Can Economic Deprivation Protect Health? Paradoxical Multilevel Effects of Poverty on Hispanic Children’s Wheezing
Abstract
:1. Introduction
2. Methods
2.1. Study Area
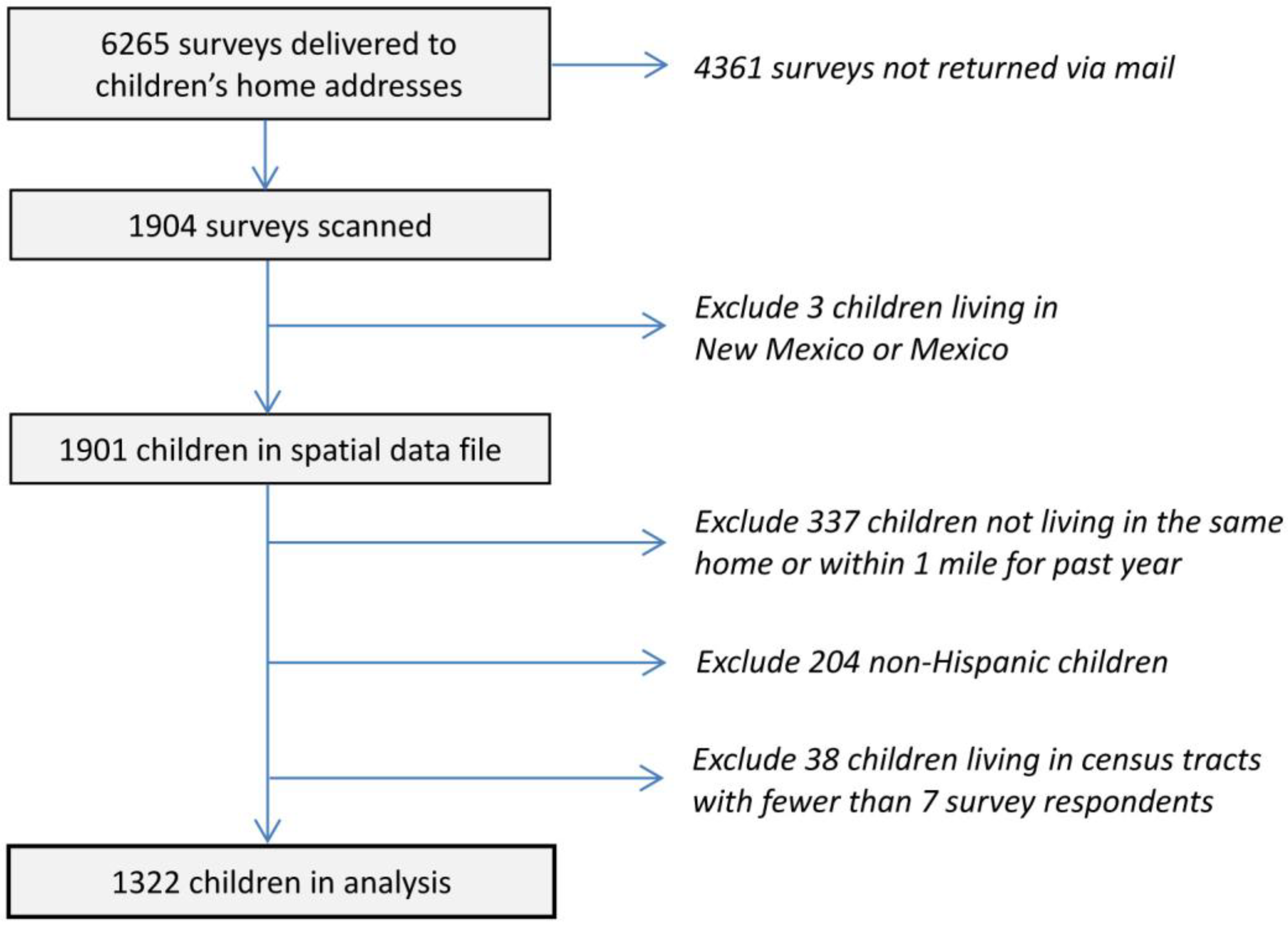
2.2. Study Design and Subjects

2.3. Dependent Variable
| Variable | Survey Question | Coding | Justification |
|---|---|---|---|
| Individual-level | |||
| Current Wheeze | Has your child had wheezing or whistling in the chest in the last12 months? From the International Study of Asthma and Allergies in Childhood (ISAAC) | 1 = Yes 0 = No | Wheezing is a common symptom of asthma. It is easily recognized by parents and is more specific to asthma than cough [37]. Current wheeze was selected instead of diagnosed asthma due to this study’s emphasis on immigration, a characteristic that shapes access to medical care and thus an asthma diagnosis. |
| Sex (Male) | What is the child’s sex? | 1 = Male 0 = Female | Boys have higher rates of asthma and other respiratory health problems than girls [38]. |
| Age | What is the child’s age (in years)? | Continuous variable | Asthma rates vary by age [39]. |
| Poverty Status | (a) How many people are living or staying at this address? (b) Which of the following best describes your yearly total household income for 2011 before taxes? | 1 = Poor 0 = Non-poor | Asthma rates are higher for children of lower socioeconomic status [40,41]. |
| General Health Status | How would you describe the overall health of the child? From the ISAAC | 1 = Very good 0 = Not very good | Health status is used as a medical history variable to account for the child’s underlying state of health [42]. |
| Obesity Status | (a) How tall is the child as of now? (b) How much does the child weigh as of now? (c) What is the child’s sex? (d) What is the child’s age (in years)? | 1 = Obese 0 = Not obese | Being overweight is associated with higher rates of asthma generally [43], and among Hispanic children specifically [44]. |
| Current Smoking | At any time during the past 12 months, has anybody smoked inside your child’s home? | 1 = Yes 0 = No | Smoking inside homes is an important cause of respiratory illness [45,46]. |
| Mold | Has your child’s home had mold or musty odors during the past 12 months? | 1 = Yes 0 = No | Moldy/damp housing environments are associated with wheezing and asthma [47,48,49]. |
| Nativity/Upbringing in El Paso (EP) | How long has this child lived in El Paso County? | 1 = Born/raised in El Paso 0 = Not born/raisedin El Paso | Children’s asthma and allergy prevalence increased with longer residential duration in El Paso [50]. |
