Surveillance of Hospital Contacts among Danish Seafarers and Fishermen with Focus on Skin and Infectious Diseases—A Population-Based Cohort Study
Abstract
:1. Introduction
2. Experimental Section
2.1. General Information and Time Periods
2.2. Occupational Hospitalization Register
2.3. Inclusion Criteria for the Occupational Cohorts
2.4. Follow-Up of Diagnoses in the Occupational Hospitalization Register
2.5. Sub-Analyses
2.6. Statistical Analyses
3. Results and Discussion
3.1. Study Population
| Characteristics | Job Type 2 | Baseline 1994 | Baseline 1999 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number | Mean Age 3 | Vital Status | Number | Mean Age 3 | Vital Status | |||||||||
| N | Years | Alive 4 | Emigrated 5 | N | years | Alive 4 | Emigrated 5 | |||||||
| N | % | N | % | N | % | N | % | |||||||
| Men | ||||||||||||||
| Fishermen | Fishermen | 4570 | 37.2 ± 9.8 | 4468 | 97.8 | 58 | 1.3 | 3470 | 39.5 ± 10.1 | 3397 | 97.9 | 45 | 1.3 | |
| Seafarers | Officers | 5061 | 40.2 ± 10.0 | 4942 | 97.7 | 167 | 3.3 | 5375 | 41.3 ± 10.2 | 5253 | 97.7 | 165 | 3.1 | |
| Non-officers | 5170 | 35.0 ± 11.1 | 5037 | 97.4 | 192 | 3.7 | 5867 | 37.2 ± 11.4 | 5731 | 97.7 | 171 | 2.9 | ||
| Women | ||||||||||||||
| Seafarers | Officers | 90 | 32.8 ± 7.5 | 88 | 97.8 | 6 | 6.7 | 100 | 31.3 ± 7.3 | 100 | 100 | 4 | 4.0 | |
| Non-officers | 1762 | 31.6 ± 9.4 | 1752 | 99.4 | 53 | 3.0 | 2494 | 33.7 ± 10.5 | 2475 | 99.2 | 65 | 2.6 | ||
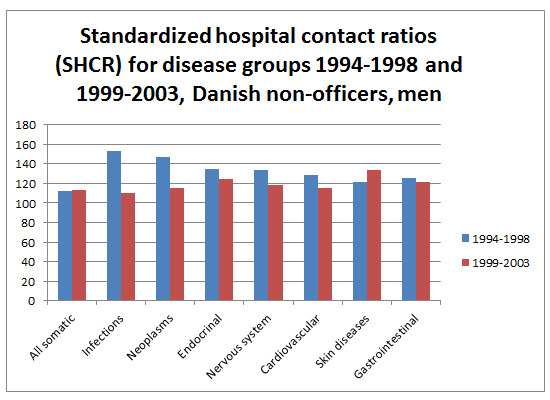
3.2. Standardized Hospital Contact Ratios for Overall ICD-10 Disease Groups by Gender, Job Type, and Time Period, with a Follow-up of Five or Seven Years
| ICD-10 1 | Site | Job Type | 1994–1998 | 1999–2003 | Trend 2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cases | SHCR | 95% CI | Cases | SHCR | 95% CI | SHCR Ratio | 95% CI | |||
| A00-B99 | Infectious diseases | Fishermen | 51 | 77 | 58–102 | 58 | 101 | 77–131 | 1.31 | 0.90–1.90 |
| A00-B99 | Officers | 69 | 99 | 77–126 | 85 | 98 | 78–121 | 0.98 | 0.72–1.35 | |
| A00-B99 | Non-officers | 119 | 153 | 128–183 | 111 | 110 | 92–133 | 0.72 | 0.56–0.93 | |
| C00-D48 | Neoplastic diseases | Fishermen 3 | 120 | 120 | 100–144 | 103 | 115 | 95–140 | 0.96 | 0.74–1.25 |
| C00-D48 | Officers 3 | 177 | 135 | 116–156 | 158 | 104 | 89–121 | 0.77 | 0.62–0.95 | |
| C00-D48 | Non-officers 3 | 157 | 147 | 126–172 | 162 | 115 | 99–135 | 0.78 | 0.63–0.98 | |
| D50-D89 | Lymphohematopoietic diseases | Fishermen | 4 | 35 | 10–90 | 14 | 123 | 67–206 | 3.47 | 1.14–10.55 |
| D50-D89 | Officers | 13 | 94 | 50–161 | 23 | 121 | 77–182 | 1.29 | 0.65–2.54 | |
| D50-D89 | Non-officers | 9 | 74 | 34–141 | 18 | 99 | 59–157 | 1.33 | 0.60–2.97 | |
| E00-E90 | Endocrinal and nutritional diseases | Fishermen 3 | 40 | 67 | 48–92 | 44 | 82 | 59–110 | 1.21 | 0.79–1.86 |
| E00-E90 | Officers 3 | 71 | 97 | 76–122 | 98 | 111 | 90–135 | 1.15 | 0.84–1.55 | |
| E00-E90 | Non-officers 3 | 82 | 135 | 107–167 | 102 | 124 | 102–150 | 0.92 | 0.69–1.23 | |
