Benefits of Selected Physical Exercise Programs in Detention: A Randomized Controlled Study
Abstract
:1. Introduction
2. Methods
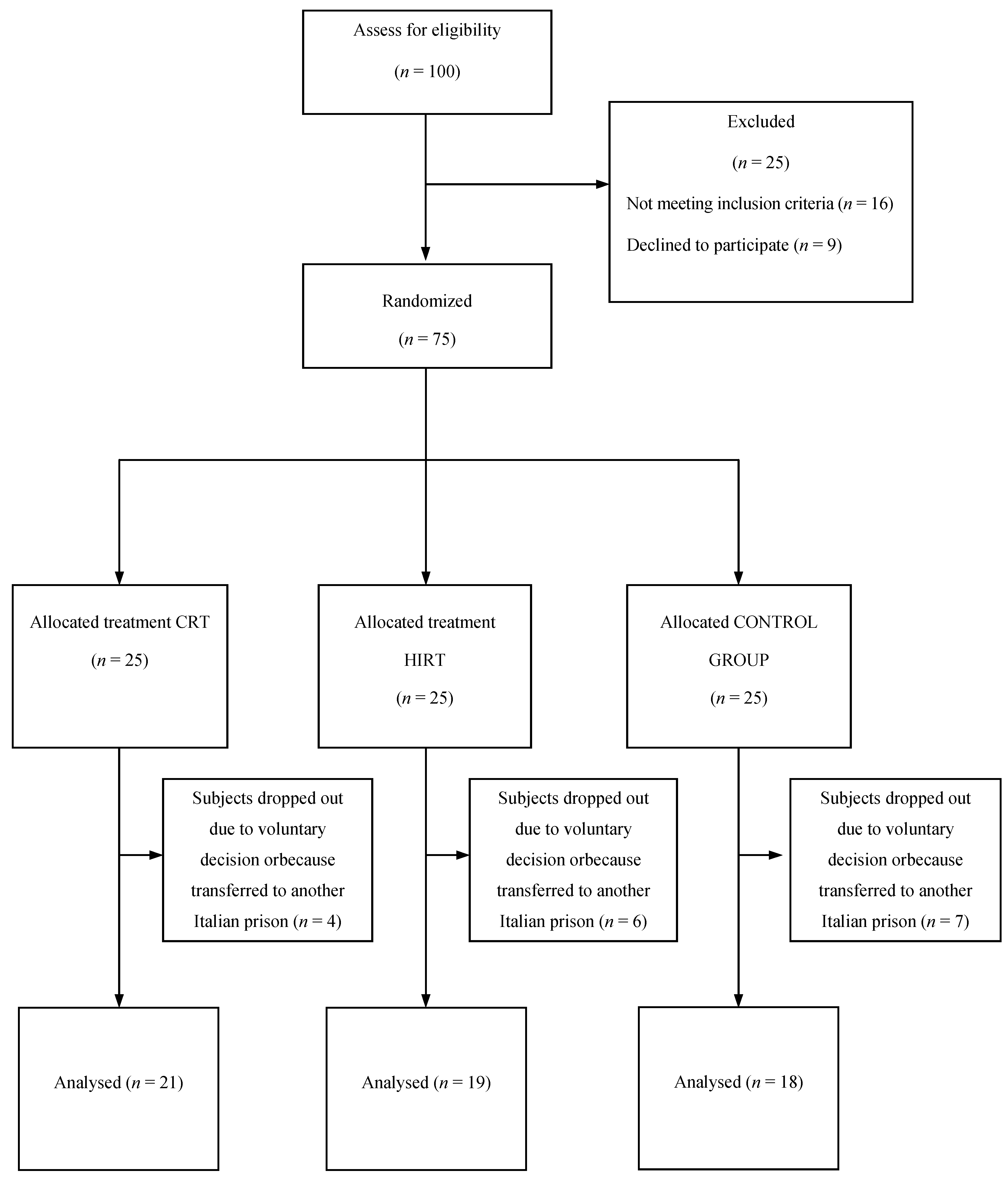
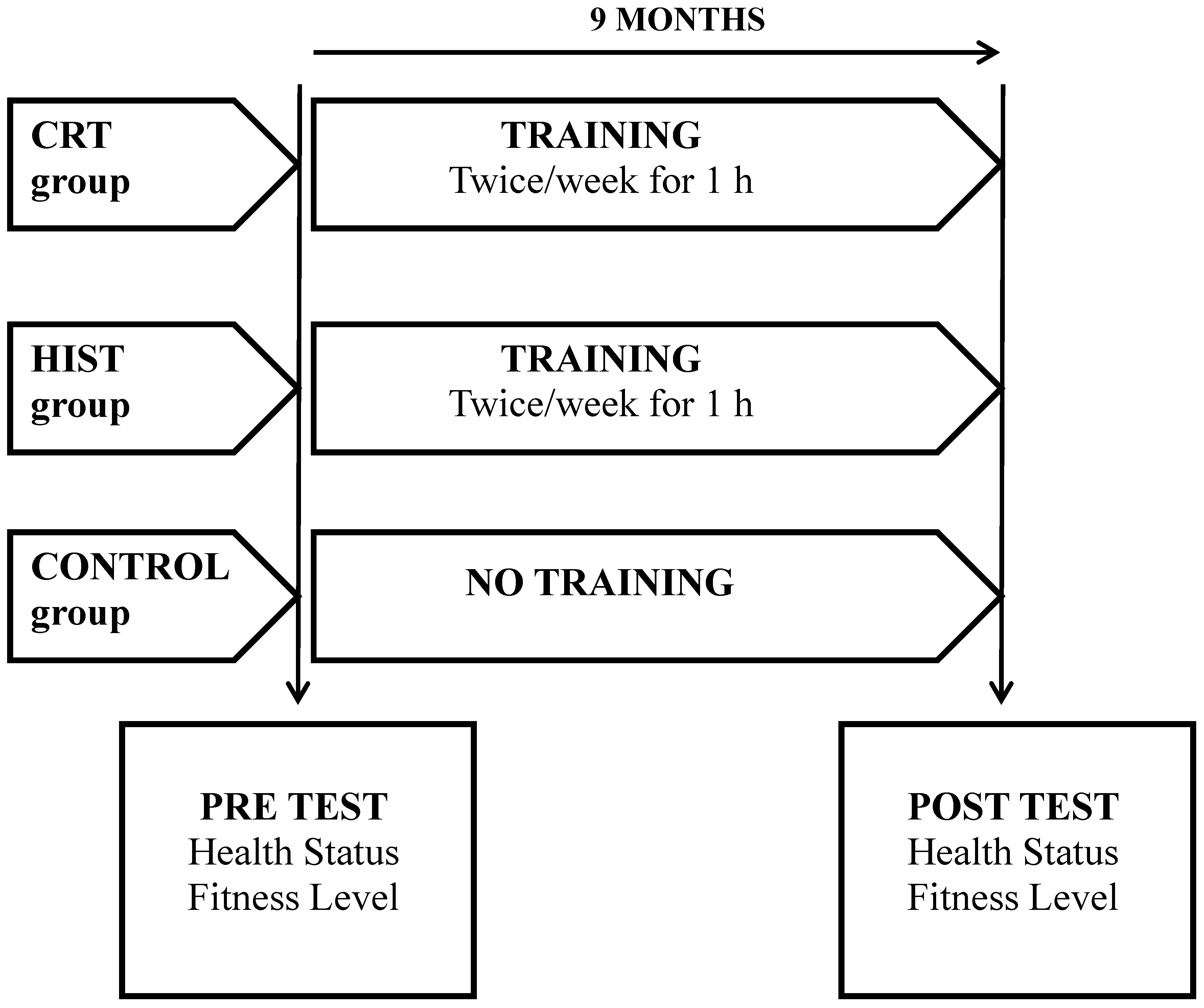
2.1. Study Design
2.2. Subjects
| CRT (n = 25) | HIRT (n = 25) | CONTROL GROUP (n =25) | |
|---|---|---|---|
| Age (years) | 30.1 ± 5.9 | 33.9 ± 6.8 | 32.8 ± 8.9 |
| Prison term (years) | 6.5 ± 4.8 | 9.7 ± 5.2 | 10.8 ± 7.2 |
| Prisonterm completed (years) | 3.7 ± 2.8 | 5.4 ± 4.7 | 4.3 ± 3.5 |
| Prisonterm remaining (years) | 2.8 ± 4.3 | 4.4 ± 2.2 | 6.5 ± 5.6 |
2.3. Experimental Procedures
2.4. Health Status Measures
2.5. Fitness Level Testing Session
2.6. Statistical Analyses
3. Results
4. Discussion
| Variable | CRT (n = 21) | HIST (n = 19) | CONTROL GROUP (n = 18) | ηp2 | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PRE | POST | PRE | POST | PRE | POST | ||||||||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||||||||
| BMI (kg/m2) | 29.6 | ± | 4.1 ** | 28.0 | ± | 3.5 | 27.8 | ± | 3.8 | 27.5 | ± | 2.6 | 28.3 | ± | 2.7 ** | 28.7 | ± | 2.7 | 0.07 |
| SBP (mmHg) | 124.7 | ± | 8.1 ** | 113.0 | ± | 11.9 | 121.0 | ± | 8.9 | 119.3 | ± | 11.0 | 119.2 | ± | 6.4 | 120.8 | ± | 16.6 | 0.08 |
| DBP (mmHg) | 73.3 | ± | 7.0 ** | 67.3 | ± | 7.0 | 74.0 | ± | 5.1 | 70.0 | ± | 4.1 | 68.5 | ± | 9.0 | 71.9 | ± | 7.5 | 0.06 |
| SPO2 (%) | 96.6 | ± | 3.8 | 98.6 | ± | 0.8 ## | 97.8 | ± | 1.5 | 98.6 | ± | 1.0 ## | 97.8 | ± | 0.9 | 97.4 | ± | 1.1 | 0.05 |
| CVF (L) | 4.8 | ± | 0.7 | 4.9 | ± | 0.7 | 4.9 | ± | 0.7 | 5.0 | ± | 0.6 | 4.8 | ± | 0.4 | 4.9 | ± | 0.5 | 0.13 |
| FEV1 (L) | 4.2 | ± | 0.7 | 4.3 | ± | 0.6 | 4.1 | ± | 0.4 | 4.2 | ± | 0.4 | 4.1 | ± | 0.3 | 4.2 | ± | 0.3 | 0.05 |
| Tiffenauindex (%) | 87.7 | ± | 8.8 | 87.1 | ± | 7.8 | 85.1 | ± | 6.3 | 84.2 | ± | 8.1 | 85.6 | ± | 7.9 | 86.2 | ± | 8.4 | 0.003 |
| C-Total (mmol/L) | 5.1 | ± | 1.1 | 5.1 | ± | 1.0 | 4.8 | ± | 0.6 ** | 5.0 | ± | 0.6 | 5.1 | ± | 0.6 | 5.2 | ± | 0.9 | 0.007 |
| C-HDL (mmol/L) | 1.2 | ± | 0.3 ** | 1.4 | ± | 0.2 # | 1.1 | ± | 0.3 ** | 1.3 | ± | 0.4 | 1.2 | ± | 0.4 | 1.2 | ± | 0.3 | 0.33 |
| C-LDL (mmol/L) | 2.9 | ± | 1.1 | 2.8 | ± | 1.0 | 2.8 | ± | 0.8 | 2.8 | ± | 0.8 | 3.0 | ± | 0.6 | 3.1 | ± | 0.9 | 0.002 |
