An Examination of the Effects of Propolis and Quercetin in a Rat Model of Streptozotocin-Induced Diabetic Peripheral Neuropathy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Procedures and Animals
2.2. Experimental Design
2.3. Evaluation of Rat Sciatic Nerves: Histopathological Analysis and Transmission Electron Microscopy
2.4. TUNEL Assay
2.5. Immunohistochemical Staining
2.6. Biochemical Analysis
2.7. Statistical Analysis
3. Results
3.1. Changes in Body Weight and Blood Sugar Levels
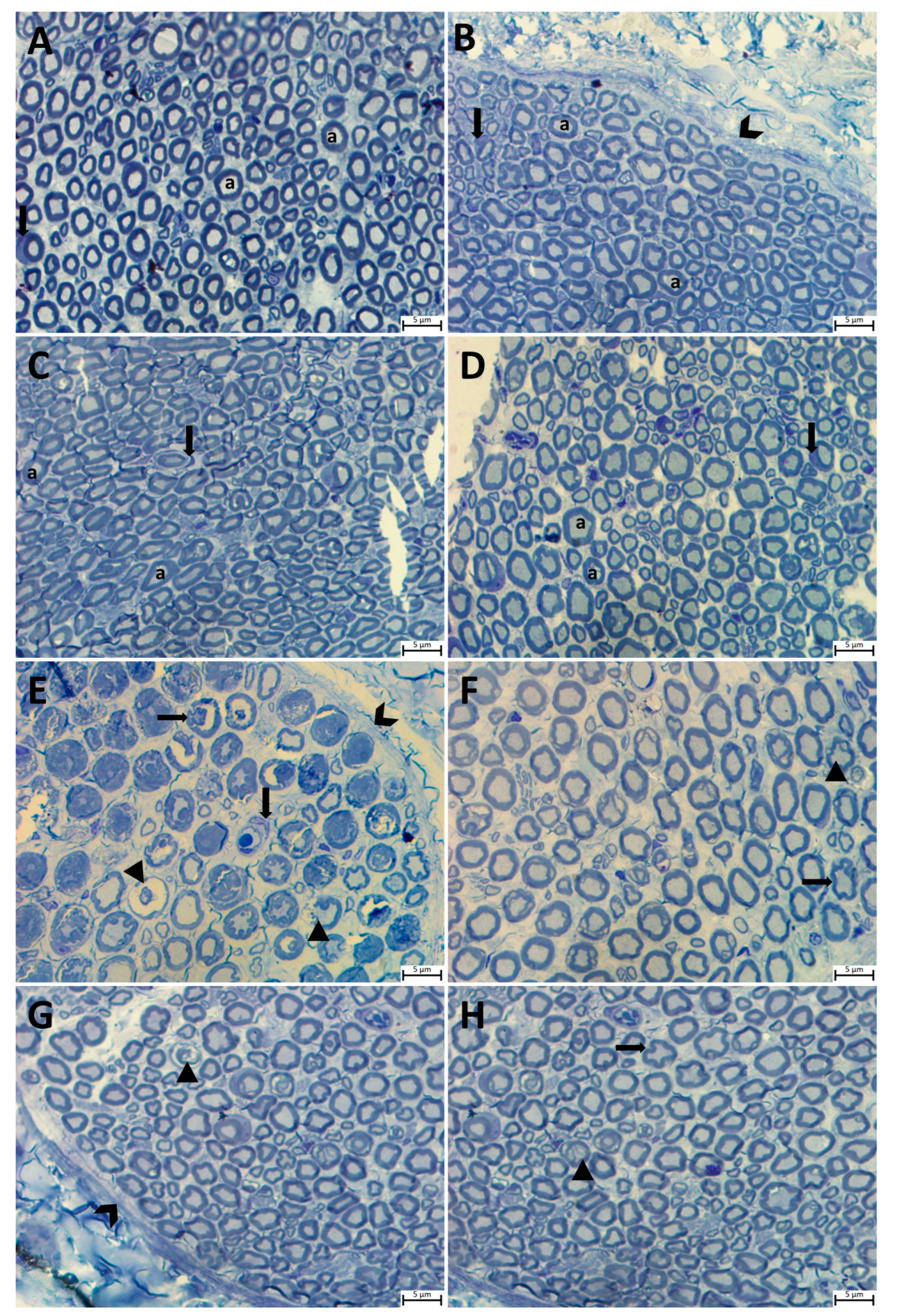
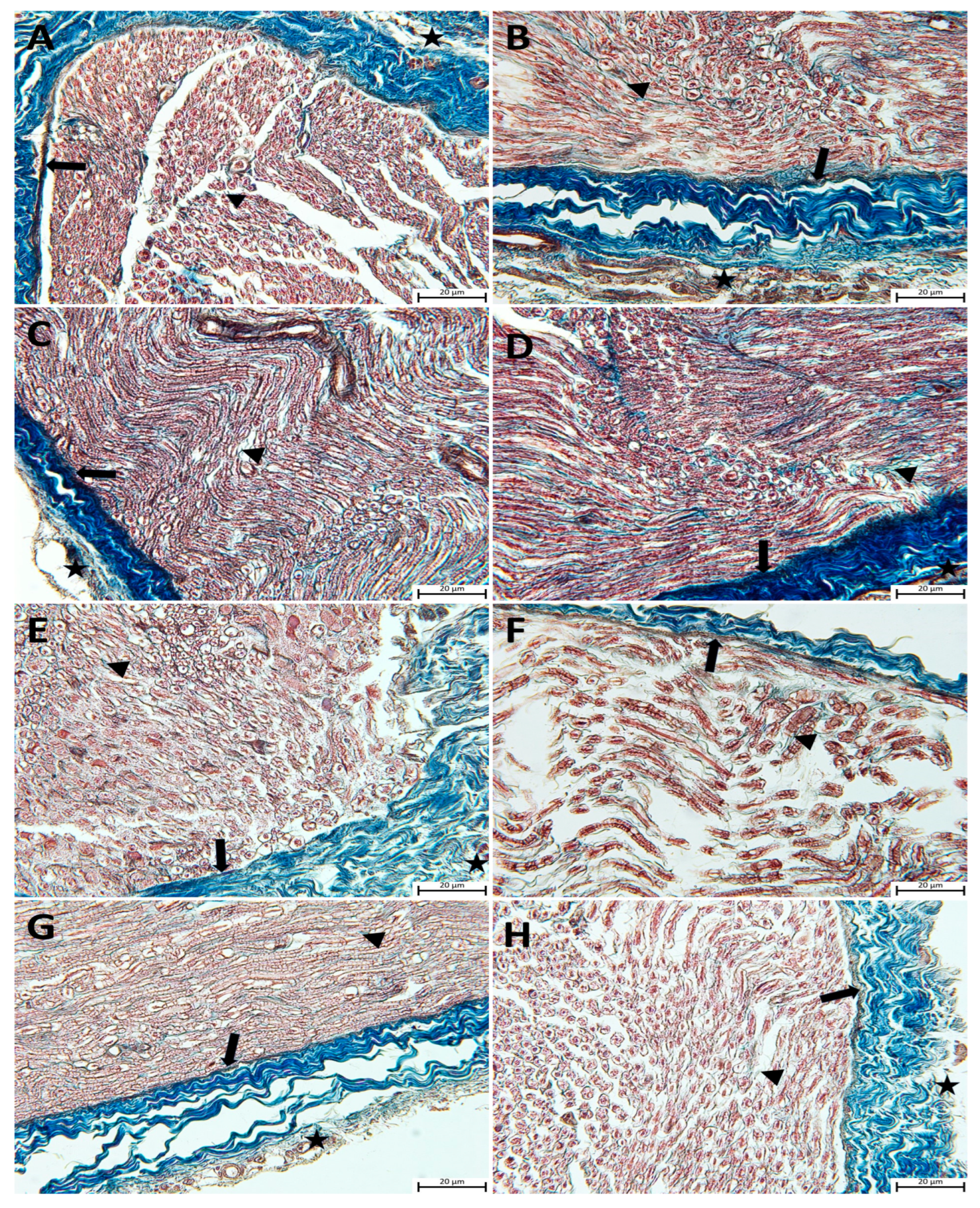
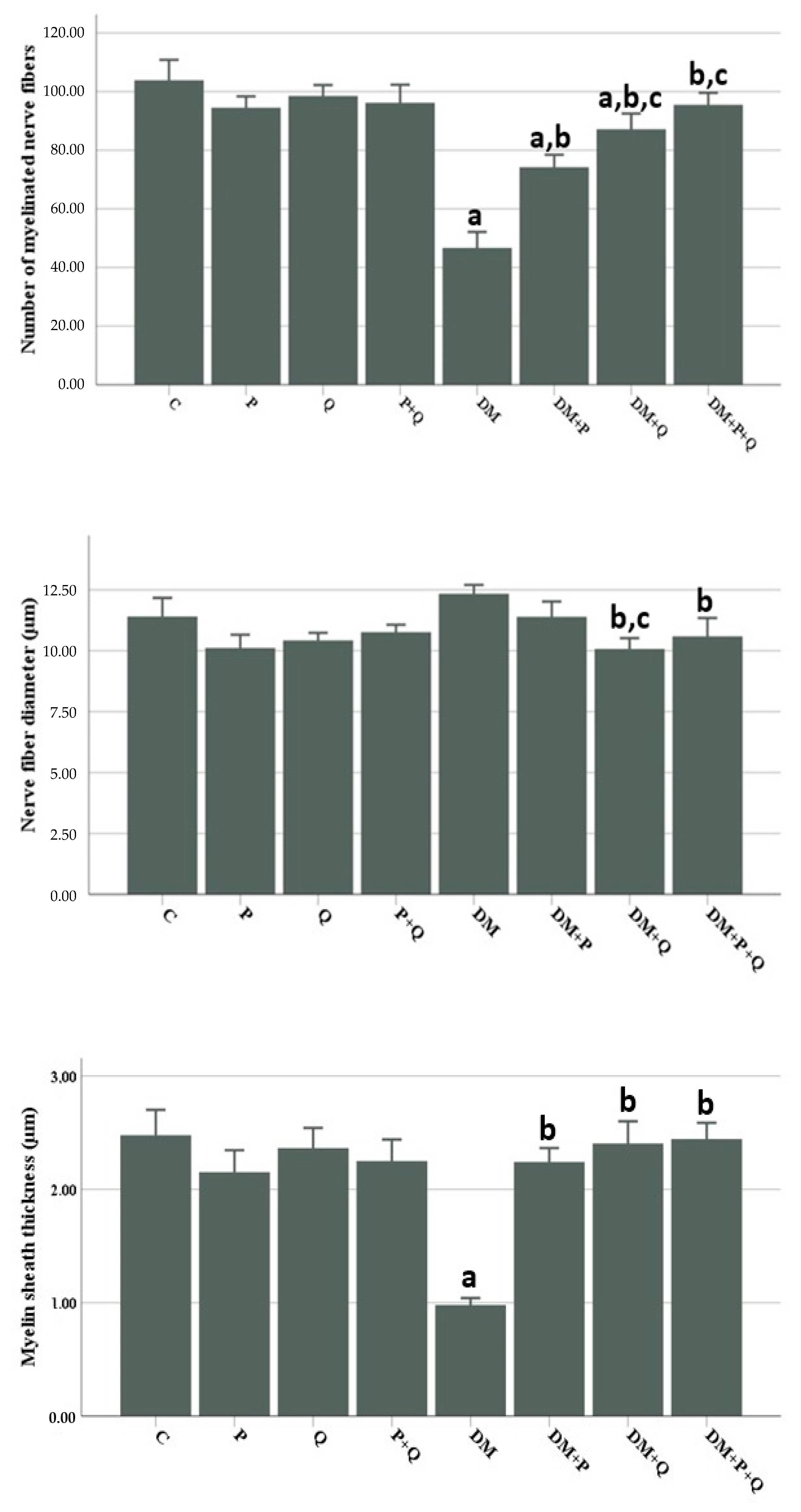
3.2. Histopathological and Morphometric Observations
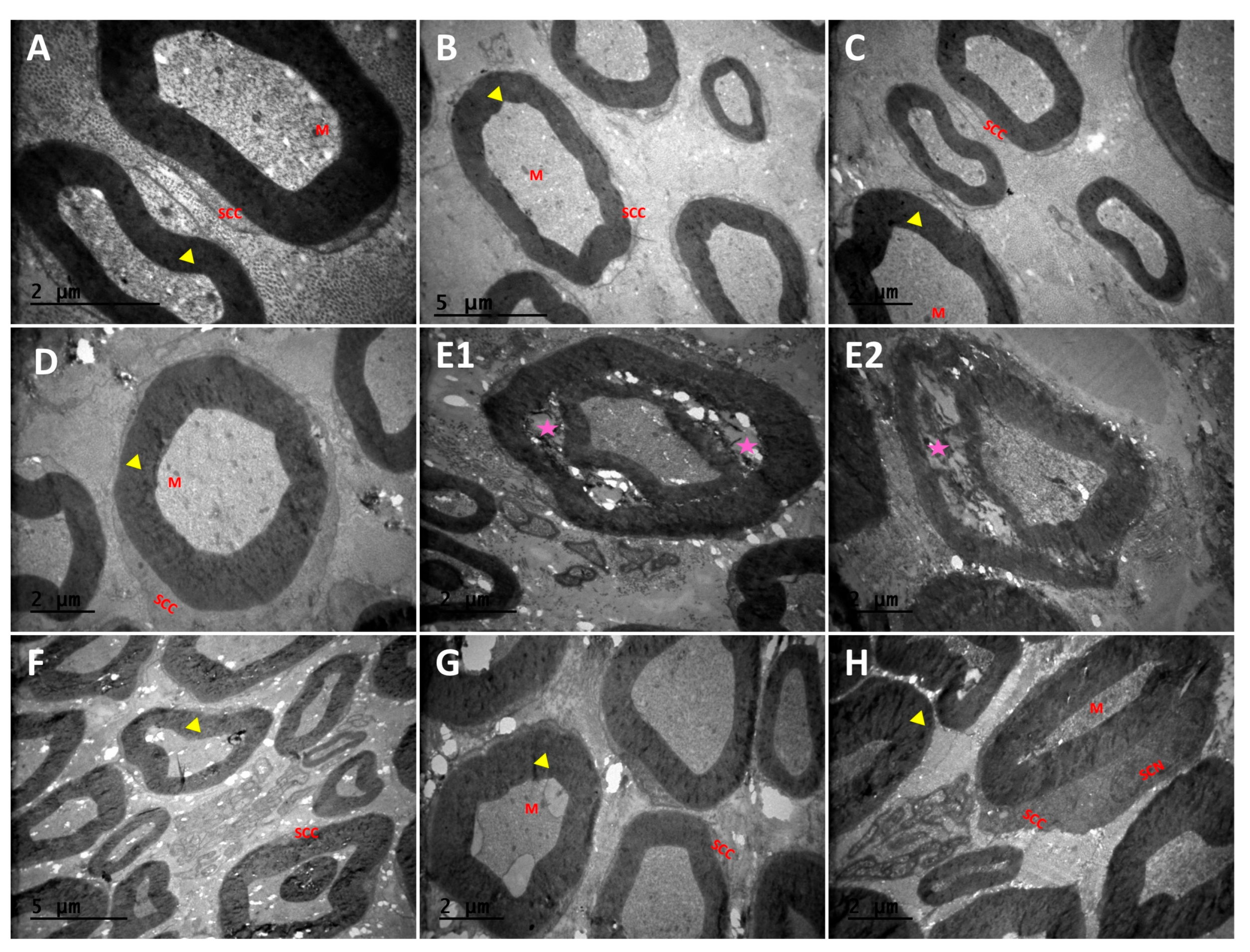
3.3. Transmission Electron Microscopy Observation Results for Sciatic Nerve Tissue
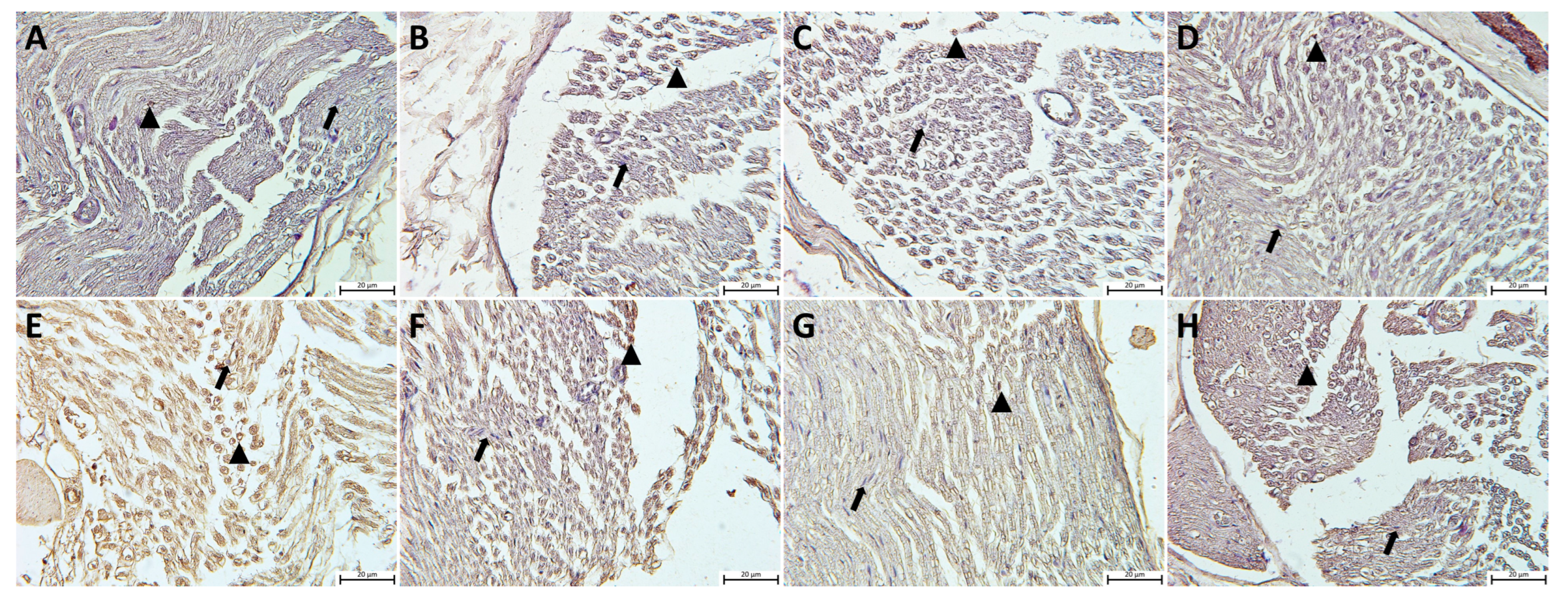
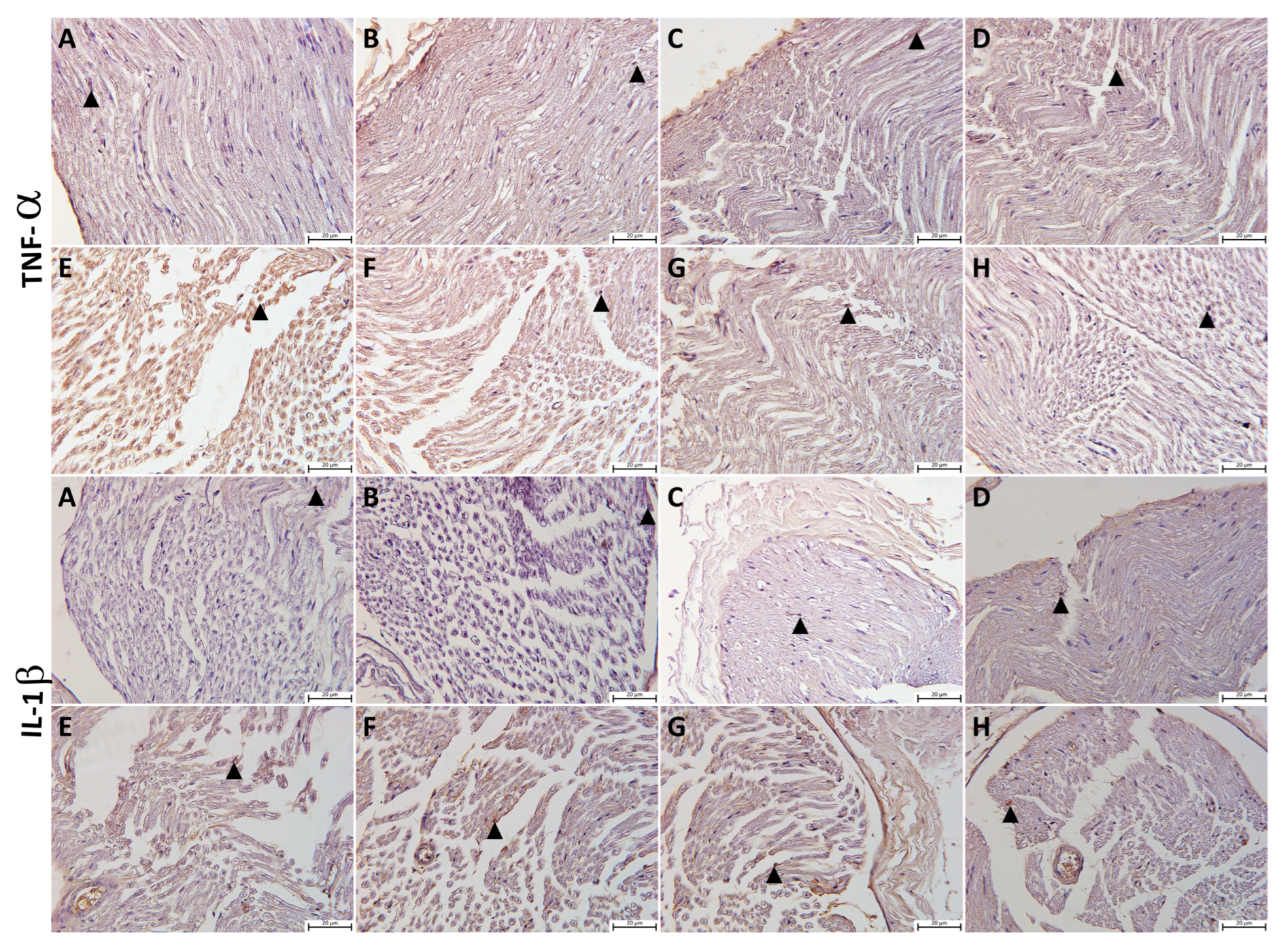
3.4. Evaluation of Immunohistochemistry and TUNEL Staining Results
3.5. Biochemical Parameter Findings
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Feldman, E.L.; Callaghan, B.C.; Pop-Busui, R.; Zochodne, D.W.; Wright, D.E.; Bennett, D.L.; Bril, V.; Russell, J.W.; Viswanathan, V. Diabetic neuropathy. Nat. Rev. Dis. Primers 2019, 5, 42. [Google Scholar] [CrossRef]
- Boyle, J.P.; Thompson, T.J.; Gregg, E.W.; Barker, L.E.; Williamson, D.F. Projection of the year 2050 burden of diabetes in the US adult population: Dynamic modeling of incidence, mortality, and prediabetes prevalence. Popul. Health Metr. 2010, 8, 29. [Google Scholar] [CrossRef]
- Selvarajah, D.; Kar, D.; Khunti, K.; Davies, M.J.; Scott, A.R.; Walker, J.; Tesfaye, S. Diabetic peripheral neuropathy: Advances in diagnosis and strategies for screening and early intervention. Lancet Diabetes Endocrinol. 2019, 7, 938–948. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Chopp, M.; Szalad, A.; Lu, X.; Zhang, Y.; Wang, X.; Cepparulo, P.; Lu, M.; Li, C.; Zhang, Z.G. Exosomes Derived From Schwann Cells Ameliorate Peripheral Neuropathy in Type 2 Diabetic Mice. Diabetes 2020, 69, 749–759. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Yang, X.; Sun, B.; Zhu, C. Perspectives of glycemic variability in diabetic neuropathy: A comprehensive review. Commun. Biol. 2021, 7, 1366. [Google Scholar] [CrossRef] [PubMed]