| G00-G99 | Diseases of the nervous system | Fishermen | 120 | 152 | 127–182 | 105 | 144 | 119–175 | 0.95 | 0.73–1.23 |
| G00-G99 | Officers | 86 | 92 | 73–113 | 94 | 80 | 65–98 | 0.88 | 0.65–1.18 | |
| G00-G99 | Non-officers | 111 | 134 | 111–161 | 136 | 118 | 100–140 | 0.88 | 0.69–1.13 | |
| H00-H59 | Diseases of the eye/ eye surroundings | Fishermen | 62 | 65 | 50–84 | 55 | 62 | 47–81 | 0.95 | 0.66–1.37 |
| H00-H59 | Officers | 63 | 59 | 45–75 | 107 | 77 | 64–93 | 1.31 | 0.96–1.78 | |
| H00-H59 | Non-officers | 104 | 96 | 79–116 | 152 | 103 | 87–120 | 1.07 | 0.83–1.37 | |
| H60-H95 | Diseases of the ear/ proc mastoideus | Fishermen | 71 | 87 | 68–109 | 78 | 101 | 80–126 | 1.16 | 0.84–1.60 |
| H60-H95 | Officers | 97 | 91 | 73–110 | 124 | 93 | 78–111 | 1.03 | 0.79–1.34 | |
| H60-H95 | Non-officers | 69 | 78 | 61–99 | 125 | 101 | 85–121 | 1.29 | 0.96–1.73 | |
| I00-I99 | Cardiovascular diseases | Fishermen 3 | 228 | 105 | 92–120 | 221 | 106 | 93–121 | 1.01 | 0.84–1.21 |
| I00-I99 | Officers 3 | 277 | 96 | 85–108 | 348 | 98 | 88–108 | 1.02 | 0.87–1.20 | |
| I00-I99 | Non-officers 3 | 286 | 129 | 115–145 | 366 | 115 | 103–127 | 0.89 | 0.76–1.04 | |
| J00-J99 | Respiratory diseases | Fishermen 3 | 150 | 105 | 89–123 | 129 | 111 | 94–132 | 1.06 | 0.84–1.35 |
| J00-J99 | Officers 3 | 149 | 93 | 79–109 | 154 | 85 | 73–99 | 0.91 | 0.73–1.14 | |
| J00-J99 | Non-officers 3 | 194 | 118 | 103–136 | 225 | 114 | 100–130 | 0.97 | 0.80–1.17 | |
| K00-K93 | Gastrointestinal diseases | Fishermen | 385 | 125 | 113–138 | 299 | 114 | 102–128 | 0.91 | 0.78–1.06 |
| K00-K93 | Officers | 354 | 96 | 87–107 | 385 | 91 | 82–101 | 0.94 | 0.82–1.09 | |
| K00-K93 | Non-officers | 414 | 125 | 114–138 | 508 | 121 | 111–132 | 0.97 | 0.85–1.10 | |
| L00-L99 | Skin diseases incl. subcutaneous diseases | Fishermen | 128 | 122 | 103–146 | 123 | 131 | 110–156 | 1.07 | 0.83–1.37 |
| L00-L99 | Officers | 94 | 85 | 68–104 | 112 | 78 | 65–94 | 0.92 | 0.70–1.22 | |
| L00-L99 | Non-officers | 147 | 121 | 103–142 | 218 | 134 | 117–153 | 1.11 | 0.90–1.37 | |
| M00-M99 | Bone, muscle, soft tissue diseases | Fishermen 4 | 546 | 122 | 113–133 | 494 | 118 | 108–129 | 0.97 | 0.86–1.09 |
| M00-M99 | Officers 4 | 384 | 75 | 68–83 | 499 | 75 | 69–82 | 1.00 | 0.87–1.14 | |
| M00-M99 | Non-officers 4 | 530 | 107 | 98–117 | 730 | 106 | 98–114 | 0.99 | 0.88–1.11 | |
| N00-N99 | Genitourinary tract diseases | Fishermen | 104 | 76 | 63–92 | 99 | 81 | 66–99 | 1.07 | 0.81–1.41 |
| N00-N99 | Officers | 160 | 98 | 84–114 | 229 | 118 | 104–135 | 1.21 | 0.99–1.48 | |
| N00-N99 | Non-officers | 149 | 100 | 85–117 | 215 | 108 | 94–123 | 1.08 | 0.88–1.33 | |
| S00-T98 | Lesions to one or more body regions | Fishermen | 1744 | 109 | 104–114 | 1487 | 118 | 112–124 | 1.08 | 1.01–1.16 |
| S00-T98 | Officers | 1232 | 69 | 65–73 | 1471 | 69 | 66–73 | 1.00 | 0.93–1.08 | |
| S00-T98 | Non-officers | 2118 | 111 | 106–116 | 2584 | 114 | 109–118 | 1.02 | 0.96–1.08 | |