| Primary Caretaker (PC) Born in the US | Primary caretakers were asked: “Where were you born?” | 1 = US-born 0 = Foreign-born | Hispanic children born to US-born mothers have higher rates of asthma than those born to foreign-born mothers [51]. |
| Neighborhood-level | |||
| % Poverty (Economic Deprivation) | Percent of families residing in the census tract living below the poverty line | Continuous variable | Most but not all studies find neighborhood poverty to be a respiratory health risk factor [9,10,15]. |
2.4. Individual-Level Independent Variable
2.5. Neighborhood-Level Independent Variable
2.6. Descriptive Statistics
| N | Mean a | SD | Min | Max | % Missing | |
|---|---|---|---|---|---|---|
| Individual | ||||||
| Current Wheeze | 1268 | 0.14 | 0.35 | 0 | 1 | 2.42 |
| Sex (Male) | 1259 | 0.49 | 0.50 | 0 | 1 | 3.15 |
| Age | 1225 | 10.38 | 0.77 | 7 | 13 | 5.72 |
| Poverty | 1133 | 0.43 | 0.50 | 0 | 1 | 12.46 |
| Excellent/Very Good Health Status | 1291 | 0.70 | 0.46 | 0 | 1 | 0.59 |
| Obesity | 869 | 0.14 | 0.35 | 0 | 1 | 33.21 |
| Smoking | 1243 | 0.08 | 0.27 | 0 | 1 | 4.25 |
| Mold | 1247 | 0.13 | 0.33 | 0 | 1 | 4.03 |
| Born/Raised EP b | 1148 | 0.69 | 0.46 | 0 | 1 | 11.44 |
| PC c Born U.S. | 1273 | 0.44 | 0.50 | 0 | 1 | 1.98 |
| Neighborhood | ||||||
| % Poverty | 63 | 23.27 | 17.32 | 0.70 | 69.30 | 0 |
2.7. Analytic Strategy
3. Results
| Variables | Model 1 | Model 2 | ||||
|---|---|---|---|---|---|---|
| Coef. | OR | 95% CI | Coef. | OR | 95% CI | |
| Intercept | −0.628 | 0.534 | (0.070, 4.051) | −0.466 | 0.627 | (0.085, 4.617) |
| Individual | ||||||
| Sex (Male) | 0.236 | 1.266 | (0.957, 1.675) | 0.226 | 1.254 | (0.948, 1.659) |
| Age | −0.146 | 0.864 | (0.712, 1.049) | −0.135 | 0.874 | (0.720, 1.061) |
| Poverty | −0.372 ** | 0.689 | (0.505, 0.940) | −0.158 | 0.854 | (0.591, 1.233) |
| Excellent/Very Good Health Status | −0.940 *** | 0.391 | (0.278, 0.548) | −1.000 *** | 0.368 | (0.258, 0.526) |
| Obesity | 0.162 | 1.176 | (0.762, 1.814) | 0.204 | 1.226 | (0.793, 1.895) |
| Smoking | −0.124 | 0.884 | (0.478, 1.633) | −0.067 | 0.935 | (0.509, 1.716) |
| Mold | 0.408 | 1.503 | (0.944, 2.394) | 0.431 | 1.540 | (0.965, 2.456) |
| Born/Raised EP a | 0.728 *** | 2.072 | (1.355, 3.167) | 0.739 *** | 2.094 | (1.363, 3.218) |
| PC b Born US | 0.734 *** | 2.084 | (1.547, 2.807) | 0.692 *** | 1.998 | (1.485, 2.688) |
| Neighborhood | ||||||
| % Poverty | -- | -- | -- | −0.013 ** | 0.987 | (0.978, 0.997) |
| Variables | Coef. | OR | 95% CI |
|---|---|---|---|
| Intercept | −0.426 | 0.653 | (0.088, 4.834) |