- Caturano, A.; D’Angelo, M.; Mormone, A.; Russo, V.; Mollica, M.P.; Salvatore, T.; Galiero, R.; Rinaldi, L.; Vetrano, E.; Marfella, R.; et al. Oxidative Stress in Type 2 Diabetes: Impacts from Pathogenesis to Lifestyle Modifications. Curr. Issues Mol. Biol. 2023, 45, 6651–6666. [Google Scholar] [CrossRef] [PubMed]
- Cho, E.; Kim, W. Effect of Acupuncture on Diabetic Neuropathy: A Narrative Review. Int. J. Mol. Sci. 2021, 9, 8575. [Google Scholar] [CrossRef] [PubMed]
- Sani, L.; Cardinault, N.; Astier, J.; Darmon, P.; Landrier, J.F. Poplar Propolis Improves Insulin Homeostasis in Non-Diabetic Insulin-Resistant Volunteers with Obesity: A Crossover Randomized Controlled Trial. Antioxidants 2023, 12, 1481. [Google Scholar] [CrossRef] [PubMed]
- Ates, O.; Cayli, S.R.; Yucel, N.; Altinoz, E.; Kocak, A.; Durak, M.A.; Turkoz, Y.; Yologlu, S. Central nervous system protection by resveratrol in streptozotocin-induced diabetic rats. J. Clin. Neurosci. 2007, 14, 256–260. [Google Scholar] [CrossRef] [PubMed]
- Chavda, V.P.; Chaudhari, A.Z.; Teli, D.; Balar, P.; Vora, L. Propolis and Their Active Constituents for Chronic Diseases. Biomedicines 2023, 11, 259. [Google Scholar] [CrossRef]
- Kanbur, M.; Erarslan, G.; Silici, S. Antioxidant effect of propolis against exposure to propetamphos in rats. Ecotoxicol. Environ. Saf. 2009, 72, 909–915. [Google Scholar] [CrossRef]
- Kuramoto, H.; Nakanishi, T.; Takegawa, D.; Mieda, K.; Hosaka, K. Caffeic Acid Phenethyl Ester Induces Vascular Endothelial Growth Factor Production and Inhibits CXCL10 Production in Human Dental Pulp Cells. Curr. Issues Mol. Biol. 2022, 44, 5691–5699. [Google Scholar] [CrossRef]
- Geng, F.; Zhao, L.; Cai, Y.; Zhao, Y.; Jin, F.; Li, Y.; Li, T.; Yang, X.; Li, S.; Gao, X.; et al. Quercetin Alleviates Pulmonary Fibrosis in Silicotic Mice by Inhibiting Macrophage Transition and TGF-β-Smad2/3 Pathway. Curr. Issues Mol. Biol. 2023, 45, 3087–3101. [Google Scholar] [CrossRef]
- Harwood, M.; Danielewska-Nikiel, B.; Borzelleca, J.F.; Flamm, G.W.; Williams, G.M.; Lines, T.C. A critical review of the data related to the safety of quercetin and lack of evidence of in vivo toxicity, including lack of genotoxic/carcinogenic properties. Food Chem. Toxicol. 2007, 45, 2179–2205. [Google Scholar] [CrossRef]
- Askari, V.R.; Rahimi, V.B.; Zamani, P.; Fereydouni, N.; Rahmanian-Devin, P.; Sahebkar, A.H.; Rakhshandeh, H. Evaluation of the effects of Iranian propolis on the severity of post operational-induced peritoneal adhesion in rats. Biomed. Pharmacother. 2018, 99, 346–353. [Google Scholar] [CrossRef]