| A00-E90, G00-T98 | All excl. F (psychiatric diseases) | Fishermen | 2552 | 107 | 103–112 | 2084 | 113 | 108–118 | 1.05 | 0.99–1.11 |
| A00-E90, G00-T98 | Officers | 2291 | 80 | 77–84 | 2610 | 80 | 77–83 | 1.00 | 0.94–1.06 | |
| A00-E90, G00-T98 | Non-officers | 3037 | 112 | 108–116 | 3568 | 113 | 109–116 | 1.01 | 0.96–1.06 | |
| ICD-10 1 | Site | Job Type | 1994–1998 | 1999–2003 | Trend 2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cases | SHCR | 95% CI | Cases | SHCR | 95% CI | SHCR ratio | 95% CI | |||
| A00-B99 | Infectious diseases | Officers | 0 | 0 | 0–225 | 0 | 0 | 0–159 | - | - |
| A00-B99 | Non-officers | 30 | 99 | 67–142 | 57 | 120 | 91–155 | 1.21 | 0.78–1.88 | |
| C00-D48 | Neoplastic diseases | Officers | 1 | 23 | 1–129 | 3 | 69 | 14–203 | - | - |
| C00-D48 | Non-officer 3 | 90 | 114 | 92–140 | 140 | 116 | 98–137 | 1.02 | 0.78–1.32 | |
| D50-D89 | Lymphohematopoietic diseases | Officers | 0 | 0 | 0–1171 | 0 | 0 | 0–752 | - | - |
| D50-D89 | Non-officers | 4 | 81 | 22–209 | 9 | 86 | 40–164 | - | - | |
| E00-E90 | Endocrinal and nutritional diseases | Officers | 1 | 61 | 2–339 | 1 | 48 | 1–268 | - | - |
| E00-E90 | Non-officers 3 | 25 | 80 | 52–118 | 47 | 87 | 64–115 | 1.09 | 0.67–1.77 | |
| G00-G99 | Diseases of the nervous system | Officers | 3 | 188 | 39–548 | 0 | 0 | 0–146 | - | - |
| G00-G99 | Non-officers | 37 | 120 | 85–165 | 58 | 110 | 84–143 | 0.92 | 0.61-1.39 | |
| H00-H59 | Diseases of the eye/ eye surroundings | Officers | 1 | 76 | 2–421 | 0 | 0 | 0–171 | - | - |
| H00-H59 | Non-officers | 23 | 85 | 54–127 | 42 | 87 | 63–117 | 1.02 | 0.61–1.70 | |
| H60-H95 | Diseases of the ear/ proc mastoideus | Officers | 1 | 96 | 3–537 | 2 | 175 | 21–630 | - | - |
| H60-H95 | Non-officers | 25 | 122 | 79–181 | 31 | 90 | 61–127 | 0.73 | 0.43–1.24 | |
| I00-I99 | Cardiovascular diseases | Officers | 1 | 34 | 1–189 | 4 | 106 | 29–272 | - | - |
| I00-I99 | Non-officers 3 | 73 | 135 | 106–170 | 124 | 118 | 99–140 | 0.87 | 0.65–1.16 | |
| J00-J99 | Respiratory diseases | Officers | 2 | 74 | 9–268 | 5 | 153 | 49–356 | - | - |
| J00-J99 | Non-officers 3 | 67 | 119 | 92–151 | 100 | 121 | 99–148 | 1.02 | 0.75-1.39 | |
| K00-K93 | Gastrointestinal diseases | Officers | 3 | 65 | 13–189 | 1 | 16 | 0–87 | - | - |
| K00-K93 | Non-officers | 125 | 134 | 112–159 | 192 | 120 | 104–138 | 0.90 | 0.72–1.12 | |
| L00-L99 | Skin diseases incl. subcutaneous diseases | Officers | 3 | 140 | 29–410 | 2 | 65 | 8–235 | - | - |
| L00-L99 | Non-officers | 50 | 111 | 82–146 | 94 | 125 | 101–153 | 1.12 | 0.80–1.59 | |
| M00-M99 | Bone, muscle, soft tissue diseases | Officers | 3 | 37 | 8–107 | 6 | 56 | 21–123 | 1.54 | 0.39–6.17 |
| M00-M99 | Non-officers | 171 | 109 | 93–126 | 293 | 106 | 95–119 | 0.98 | 0.81–1.18 | |
| N00-N99 | Genitourinary tract diseases | Officers | 7 | 70 | 28–144 | 9 | 72 | 33–137 | 1.04 | 0.39–2.78 |
| N00-N99 | Non-officers | 218 | 111 | 97–127 | 298 | 102 | 91–115 | 0.92 | 0.77–1.10 | |