| Individual | |||
| Sex (Male) | 0.229 | 1.258 | (0.950, 1.666) |
| Age | −0.131 | 0.877 | (0.721, 1.067) |
| Poverty | −0.429 | 0.651 | (0.365, 1.161) |
| Excellent/Very Good Health Status | −1.016 *** | 0.362 | (0.253, 0.519) |
| Obesity | 0.203 | 1.225 | (0.795, 1.888) |
| Smoking | −0.057 | 0.944 | (0.516, 1.727) |
| Mold | 0.430 | 1.537 | (0.964, 2.449) |
| Born/Raised EP a | 0.747 *** | 2.110 | (1.380, 3.226) |
| PC b Born US | 0.690 *** | 1.994 | (1.482, 2.683) |
| Neighborhood | |||
| % Poverty | −0.017 ** | 0.983 | (0.969, 0.998) |
| Cross-level Interaction | |||
| % Poverty × Poverty (household) | 0.008 | 1.009 | (0.991, 1.027) |
4. Discussion
5. Conclusions
Acknowledgements
Author Contributions
Conflicts of Interest
References
- Shankardass, K.; McConnell, R.S.; Milam, J.; Berhane, K.; Tatalovich, Z.; Wilson, J.P. The association between contextual socioeconomic factors and prevalent asthma in a cohort of Southern California school children. Soc. Sci. Med. 2007, 65, 1792–1806. [Google Scholar] [CrossRef]
- Wright, R.J.; Subramanian, S.V. Advancing a multilevel framework for epidemiologic research on asthma disparities. Chest 2007, 132, 757S–769S. [Google Scholar] [CrossRef]
- Canino, G.; McQuaid, E.L.; Rand, C.S. Addressing asthma health disparities: A multilevel challenge. J. Allergy Clin. Immunol. 2009, 123, 1209–1219. [Google Scholar] [CrossRef]
- Brown, A.F.; Ang, A.; Pebley, A.R. The relationship between neighborhood characteristics and self-rated health for adults with chronic conditions. Am. J. Public Health 2007, 97, 926–932. [Google Scholar] [CrossRef]
- Krieger, N.; Chen, J.; Waterman, P.; Soobader, M.-J.; Subramanian, S.; Carson, R. Choosing area based socioeconomic measures to monitor social inequalities in low birth weight and childhood lead poisoning: The public health disparities geocoding project. J. Epidemiol. Commun. Health 2003, 57, 186–199. [Google Scholar] [CrossRef]
- Morenoff, J.D. Neighborhood mechanisms and the spatial dynamics of birthweight. Am. J. Soc. 2003, 108, 976–1017. [Google Scholar] [CrossRef]
- Pearl, M.; Braveman, P.; Abrams, B. The relationship of neighborhood socioeconomic characteristics to birth weight among 5 ethnic groups in California. Am. J. Public Health 2001, 91, 1808–1814. [Google Scholar] [CrossRef]
- Pickett, K.E.; Ahern, J.E.; Selvin, S.; Abrams, B. Neighborhood socioeconomic status, maternal race and preterm delivery: A case-control study. Ann. Epidemiol. 2002, 12, 410–418. [Google Scholar] [CrossRef]