- Wu, L.; Wang, C.; Li, J.; Li, S.; Feng, J.; Liu, T.; Xu, S.; Wang, W.; Lu, X.; Chen, K.; et al. Hepatoprotective effect of quercetin via TRAF6/JNK pathway in acute hepatitis. Biomed. Pharmacother. 2017, 96, 1137–1146. [Google Scholar] [CrossRef]
- Yuluğ, E.; Türedi, S.; Yıldırım, Ö.; Yenilmez, E.; Aliyazıcıoğlu, Y.; Demir, S.; Özer-Yaman, S.; Menteşe, A. Biochemical and morphological evaluation of the effects of propolis on cisplatin induced kidney damage in rats. Biotech. Histochem. 2019, 94, 204–213. [Google Scholar] [CrossRef]
- Türedi, S.; Yuluğ, E.; Alver, A.; Bodur, A.; İnce, İ. A morphological and biochemical evaluation of the effects of quercetin on experimental sciatic nerve damage in rats. Exp. Ther. Med. 2018, 15, 3215–3224. [Google Scholar]
- Kiss, P.; Banki, E.; Gaszner, B.; Nagy, D.; Helyes, Z.; Pal, E.; Reman, G.; Toth, G.; Tamas, A.; Reglodi, D. Protective Effects of PACAP in a Rat Model of Diabetic Neuropathy. Int. J. Mol. Sci. 2021, 2, 10691. [Google Scholar] [CrossRef]
- Abueid, L.; Uslu, Ü.; Cumbul, A.; Öğünç, A.V.; Ercan, F.; Alican, İ. Inhibition of 5 lipoxygenase by zileuton in a rat model of myocardial infarction. Anatol. J. Cardiol. 2017, 17, 269–275. [Google Scholar] [CrossRef]
- Erel, O. A novel automated method to measure total antioxidant response against potent free radical reactions. Clin. Biochem. 2004, 37, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Erel, O. A new automated colorimetric method for measuring total oxidant status. Clin. Biochem. 2005, 38, 1103–1111. [Google Scholar] [CrossRef] [PubMed]
- Selek, S.; Aslan, M.; Horoz, M.; Gur, M.; Erel, O. Oxidative status and serum PON1 activity in beta-thalassemia minor. Clin. Biochem. 2007, 40, 287–291. [Google Scholar] [CrossRef] [PubMed]
- Ohkawa, H.; Ohishi, N.; Yagi, K. Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal. Biochem. 1979, 95, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Stavniichuk, R.; Obrosov, A.A.; Drel, V.R.; Nadler, J.L.; Obrosova, I.G.; Yorek, M.A. 12/15-Lipoxygenase inhibition counteracts MAPK phosphorylation in mouse and cell culture models of diabetic peripheral neuropathy. J. Diabetes Mellit. 2013, 3. [Google Scholar] [CrossRef] [PubMed]
