Novel Spray Dried Glycerol 2-Phosphate Cross-Linked Chitosan Microparticulate Vaginal Delivery System—Development, Characterization and Cytotoxicity Studies
Abstract
:1. Introduction
2. Results and Discussion
2.1. Characterization of Microparticles
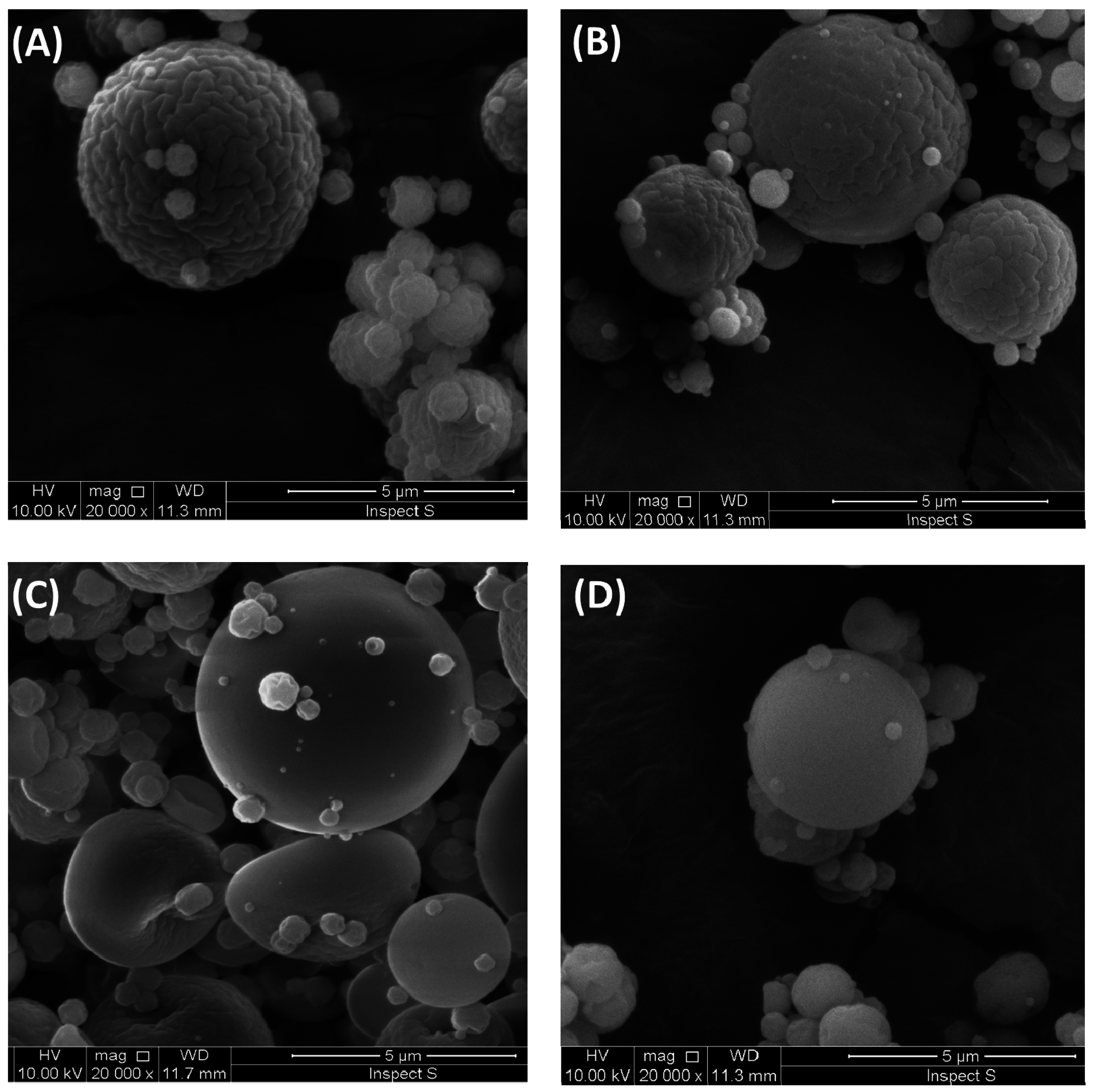
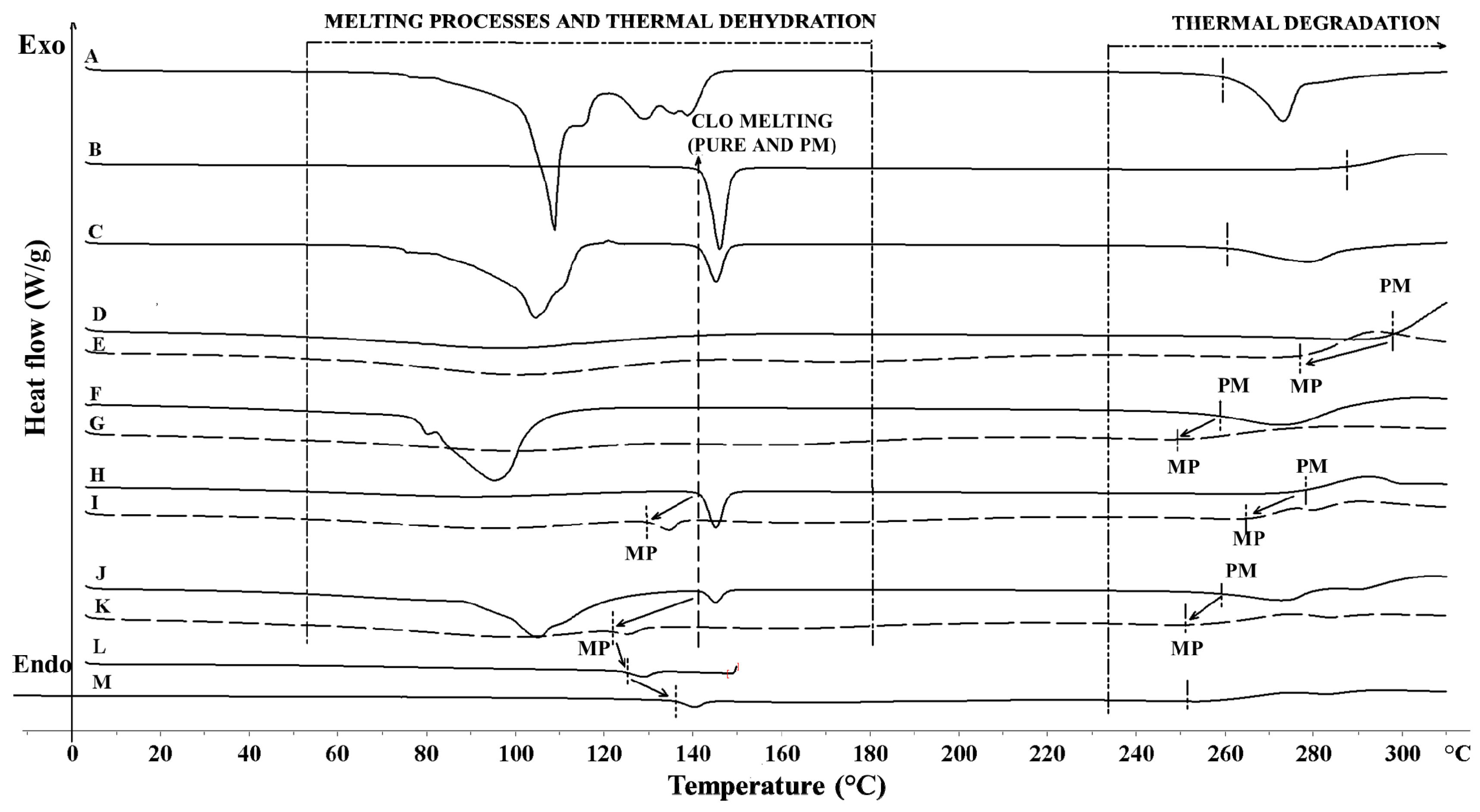
2.2. SEM and DSC Studies
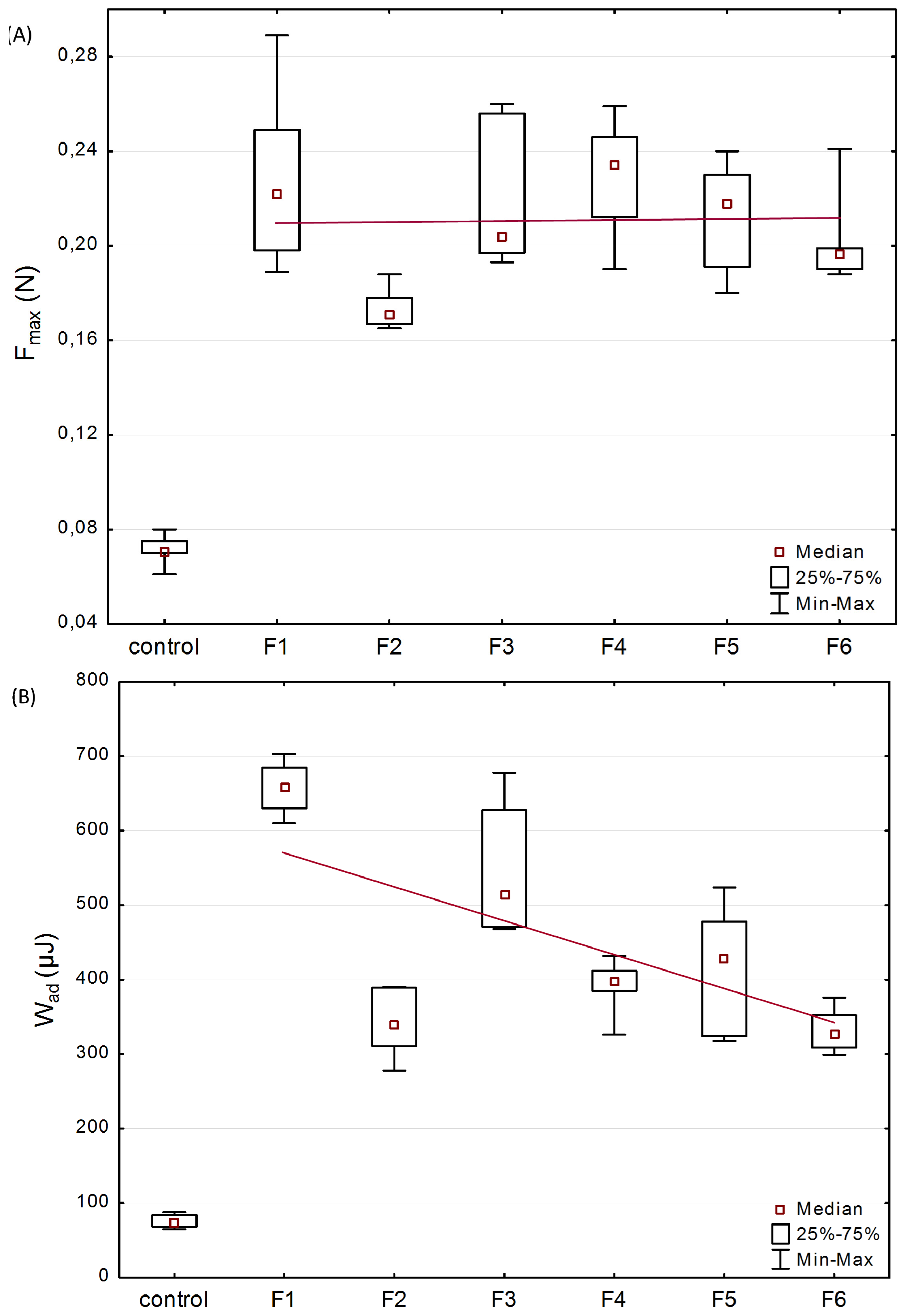
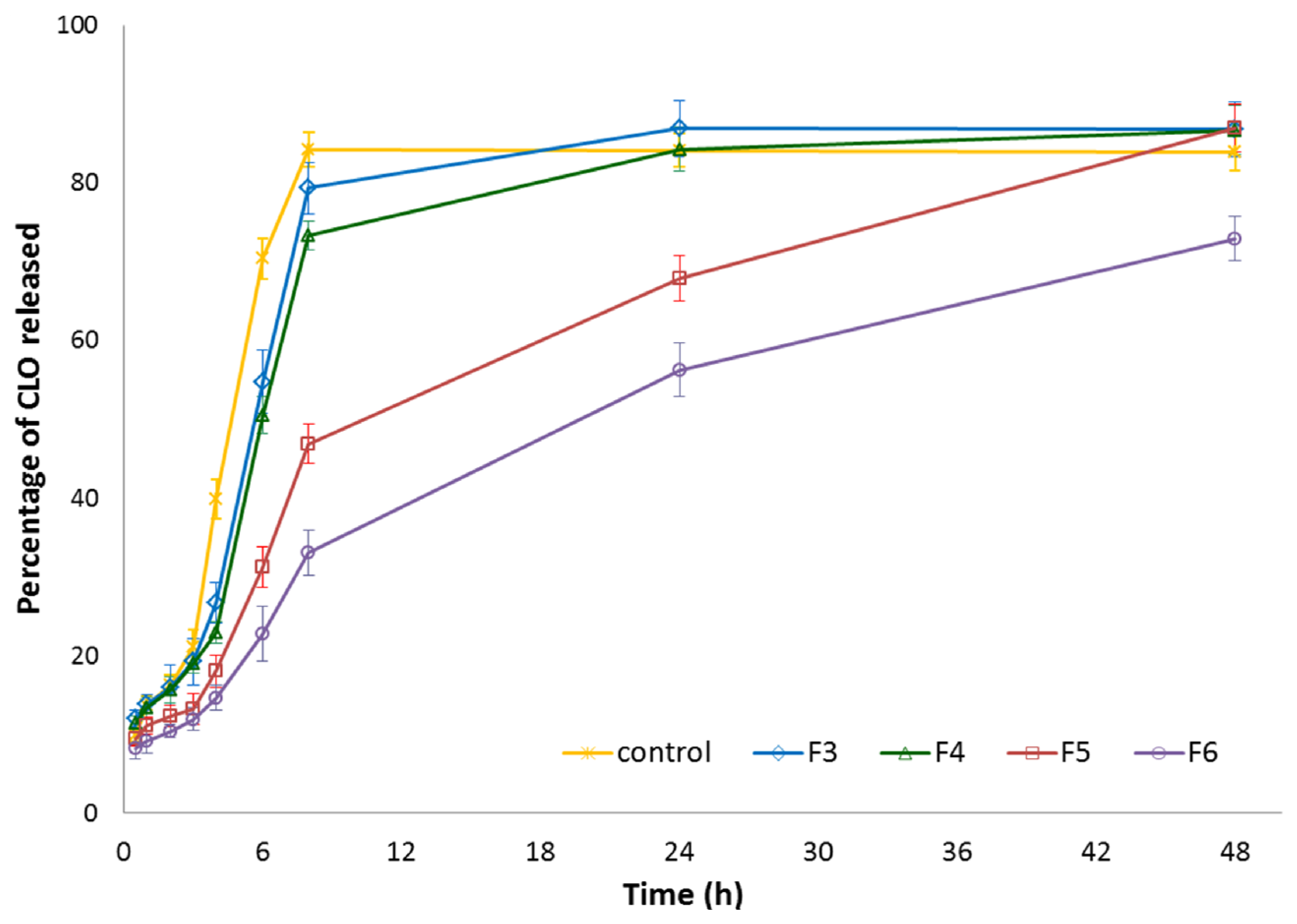
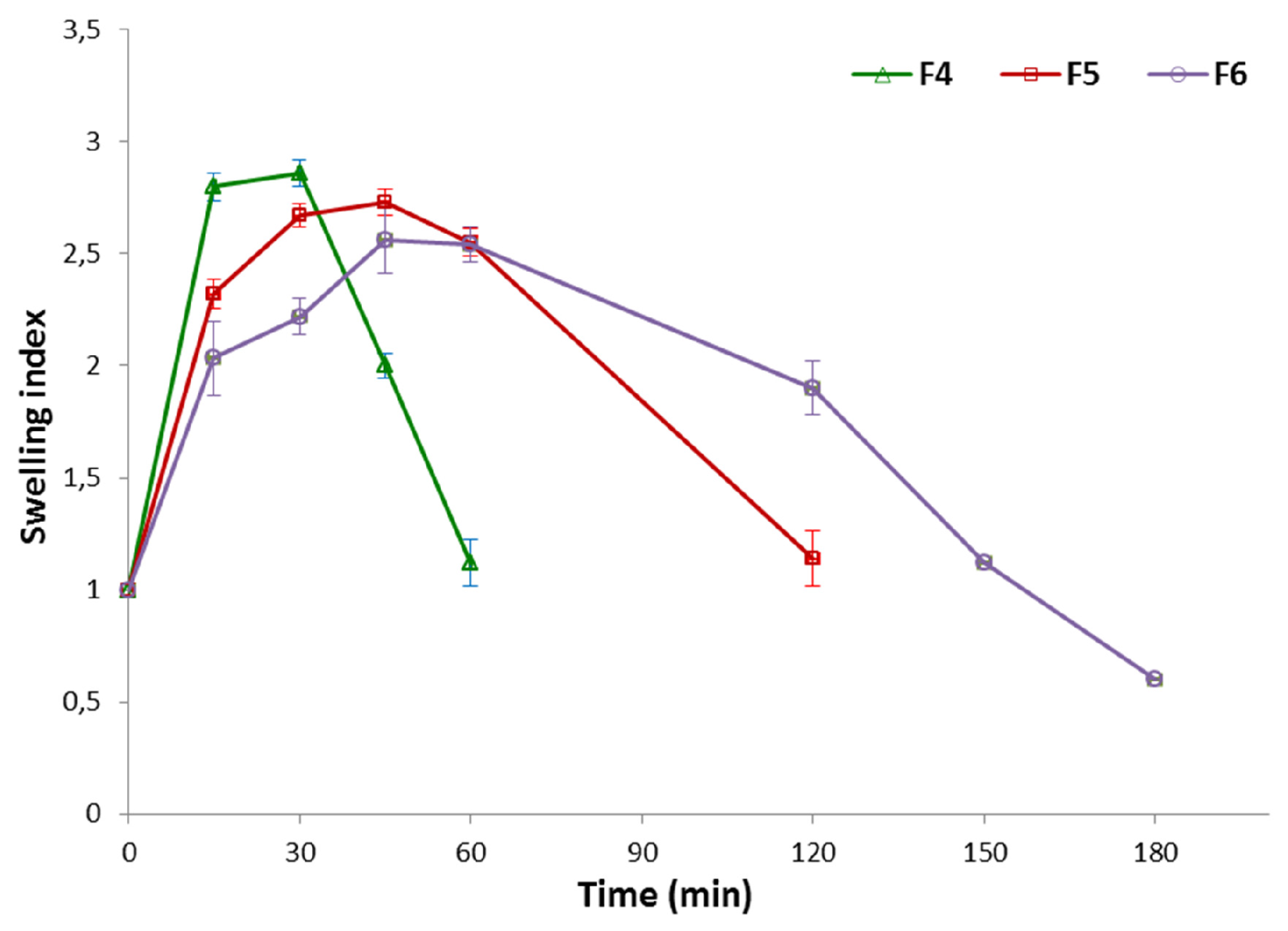
2.3. Mucoadhesive and in Vitro Drug Release Studies
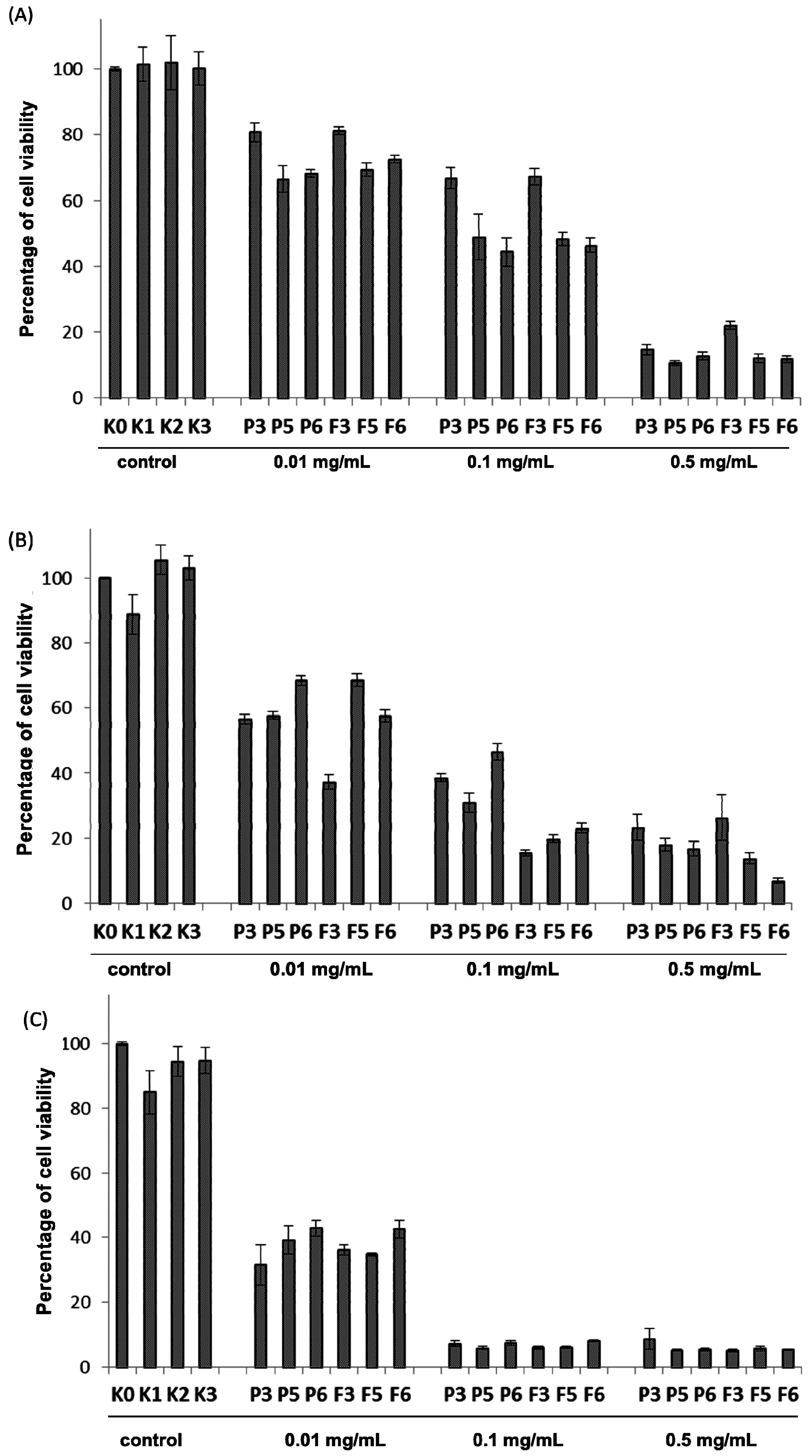
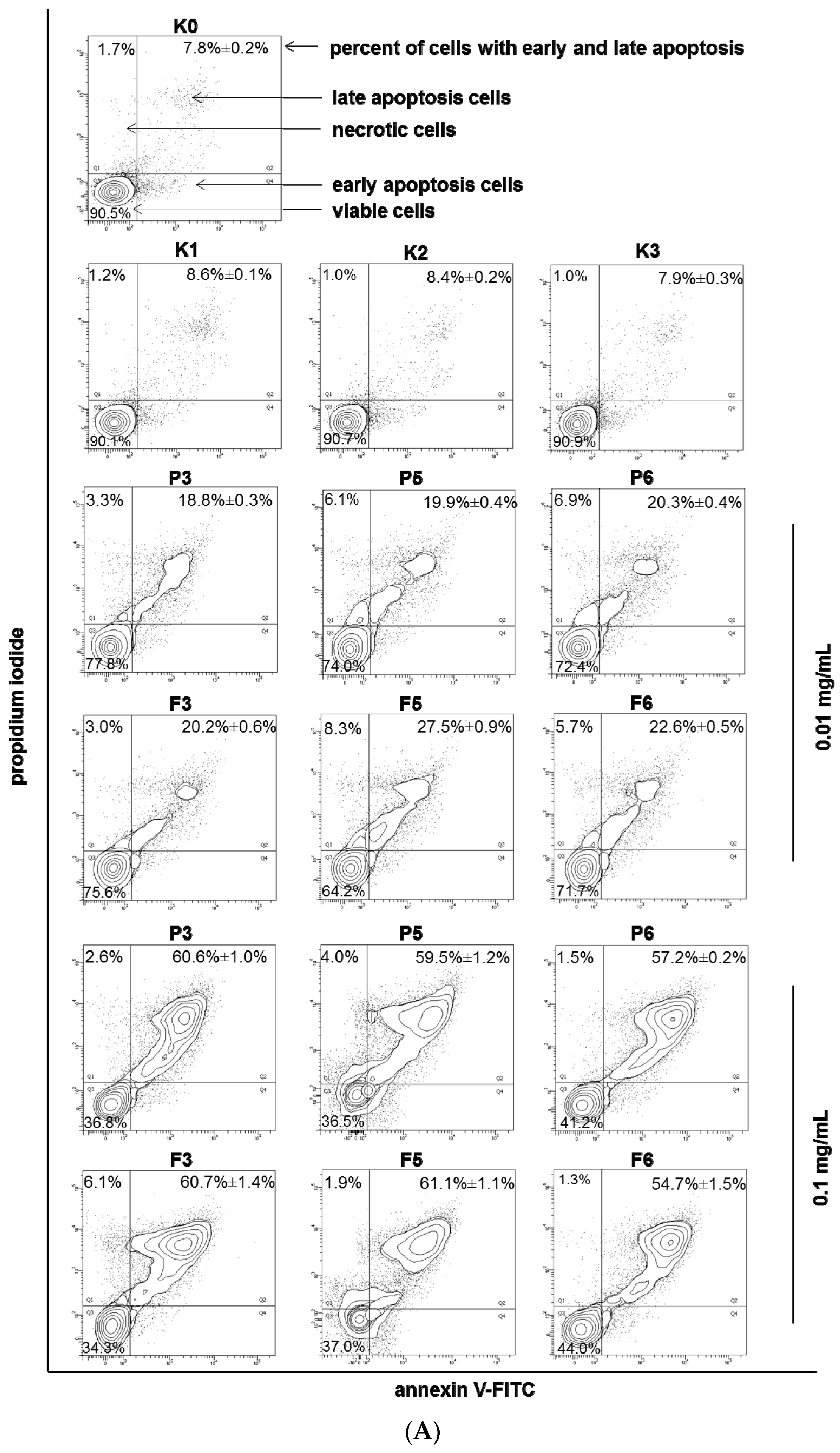
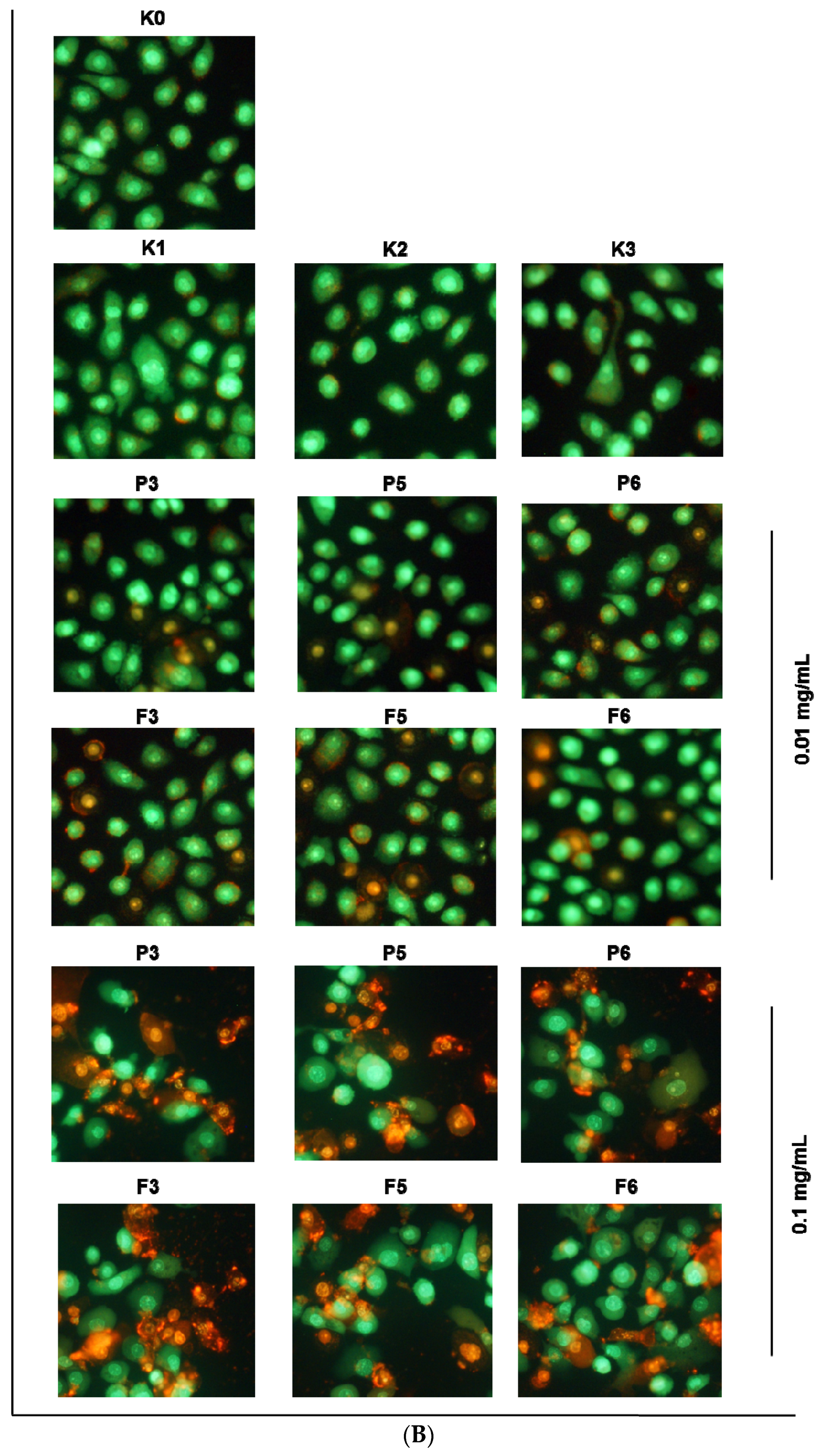
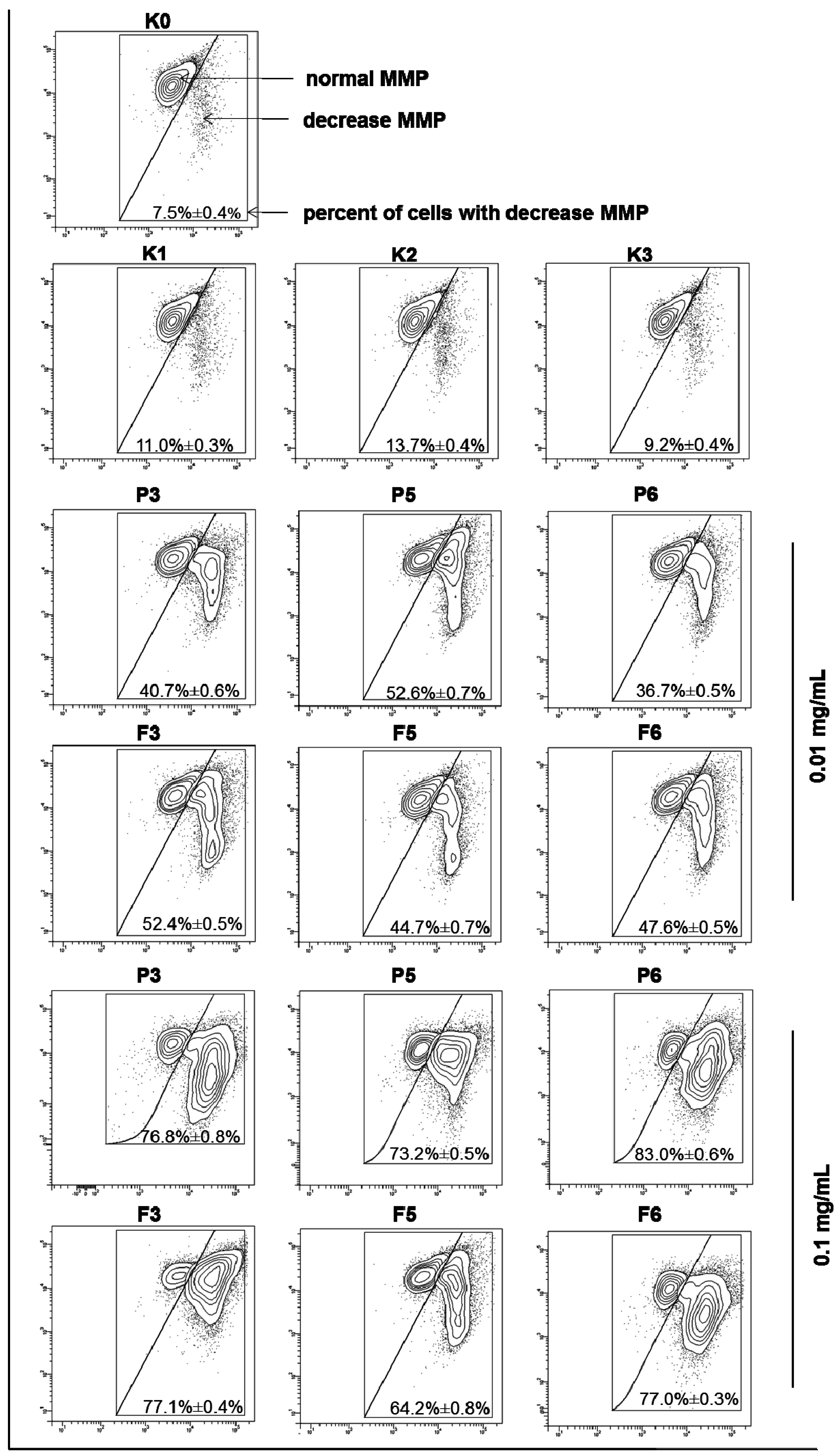
2.4. In Vitro Cytotoxicity Studies
3. Materials and Methods
3.1. Materials
3.2. Preparation of Microparticles
3.3. Morphology and Microparticle Size Analysis
3.4. Drug Loading, Encapsulation Efficacy and Production Yield
3.5. Moisture Content Determination
3.6. Differential Scanning Calorimetry
3.7. Determination of the Mucoadhesive Properties
3.8. Determination of the Residence Time
3.9. Swelling Index Test
3.10. In Vitro Drug Release Studies
3.11. Cell Culture
3.12. MTT Assay
3.13. Flow Cytometry Assessment of Annexin V-FITC/Propidium Iodide Binding
3.14. Fluorescent Microscopy Assay
3.15. Analysis of Mitochondrial Membrane Potential
3.16. Statistical Analysis
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Martín-Villena, M.J.; Fernández-Campos, F.; Calpena-Campmany, A.C.; Bozal-de Febrer, N.; Ruiz-Martínez, M.A.; Clares-Naveros, B. Novel microparticulate systems for the vaginal delivery of nystatin: Development and characterization. Carbohydr. Polym. 2013, 94, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Singh, M.N.; Hemant, K.S.Y.; Ram, M.; Shivakumar, H.G. Microencapsulation: A promising technique for controlled drug delivery. Res. Pharm. Sci. 2010, 5, 65–77. [Google Scholar] [PubMed]
- Sezer, A.D.; Cevher, E. Topical drug delivery using chitosan nano- and microparticles. Expert Opin. Drug Deliv. 2012, 9, 1129–1146. [Google Scholar] [CrossRef] [PubMed]
- Mishra, M.; Mishra, B. Mucoadhesive microparticles as potential carriers in inhalation delivery of doxycycline hyclate: A comparative study. Acta Pharm. Sin. B 2012, 2, 518–526. [Google Scholar] [CrossRef]