| S00-T98 | Lesions to one or more body regions | Officers | 22 | 99 | 62–150 | 33 | 114 | 79–160 | 1.15 | 0.67–1.97 |
| S00-T98 | Non-officers | 567 | 126 | 116–136 | 868 | 121 | 113–129 | 0.96 | 0.87–1.07 | |
| A00-E90, G00-T98 | All excl. F (psychiatric diseases) | Officers | 52 | 79 | 59–104 | 68 | 86 | 67–109 | 1.09 | 0.76–1.56 |
| A00-E90, G00-T98 | Non-officers | 1277 | 110 | 104–116 | 1688 | 106 | 101–111 | 0.96 | 0.89–1.03 | |
3.3. Standardized Hospital Contact Ratios for Infectious and Skin Diseases by Gender, Job Type, and Time Period
| ICD-10 1,2 | Site | Job Type | 1994–1998 | 1999–2003 | Trend 3 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cases | SHCR | 95% CI | Cases | SHCR | 95% CI | SHCR ratio | 95% CI | |||
| Men | ||||||||||
| A00-B99 | Infectious diseases | Fishermen | 51 | 77 | 58–102 | 58 | 101 | 77–131 | 1.31 | 0.90–1.90 |
| A00-B99 | Officers | 69 | 99 | 77–126 | 85 | 98 | 78–121 | 0.98 | 0.72–1.35 | |
| A00-B99 | Non-officers | 119 | 153 | 128–183 | 111 | 110 | 92–133 | 0.72 | 0.56–0.93 | |
| A15-A19 | Tuberculosis | Fishermen | 6 | 446 | 164–971 | 9 | 954 | 437–1811 | ||
| A15-A19 | Non-officers | 5 | 349 | 113–814 | 4 | 252 | 69–645 | |||
| B15-B19 | Hepatitis | Fishermen | 3 | 83 | 17–242 | 4 | 150 | 41–385 | ||
| B15-B19 | Non-officers | 12 | 303 | 157–530 | 8 | 185 | 80–365 | |||
| B20-B24 | HIV | Officers | 4 | 143 | 39–366 | 3 | 146 | 30–426 | ||
| B20-B24 | Non-officers | 7 | 275 | 110–567 | 7 | 349 | 140–720 | |||
| B50-B54 | Protozoal diseases | Officers | 9 | 783 | 358–1486 | 3 | 249 | 51–726 | ||
| B50-B54 | Non-officers | 4 | 290 | 79–742 | 4 | 282 | 77–722 | |||
| Z20 | Contact with infectious disease | Fishermen | 10 | 241 | 116–443 | 8 | 110 | 47–217 | ||
| Z20 | Officers | 4 | 94 | 26–241 | 4 | 37 | 10–95 | |||
| Z20 | Non-officers | 8 | 166 | 72–327 | 12 | 97 | 50–170 | |||
| L00-L99 | Skin diseases incl. subcutaneous diseases | Fishermen | 128 | 122 | 103–146 | 123 | 131 | 110–156 | 1.07 | 0.83–1.37 |
| L00-L99 | Officers | 94 | 85 | 68–104 | 112 | 78 | 65–94 | 0.92 | 0.70–1.22 | |
| L00-L99 | Non-officers | 147 | 121 | 103–142 | 218 | 134 | 117–153 | 1.11 | 0.90–1.37 | |
| L20-L30 | Dermatitis and eczema | Fishermen | 5 | 43 | 14–100 | 25 | 217 | 140–320 | 5.06 | 1.94–13.21 |
| L20-L30 | Officers | 4 | 31 | 8–79 | 11 | 62 | 31–110 | 1.99 | 0.63–6.24 | |
| L20-L30 | Non-officers | 10 | 76 | 36–140 | 29 | 150 | 101–216 | 1.98 | 0.96–4.06 | |
| L23 | Allergic dermatitis and eczema | Fishermen | 3 | 153 | 32–447 | 18 | 797 | 472–1259 | ||
| L23 | Non-officers | 3 | 143 | 30–419 | 8 | 214 | 92–421 | |||
| L25 | Non-specified contact dermatitis | Non-officers | 1 | 73 | 2–405 | 4 | 289 | 79–740 | ||
| Women | ||||||||||
| A00-B99 | Infectious diseases | Non-officers | 30 | 99 | 67–142 | 57 | 120 | 91–155 | 1.21 | 0.78–1.88 |
| L00-L99 | Skin diseases incl. subcutaneous diseases | Non-officers | 50 | 111 | 82–146 | 94 | 125 | 101–153 | 1.12 | 0.80–1.59 |
