Short-Term Effects of Gaseous Pollutants and Particulate Matter on Daily Hospital Admissions for Cardio-Cerebrovascular Disease in Lanzhou: Evidence from a Heavily Polluted City in China
Abstract
:1. Introduction
2. Materials and Methods
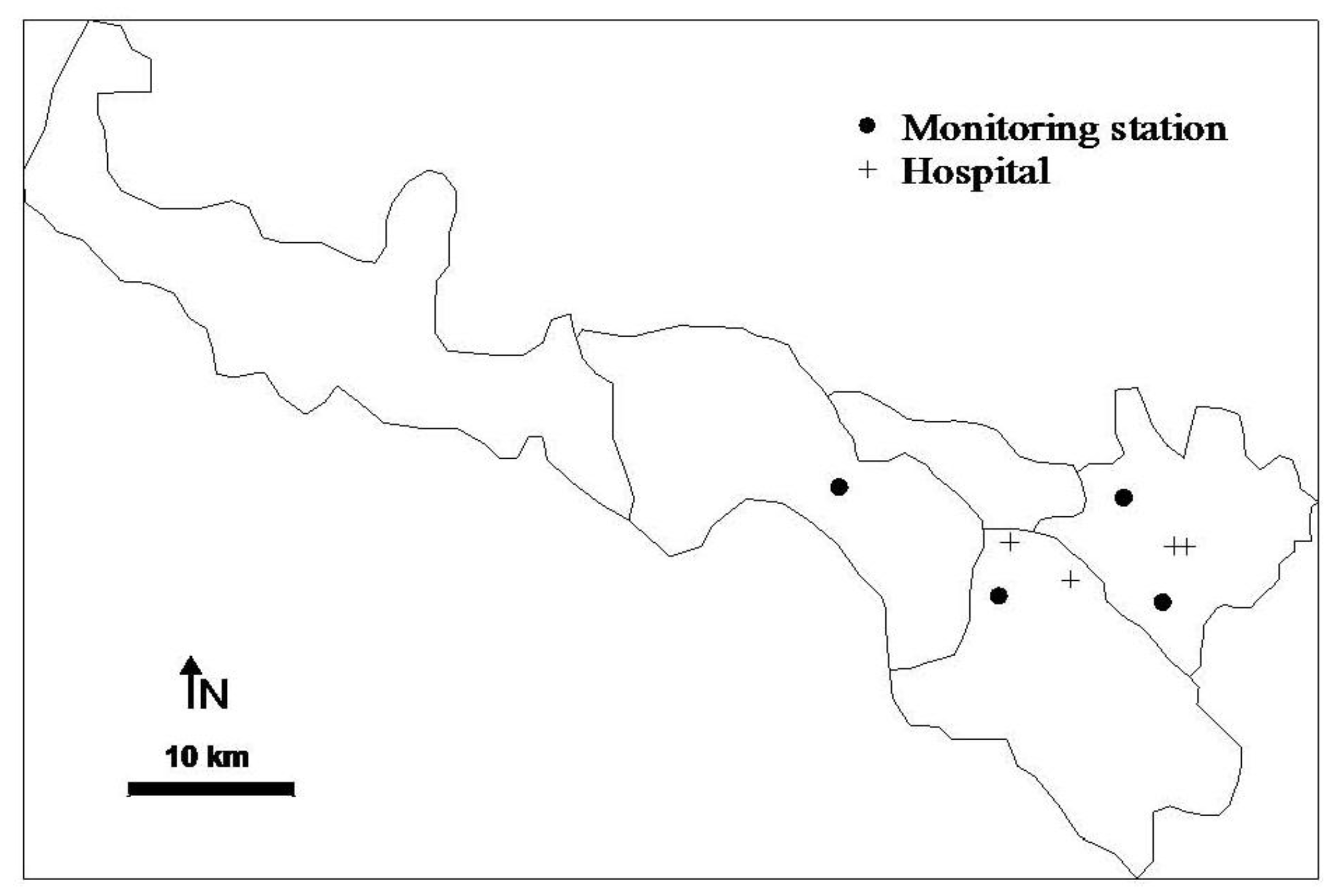
2.1. Data Collection
2.2. Statistical Methods
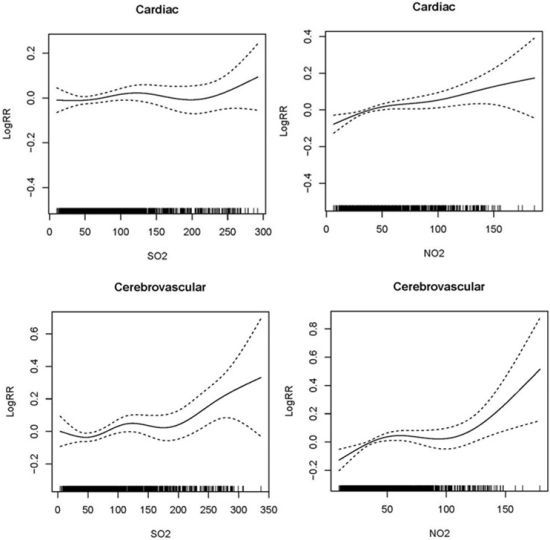
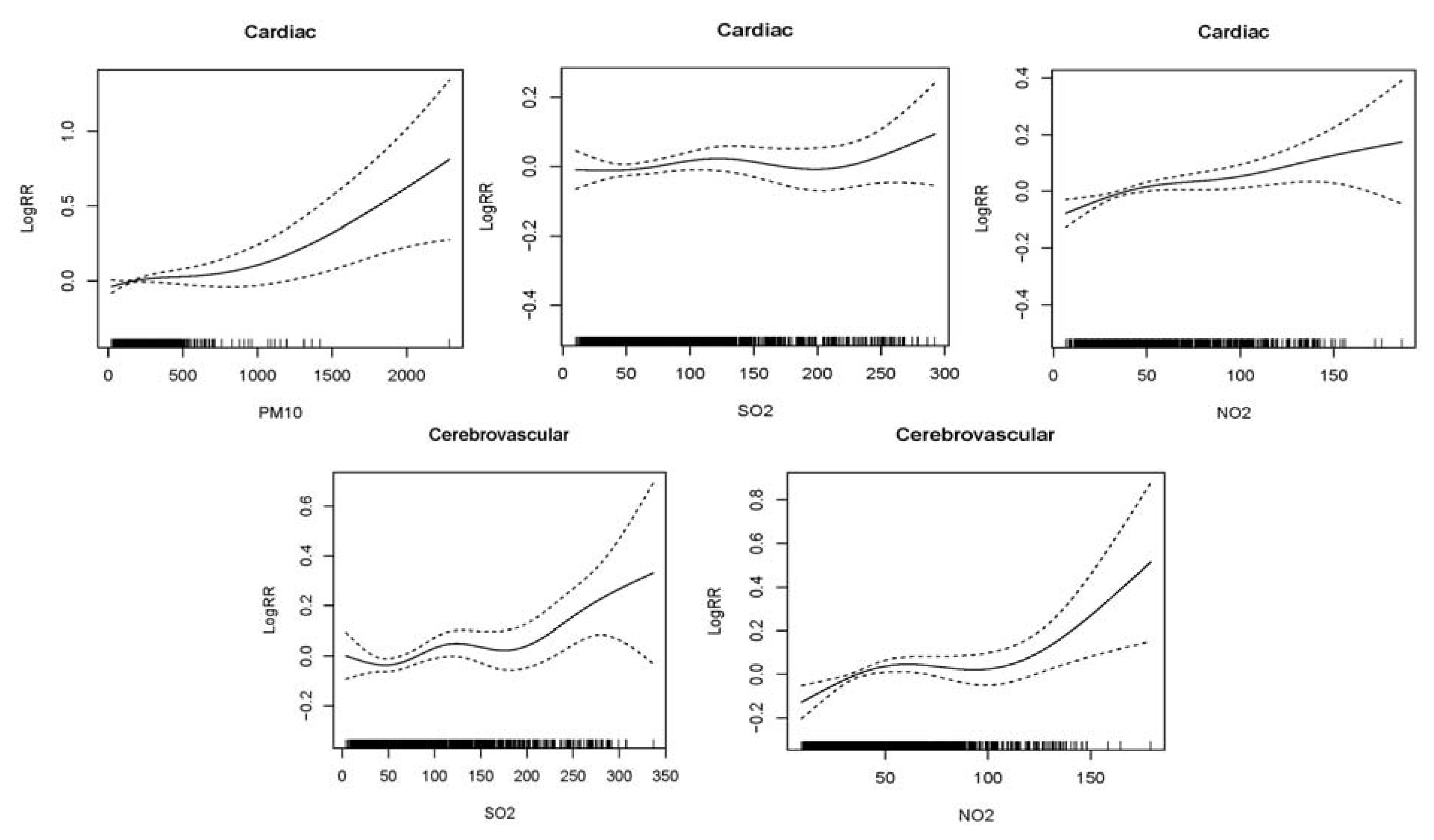
3. Results
| Mean | SD | Min | P25 | Median | P75 | Max | IQR | |
|---|---|---|---|---|---|---|---|---|
| Daily Hospital admissions | ||||||||
| Cardiac diseases | 9.65 | 5.64 | 0 | 5 | 9 | 13 | 36 | 8 |
| Cerebrovascular diseases | 5.82 | 3.88 | 0 | 3 | 5 | 8 | 23 | 5 |
| Meteorology measures | ||||||||
| Temperature (°C) | 11.08 | 9.92 | −12.20 | 2.10 | 11.90 | 20.00 | 30.10 | 17.90 |
| Relative humidity (%) | 50.46 | 14.03 | 15.90 | 40.20 | 50.70 | 60.30 | 89.80 | 20.1 |
| Air pollutants concentrations | ||||||||
| PM10 (μg/m3) | 187.07 | 125.78 | 16.00 | 101.00 | 148.00 | 235.00 | 2,561.00 | 134.00 |
| SO2 (μg/m3) | 79.11 | 61.43 | 2.00 | 37.00 | 58.00 | 106.00 | 371.00 | 69.00 |
| NO2 (μg/m3) | 45.81 | 29.30 | 4.00 | 25.00 | 37.50 | 56.00 | 260.00 | 31.00 |
| Cold season a | ||||||||
| PM10 (μg/m3) | 276.04 | 214.39 | 21.00 | 149.00 | 222.00 | 333.00 | 2561.00 | 184.00 |
| SO2 (μg/m3) | 114.87 | 66.76 | 6.00 | 65.00 | 100.00 | 148.00 | 371.00 | 83.00 |
| NO2 (μg/m3) | 58.78 | 33.15 | 4.00 | 35.00 | 50.00 | 75.00 | 260.00 | 40.00 |
| Warm season b | ||||||||
| PM10 (μg/m3) | 125.69 | 65.71 | 16.00 | 86.00 | 114.00 | 149.00 | 880.00 | 63.00 |
| SO2 (μg/m3) | 43.89 | 24.53 | 2.00 | 28.00 | 40.00 | 54.00 | 182.00 | 26.00 |
| NO2 (μg/m3) | 33.04 | 17.15 | 4.00 | 22.00 | 29.00 | 40.00 | 123.00 | 18.00 |
| Temperature | Relative humidity | PM10 | SO2 | |
|---|---|---|---|---|
| PM10 | −0.454 ** | −0.320 ** | ||
| SO2 | −0.585 ** | −0.296 ** | 0.624 ** | |
| NO2 | −0.465 ** | −0.218 ** | 0.643 ** | 0.640** |
| Lag structures | Cardiac diseases | Cerebrovascular diseases | |||
|---|---|---|---|---|---|
| Change % (95%CI) | P value | Change % (95%CI) | P value | ||
| PM10 | Single-day lag | ||||
| 0 | 1.28 (−0.21~2.80) | 0.09 | −0.77 (−3.44~1.97) | 0.58 | |
| 1 | 1.66 (0.13~3.20) | 0.03 | −1.43 (−3.64~0.83) | 0.21 | |
| 2 | 1.54 (0.06~3.05) | 0.04 | −1.38 (−3.47~0.76) | 0.20 | |
| 3 | −0.25 (−1.66~1.19) | 0.74 | −1.50 (−3.45~0.50) | 0.14 | |
| Cumulative-day lag | |||||