- Sima, A.A.; Sugimoto, K. Experimental diabetic neuropathy: An update. Diabetologia 1999, 42, 773–788. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; Wang, F.; Shal, B.; Khan, A.U.; Zahra, S.S.; Haq, I.U.; Khan, S.; Rengasamy, K.R. Anti-neuropathic pain activity of Ajugarin-I via activation of Nrf2 signaling and inhibition of TRPV1/TRPM8 nociceptors in STZ-induced diabetic neuropathy. Pharmacol. Res. 2022, 183, 106392. [Google Scholar] [CrossRef] [PubMed]
- Addepalli, V.; Suryavanshi, S.V. Catechin attenuates diabetic autonomic neuropathy in streptozotocin induced diabetic rats. Biomed. Pharmacother. 2018, 108, 1517–1523. [Google Scholar] [CrossRef]
- Resham, K.; Khare, P.; Bishnoi, M.; Sharma, S.S. Neuroprotective effects of isoquercitrin in diabetic neuropathy via Wnt/β-catenin signaling pathway inhibition. Biofactors 2020, 46, 411–420. [Google Scholar] [CrossRef]
- Nna, V.U.; Abu Bakar, A.B.; Zakaria, Z.; Othman, Z.A.; Jalil, N.A.C.; Mohamed, M. Malaysian Propolis and Metformin Synergistically Mitigate Kidney Oxidative Stress and Inflammation in Streptozotocin-Induced Diabetic Rats. Molecules 2021, 26, 3441. [Google Scholar] [CrossRef]
- Anjaneyulu, M.; Chopra, K. Quercetin, a bioflavonoid, attenuates thermal hyperalgesia in a mouse model of diabetic neuropathic pain. Prog. Neuropsychopharmacol. Biol. Psychiatry 2003, 27, 1001–1005. [Google Scholar] [CrossRef]
- Hicks, C.W.; Selvin, E. Epidemiology of Peripheral Neuropathy and Lower Extremity Disease in Diabetes. Curr. Diabetes Rep. 2019, 27, 86. [Google Scholar] [CrossRef] [PubMed]
- Sameni, H.R.; Ramhormozi, P.; Bandegi, A.R.; Taherian, A.A.; Mirmohammadkhani, M.; Safari, M. Effects of ethanol extract of propolis on histopathological changes and anti-oxidant defense of kidney in a rat model for type 1 diabetes mellitus. J. Diabetes Investig. 2016, 7, 506–513. [Google Scholar] [CrossRef] [PubMed]
- Ibáñez, B.; Melero, A.; Montoro, A.; San Onofre, N.; Soriano, J.M. Radioprotective Effects from Propolis: A Review. Molecules 2023, 28, 5842. [Google Scholar] [CrossRef] [PubMed]
- Zu, G.; Sun, K.; Li, L.; Zu, X.; Han, T.; Huang, H. Mechanism of quercetin therapeutic targets for Alzheimer disease and type 2 diabetes mellitus. Sci. Rep. 2021, 25, 22959. [Google Scholar] [CrossRef] [PubMed]
- Tang, L.; Li, K.; Zhang, Y.; Li, H.; Li, A.; Xu, Y.; Wei, B. Quercetin liposomes ameliorate streptozotocin-induced diabetic nephropathy in diabetic rats. Sci. Rep. 2020, 12, 2440. [Google Scholar] [CrossRef] [PubMed]