| L20-L30 | Dermatitis and eczema | Non-officers | 8 | 111 | 48–218 | 19 | 150 | 90–234 | 1.35 | 0.59–3.09 |
| L23 | Allergic dermatitis | Non-officers | 1 | 57 | 2–315 | 3 | 97 | 20–283 | ||
| L24 | Toxic dermatitis | Non-officers | 3 | 246 | 51–720 | 3 | 165 | 34–483 | ||
| ICD-10 1,2 | Site | Type of Ship | Persons | Cases | SHCR | 95% CI |
|---|---|---|---|---|---|---|
| A00-B99 | Infectious diseases | Passenger | 1992 | 72 | 123 | 96–155 |
| A00-B99 | Other | 6495 | 243 | 127 | 112–144 | |
| A15-A19 | Tuberculosis | Passenger | 1992 | 3 | 262 | 54–767 |
| A15-A19 | Other | 6495 | 7 | 195 | 78–402 | |
| B15-B19 | Hepatitis | Passenger | 1992 | 3 | 102 | 21–299 |
| B15-B19 | Other | 6495 | 21 | 218 | 135–333 | |
| B20-B24 | HIV | Passenger | 1992 | 4 | 248 | 68–636 |
| B20-B24 | Other | 6495 | 12 | 232 | 120–405 |
3.4. Discussion
3.4.1. Main Findings
3.4.2. Main Strength and Possible Disadvantages of the Study
3.4.3. Comparison with Other Studies
4. Conclusions
Ethics Approval
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Hansen, H.L.; Pedersen, G. Influence of occupational accidents and deaths related to lifestyle on mortality among merchant seafarers. Int. J. Epidemiol. 1996, 25, 1237–1243. [Google Scholar] [CrossRef] [PubMed]
- Morales-Suarez-Varela, M.; Llopis-Gonzalez, A.; Garcia-Andres, J.; Jimenez-Lopez, M.C. A study of the health of seafaring workers of Valencia, Spain. Int. J. Occup. Environ. Health 1997, 3, 132–143. [Google Scholar] [CrossRef] [PubMed]
- Tomaszunas, S.; Renke, W.; Filikowski, J.; Rzepiak, M.; Zaborski, L. Diseases and work-related injuries in Polish seafarers and conditions of their work on foreign-flag ships. Bull. Inst. Marit. Trop. Med. Gdynia 1997, 48, 49–58. [Google Scholar] [PubMed]
- Roberts, S.E. Mortality from disease among seafarers in British merchant shipping (1976–1995). Int. Marit. Health 2002, 53, 43–58. [Google Scholar] [PubMed]
- Kaerlev, L.; Hansen, J.; Hansen, H.L.; Nielsen, P.S. Cancer incidence among Danish seafarers—A population-based cohort study. Occup. Environ. Med. 2005, 62, 761–765. [Google Scholar] [CrossRef] [PubMed]
- Hansen, H.L.; Tüchsen, F.; Hannerz, H. Hospitalization among seafarers on merchant ships. Occup. Environ. Med. 2005, 62, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Kaerlev, L.; Dahl, S.; Nielsen, P.S.; Olsen, J.; Hannerz, H.; Jensen, A.; Tüchsen, F. Hospital contacts for chronic diseases among Danish seafarers and fishermen—A population-based cohort study. Scand. J. Pub. Health 2007, 35, 481–489. [Google Scholar] [CrossRef]
- Kaerlev, L.; Jensen, A.; Nielsen, P.S.; Olsen, J.; Hannerz, H.; Tüchsen, F. Hospital contacts for injuries and musculoskeletal diseases among seamen and fishermen—A population-based cohort study. BMC Musculoskelet. Disord. 2008. [Google Scholar] [CrossRef] [Green Version]