- Patel, J.K.; Patil, P.S.; Sutariya, V.B. Formulation and characterization of mucoadhesive microparticles of cinnarizine hydrochloride using supercritical fluid technique. Curr. Drug Deliv. 2016, 10, 317–325. [Google Scholar] [CrossRef]
- Szekalska, M.; Amelian, A.; Winnicka, K. Alginate microspeheres obtained by the spray drying technique as mucoadhesive carriers of ranitidine. Acta Pharm. 2015, 65, 15–27. [Google Scholar] [CrossRef] [PubMed]
- Cerchiara, T.; Abruzzo, A.; Parolin, C.; Vitali, B.; Bigucci, F.; Gallucci, M.C.; Nicoletta, F.P.; Luppi, B. Microparticles based on chitosan/carboxymethylcellulose polyelectrolyte complexes for colon delivery of vancomycin. Carbohydr. Polym. 2016, 143, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Sinha, V.R.; Singla, A.K.; Wadhawan, S.; Kaushik, R.; Kumria, R.; Bansal, K.; Dhawan, S. Chitosan microspheres as a potential carrier for drugs. Int. J. Pharm. 2004, 274, 1–33. [Google Scholar] [CrossRef] [PubMed]
- Wassmer, S.; Rafat, M.; Fong, W.G.; Baker, A.N.; Tsilfidis, C. Chitosan microparticles for delivery of proteins to the retina. Acta Biomater. 2013, 9, 7855–7864. [Google Scholar] [CrossRef] [PubMed]
- Dash, M.; Chiellini, F.; Ottenbrite, R.M.; Chiellini, E. Chitosan—A versatile semi-synthetic polymer in biomedical applications. Prog. Polym. Sci. 2011, 36, 981–1014. [Google Scholar] [CrossRef]
- Ifuku, S. Chitin and chitosan nanofibers: Preparation and chemical modifications. Molecules 2014, 19, 18367–18380. [Google Scholar] [CrossRef] [PubMed]
- Kong, M.; Chen, X.G.; Xing, K.; Park, H.J. Antimicrobial properties of chitosan and mode of action: A state of the art review. Int. J. Food Microbiol. 2010, 144, 51–63. [Google Scholar] [CrossRef] [PubMed]
- Shaji, J.; Jain, V.; Lodha, S. Chitosan: A novel pharmaceutical excipient. Int. J. Pharm. Appl. Sci. 2010, 1, 11–28. [Google Scholar]
- Yeh, T.H.; Hsu, L.W.; Tseng, M.T.; Lee, P.L.; Sonjae, K.; Ho, Y.C.; Sung, H.W. Mechanism and consequence of chitosan-mediated reversible epithelial tight junction opening. Biomaterials 2011, 32, 6164–6173. [Google Scholar] [CrossRef] [PubMed]
- Nilsen-Nygaard, J.; Strand, S.P.; Vårum, K.M.; Draget, K.I.; Nordgård, C.T. Chitosan: Gels and interfacial properties. Polymers 2015, 7, 552–579. [Google Scholar] [CrossRef]
