (0.47) | 2.34 (0.47) | 2.36 (0.47) | 2.35 (0.51) | 2.54 (0.72) |
| VS | 2.43 (0.44) | 2.37 (0.57) | 2.39 (0.45) | 2.48 (0.52) | 2.53 (0.56) | 2.59 (0.63) |
| EO Sway | 2.83 (0.52) | 2.92 (0.98) | 2.77 (0.64) | 2.83 (0.53) | 2.84 (0.52) | 2.98 (0.59) |
| EC Sway | 2.89 (0.47) | 2.96 (0.91) | 2.64 (0.50) | 3.12 (0.69) | 3.14 (0.96) | 3.24 (1.35) |
| VS Sway | 3.28 (0.90) b | 2.39 (0.71) a,b | 2.63 (1.17) | 3.10 (1.34) | 3.42 (1.38) a | 3.34 (1.48) |
| Sway Area (cm2) ‡ | ||||||
| EO | 6.77 (3.73) | 7.10 (2.39) | 7.04 (3.51) | 8.19 (5.25) | 7.41 (4.21) | 7.18 (5.82) |
| EC | 6.96 (2.57) | 7.99 (3.50) | 7.90 (3.42) | 8.32 (5.14) | 7.06 (3.72) | 7.42 (5.30) |
| VS | 7.08 (2.26) | 7.80 (3.38) | 7.79 (3.00) | 9.87 (7.54) | 8.22 (4.84) | 7.69 (5.14) |
| EO Sway | 9.56 (3.08) | 11.51 (7.40) | 9.64 (4.28) | 10.08 (5.24) | 10.65 (5.55) | 9.53 (4.28) |
| EC Sway | 12.20 (7.05) | 16.17 (13.73) | 12.02 (8.59) | 15.51 (11.17) | 14.52 (6.53) | 14.07 (6.94) |
| VS Sway | 16.11 (9.40) | 22.74 (29.04) | 16.72 (11.16) | 23.75 (13.23) | 19.34 (10.11) | 16.44 (9.81) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lugade, V.; Torbitt, M.; O’Brien, S.R.; Silsupadol, P. Smartphone- and Paper-Based Delivery of Balance Intervention for Older Adults Are Equally Effective, Enjoyable, and of High Fidelity: A Randomized Controlled Trial. Sensors 2023, 23, 7451. https://doi.org/10.3390/s23177451
Lugade V, Torbitt M, O’Brien SR, Silsupadol P. Smartphone- and Paper-Based Delivery of Balance Intervention for Older Adults Are Equally Effective, Enjoyable, and of High Fidelity: A Randomized Controlled Trial. Sensors. 2023; 23(17):7451. https://doi.org/10.3390/s23177451
Chicago/Turabian StyleLugade, Vipul, Molly Torbitt, Suzanne R. O’Brien, and Patima Silsupadol. 2023. "Smartphone- and Paper-Based Delivery of Balance Intervention for Older Adults Are Equally Effective, Enjoyable, and of High Fidelity: A Randomized Controlled Trial" Sensors 23, no. 17: 7451. https://doi.org/10.3390/s23177451