| 01 | 2.32 (0.55~4.12) | 0.01 | −1.72 (−4.60~1.25) | 0.25 | |
| 02 | 2.13 (0.15~4.15) | 0.03 | −2.39 (−5.43~0.75) | 0.13 | |
| 03 | 0.91 (−1.19~3.06) | 0.40 | −3.01 (−6.12~0.21) | 0.18 | |
| SO2 | Single-day lag | ||||
| 0 | 2.34 (0.23~4.49) | 0.03 | 3.80 (0.63~7.08) | 0.02 | |
| 1 | 0.81 (−1.27~2.92) | 0.45 | 4.03 (0.87~7.29) | 0.01 | |
| 2 | 1.82 (−0.26~3.95) | 0.09 | 4.26 (1.07~7.55) | 0.01 | |
| 3 | 1.24 (−0.85~3.38) | 0.25 | 3.09 (−0.09~6.37) | 0.06 | |
| Cumulative-day lag | |||||
| 01 | 1.98 (−0.31~4.32) | 0.09 | 4.71 (1.23~8.30) | 0.01 | |
| 02 | 2.29 (−0.11~4.76) | 0.06 | 5.40 (1.72~9.23) | <0.00 | |
| 03 | 2.29 (−0.21~4.86) | 0.07 | 5.53 (1.69~9.53) | <0.00 | |
| NO2 | Single-day lag | ||||
| 0 | 3.47 (1.67~5.30) | <0.00 | 4.06 (1.36~6.84) | <0.00 | |
| 1 | 2.68 (0.87~4.52) | <0.00 | 3.26 (0.56~6.04) | 0.02 | |
| 2 | 2.43 (0.60~4.29) | 0.01 | 2.43 (−0.29~5.22) | 0.08 | |
| 3 | 1.42 (−0.39~3.27) | 0.13 | 3.04 (0.30~5.86) | 0.03 | |
| Cumulative-day lag | |||||
| 01 | 3.78 (1.80~5.80) | <0.00 | 4.39 (1.43~7.43) | <0.00 | |
| 02 | 3.94 (1.83~6.09) | <0.00 | 4.40 (1.25~7.64) | 0.01 | |
| 03 | 3.77 (1.55~6.03) | <0.00 | 4.76 (1.45~8.19) | <0.00 | |
| Cardiac diseases | Cerebrovascular diseases | ||||||
|---|---|---|---|---|---|---|---|
| n a | Change % (95%CI) | p value | N a | Change % (95%CI) | p value | ||
| Gender | |||||||
| Male | PM10 | 5.94 | 2.05 (−0.17~4.32) | 0.07 | 3.79 | −0.21 (−3.47~3.17) | 0.90 |
| SO2 | 2.33 (−0.72~5.49) | 0.14 | 6.47 (2.41~10.68) | <0.00 | |||
| NO2 | 3.64 (0.54~6.84) | 0.02 | 4.45 (0.38~8.68) | 0.03 | |||
| Female | PM10 | 3.71 | 2.99 (0.10~5.96) | 0.04 | 2.03 | −3.72 (−8.39~1.19) | 0.14 |
| SO2 | 5.82 (1.63~10.17) | 0.01 | 2.65 (−3.53~9.24) | 0.41 | |||
| NO2 | 6.25 (1.98~10.70) | <0.00 | 6.06 (0.47~11.95) | 0.03 | |||
| Age | |||||||
| <65 | PM10 | 4.15 | 2.19 (−0.35~4.80) | 0.09 | 2.98 | −0.65 (−4.39~3.25) | 0.74 |
| SO2 | 2.82 (−0.41~6.16) | 0.09 | 3.97 (−1.32~9.55) | 0.14 | |||
| NO2 | 3.04 (−0.15~6.33) | 0.06 | 2.92 (−1.44~7.47) | 0.19 | |||
| ≥65 | PM10 | 5.50 | 2.47 (0.03~4.98) | 0.04 | 2.84 | −1.98 (−5.79~1.98) | 0.32 |
| SO2 | 2.05 (−0.69~4.86) | 0.14 | 6.15 (0.77~11.83) | 0.02 | |||
| NO2 | 4.60 (1.83~7.45) | <0.00 | 5.85 (1.15~10.78) | 0.01 | |||
| Season a | Cardiac diseases | Cerebrovascular diseases | ||||
|---|---|---|---|---|---|---|
| n b | Change % (95%CI) | p value | n b | Change % (95%CI) | p value | |
| Cold season | ||||||