- Andersen, T.; Bleher, S.; Eide Flaten, G.; Tho, I.; Mattsson, S.; Škalko-Basnet, N. Chitosan in mucoadhesive drug delivery: Focus on local vaginal therapy. Mar. Drugs 2015, 13, 222–236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kavianinia, I.; Plieger, P.G.; Cave, N.J.; Gopakumar, G.; Dunowska, M.; Kandile, N.G.; Harding, D.R. Design and evaluation of a novel chitosan-based system for colon-specific drug delivery. Int. J. Biol. Macromol. 2016, 85, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Sánchez, M.P.; Martín-Illana, A.; Ruiz-Caro, R.; Bermejo, P.; Abad, M.J.; Carro, R.; Bedoya, L.M.; Tamayo, A.; Rubio, J.; Fernández-Ferreiro, A.; et al. Chitosan and kappa-carrageenan vaginal acyclovir formulations for prevention of genital herpes. In vitro and ex vivo evaluation. Mar. Drugs 2015, 13, 5976–5992. [Google Scholar] [CrossRef] [PubMed]
- Caetano, L.A.; Almeida, A.J.; Gonçalves, L.M. Effect of experimental parameters on alginate/chitosan microparticles for BCG encapsulation. Mar. Drugs 2016, 14, 90–120. [Google Scholar] [CrossRef] [PubMed]
- Brako, F.; Raimi-Abraham, B.; Mahalingam, S.; Craig, D.Q.M.; Edirisinghe, M. Making nanofibres of mucoadhesive polymer blends for vaginal therapies. Eur. Polym. J. 2015, 70, 186–196. [Google Scholar] [CrossRef]
- Parhizkar, M.; Sofokleous, P.; Stride, E.; Edirisinghe, M. Novel preparation of controlled porosity particle/fibre loaded scaffolds using a hybrid micro-fluidic and electrohydrodynamic technique. Biofabrication 2014, 6, 045010–045024. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Zhang, C.; Agrahari, V.; Murowchick, J.B.; Oyler, N.A.; Youan, B.B. Spray drying tenofovir loaded mucoadhesive and pH-sensitive microspheres intended for HIV prevention. Antivir. Res. 2013, 97, 334–346. [Google Scholar] [CrossRef] [PubMed]
- Bohr, A.; Wan, F.; Kristensen, J.; Dyas, M.; Stride, E.; Baldursdottír, S.; Edirisinghe, M.; Yang, M. Pharmaceutical microparticle engineering with electrospraying: The role of mixed solvent systems in particle formation and characteristics. J. Mater. Sci. Mater. Med. 2015, 26, 61–74. [Google Scholar] [CrossRef] [PubMed]
- Eltayeb, M.; Stride, E.; Edirisinghe, M.; Harker, A. Electrosprayed nanoparticle delivery system for controlled release. Mater. Sci. Eng. C Mater. Biol. Appl. 2016, 66, 138–146. [Google Scholar] [CrossRef] [PubMed]