- Kaerlev, L.; Jensen, A.; Nielsen, P.S.; Olsen, J.; Hannerz, H.; Tüchsen, F. Hospital contacts for noise related hearing loss among Danish seafarers and fishermen—A population-based cohort study. Noise Health 2008, 10, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Brandt, L.P.; Kirk, N.U.; Jensen, O.C.; Hansen, H.L. Mortality among Danish merchant seamen from 1970 to 1985. Amer. J. Ind. Med. 1994, 25, 867–876. [Google Scholar] [CrossRef]
- Jensen, O.C. Mortality in Danish fishermen. Bull. Inst. Marit. Trop. Med. Gdynia 1996, 47, 5–10. [Google Scholar] [PubMed]
- Lawrie, T.; Matheson, T.; Ritchie, L.; Murphy, E.; Bond, C. The health and lifestyle of Scottish fishermen: A need for health promotion. Health Educ. Res. 2004, 19, 373–379. [Google Scholar] [CrossRef] [PubMed]
- Coggon, D.; Harris, E.C.; Brown, T.; Rice, S.; Palmer, K.T. Occupation and mortality related to alcohol, drugs and sexual habits. Occup. Med. 2010, 60, 348–353. [Google Scholar] [CrossRef]
- Oldenburg, M.; Latza, U.; Baur, X. Occupational health risks due to shipboard cockroaches. Int. Arch. Occup. Environ. Health 2008, 81, 727–734. [Google Scholar] [CrossRef] [PubMed]
- Oldenburg, M.; Kuechmeister, B.; Ohnemus, U.; Baur, X.; Moll, I. Actinic keratosis among seafarers. Arch. Dermatol. Res. 2013, 305, 787–796. [Google Scholar] [CrossRef] [PubMed]
- Borch, D.F.; Hansen, H.L.; Burr, H.; Jepsen, J.R. Surveillance of maritime deaths on board Danish merchant ships, 1986–2009. Int. Marit. Health 2012, 63, 7–16. [Google Scholar] [PubMed]
- Zwierz, C. Examinations of digestive system parasitoses in people back from the tropics and subtropics. Bull. Inst. Marit Trop. Med. Gdynia 1985, 36, 69–75. [Google Scholar] [PubMed]
- Jensen, O.; Sorensen, J.F.L.; Kaerlev, L.; Canals, M.L.; Nikolic, N.; Saarni, H. Self-reported injuries among seafarers. Questionnaire validity and results from an international study. Accid. Anal. Prev. 2004, 36, 405–413. [Google Scholar] [CrossRef]
- Kærlev, L. Fiskeri og Helbred. Et Pilot Studie (Fishery and Health, A Pilot Study); Forskningsenheden for Maritim Medicin (Research Unit of Maritime Medicine): Esbjerg, Denmark, 2005. (In Danish) [Google Scholar]
- Matheson, C.; Morrison, S.; Murphy, E.; Lawrie, T.; Ritchie, L.; Bond, C. The health of fishermen in the catching sector of the fishing industry: A gap analysis. Occup. Med. 2001, 51, 305–311. [Google Scholar] [CrossRef]
- Hansen, H.L.; Jensen, J. Female seafarers adopt the high risk lifestyle of male seafarers. Occup. Environ. Med. 1998, 55, 49–51. [Google Scholar] [CrossRef] [PubMed]
- Burr, H.; Bjorner, J.B.; Kristensen, T.S.; Tüchsen, F.; Bach, E. Trends in the Danish working environment in 1990–2000 and their associations with labor-force changes. Scand. J. Work Environ. Health 2003, 29, 270–279. [Google Scholar] [CrossRef] [PubMed]
- Report II: Report on an ILO Investigation into the Living and Working Conditions of Seafarers; International Labour Office (ILO): Geneva, Switzerland, 2002.
- Hansen, H.L.; Hansen, K.G.; Andersen, P.L. Incidence and relative risk for hepatitis A, hepatitis B and tuberculosis and occurrence of malaria among merchant seamen. Scand. J. Infect. Dis. 1996, 28, 107–110. [Google Scholar] [CrossRef] [PubMed]