- Ojo, O.O.; Olorunsogo, O.O. Quercetin and vitamin E attenuate diabetes-induced testicular anomaly in Wistar rats via the mitochondrial-mediated apoptotic pathway. Andrologia 2021, 53, e14185. [Google Scholar] [CrossRef]
- Elbe, H.; Vardi, N.; Esrefoglu, M.; Ates, B.; Yologlu, S.; Taskapan, C. Amelioration of streptozotocin-induced diabetic nephropathy by melatonin, quercetin, and resveratrol in rats. Hum. Exp. Toxicol. 2015, 34, 100–113. [Google Scholar] [CrossRef]
- Wang, X.; Huan, Y.; Li, C.; Cao, H.; Sun, S.; Lei, L.; Liu, Q.; Liu, S.; Ji, W.; Liu, H.; et al. Diphenyl diselenide alleviates diabetic peripheral neuropathy in rats with streptozotocin-induced diabetes by modulating oxidative stress. Biochem. Pharmacol. 2020, 182, 114221. [Google Scholar] [CrossRef]
- Mert, T.; Sahin, E.; Yaman, S.; Sahin, M. Pulsed magnetic field treatment ameliorates the progression of peripheral neuropathy by modulating the neuronal oxidative stress, apoptosis and angiogenesis in a rat model of experimental diabetes. Arch. Physiol. Biochem. 2022, 128, 1658–1665. [Google Scholar] [CrossRef]
- Sayın, R.; Aslan, M.; Kucukoglu, M.E.; Luleci, A.; Atmaca, M.; Esen, R.; Demir, H. Serum prolidase enzyme activity and oxidative stress levels in patients with diabetic neuropathy. Endocrine 2014, 47, 146151. [Google Scholar] [CrossRef]
- Rivera-Yañez, N.; Rivera-Yañez, C.R.; Pozo-Molina, G.; Méndez-Catalá, C.F.; Méndez-Cruz, A.R.; Nieto-Yañez, O. Biomedical Properties of Propolis on Diverse Chronic Diseases and Its Potential Applications and Health Benefits. Nutrients 2020, 13, 78. [Google Scholar] [CrossRef]
- Cantarelli, M.A.; Camina, J.M.; Pettenati, E.M.; Marchevsky, E.J.; Pellerano, R.G. Trace mineral content of Argentinean raw propolis by neutron activation analysis (NAA): Assessment of geographical provenance by chemometrics. LWT-Food Sci. Technol. 2011, 44, 256–260. [Google Scholar] [CrossRef]
- Scheller, S.; Wilczok, T.; Imielski, S.; Krol, W.; Gabrys, J.; Shani, J. Free radical scavenging by ethanol extract of propolis. Int. J. Radiat. Biol. 1990, 57, 461–465. [Google Scholar] [CrossRef]
- Chiu, H.F.; Han, Y.C.; Shen, Y.C.; Golovinskaia, O.; Venkatakrishnan, K.; Wang, C.K. Chemopreventive and Chemotherapeutic Effect of Propolis and Its Constituents: A Mini-review. J. Cancer Prev. 2020, 25, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Sallam, A.A.; Ahmed, M.M.; El-Magd, M.A.; Magdy, A.; Ghamry, H.I.; Alshahrani, M.Y.; Abou El-Fotoh, M.F. Quercetin-Ameliorated, Multi-Walled Carbon Nanotubes-Induced Immunotoxic, Inflammatory, and Oxidative Effects in Mice. Molecules 2022, 27, 2117. [Google Scholar] [CrossRef]