- Grineski, S.E. Incorporating health outcomes into environmental justice research: The case of children’s asthma and air pollution in Phoenix, Arizona. Environ. Hazards 2007, 7, 360–371. [Google Scholar]
- Corburn, J.; Osleeb, J.; Porter, M. Urban asthma and the neighborhood environment in New York City. Health Place 2006, 12, 167–179. [Google Scholar] [CrossRef]
- Grineski, S.E.; Collins, T.W.; Chakraborty, J.; McDonald, Y.J. Environmental health justice: Exposure to air toxics and children’s respiratory hospital admissions. Profess. Geogr. 2013, 65, 31–46. [Google Scholar] [CrossRef]
- Juhn, Y.J.; St Sauver, J.; Katusic, S.; Vargas, D.; Weaver, A.; Yunginger, J. The influence of neighborhood environment on the incidence of childhood, asthma: A multilevel approach. Soc. Sci. Med. 2005, 60, 2453–2464. [Google Scholar] [CrossRef]
- Sternthal, M.J.; Jun, H.-J.; Earls, F.; Wright, R.J. Community violence and urban childhood asthma. Eur. Respir. J. 2010, 36, 1400–1409. [Google Scholar] [CrossRef]
- Holt, E.W.; Theall, K.P.; Rabito, F.A. Individual, housing and neighborhood correlations of asthma among young urban children. J. Urban Health 2013, 90, 116–129. [Google Scholar]
- Li, X.; Sundquist, J.; Calling, S.; Zoller, B.; Sundquist, K. Mothers, places and risk of hospitalization for childhood asthma: A nationwide study from Sweden. Clin. Exp. Allergy 2013, 43, 652–658. [Google Scholar]
- Pearlman, D.N.; Zierler, S.; Meersman, S.; Kim, H.; Viner-Brown, S.I.; Caron, C. Race disparities in childhood asthma: Does where you live matter? J. Natl Med. Assoc. 2006, 98, 240–247. [Google Scholar]
- Cagney, K.A.; Browning, C.R.; Wallace, D.M. The Latino paradox in neighborhood context: The case of asthma and other respiratory conditions. Am. J. Public Health 2007, 97, 919–925. [Google Scholar] [CrossRef]
- US Bureau of the Census. 2010 US Decennial Census. Available online: http://factfinder2.census.gov/faces/nav/jsf/pages/index.xhtml (accessed on 1 May 2014).
- US Bureau of the Census. American Community Survey, 2007–2011 5-year Estimates. Available online: http://factfinder2.census.gov/faces/nav/jsf/pages/index.xhtml (accessed on 1 May 2014).
- Grineski, S.E.; Collins, T.W.; Chavez-Payan, P.; Jimenez, A.; Kim, Y.; Gaines, M.; Clark-Reyna, S. Social disparities in children’s respiratory health in El Paso, Texas. Int. J. Environ. Res. Public Health 2014, 11, 2941–2957. [Google Scholar] [CrossRef]
- American Lung Association. Trends in Asthma Morbidity and Mortality. Available online: http://www.lung.org/finding-cures/our-research/trend-reports/asthma-trend-report.pdf (accessed on 1 May 2014).