- Hansen, H.L. Occupation-Related Morbidity and Mortality among Merchant Seafarers with Particular Reference to Infectious Diseases; Institute of Maritime Medicine, South Jutland University Press: Esbjerg, Danmark, 1996. [Google Scholar]
- Towianska, A.; Dabrowski, J.; Rozlucka, E. HIV antibodies in seafarers, fishermen and in other population groups in the Gdansk Region (1993–1996). Bull. Inst. Marit. Trop. Med. Gdynia 1996, 47, 67–72. [Google Scholar] [PubMed]
- Svendsen, K.; Hilt, B. Skin disorders in ship’s engineers exposed to oils and solvents. Contact Dermat. 1997, 36, 216–220. [Google Scholar] [CrossRef]
- Moen, B.E.; Nilsson, R.; Nordlinder, R.; Ovrebø, S.; Bleie, K.; Skorve, A.H.; Hollund, B.E. Assessment of exposure to polycyclic aromatic hydrocarbons in engine rooms by measurement of urinary 1-hydroxypyrene. Occup. Environ. Med. 1996, 53, 692–696. [Google Scholar] [CrossRef] [PubMed]
- Danmarks Kutternøgle 2000; Silver Star Reklame: Skagen, Denmark, 2000.
- Tüchsen, F.; Bach, E.; Marmot, M. Occupation and hospitalization with ischaemic heart diseases: A new nationwide surveillance system based on hospital admissions. Int. J. Epidemiol. 1992, 21, 450–459. [Google Scholar] [CrossRef] [PubMed]
- Lynge, E.; Sandegaard, J.L.; Rebolj, M. The Danish national patient register. Scand. J. Public Health 2011, 39, 30–33. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, C.B. The Danish civil registration system. Scand. J. Public Health 2011, 39, 22–25. [Google Scholar] [CrossRef] [PubMed]
- Schlaich, C.C.; Oldenburg, M.; Lamshöft, M.M. Estimating the risk of communicable diseases aboard cargo ships. J. Travel. Med. 2009, 16, 402–406. [Google Scholar] [CrossRef] [PubMed]
- Scerbavicienë, R.; Pilipavicius, R. Malaria among seamen in Klaipeda in 1999–2008. Int. Marit. Health 2009, 60, 29–32. [Google Scholar] [PubMed]
- Grappasonni, I.; Paci, P.; Mazzucchi, F.; Amenta, F. Survey on HIV risk perception and sexual behaviours among seafarers. Int. Marit. Health 2011, 62, 131–137. [Google Scholar] [PubMed]
- Dahl, E. HIV (human immunodeficiency virus) testing and prevention in the cruise industry. Int. Marit. Health 2011, 62, 3–7. [Google Scholar]
- Hansen, H.L.; Henrik Andersen, P.; Lillebaek, T. Routes of M. tuberculosis transmission among merchant seafarers. Scand. J. Infect. Dis. 2006, 38, 882–887. [Google Scholar] [CrossRef] [PubMed]
- Haddad, V, Jr.; Lupi, O.; Lonza, J.P.; Tyring, S.K. Tropical dermatology: Marine and aquatic dermatology. J. Amer. Acad. Dermatol. 2009, 61, 733–750. [Google Scholar] [CrossRef]
- Hansen, H.L.; Pedersen, G. Poisoning at sea: Injuries caused by chemicals aboard Danish merchant ships 1988–1996. J. Toxicol. Clin. Toxicol. 2001, 39, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Budnik, L.T.; Wegner, R.; Rogall, U.; Baur, X. Accidental exposure to polychlorinated biphenyls (PCB) in waste cargo after heavy seas. Global waste transport as a source of PCB exposure. Int Arch. Occup. Environ. Health 2014, 87, 125–135. [Google Scholar] [CrossRef] [PubMed]