- Dhanya, R. Quercetin for managing type 2 diabetes and its complications, an insight into multitarget therapy. Biomed. Pharmacother. 2022, 146, 112560. [Google Scholar] [CrossRef]
- Yan, L.; Vaghari-Tabari, M.; Malakoti, F.; Moein, S.; Qujeq, D.; Yousefi, B.; Asemi, Z. Quercetin: An effective polyphenol in alleviating diabetes and diabetic complications. Crit. Rev. Food Sci. Nutr. 2022, 25, 9163–9186. [Google Scholar] [CrossRef] [PubMed]
- Höke, A. Animal models of peripheral neuropathies. Neurotherapeutics 2012, 9, 262–269. [Google Scholar] [CrossRef]
- Zulhendri, F.; Perera, C.O.; Tandean, S. Can Propolis Be a Useful Adjuvant in Brain and Neurological Disorders and Injuries? A Systematic Scoping Review of the Latest Experimental Evidence. Biomedicines 2021, 9, 1227. [Google Scholar] [CrossRef] [PubMed]
- Nosratiyan, M.; Farjah, G.H.; Karimipour, M.; Pourheidar, B. The Effect of Propolis-Gum Arabic as a Novel Nerve Guidance Channel on Regeneration of Sciatic Nerve in Male Rats. Turk. Neurosurg. 2021, 31, 361–367. [Google Scholar] [CrossRef]
- Shao, Q.; Zhao, M.; Pei, W.; Pu, Y.; Liu, M.; Liu, W.; Yu, Z.; Chen, K.; Liu, H.; Deng, B. Pinocembrin Promotes OPC Differentiation and Remyelination via the mTOR Signaling Pathway. Neurosci. Bull. 2021, 37, 1314–1324. [Google Scholar] [CrossRef] [PubMed]
- Bai, L.; Li, X.; He, L.; Zheng, Y.; Lu, H.; Li, J.; Zhong, L.; Tong, R.; Jiang, Z.; Shi, J.; et al. Antidiabetic Potential of Flavonoids from Traditional Chinese Medicine: A Review. Am. J. Chin. Med. 2019, 47, 933–957. [Google Scholar] [CrossRef]
- Chis, I.C.; Clichici, A.; Nagy, A.L.; Oros, A.; Catoi, C.; Clichici, S. Quercetin in association with moderate exercise training attenuates injuries induced by experimental diabetes in sciatic nerves. J. Physiol. Pharmacol. 2017, 68, 877–886. [Google Scholar]
- Xie, J.; Song, W.; Liang, X.; Zhang, Q.; Shi, Y.; Liu, W.; Shi, X. Protective effect of quercetin on streptozotocin-induced diabetic peripheral neuropathy rats through modulating gut microbiota and reactive oxygen species level. Biomed. Pharmacother. 2020, 127, 110147. [Google Scholar] [CrossRef]