- Dillman, D.A.; Smyth, J.D.; Christian, L.M. Internet, Mail, and Mixed-Mode Surveys: The Tailored Design Method, 3rd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2009. [Google Scholar]
- Curtin, R.; Presser, S.; Singer, E. The effects of response rate changes on the index of consumer sentiment. Public Opin. Q. 2000, 64, 413–428. [Google Scholar] [CrossRef]
- Holbrook, A.; Krosnick, J.; Pfent, A. The causes and consequences of response rates in surveys by the news media and government contractor survey research firms. In Advances in Telephone Survey Methodology; Lepkowski, J.M., Tucker, N.C., Brick, J.M., De Leeuw, E.D., Japec, L., Lavrakas, P.J., Link, M.W., Sangster, R.L., Eds.; Wiley: New York, NY, USA, 2008; pp. 499–528. [Google Scholar]
- Keeter, S.; Kennedy, C.; Dimock, M.; Best, J.; Craighill, P. Gauging the impact of growing nonresponse on estimates from a National RDD Telephone Survey. Public Opin. Q. 2006, 70, 759–779. [Google Scholar] [CrossRef]
- Visser, P.S.; Krosnick, J.A.; Marquette, J.; Curtin, M. Mail surveys for election forecasting? An evaluation of the Columbus Dispatch Poll. Public Opin. Q. 1996, 60, 181–227. [Google Scholar] [CrossRef]
- United States-México Border Health Commission. Health Disparities and the U.S.-México Border: Challenges and Opportunities; United States-México Border Health Commission: El Paso, TX, USA, 2010. [Google Scholar]
- EPISD. Enrollment Statistics, 2011–2012. Available online: http://www.episd.org/district_info/enrollment_stats.php (accessed on 1 May 2014).
- Penn, D.A. Estimating missing values from the general social survey: An application of multiple imputation. Soc. Sci. Q. 2007, 88, 573–584. [Google Scholar] [CrossRef]
- Enders, C.K. Applied Missing Data Analysis; Guilford Press: New York, NY, USA, 2010. [Google Scholar]
- Asher, M.I.; Barry, D.; Clayton, T.; Crane, J.; Souza, W.D.; Ellwood, P.; Ford, R.P.K.; Mitchell, E.A.; Moyes, C.; Pattemore, P.; Pearce, N.; Stewart, A.W. The burden of symptoms of asthma, allergic rhino conjunctivitis and atopic eczema in children and adolescents in six New Zealand centers: ISAAC Phase One. NZ Med. J. 2001, 114, 114–120. [Google Scholar]
- Björkstén, B.; Aït-Khaled, N.; Innes Asher, M.; Clayton, T.O.; Robertson, C.; the ISAAC Phase Three Study Group. Global analysis of breast feeding and risk of symptoms of asthma, rhino conjunctivitis and eczema in 6–7 year old children: ISAAC Phase Three. Allergologia et Immunopatholgia 2011, 39, 318–325. [Google Scholar] [CrossRef]
- Brunekreef, B.; Mutius, E.V.; Wong, G.K.; Odhiambo, J.A.; Clayton, T.O.; the ISAAC Phase Three Study Group. Early life exposure to farm animals and symptoms of asthma, rhino conjunctivitis and eczema: An ISAAC Phase Three Study. Int. J. Epidemiol. 2012, 41, 753–761. [Google Scholar] [CrossRef]
- Ellwood, P.; Asher, M.I.; Bjorksten, B.; Burr, M.; Pearce, N.; Robertson, C.F.; the ISAAC Phase One Study Group. Diet and asthma, allergic rhino conjunctivitis and atopic eczema symptom prevalence: An ecological analysis of the International Study of Asthma and Allergies in Childhood (ISAAC) data. Eur. Respir. J. 2001, 17, 436–443. [Google Scholar] [CrossRef]
- Kim, Y.; Collins, T.; Grineski, S. Neighborhood context and the Hispanic health paradox: Differential effects of immigrant density on children’s wheezing by poverty, nativity and medical history. Health Place 2014, 27, 1–8. [Google Scholar] [CrossRef]