| CHD riskindex | 4.6 | ± | 1.8 ** | 3.8 | ± | 1.1 | 5.0 | ± | 2.6 * | 4.3 | ± | 1.8 | 4.7 | ± | 1.9 | 4.4 | ± | 1.8 | 0.17 |
| Triglycerides (mmol/L) | 2.1 | ± | 0.5 * | 2.0 | ± | 0.4 | 2.1 | ± | 0.3 | 2.0 | ± | 0.3 | 1.9 | ± | 0.4 * | 2.0 | ± | 0.4 | 0.06 |
| Variable | CRT (n = 21) | HIST (n = 19) | CONTROL GROUP (n = 18) | ηp2 | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PRE | POST | PRE | POST | PRE | POST | ||||||||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||||||||
| Step test (mL/kg/min) | 28.9 | ± | 5.1 ** | 31.4 | ± | 4.6 ## | 28.8 | ± | 4.2 | 28.5 | ± | 4.1 | 27.0 | ± | 4.2 | 26.5 | ± | 4.3 | 0.07 |
| Sit and Reach (cm) | 23.8 | ± | 6.3 ** | 29.0 | ± | 6.9 ##,† | 19.3 | ± | 6.2 | 21.8 | ± | 5.5 | 20.7 | ± | 3.7 | 22.2 | ± | 4.8 | 0.30 |
| Half sit up test (n) | 26.5 | ± | 5.5 ** | 31.4 | ± | 9.1† | 29.4 | ± | 6.8 ** | 42.8 | ± | 12.8 # | 29.6 | ± | 8.7 | 31.2 | ± | 10.8 | 0.26 |
| Push up test (n) | 33.3 | ± | 10.4 ** | 43.8 | ± | 12.5 ## | 25.7 | ± | 10.2 ** | 35.7 | ± | 13.9 | 30.7 | ± | 13.3 | 24.8 | ± | 16.8 | 0.10 |
| Armcurl test (n) | 22.9 | ± | 3.9 ** | 28.9 | ± | 4.8 ##,† | 19.7 | ± | 4.9 * | 23.7 | ± | 4.3 ## | 20.1 | ± | 3.7 | 17.8 | ± | 5.5 | 0.19 |
| Flamingo balance test (s) | 3.1 | ± | 1.8 | 2.1 | ± | 2.3 ## | 4.9 | ± | 3.8 * | 2.9 | ± | 1.8 ## | 3.2 | ± | 2.9 ** | 5.8 | ± | 3.3 | 0.003 |
| 10 × 5 shuttle test (s) | 25.9 | ± | 2.7 ** | 21.9 | ± | 2.3 ## | 27.3 | ± | 3.0 ** | 23.8 | ± | 1.3 ## | 24.9 | ± | 4.6 * | 27.1 | ± | 4.5 | 0.25 |
5. Conclusions
Acknowledgments
Conflicts of Interest
References
- De Viggiani, N. Unhealthy prisons: Exploring structural determinants of prison health. Sociol. Health Illn. 2007, 29, 115–135. [Google Scholar] [CrossRef]
- Walmsley, R. World Prison Population List, 8th ed; International Centre for Prison Studies, Kings College London: London, UK, 2009. [Google Scholar]
- Fazel, S.; Baillargeon, J. The health of prisoners. Lancet 2011, 12, 956–965. [Google Scholar] [CrossRef]
- Baillargeon, J.; Black, S.A.; Pulvino, J.; Dunn, K. The disease profile for Texas prison inmates. Ann. Epidemiol. 2000, 10, 74–80. [Google Scholar]