- Parhizkar, M.; Reardon, P.J.; Knowles, J.C.; Browning, R.J.; Stride, E.; Pedley, B.R.; Harker, A.H.; Edirisinghe, M. Electrohydrodynamic encapsulation of cisplatin in poly (lactic-co-glycolic acid) nanoparticles for controlled drug delivery. Nanomedicine 2016, 12, 1919–1929. [Google Scholar] [CrossRef] [PubMed]
- Gupta, N.V.; Natasha, S.; Getyala, A.; Bhat, R.S. Bioadhesive vaginal tablets containing spray dried microspheres loaded with clotrimazole for treatment of vaginal candidiasis. Acta Pharm. 2013, 63, 359–372. [Google Scholar] [CrossRef] [PubMed]
- Hani, U.; Shivakumar, H.G.; Gowrav, M.P. Formulation design and evaluation of a novel vaginal delivery system of clotrimazole. Int. J. Pharm. Sci. Res. 2014, 5, 220–227. [Google Scholar]
- Cal, K.; Sollohub, K. Spray drying technique. I: Hardware and process parameters. J. Pharm. Sci. 2010, 99, 575–586. [Google Scholar] [CrossRef] [PubMed]
- Anal, A.K.; Stevens, W.F.; Remuñán-López, C. Ionotropic cross-linked chitosan microspheres for controlled release of ampicillin. Int. J. Pharm. 2006, 7, 166–173. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.; Thakur, K.; Sharma, G.; Kush, P.; Jain, U.K. Fabrication, characterization and cytotoxicity studies of ionically cross-linked docetaxel loaded chitosan nanoparticles. Carbohydr. Polym. 2016, 137, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Mourya, V.K.; Inamdar, N.N. Chitosan—Modifications and applications: Opportunities galore. React. Funct. Polym. 2008, 68, 1013–1051. [Google Scholar] [CrossRef]
- Ding, K.; Yang, Z.; Zhang, Y.L.; Xu, J.Z. Injectable thermosensitive chitosan/β-glycerophosphate/collagen hydrogel maintains the plasticity of skeletal muscle satellite cells and supports their in vivo viability. Cell Biol. Int. 2013, 37, 977–987. [Google Scholar] [CrossRef] [PubMed]
- Rossi, S.; Ferrari, F.; Bonferoni, M.C.; Sandri, G.; Faccendini, A.; Puccio, A.; Caramella, C. Comparison of poloxamer- and chitosan-based thermally sensitive gels for the treatment of vaginal mucositis. Drug Dev. Ind. Pharm. 2014, 40, 352–360. [Google Scholar] [CrossRef] [PubMed]
- Supper, S.; Anton, N.; Seidel, N.; Riemenschnitter, M.; Curdy, C.; Vandamme, T. Thermosensitive chitosan/glycerophosphate-based hydrogel and its derivatives in pharmaceutical and biomedical applications. Expert Opin. Drug Deliv. 2014, 11, 249–267. [Google Scholar] [CrossRef] [PubMed]