| PM10 | 9.72 | 7.92 (1.91~14.30) | 0.01 | 5.58 | −4.67 (−13.0~4.58) | 0.31 |
| SO2 | 2.02 (−0.21~4.29) | 0.08 | 5.76 (1.65~10.04) | 0.01 | ||
| NO2 | 2.94 (0.68~5.25) | 0.01 | 4.58 (1.02~8.27) | 0.01 | ||
| Warm season | ||||||
| PM10 | 9.59 | 5.81 (−0.20~12.18) | 0.06 | 6.06 | −2.90 (−6.11~0.41) | 0.08 |
| SO2 | 1.97 (−3.82~8.10) | 0.51 | 2.81 (−7.84~14.68) | 0.62 | ||
| NO2 | 8.41 (3.69~13.34) | <0.00 | 5.39 (−1.74~13.03) | 0.14 | ||
| Models | Cardiac diseases | Cerebrovascular diseases | ||
|---|---|---|---|---|
| Change % (95%CI) | p value | Change % (95%CI) | p value | |
| PM10 | 2.13 (0.15~4.15) | 0.03 | −2.39 (−5.43~0.75) | 0.13 |
| + SO2 | 1.97 (−0.03~4.01) | 0.05 | −1.84 (−4.88~1.29) | 0.25 |
| + NO2 | 1.27 (−0.80~3.38) | 0.23 | −2.10 (−5.14~1.05) | 0.19 |
| + SO2+ NO2 | 1.27 (−0.80~3.38) | 0.23 | −2.04 (−5.10~1.12) | 0.20 |
| SO2 | 2.29 (−0.11~4.76) | 0.06 | 5.40 (1.72~9.23) | <0.00 |
| + PM10 | 2.58 (−0.29~5.54) | 0.08 | 8.52 (4.65~12.53) | <0.00 |
| + NO2 | −0.24 (−3.57~3.22) | 0.89 | 5.82 (1.34~10.50) | 0.01 |
| + PM10+ NO2 | −0.05 (−3.45~3.46) | 0.98 | 5.86 (1.37~10.54) | 0.01 |
| NO2 | 3.94 (1.83~6.09) | <0.00 | 4.40 (1.25~7.64) | 0.01 |
| + PM10 | 4.16 (1.55~6.84) | <0.00 | 6.97 (3.59~10.46) | <0.00 |
| + SO2 | 4.71 (1.64~7.88) | <0.00 | 4.00 (0.08~8.07) | 0.04 |
| + PM10+ SO2 | 4.18 (1.02~7.45) | 0.01 | 4.82 (0.81~8.98) | 0.02 |
4. Conclusions
Acknowledgments
Conflict of Interest
References
- WHO. Cause of Death. Available online: http://www.who.int/healthinfo/global_burden_disease/cod_2008_sources_methods.pdf (accessed on 25 December 2012).
- He, J.; Gu, D.; Wu, X.; Reynolds, K.; Duan, X.; Yao, C.; Wang, J.; Chen, C.-S.; Chen, J.; Wildman, R.P.; et al. Major causes of death among men and women in China. N. Engl. J. Med. 2005, 353, 1124–1134. [Google Scholar] [CrossRef]
- Larrieu, S.; Jusot, J.-F.; Blanchard, M.; Prouvost, H.L.N.; Declercq, C.; Fabre, P.; Pascal, L.; Tertre, A.L.; Wagner, V.R.N.; Rivie’re, S.P.; et al. Short term effects of air pollution on hospitalizations for cardiovascular diseases in eight French cities: The psas program. Sci. Total Envir. 2007, 387, 105–112. [Google Scholar]
- Wong, C.M.; Atkinson, R.W.; Anderson, H.R.; Hedley, A.J.; Ma, S.; Chau, P.Y.; Lam, T.H. A tale of two cities: Effects of air pollution on hospital admissions in Hong Kong and London compared. Environ. Health Perspect. 2002, 110, 67–77. [Google Scholar]