- Pérez-Moreno, F.; Cámara-Sánchez, M.; Tremblay, J.F.; Riera-Rubio, V.J.; Gil-Paisan, L.; Lucia, A. Benefits of exercise training in spanish prison inmates. Int. J. Sports Med. 2007, 28, 1–7. [Google Scholar] [CrossRef]
- Marshall, T.; Simpson, S.; Stevens, A. Use of health services by prison inmates: Comparisons with the community. J. Epidemiol. Commun. Health 2001, 55, 364–365. [Google Scholar] [CrossRef]
- Owens, J.F. It is never too late; Changes in physical activity foster change in cardiovascular risk factor in middle aged women. Int. J. Sports Med. 2003, 6, 22–28. [Google Scholar]
- Wang, E.A.; Pletcher, M.; Lin, F.; Vittinghoff, E.; Kertesz, S.G.; Kiefe, C.I.; Bibbins-Domingo, K. Incarceration, incident hypertension, and access to health care: Findings from the coronary artery risk development in young adults (CARDIA) study. Arch. Intern. Med. 2009, 169, 687–693. [Google Scholar] [CrossRef]
- Hardman, A.E. Physical activity, obesity and blood lipids. Int. J. Obes. (Lond.) 1999, 23, S64–S71. [Google Scholar]
- Després, J.P. Dyslipidaemia and obesity. Baillieres Clin. Endocrinol. Metab. 1994, 8, 629–660. [Google Scholar]
- Couillard, C.; Després, J.P.; Lamarche, B.; Bergeron, J.; Gagnon, J.; Leon, A.S.; Rao, D.C.; Skinner, J.S.; Wilmore, J.H.; Bouchard, C. Effects of endurance exercise training on plasma HDL cholesterol levels depend on levels of triglycerides: Evidence from men of the Health, Risk Factors, Exercise Training and Genetics (HERITAGE) Family Study. Arterioscler. Thromb. Vasc. Biol. 2001, 21, 1226–1232. [Google Scholar] [CrossRef]
- Minges, K.E.; Cormick, G.; Unglik, E.; Dunstan, D.W. Evaluation of a resistance training program for adults with or at risk of developing diabetes: An effectiveness study in a community setting. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 50. [Google Scholar] [CrossRef]
- Lloyd-Jones, D.M.; Hong, Y.; Labarthe, D.; Mozaffarian, D.; Appel, L.J.; van Horn, L.; Greenlund, K.; Daniels, S.; Nichol, G.; Tomaselli, G.F.; On behalf of the American Strategic Planning Task Force and Statistics Committee ; et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association’s Strategic Impact Goal through 2020 and beyond. Circulation 2010, 121, 586–613. [Google Scholar] [CrossRef]