- Szymańska, E.; Sosnowska, K.; Miltyk, W.; Rusak, M.; Basa, A.; Winnicka, K. The effect of β-glycerophosphate cross-linking on chitosan cytotoxicity and properties of hydrogels for vaginal application. Polymers 2015, 7, 2223–2244. [Google Scholar] [CrossRef]
- Szymańska, E.; Winnicka, K.; Wieczorek, P.; Sacha, P.T.; Tryniszewska, E.A. Influence of unmodified and beta-glycerophosphate cross-linked chitosan on anti-Candida activity of clotrimazole in semi-solid delivery systems. Int. J. Mol. Sci. 2014, 15, 17765–17777. [Google Scholar] [CrossRef] [PubMed]
- Mucha, M.; Pawlak, A. Thermal analysis of chitosan and its blends. Thermochim. Acta 2005, 427, 69–76. [Google Scholar] [CrossRef]
- Sigma Aldrich. Available online: http://www.sigmaaldrich.com/catalog/product/sigma/g9422?lang=en®ion=SI (assessed on 3 August 2016).
- Bromana, E.; Khoob, C.; Taylor, L.S. A comparison of alternative polymer excipients and processing methods for making solid dispersions of a poorly water soluble drug. Int. J. Pharm. 2001, 222, 139–151. [Google Scholar] [CrossRef]
- D’Cruz, O.J.; Erbeck, D.; Uckun, F.M. A study of the potential of the pig as a model for the vaginal irritancy of benzalkonium chloride in comparison to the nonirritant microbicide PHI-443 and the spermicide vanadocene dithiocarbamate. Toxicol. Pathol. 2005, 33, 465–476. [Google Scholar] [CrossRef] [PubMed]
- Abruzzo, A.; Bigucci, F.; Cerchiara, T.; Saladini, B.; Gallucci, M.C.; Cruciani, F.; Vitali, B.; Luppi, B. Chitosan/alginate complexes for vaginal delivery of chlorhexidine digluconate. Carbohydr. Polym. 2013, 91, 651–658. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, M.; Gonçalves, I.C.; Nardecchia, S.; Amaral, I.F.; Barbosa, M.A.; Martins, M.C. Modulation of stability and mucoadhesive properties of chitosan microparticles for therapeutic gastric application. Int. J. Pharm. 2013, 454, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Chenite, A.; Buschmann, M.; Wang, D.; Chaput, C.; Kandani, N. Rheological characterisation of thermogelling chitosan/glycerol-phosphate solutions. Carbohydr. Polym. 2001, 46, 39–47. [Google Scholar] [CrossRef]
- Nakamura, F.; Ohta, R.; Machida, Y.; Nagai, T. In vitro and in vivo nasal mucoadhesion of some water-soluble polymers. Int. J. Pharm. 1996, 134, 173–181. [Google Scholar] [CrossRef]
- Gupta, J.; Tao, J.Q.; Garg, S.; Al-Kassas, R. Design and development of an in vitro assay for evaluation of solid vaginal dosage forms. Pharmacol. Pharm. 2011, 2, 289–298. [Google Scholar] [CrossRef]