- Wong, C.-M.; Vichit-Vadakan, N.; Kan, H.; Qian, Z. Public health and air pollution in Asia (PAPA): A multicity study of short-term effects of air pollution on mortality. Environ. Health Perspect. 2008, 116, 1195–1202. [Google Scholar] [CrossRef]
- Sunyer, J.; Ballester, F.; Tertre, A.L.; Atkinson, R.; Ayres, J.G.; Forastiere, F.; Forsberg, B.; Vonk, J.M.; Bisanti, L.; Tenías, J.M.; et al. The association of daily sulfur dioxide air pollution levels with hospital admissions for cardiovascular diseases in Europe (the Aphea-II study). Eur. Heart J. 2003, 24, 752–760. [Google Scholar]
- Ballester, F.; Rodriguez, P.; Iniguez, C.; Saez, M.; Daponte, A.; Galan, I.; Taracido, M.; Arribas, F.; Bellido, J.; Cirarda, F.B.; et al. Air pollution and cardiovascular admissions association in Spain: Results within the emecas project. J. Epidemiol. Community Health 2006, 60, 328–336. [Google Scholar]
- Barnett, A.G.; Williams, G.M.; Schwartz, J.; Best, T.L.; Neller, A.H.; Petroeschevsky, A.L.; Simpson, R.W. The effects of air pollution on hospitalizations for cardiovascular disease in elderly people in australian and New Zealand cities. Environ. Health Perspect. 2006, 114, 1018–1023. [Google Scholar]
- Poloniecki, J.D.; Atkinson, R.W.; de Leon, A.P.; Anderson, H.R. Daily time series for cardiovascular hospital admissions and previous day’s air pollution in London, UK. Occup. Environ. Med. 1997, 54, 535–540. [Google Scholar] [CrossRef]
- Chang, C.-C.; Tsai, S.-S.; Ho, S.-C.; Yang, C.-Y. Air pollution and hospital admissions for cardiovascular disease in Taipei, Taiwan. Environ. Res. 2005, 98, 114–119. [Google Scholar] [CrossRef]
- Guo, Y.; Jia, Y.; Pan, X.; Liu, L.; Wichmann, H.E. The association between fine particulate air pollution and hospital emergency room visits for cardiovascular diseases in Beijing, China. Sci. Total Environ. 2009, 407, 4826–4830. [Google Scholar] [CrossRef]
- Pan, X.; Yang, M.; Fan, T. Time-series analysis of air pollution and cardiovascular mortality in Beijing, China. Epidemiology 2008, 19, S170–S171. [Google Scholar]
- Kan, H.; Chen, B. A case-crossover analysis of air pollution and daily mortality in Shanghai. J. Occup. Health 2003, 45, 119–124. [Google Scholar] [CrossRef]
- Chen, R.; Chu, C.; Tan, J.; Cao, J.; Song, W.; Xu, X.; Jiang, C.; Ma, W.; Yang, C.; Chen, B.; et al. Ambient air pollution and hospital admission in Shanghai, China. J. Hazard. Mater. 2010, 181, 234–240. [Google Scholar] [CrossRef]