- Jenkins, M.A.; Clarke, J.R.; Carlin, J.B.; Robertson, C.F.; Hopper, J.L.; Dalton, M.F.; Giles, G.G. Validation of questionnaire and bronchial hyper-responsiveness against respiratory physician assessment in the diagnosis of asthma. Int. J. Epidemiol. 1996, 25, 609–616. [Google Scholar] [CrossRef]
- Warren, N. Potential Data Sources for Asthma Surveillance at a County and State Level in California; Regional Asthma Management and Prevention Initiative: Berkley, CA, USA, 1999. [Google Scholar]
- Centers for Diesease Control and Prevention (CDC). Asthma’s Impact on the Nation: Data from the CDC National Asthma Control Program. 2013. Available online: http://www.cdc.gov/asthma/impacts_nation/AsthmaFactSheet.pdf (accessed on 1 May 2014). [Google Scholar]
- Centers for Disease Control and Prevention (CDC). National Health Interview Survey Data, 2007, National Center for Health Statistics. 2007. Available online: http://www.cdc.gov/asthma/nhis/07/table4-1.htm (accessed on 1 May 2014). [Google Scholar]
- Mitchell, E.A.; Stewart, A.W.; Pattemore, P.K.; Asher, M.I.; Harrison, A.C.; Rea, H.H. Socioeconomic status in childhood asthma. Int. Epidemiol. Assoc. 1989, 18, 888–890. [Google Scholar] [CrossRef]
- Mielck, A.; Reitmeir, P.; Wjst, M. Severity of childhood asthma by socioeconomic status. Int. Epidemiol. Assoc. 1996, 25, 388–393. [Google Scholar] [CrossRef]
- Aligne, C.A.; Auinger, P.; Byrd, R.S.; Weitzman, M. Risk factors for pediatric asthma: Contributions of poverty, race, and urban residence. Am. J. Respir. Crit. Care Med. 2000, 162, 873–877. [Google Scholar] [CrossRef]
- Delgado, J.; Barranco, P.; Quirce, S. Obesity and asthma. J. Invest. Allergol. Clin. Immunol. 2008, 18, 420–425. [Google Scholar]
- Morales, L.S.; Lara, M.; Kington, R.S.; Valdez, R.O.; Escarce, J.J. Socioeconomic, cultural, and behavioral factors affecting Hispanic health outcomes. J. Health Care Poor Underserv. 2002, 13, 477–503. [Google Scholar] [CrossRef]
- Burr, M.L.; Anderson, H.R.; Austin, J.B.; Harkins, L.S.; Kaur, B.; Strachan, D.P.; Warner, J.O. Respiratory symptoms and home environment in children: A national survey. Thorax 1999, 54, 27–32. [Google Scholar]
- Radic, S.D.; Gvozdenovic, B.S.; Pesic, I.M.; Zivkovic, Z.M.; Skodric-Trifunovic, V. Exposure to tobacco smoke among asthmatic children: Parents’ smoking habits and level of education. Int. J. Tubercul. Lung Dis. 2011, 15, 276–280. [Google Scholar]
- Strachan, D.P. Damp housing and childhood asthma: Validation of reporting of symptoms. Brit. Med. J. 1988, 297, 1223–1226. [Google Scholar] [CrossRef]
- Strachan, D.P.; Sanders, C.H. Damp housing and childhood asthma; Respiratory effects of indoor air temperature and relative humidity. J. Epidemiol. Commun. Health 1989, 43, 7–14. [Google Scholar] [CrossRef]
- Williamson, I.J.; Martin, C.J.; McGill, G.; Monie, R.D.H.; Fennerty, A.G. Damp housing and asthma: A case-control study. Thorax 1997, 52, 229–234. [Google Scholar] [CrossRef]
- Svendsen, E.R.; Gonzales, M.; Ross, M.; Neas, L.M. Variability in childhood allergy and asthma across ethnicity, language, and residency duration in El Paso, Texas: A cross-sectional study. Environ. Health 2009, 8, 1–15. [Google Scholar] [CrossRef]
- Subramanian, S.V.; Jun, H.-J.; Kawachi, I.; Wright, R.J. Contribution of race/ethnicity and country of origin to variations in lifetime reported asthma: Evidence for a nativity advantage. Am. J. Public Health 2009, 99, 690–697. [Google Scholar] [CrossRef]
- US Department of Health and Human Services. 2011 Federal poverty guidelines. Fed. Regist. 2011, 76, 3637–3638. [Google Scholar]