- Ghanbarzadeh, M.; Mohamadi, A. Aerobic exercise on mental health of prisoner people. JPES 2012, 12, 217–221. [Google Scholar]
- Perez, F. Programa de adherenciaal ejercicio fisico, dirigido a usuarios de Programas de Mantenimiento con Metadona (PMM). Rev. Esp. Sanid. Penit. 2002, 4, 114–117. [Google Scholar]
- Kraemer, W.J.; Adams, K.; Cafarelli, E.; Dudey, G.; Dody, C.; Faigenbaum, M.S.; Fleck, S.J.; Franklin, B.; Fry, A.C.; Newton, R.U.; Potteigr, J.; Stone, M.H; Ratamess, N.N.; McBride, T.T. American College of Sports Medicine position stand: Progression models in resistance training for healthy adults. Med. Sci. Sports Exerc. 2002, 34, 36–380. [Google Scholar] [CrossRef]
- Lohman, T.G.; Roche, A.F.; Matorell, L.R. Anthropometric Standardization Reference Manual; Human Kinetics: Champaign, IL, USA, 1988. [Google Scholar]
- Parameswaran, G.I.; Brand, K.; Dolan, J. Pulse oximetry as a potential screening tool for lowerextremity arterial disease in asymptomatic patients with diabetes mellitus. Arch. Intern. Med. 2005, 165, 442–446. [Google Scholar] [CrossRef]
- Mendelson, Y. Pulse oximetry: Theory and applications for noninvasive monitoring. Clin. Chem. 1992, 38, 1601–1607. [Google Scholar]
- Friedewald, W.T.; Levy, R.I.; Fredrickson, D.S. Estimation of the concentration oflow-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin. Chem. 1972, 18, 499–502. [Google Scholar]
- Lemieux, I.; Laperriere, L.; Dzavik, V.; Tremblay, G.; Bourgeois, J.; Despres, J.P. A 16-week fenofibrate treatment increases LDL particle size in type IIA dyslipidemic patients. Atherosclerosis 2002, 162, 363–371. [Google Scholar] [CrossRef]
- Siconolfi, S.F.; Garber, C.E.; Lasater, T.M.; Carleton, R.A. A simple, valid step test for estimating maximal oxygen uptake in epidemiologic studies. Am. J. Epidemiol. 1985, 121, 382–390. [Google Scholar]
- Van Hees, L.; Lefevre, J.; Philippaerts, R.; Martens, M.; Huygens, W.; Troosters, T.; Beunen, G. How to assess physical activity? How to assess physical fitness? Eur. J. Cardiovasc. Prev. Rehabil. 2005, 12, 102–114. [Google Scholar]
- Golding, L.A. YMCA Fitness and Assessment Manual; Human Kinetics: Champaign, IL, USA, 2000. [Google Scholar]