- Guo, Y.; Barnett, A.G.; Zhang, Y.; Tong, S.; Yu, W.; Pan, X. The short-term effect of air pollution on cardiovascular mortality in Tianjin, China: Comparison of time series and case-crossover analyses. Sci. Total Envir. 2010, 409, 300–306. [Google Scholar] [CrossRef]
- Xu, Z.; Yu, D.; Jing, L.; Xu, X. Air pollution and daily mortality in Shenyang, China. Arch. Environ. Health 2000, 55, 115–120. [Google Scholar] [CrossRef]
- Qi, B.; Zhang, Z.; Zhu, X.; Ma, M.; Ding, X. Environment and atmospheric pollution. Gansu Province, China. Gansu Nationality Press 2001, 200–252. (In Chinese). [Google Scholar]
- WHO. Urban Outdoor Air pollution Database. Available online: http://www.who.int/phe/health_topics/outdoorair/databases/en/index.html (accessed on 10 August 2012).
- Kan, H.; Chen, B.; Hong, C. Health impact of outdoor air pollution in china: Current knowledge and future research needs. Environ. Health Perspect. 2009, 117, A187. [Google Scholar]
- Samoli, E.; Analitis, A.; Touloumi, G.; Schwartz, J.; Anderson, H.R.; Sunyer, J.; Bisanti, L.; Zmirou, D.; Vonk, J.M.; Pekkanen, J.; et al. Estimating the exposure-response relationships between particulate matter and mortality within the Aphea multicity project. Environ. Health Perspect. 2005, 113, 88–95. [Google Scholar]
- Cao, J.; Li, W.; Tan, J.; Song, W.; Xu, X.; Jiang, C.; Chen, G.; Chen, R.; Ma, W.; Chen, B.; et al. Association of ambient air pollution with hospital outpatient and emergency room visits in Shanghai, China. Sci. Total Envir. 2009, 407, 5531–5536. [Google Scholar] [CrossRef]
- Ren, C.; Williams, G.M.; Tong, S. Does particulate matter modify the association between temperature and cardiorespiratory diseases? Environ. Health Perspect. 2006, 114, 1690–1696. [Google Scholar]
- Hastie, T.; Tibshirani, R. Generalized additive models for medical research. Stat. Methods Med. Res. 1995, 4, 187–196. [Google Scholar]
- Ren, C.; Williams, G.M.; Mengersen, K.; Morawska, L.; Tong, S. Does temperature modify short-term effects of ozone on total mortality in 60 large eastern us communities?—An assessment using the nmmaps data. Environ. Int. 2008, 34, 451–458. [Google Scholar] [CrossRef]
- Zhang, F.; Li, L.; Krafft, T.; Lv, J.; Wang, W.; Pei, D. Study on the association between ambient air pollution and daily cardiovascular and respiratory mortality in an urban district of Beijing. Int J. Environ. Res. Public Health 2011, 8, 2109–2123. [Google Scholar] [CrossRef]