- Centers for Disease Control and Prevention (CDC). Clinical Growth Charts, Set 1: Clinical Charts with 5th and 95th Percentiles, Children 2 to 20 Years, Boys BMI-for-age, Girls BMI-for-Age. 2000. Available online: http://www.cdc.gov/growthcharts/clinical_charts.htm#Set1 (accessed on 1 May 2014). [Google Scholar]
- Lê, F.; Roux, A.; Morgenstern, H. Effects of child and adolescent health on educational progress. Soc. Sci. Med. 2013, 76, 57–66. [Google Scholar] [CrossRef]
- Spernak, S.M.; Schottenbauer, M.A.; Ramey, S.L.; Ramey, C.T. Child health and academic achievement among former head start children. Child. Youth Serv. Rev. 2006, 28, 1251–1261. [Google Scholar] [CrossRef]
- Raudenbush, S.W.; Bryk, A.S. Hierarchical Linear Models: Applications and Data Analysis Methods; Sage: Thousand Oaks, NJ, USA, 2002. [Google Scholar]
- Belsley, D.; Kuh, E.; Welsch, R. Regression Diagnostics: Identifying Influential Data and Sources of Collinearity; Wiley: Hoboken, NJ, USA, 1980. [Google Scholar]
- Basagaña, X.; Sunyer, J.; Kogevinas, M.; Zock, J.; Duran-Tauleria, E.; Jarvis, D.; Burney, P.; Anto, J.M. Socioeconomic status and asthma prevalence in young adults. Am. J. Epidemiol. 2004, 160, 178–188. [Google Scholar] [CrossRef]
- Cagney, K.A.; Browning, C.R.; Wallace, D.M. Explaining the Latino Asthma Advantage: The Role of Neighborhood Social Context. Population Association of America Annual Meeting: Philadelphia, PA, USA, 2005. Available online: https://ssa.uchicago.edu/sites/default/files/uploads/10212004.pdf (accessed on 1 May 2014).
- Richter, N.L.; Gorey, K.M.; Haji-Jama, S.; Luginaah, I.N. Care and survival of Mexican American women with node negative breast cancer: Historical cohort evidence of health insurance and barrio advantages. J. Immigr. Minor. Health 2013. [Google Scholar] [CrossRef]
- Wen, M.; Browning, C.R.; Cagney, K.A. Poverty, affluence, and income inequality: Neighborhood economic structure and its implications for health. Soc. Sci. Med. 2003, 57, 843–860. [Google Scholar] [CrossRef]
- Philips, B.U.; Belasco, E.; Markides, K.S.; Gong, G. Socioeconomic deprivation as a determinant of cancer mortality and the Hispanic paradox in Texas, USA. Int. J. Equity Health 2013, 12, 26. [Google Scholar] [CrossRef]
- Emerick, N.A.; Curry, T.R.; Collins, T.W.; Fernando Rodriguez, S. Homicide and social disorganization on the border: Implications for Latino and immigrant populations. Soc. Sci. Q. 2013. [Google Scholar] [CrossRef]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Collins, T.W.; Kim, Y.-a.; Grineski, S.E.; Clark-Reyna, S. Can Economic Deprivation Protect Health? Paradoxical Multilevel Effects of Poverty on Hispanic Children’s Wheezing. Int. J. Environ. Res. Public Health 2014, 11, 7856-7873. https://doi.org/10.3390/ijerph110807856
Collins TW, Kim Y-a, Grineski SE, Clark-Reyna S. Can Economic Deprivation Protect Health? Paradoxical Multilevel Effects of Poverty on Hispanic Children’s Wheezing. International Journal of Environmental Research and Public Health. 2014; 11(8):7856-7873. https://doi.org/10.3390/ijerph110807856
Chicago/Turabian StyleCollins, Timothy W., Young-an Kim, Sara E. Grineski, and Stephanie Clark-Reyna. 2014. "Can Economic Deprivation Protect Health? Paradoxical Multilevel Effects of Poverty on Hispanic Children’s Wheezing" International Journal of Environmental Research and Public Health 11, no. 8: 7856-7873. https://doi.org/10.3390/ijerph110807856