- Cooper Institute. Physical Fitness Assessments and Norms; The Cooper Institute: Dallas, TX, USA, 2005. [Google Scholar]
- Osness, W.H.; Adrian, M.; Clark, B.; Hoeger, W.; Raab, D.; Wisnell, R. Functional Fitness Assessment for Adults Over 60 Years (A Field Based Assessment); American Alliance for Health, Physical Education Recreation and Dance (AAHPRED): Reston, VA, USA, 1990. [Google Scholar]
- Stewart, I.B.; Pickering, R.L. Effect of prolonged exercise on arterial oxygen saturation in athletes susceptible to exercise-induced hypoxemia. Scand. J. Med. Sci. Sports. 2007, 17, 445–451. Available online: http://eprints.qut.edu.au/view/person/Pickering,_Rachel.html(accessed (accessed on 19 June 2006). [Google Scholar]
- Attili, A.K.; Kazerooni, E.A.; Gross, B.H.; Flaherty, K.R.; Myers, J.L.; Martinez, F.J. Smoking-related interstitial lung disease: Radiologic-clinical-pathologic correlation. Radiographics 2008, 28, 1383–1396. [Google Scholar] [CrossRef]
- Haskell, W.L. The influence of exercise on the concentrations of triglyceride and cholesterol in human plasma. Exerc. Sport Sci. Rev. 1984, 12, 205–244. [Google Scholar] [CrossRef]
- Goldberg, L.; Elliot, D.L. The effect of physical activity on lipid and lipoprotein levels. Med. Clin. North Am. 1985, 69, 41–55. [Google Scholar]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.M.; Nieman, D.C.; Swain, D.P. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar]
- Lauer, M.S.; Okin, P.M.; Larson, M.G.; Evans, J.C.; Levy, D. Prognostic implications of chronotropic incompetence in the Framingham heart study. Circulation 1996, 93, 1520–1526. [Google Scholar] [CrossRef]
- Mazzetti, S.A.; Kraemer, W.J.; Volek, J.S.; Duncan, N.D.; Ratamess, N.A.; Gómez, A.L.; Newton, R.U.; Häkkinen, K.; Fleck, S.J. The influence of direct supervision of resistance training on strength performance. Med. Sci. Sports Exerc. 2000, 32, 1175–1184. [Google Scholar] [CrossRef]
- Dunn, A.L.; Trivedi, M.H.; Kampert, J.B.; Clark, C.G.; Chambliss, H.O. Exercise treatment for depression: Efficacy and dose response. Am. J. Prev. Med. 2005, 28, 1–8. [Google Scholar]
- Schlicht, J. Strength training for older adults: Prescription guidelines for nurses in advanced practice. J. Gerontol. Nurs. 2000, 26, 25–32. [Google Scholar]