- Levy, B.S.; Nassetta, W.J. The adverse health effects of oil spills: A review of the literature and a framework for medically evaluating exposed individuals. Int J. Occup. Environ. Health 2011, 17, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Burke, W.A.; Griffith, D.C.; Scott, C.M.; Howell, E.R. Skin problems related to the occupation of commercial fishing in North Carolina. N. C. Med. J. 2006, 7, 260–265. [Google Scholar]
- Jensen, O.C.; Stage, S.; Noer, P.; Kaerlev, L. Classification of working processes to facilitate occupational hazard coding on industrial trawlers. Amer. J. Ind. Med. 2003, 44, 424–430. [Google Scholar] [CrossRef]
- Hemmingsson, T.; Lundberg, I.; Nilsson, R.; Allebeck, P. Health-related selection to seafaring occupations and its effects on morbidity and mortality. Amer. J. Ind. Med. 1997, 31, 662–668. [Google Scholar] [CrossRef]
- Madsen, K.M.; Schønheyder, H.C.; Kristensen, B.; Nielsen, G.L.; Sørensen, H.T. Can hospital discharge diagnosis be used for surveillance of bacteremia? A data quality study of a Danish hospital discharge registry. Infect. Control. Hosp. Epidemiol. 1998, 19, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Thomsen, R.W.; Riis, A.; Nørgaard, M.; Jacobsen, J.; Christensen, S.; McDonald, C.J.; Sørensen, H.T. Rising incidence and persistently high mortality of hospitalized pneumonia: A 10-year population- based study in Denmark. J. Intern. Med. 2006, 259, 410–417. [Google Scholar] [CrossRef] [PubMed]
- Holland-Bill, L.; Xu, H.; Sørensen, H.T.; Acquavella, J.; Sværke, C.; Gammelager, H.; Ehrenstein, V. Positive predictive value of primary inpatient discharge diagnoses of infection among cancer patients in the Danish national registry of patients. Ann. Epedemiol. 2014, 24, 593–597. [Google Scholar] [CrossRef]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaerlev, L.; Jensen, A.; Hannerz, H. Surveillance of Hospital Contacts among Danish Seafarers and Fishermen with Focus on Skin and Infectious Diseases—A Population-Based Cohort Study. Int. J. Environ. Res. Public Health 2014, 11, 11931-11949. https://doi.org/10.3390/ijerph111111931
Kaerlev L, Jensen A, Hannerz H. Surveillance of Hospital Contacts among Danish Seafarers and Fishermen with Focus on Skin and Infectious Diseases—A Population-Based Cohort Study. International Journal of Environmental Research and Public Health. 2014; 11(11):11931-11949. https://doi.org/10.3390/ijerph111111931
Chicago/Turabian StyleKaerlev, Linda, Anker Jensen, and Harald Hannerz. 2014. "Surveillance of Hospital Contacts among Danish Seafarers and Fishermen with Focus on Skin and Infectious Diseases—A Population-Based Cohort Study" International Journal of Environmental Research and Public Health 11, no. 11: 11931-11949. https://doi.org/10.3390/ijerph111111931