- Baldrick, P. The safety of chitosan as a pharmaceutical excipient. Regul. Toxicol. Pharmacol. 2010, 56, 290–299. [Google Scholar] [CrossRef] [PubMed]
- Gades, M.D.; Stern, J.S. Chitosan supplementation and fecal fat excretion in men. Obes. Res. 2003, 11, 683–688. [Google Scholar] [CrossRef] [PubMed]
- Hirano, S.; Iwata, M.; Yamanaka, K.; Tanaka, H.; Toda, T.; Inui, H. Enhancement of serum lysozyme activity by injecting a mixture of chitosan oligosaccharides intravenously in rabbits. Agric. Biol. Chem. 1991, 55, 2623–2629. [Google Scholar]
- Rodrigues, S.; Dionísio, M.; López, C.R.; Grenha, A. Biocompatibility of chitosan carriers with application in drug delivery. J. Func. Biomater. 2012, 3, 615–641. [Google Scholar] [CrossRef] [PubMed]
- Martin, D.; Lenardo, M. Morphological, biochemical, and flow cytometric assays of apoptosis. Curr. Protoc. Mol. Biol. 2001, 49. [Google Scholar] [CrossRef]
- Prego, C.; Torres, D.; Alonso, M.J. Chitosan nanocapsules as carriers for oral peptide delivery: Effect of chitosan molecular weight and type of salt on the in vitro behaviour and in vivo effectiveness. J. Nanosci. Nanotechol. 2006, 6, 2921–2928. [Google Scholar] [CrossRef]
- Pai, R.V.; Jain, R.R.; Bannalikor, A.S.; Menon, M.D. Development and evaluation of chitosan microparticles based dry powder inhalation formulations of rifampicin and rifabutin. J. Aerosol Med. Pulm. Drug Deliv. 2015, 29, 179–195. [Google Scholar] [CrossRef] [PubMed]
- Meng, J.; Zhang, T.; Agrahari, V.; Ezoulin, M.J.; Youan, B.B. Comparative biophysical properties of tenofovir-loaded, thiolated and nonthiolated chitosan nanoparticles intended for HIV prevention. Nanomedicine 2014, 9, 1595–1612. [Google Scholar] [CrossRef] [PubMed]
- Lemasters, J.J.; Qian, T.; Bradham, C.A.; Brenner, D.A.; Cascio, W.E.; Trost, L.C.; Nishimura, Y.; Nieminen, A.L.; Herman, B. Mitochondrial dysfunction in the pathogenesis of necrotic and apoptotic cell death. J. Bioenerg. Biomembr. 1999, 31, 305–319. [Google Scholar] [CrossRef] [PubMed]
- Czechowska-Biskup, R.; Jarosińska, D.; Rokita, B.; Ulański, P.; Rosiak, J.M. Determination degree of deacetylation of chitosan: Comparison of methods. Prog. Chem. Appl. Chitin Its Deriv. 2012, 17, 5–20. [Google Scholar]