- Yu, I.T.S.; Zhang, Y.H.; San Tam, W.W.; Yan, Q.H.; Xu, Y.J.; Xun, X.J.; Wu, W.; Ma, W.J.; Tian, L.W.; Tse, L.A.; et al. Effect of ambient air pollution on daily mortality rates in Guangzhou, China. Atmos. Environ. 2012, 46, 528–535. [Google Scholar] [CrossRef]
- Chen, R.; Li, Y.; Ma, Y.; Pan, G.; Zeng, G.; Xu, X.; Chen, B.; Kan, H. Coarse particles and mortality in three chinese cities: The China air pollution and health effects study (capes). Sci. Total Environ. 2011, 409, 4934–4938. [Google Scholar] [CrossRef]
- Dominici, F.; Peng, R.D.; Bell, M.L.; Pham, L.; McDermott, A.; Zeger, S.L.; Samet, J.M. Fine particulate air pollution and hospital admission for cardiovascular and respiratory diseases. JAMA 2006, 295, 1127–1134. [Google Scholar] [CrossRef]
- Ballester, F.; Tenias, J.M.; Perez-Hoyos, S. Air pollution and emergency hospital admissions for cardiovascular diseases in Valencia, Spain. J. Epidemiol Community Health 2001, 55, 57–65. [Google Scholar] [CrossRef]
- Le Tertre, A.; Medina, S.; Samoli, E.; Forsberg, B.; Michelozzi, P.; Boumghar, A.; Vonk, J.M.; Bellini, A.; Atkinson, R.; Ayres, J.G.; et al. Short-term effects of particulate air pollution on cardiovascular diseases in eight European cities. J. Epidemiol. Community Health 2002, 56, 773–779. [Google Scholar] [CrossRef]
- Wellenius, G.A.; Schwartz, J.; Mittleman, M.A. Air pollution and hospital admissions for ischemic and hemorrhagic stroke among medicare beneficiaries. Stroke 2005, 36, 2549–2553. [Google Scholar] [CrossRef]
- Tsai, S.-S.; Goggins, W.B.; Chiu, H.-F.; Yang, C.-Y. Evidence for an association between air pollution and daily stroke admissions in Kaohsiung, Taiwan. Stroke 2003, 34, 2612–2616. [Google Scholar] [CrossRef]
- Schwartz, J. Air pollution and blood markers of cardiovascular risk. Environ. Health Perspect. 2001, 109 Suppl 3, 405–409. [Google Scholar]
- Peters, A.; Doring, A.; Wichmann, H.E.; Koenig, W. Increased plasma viscosity during an air pollution episode: A link to mortality? Lancet 1997, 349, 1582–1587. [Google Scholar]
- Seaton, A.; Soutar, A.; Crawford, V.; Elton, R.; McNerlan, S.; Cherrie, J.; Watt, M.; Agius, R.; Stout, R. Particulate air pollution and the blood. Thorax 1999, 54, 1027–1032. [Google Scholar] [CrossRef]
- Wong, T.W.; Lau, T.S.; Yu, T.S.; Neller, A.; Wong, S.L.; Tam, W.; Pang, S.W. Air pollution and hospital admissions for respiratory and cardiovascular diseases in hong kong. Occup. Environ. Med. 1999, 56, 679–683. [Google Scholar] [CrossRef]