- Feng, Y.; Chen, L.; Luo, Q.; Wu, M.; Chen, Y.; Shi, X. Involvement of microRNA-146a in diabetic peripheral neuropathy through the regulation of inflammation. Drug Des. Dev. Ther. 2018, 12, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.X.; Lin, Z.Q.; Sun, A.L.; Shi, Y.Y.; Hong, Q.X.; Zhao, G.F. Curcumin Ameliorates the Experimental Diabetic Peripheral Neuropathy through Promotion of NGF Expression in Rats. Chem. Biodivers. 2022, 19, e202200029. [Google Scholar] [CrossRef] [PubMed]
- Balaha, M.; De Filippis, B.; Cataldi, A.; di Giacomo, V. CAPE and Neuroprotection: A Review. Biomolecules 2021, 11, 176. [Google Scholar] [CrossRef] [PubMed]

| Group | Blood Glucose Level (mg/dL) | Body Weight (g) | ||||
|---|---|---|---|---|---|---|
| Initial | First Week | Second Week | Third Week | Forth Week | ||
| Control | 89.33 ± 9.00 | 92 ± 9.20 | 94.83 ± 8.20 | 88.16 ± 3.37 | 87.83 ± 9.38 | 372.66 ± 22.28 |
| P | 84.66 ± 5.31 | 106.33 ± 12.27 | 99.33 ± 7.33 | 95.83 ± 8.10 | 90.33 ± 8.26 | 384.33 ± 32.61 |
| Q | 93.83 ± 11.25 | 102.83 ± 14.77 | 100.33 ± 8.14 | 93.16 ± 7.65 | 92.16 ± 6.24 | 389.83 ± 31.57 |
| P + Q | 97.33 ± 11.27 | 95.66 ± 18.81 | 94.33 ± 6.12 | 101.66 ± 7.86 | 98.16 ± 5.49 | 359.83 ± 41.74 |
| DM | 421.66 ± 78.17 a | 501.83 ± 137.38 a | 424.33 ± 48.19 a | 415.16 ± 55.14 a | 409.66 ± 16.13 a | 235.33 ± 41.73 a |
| DM + P | 439.5 ± 49.24 a | 421.66 ± 52.24 a | 390.16 ± 35.04 a | 357.66 ± 31.70 a.b | 297.33 ± 24.84 a.b | 301.33 ± 46.96 a |
| DM + Q | 448.16 ± 82.49 a | 401.66 ± 7.94 a | 369.83 ± 17.98 a | 350 ± 28.40 a.b | 271 ± 33.39 a.b | 334.5 ± 27.32 b |
| DM + P+ Q | 431.5 ± 89.12 a | 367.66 ± 50.14 a.b | 388.5 ± 34.09 a | 353 ± 46.67 a.b | 255.66 ± 27.69 a.b.c | 357.33 ± 36.60 b |
| Group | MDA (µmol/mL) | TOS (μmol H2O2 Eqv./L) | TAS (μmol Trolox Eqv./L) | OSI (AU) | TNF-α (pg/mL) | IL-6 (pg/mL) |
|---|---|---|---|---|---|---|
| Control | 3.56 ± 0.49 | 19.57 ± 5.90 | 1.15 ± 0.12 | 1.717 ± 0.55 | 6.55 ± 1.46 | 5.19 ± 2.92 |
| P | 2.22 ± 0.59 | 19.03 ± 11.01 | 1.18 ± 0.15 | 1.65 ± 1.00 | 4.93 ± 1.70 | 28.93 ± 3.21 |
| Q | 4.87 ± 1.43 | 17.63 ± 11.04 | 1.31 ± 0.18 | 1.35 ± 0.80 | 5.61 ± 1.42 | 31.06 ± 2.54 |
| P + Q | 3.43 ± 0.95 | 20.08 ± 9.82 | 1.36 ± 0.61 | 1.61 ± 0.84 | 4.83 ± 2.32 | 29.65 ± 3.81 |
| DM | 6.74 ± 1.89 a | 24.66 ± 7.71 | 0.82 ± 0.22 | 3.31 ± 1.84 | 5.55 ± 3.01 | 28.82 ± 11.63 a |