- Squier, C.A.; Mantz, M.J.; Schlievert, P.M.; Davis, C.C. Porcine vagina ex vivo as a model for studying permeability and pathogenesis in mucosa. J. Pharm. Sci. 2008, 97, 9–21. [Google Scholar] [CrossRef] [PubMed]
- The European Directorate for the Quality of Medicines. The European Pharmacopeia, 8th ed.; Council of Europe: Strasburg, France, 2014; Volume 1. [Google Scholar]
- Pedersen, M. Effect of hydrotropic substances on the complexation of clotrimazole with β-cyclodextrin. Drug Dev. Ind. Pharm. 1993, 19, 439–448. [Google Scholar] [CrossRef]
- Martinac, A.; Filipović-Grčić, J.; Perissutti, B.; Voinovich, D.; Pavelić, Z. Spray-dried chitosan/ethylcellulose microspheres for nasal drug delivery: Swelling study and evaluation of in vitro drug release properties. J. Microencapsul. 2005, 22, 549–561. [Google Scholar] [CrossRef] [PubMed]
- Hájková, R.; Sklenářová, H.; Matysová, L.; Švecová, P.; Solich, P. Development and validation of HPLC method for determination of clotrimazole and its two degradation products in spray formulations. Talanta 2007, 73, 483–489. [Google Scholar] [CrossRef] [PubMed]
- Szymańska, E.; Winnicka, K.; Amelian, A.; Cwalina, U. Vaginal chitosan tablets with clotrimazole-design and evaluation of mucoadhesive properties using porcine vaginal mucosa, mucin and gelatine. Chem. Pharm. Bull. 2014, 62, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Huang, M.; Khor, E.; Lim, L.Y. Uptake and cytotoxicity of chitosan molecules and nanoparticles: Effects of molecular weight and degree of deacetylation. Pharm. Res. 2004, 21, 344–353. [Google Scholar] [CrossRef] [PubMed]
- Carmichael, J.; Degraff, W.; Gazdar, A.; Minna, J.; Mitchell, J. Evaluation of a tetrazolium-based semiautomated colorimetric assay: Assessment of chemosensitivity testing. Cancer Res. 1987, 47, 936–942. [Google Scholar] [PubMed]
- Westermann, B. Molecular machinery of mitochondrial fusion and fission. J. Biol. Chem. 2008, 283, 13501–13505. [Google Scholar] [CrossRef] [PubMed]
- Winnicka, K.; Bielawski, K.; Bielawska, A. Synthesis and cytotoxic activity of G3 PAMAM-NH2 dendrimer-modified digoxin and proscillaridin A conjugates in breast cancer cells. Pharmacol. Rep. 2010, 62, 414–423. [Google Scholar] [CrossRef]
- Czarnomysy, R.; Bielawska, A.; Muszyńska, A.; Bielawski, K. Effects of novel alkyl pyridine platinum complexes on apoptosis in Ishikawa endometrial cancer cells. Med. Chem. 2015, 11, 540–550. [Google Scholar] [CrossRef] [PubMed]