- Guo, Y.; Tong, S.; Li, S.; Barnett, A.; Yu, W.; Zhang, Y.; Pan, X. Gaseous air pollution and emergency hospital visits for hypertension in Beijing, China: A time-stratified case-crossover study. Environ. Health 2010, 9, No. 57. [Google Scholar] [CrossRef]
- Etlik, O.; Tomur, A.; Kutman, M.N.; Yorukan, S.; Duman, O. The effects of sulfur dioxide inhalation and antioxidant vitamins on red blood cell lipoperoxidation. Environ. Res. 1995, 71, 25–28. [Google Scholar] [CrossRef]
- de Paula Santos, U.; Braga, A.L.; Giorgi, D.M.; Pereira, L.A.; Grupi, C.J.; Lin, C.A.; Bussacos, M.A.; Zanetta, D.M.; do Nascimento Saldiva, P.H.; Filho, M.T. Effects of air pollution on blood pressure and heart rate variability: A panel study of vehicular traffic controllers in the city of Sao Paulo, Brazil. Eur. Heart J. 2005, 26, 193–200. [Google Scholar]
- Routledge, H.C.; Manney, S.; Harrison, R.M.; Ayres, J.G.; Townend, J.N. Effect of inhaled sulphur dioxide and carbon particles on heart rate variability and markers of inflammation and coagulation in human subjects. Heart 2006, 92, 220–227. [Google Scholar] [CrossRef]
- Ta, W.; Wang, T.; Xiao, H.; Zhu, X.; Xiao, Z. Gaseous and particulate air pollution in the Lanzhou valley, China. Sci. Total Envir. 2004, 320, 163–176. [Google Scholar] [CrossRef]
- Pekkanen, J.; Brunner, E.J.; Anderson, H.R.; Tiittanen, P.; Atkinson, R.W. Daily concentrations of air pollution and plasma fibrinogen in London. Occup. Environ. Med. 2000, 57, 818–822. [Google Scholar] [CrossRef]
- Santos, U.P.; Terra-Filho, M.; Lin, C.A.; Pereira, L.A.; Vieira, T.C.; Saldiva, P.H.; Braga, A.L. Cardiac arrhythmia emergency room visits and environmental air pollution in Sao Paulo, Brazil. J. Epidemiol. Commun. Health 2008, 62, 267–272. [Google Scholar] [CrossRef]
- Chan, C.C.; Chuang, K.J.; Su, T.C.; Lin, L.Y. Association between nitrogen dioxide and heart rate variability in a susceptible population. Eur. J. Cardiovasc. Prev. Rehabil. 2005, 12, 580–586. [Google Scholar]
- de Sousa, M.R.; Barbosa, M.P.; Lombardi, F.; Ribeiro, A.L. Standard deviation of normal interbeat intervals as a risk marker in patients with left ventricular systolic dysfunction: A meta-analysis. Int. J. Cardiol. 2010, 141, 313–316. [Google Scholar] [CrossRef]