- Swain, D.P.; Franklin, B.A. Comparison of cardioprotective benefits of vigorous versus moderate intensity aerobic exercise. Am. J. Cardiol. 2006, 97, 141–147. [Google Scholar] [CrossRef]
- Cashin, A.; Potter, E.; Stevens, W.; Davidson, K.; Muldoon, D. Fit for prison: Special population health and fitness programme evaluation. Int. J. Prison. Health. 2008, 4, 208–216. [Google Scholar] [CrossRef]
- Pate, R.R.; Pratt, M.; Blair, S.N.; Haskell, W.L.; Macera, C.A.; Bouchard, C.; Buchner, D.; Ettinger, W.; Heath, G.W.; King, A.C. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA 1995, 273, 402–407. [Google Scholar]
- Meek, R.; Lewis, G. The role of sport in promoting prisoner health. Int. J. Prison. Health 2012, 8, 117–130. [Google Scholar] [CrossRef]
- Amtmann, J. Physical activity and inmate health. Correct. Compend. 2001, 26, 6–9. [Google Scholar]
- Kelley, G.A.; Kelley, K.S.; Roberts, S.; Haskell, W. Efficacy of aerobic exercise and a prudent diet for improving selected lipids and lipoproteins in adults: A meta-analysis of randomized controlled trials. BMC Med. 2011, 9, 74. [Google Scholar] [CrossRef]
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Battaglia, C.; Di Cagno, A.; Fiorilli, G.; Giombini, A.; Fagnani, F.; Borrione, P.; Marchetti, M.; Pigozzi, F. Benefits of Selected Physical Exercise Programs in Detention: A Randomized Controlled Study. Int. J. Environ. Res. Public Health 2013, 10, 5683-5696. https://doi.org/10.3390/ijerph10115683
Battaglia C, Di Cagno A, Fiorilli G, Giombini A, Fagnani F, Borrione P, Marchetti M, Pigozzi F. Benefits of Selected Physical Exercise Programs in Detention: A Randomized Controlled Study. International Journal of Environmental Research and Public Health. 2013; 10(11):5683-5696. https://doi.org/10.3390/ijerph10115683
Chicago/Turabian StyleBattaglia, Claudia, Alessandra Di Cagno, Giovanni Fiorilli, Arrigo Giombini, Federica Fagnani, Paolo Borrione, Marco Marchetti, and Fabio Pigozzi. 2013. "Benefits of Selected Physical Exercise Programs in Detention: A Randomized Controlled Study" International Journal of Environmental Research and Public Health 10, no. 11: 5683-5696. https://doi.org/10.3390/ijerph10115683