| Formu-lation | βGP:CS Ratio (w/w) | CLO:CS Ratio (w/w) | Production Yield (%) a * | Encapsulation Efficacy (%) b * | CLO Loading (%) c * | Diameter Range (Mean Diameter *) (μm) | Moisture Content (%) * | Residence Time (min) * |
|---|---|---|---|---|---|---|---|---|
| 1.0% (w/v) chitosan solution | ||||||||
| F1 | - | 1:4 | 75.4 ± 1.3 | 59.5 ± 3.1 | 11.2 ± 2.8 | n.t. | 14.3 ± 3.5 | n.t. |
| F2 | 1:2 | 1:4 | 78.0 ± 1.6 | 58.2 ± 3.9 | 8.3 ± 2.7 | n.t. | 8.9 ± 2.6 | n.t. |
| F3 | - | 1:3 | 73.5 ± 0.9 | 67.2 ± 9.1 | 16.8 ± 4.1 | 1.52–5.28 (3.39 ± 1.87) | 10.4 ± 2.9 | 60 ± 2 |
| F4 | 1:3 | 1:3 | 78.8 ± 1.2 | 59.6 ± 1.0 | 11.9 ± 2.7 | 1.49–6.33 (3.96 ± 2.45) | 7.6 ± 2.2 | 116 ± 4 |
| F5 | 1:2 | 1:3 | 79.5 ± 1.1 | 73.2 ± 9.0 | 13.3 ± 3.2 | 1.23–5.25 (3.12 ± 2.13) | 6.5 ± 2.4 | 132 ± 5 |
| F6 | 1.5:2 | 1:3 | 80.6 ± 1.9 | 68.4 ± 11.3 | 10.9 ± 2.1 | 0.93–3.93 (2.54 ± 1.59) | 7.9 ± 2.7 | 154 ± 5 |
| Abbreviation | Description | |
|---|---|---|
| K0 | non treated cells | |
| K1 | Cells treated with: | acetic buffer pH 4.5 |
| K2 | aqueous solution of βGP * | |
| K3 | aqueous solution of βGP ** | |
| P3/F3 | unmodified chitosan placebo/drug-loaded microparticles | |
| P5/F5 | βGP:chitosan (1:2) placebo/drug-loaded microparticles | |
| P6/F6 | βGP:chitosan (1.5:2) placebo/drug-loaded microparticles | |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szymańska, E.; Szekalska, M.; Czarnomysy, R.; Lavrič, Z.; Srčič, S.; Miltyk, W.; Winnicka, K. Novel Spray Dried Glycerol 2-Phosphate Cross-Linked Chitosan Microparticulate Vaginal Delivery System—Development, Characterization and Cytotoxicity Studies. Mar. Drugs 2016, 14, 174. https://doi.org/10.3390/md14100174
Szymańska E, Szekalska M, Czarnomysy R, Lavrič Z, Srčič S, Miltyk W, Winnicka K. Novel Spray Dried Glycerol 2-Phosphate Cross-Linked Chitosan Microparticulate Vaginal Delivery System—Development, Characterization and Cytotoxicity Studies. Marine Drugs. 2016; 14(10):174. https://doi.org/10.3390/md14100174
Chicago/Turabian StyleSzymańska, Emilia, Marta Szekalska, Robert Czarnomysy, Zoran Lavrič, Stane Srčič, Wojciech Miltyk, and Katarzyna Winnicka. 2016. "Novel Spray Dried Glycerol 2-Phosphate Cross-Linked Chitosan Microparticulate Vaginal Delivery System—Development, Characterization and Cytotoxicity Studies" Marine Drugs 14, no. 10: 174. https://doi.org/10.3390/md14100174