- Kan, H.; London, S.J.; Chen, G.; Zhang, Y.; Song, G.; Zhao, N.; Jiang, L.; Chen, B. Season, sex, age, and education as modifiers of the effects of outdoor air pollution on daily mortality in Shanghai, China: The public health and air pollution in Asia (PAPA) study. Environ. Health Perspect. 2008, 116, 1183–1188. [Google Scholar] [CrossRef]
- Chu, P.C.; Chen, Y.; Lu, S.; Li, Z.; Lu, Y. Particulate air pollution in lanzhou china. Environ. Int. 2008, 34, 698–713. [Google Scholar] [CrossRef]
- Qian, Z.; He, Q.; Lin, H.M.; Kong, L.; Bentley, C.M.; Liu, W.; Zhou, D. High temperatures enhanced acute mortality effects of ambient particle pollution in the “oven” city of Wuhan, China. Environ. Health Perspect. 2008, 116, 1172–1178. [Google Scholar] [CrossRef]
- Zeger, S.L.; Thomas, D.; Dominici, F.; Samet, J.M.; Schwartz, J.; Dockery, D.; Cohen, A. Exposure measurement error in time-series studies of air pollution: Concepts and consequences. Environ. Health Perspect. 2000, 108, 419–426. [Google Scholar] [CrossRef]
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Zheng, S.; Wang, M.; Wang, S.; Tao, Y.; Shang, K. Short-Term Effects of Gaseous Pollutants and Particulate Matter on Daily Hospital Admissions for Cardio-Cerebrovascular Disease in Lanzhou: Evidence from a Heavily Polluted City in China. Int. J. Environ. Res. Public Health 2013, 10, 462-477. https://doi.org/10.3390/ijerph10020462
Zheng S, Wang M, Wang S, Tao Y, Shang K. Short-Term Effects of Gaseous Pollutants and Particulate Matter on Daily Hospital Admissions for Cardio-Cerebrovascular Disease in Lanzhou: Evidence from a Heavily Polluted City in China. International Journal of Environmental Research and Public Health. 2013; 10(2):462-477. https://doi.org/10.3390/ijerph10020462
Chicago/Turabian StyleZheng, Shan, Minzhen Wang, Shigong Wang, Yan Tao, and Kezheng Shang. 2013. "Short-Term Effects of Gaseous Pollutants and Particulate Matter on Daily Hospital Admissions for Cardio-Cerebrovascular Disease in Lanzhou: Evidence from a Heavily Polluted City in China" International Journal of Environmental Research and Public Health 10, no. 2: 462-477. https://doi.org/10.3390/ijerph10020462
APA StyleZheng, S., Wang, M., Wang, S., Tao, Y., & Shang, K. (2013). Short-Term Effects of Gaseous Pollutants and Particulate Matter on Daily Hospital Admissions for Cardio-Cerebrovascular Disease in Lanzhou: Evidence from a Heavily Polluted City in China. International Journal of Environmental Research and Public Health, 10(2), 462-477. https://doi.org/10.3390/ijerph10020462