| DM + P | 8.57 ± 1.60 | 18.27 ± 6.81 | 0.98 ± 0.30 | 1.98 ± 0.98 | 4.48 ± 1.5 | 40.84 ± 6.43 |
| DM + Q | 7.62 ± 1.51 | 18.80 ± 1.27 | 1.21 ± 0.12 b | 1.56 ± 0.12 b | 5.74 ± 0.84 | 34.96 ± 3.86 |
| DM + P + Q | 6.78 ± 0.89 | 18.44 ± 6.79 | 0.75 ± 0.21 | 2.66 ± 1.33 | 4.23 ± 1.73 | 31.90 ± 3.86 b |
| Group | MDA Tissue (nmol/mg) | TOS Tissue (μmol H2O2 Eqv./mg Protein) | TAS Tissue (μmol Trolox Eqv./mg Protein) | OSI Tissue (AU) | SOD Units/mg Protein | CAT Units/mg Protein | GSH µg/mg Protein |
|---|---|---|---|---|---|---|---|
| Control | 3.87 ± 1.50 | 72.94 ± 20.31 | 5.40 ± 2.08 | 1.83 ± 1.70 | 3.15 ± 2.29 | 37.92 ± 19.93 | 265.87 ± 115.29 |
| P | 2.04 ± 1.40 | 70.84 ± 9.55 | 5.73 ± 1.21 | 1.25 ± 0.17 | 3.27 ± 1.78 | 30.29 ± 17.29 | 171.89 ± 62.27 |
| Q | 3.36 ± 1.68 | 66.56 ± 15.24 | 5.59 ± 1.24 | 1.22 ± 0.34 | 3.00 ± 0.42 | 19.31 ± 4.94 | 189.55 ± 125.62 |
| P + Q | 3.26 ± 0.63 | 60.24 ± 9.78 | 4.44 ± 2.84 | 1.93 ± 1.15 | 3.44 ± 0.83 | 27.65 ± 13.99 | 194.58 ± 94.25 |
| DM | 7.02 ± 1.92 a | 83.74 ± 13.37 | 2.87 ± 0.72 | 3.13 ± 1.16 | 5.04 ± 0.19 | 17.94 ± 6.05 | 230. 86 ± 86.95 |
| DM + P | 4.00 ± 0.99 b | 60.80 ± 30.44 | 3.07 ± 1.37 | 2.60 ± 2.11 | 3.64 ± 0.34 b | 28.10 ± 15.96 | 266.82 ± 177.88 |
| DM + Q | 3.09 ± 1.54 b | 71.57 ± 8.62 | 3.56 ± 3.5 | 3.12 ± 1.60 | 6.90 ± 1.69 | 38.88 ± 26.11 b | 227.22 ± 198.57 |
| DM + P + Q | 4.13 ± 1.62 b | 49.55 ± 15.15 b | 3. 03 ± 1.17 | 1.82 ± 0.77 | 3.40 ± 1.17 b | 19.01 ± 17.02 | 325.81 ± 139.63 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Türedi, S.; Çelik, H.; Dağlı, Ş.N.; Taşkın, S.; Şeker, U.; Deniz, M. An Examination of the Effects of Propolis and Quercetin in a Rat Model of Streptozotocin-Induced Diabetic Peripheral Neuropathy. Curr. Issues Mol. Biol. 2024, 46, 1955-1974. https://doi.org/10.3390/cimb46030128
Türedi S, Çelik H, Dağlı ŞN, Taşkın S, Şeker U, Deniz M. An Examination of the Effects of Propolis and Quercetin in a Rat Model of Streptozotocin-Induced Diabetic Peripheral Neuropathy. Current Issues in Molecular Biology. 2024; 46(3):1955-1974. https://doi.org/10.3390/cimb46030128
Chicago/Turabian StyleTüredi, Sibel, Hakim Çelik, Şeyda Nur Dağlı, Seyhan Taşkın, Uğur Şeker, and Mustafa Deniz. 2024. "An Examination of the Effects of Propolis and Quercetin in a Rat Model of Streptozotocin-Induced Diabetic Peripheral Neuropathy" Current Issues in Molecular Biology 46, no. 3: 1955-1974. https://doi.org/10.3390/cimb46030128