Non-Obese Diabetes and Its Associated Factors in an Underdeveloped Area of South China, Guangxi
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
2.3. Oral Glucose-Tolerance Test
2.4. Definition of Outcomes
2.5. Statistical Analysis
3. Results
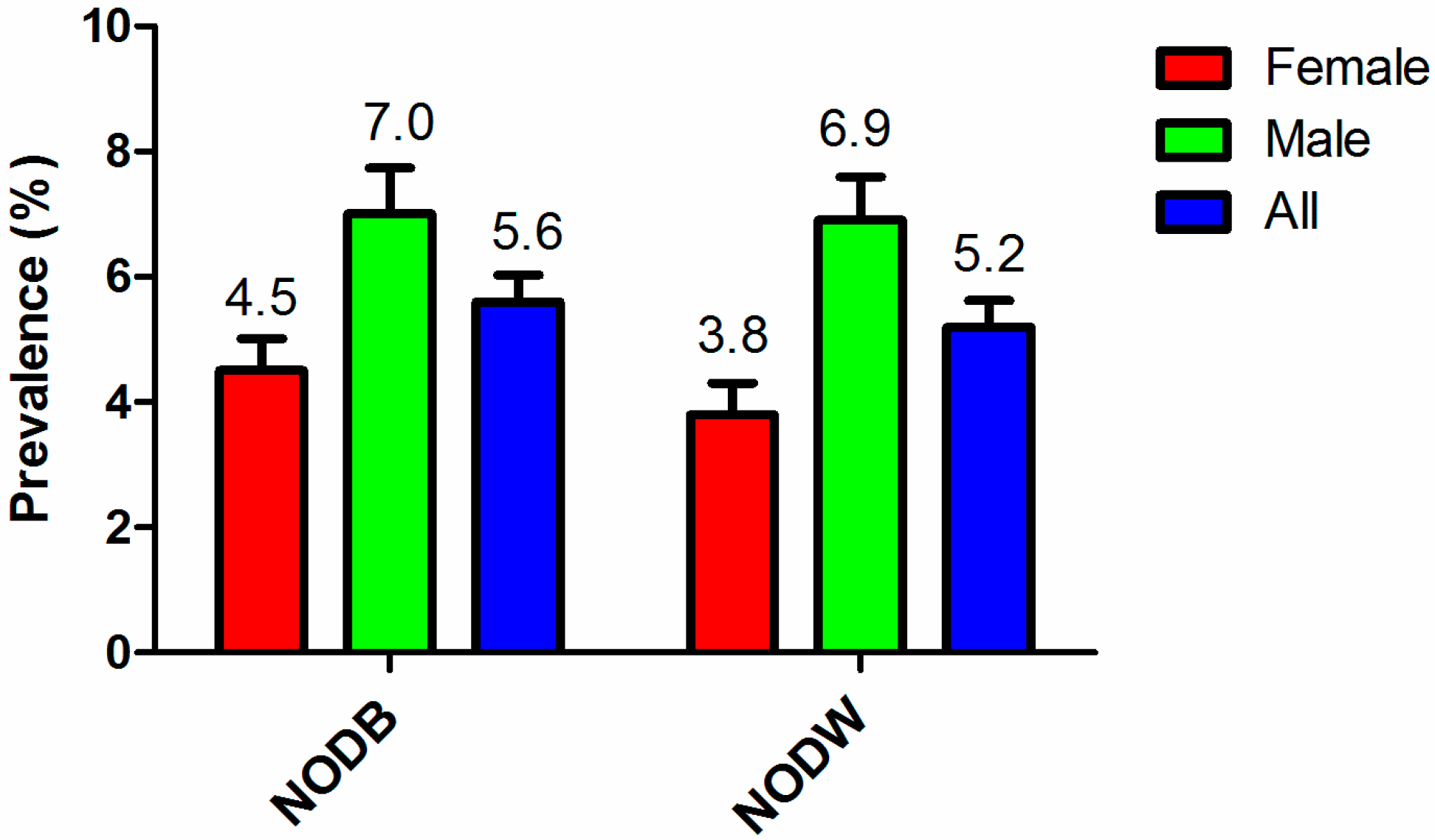
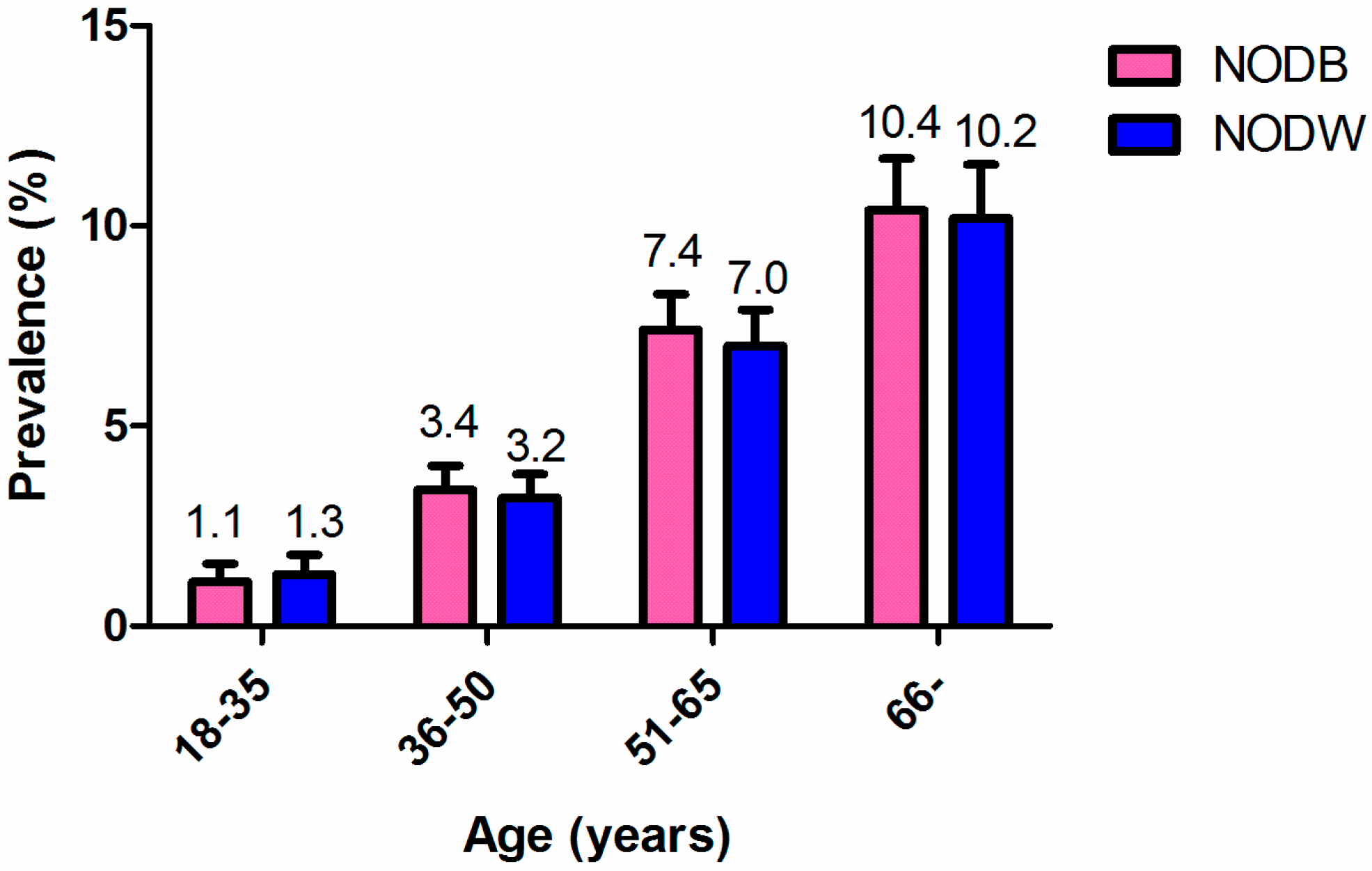
3.1. Prevalence of Non-Obese Diabetes
3.2. Characteristics of Non-Obese Diabetes Mellitus
3.3. Factors Associated with NODB and NODW
3.4. Interaction Effect on NODW
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Xu, Y.; Wang, L.; He, J.; Bi, Y.; Li, M.; Wang, T.; Wang, L.; Jiang, Y.; Dai, M.; Lu, J.; et al. Prevalence and control of diabetes in Chinese adults. JAMA 2013, 310, 948–959. [Google Scholar] [CrossRef] [PubMed]
- Scully, T. Diabetes in numbers. Nature 2012, 485, S2–S3. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Noncommunicable Diseases Country Profiles 2014. Available online: www.who.int/entity/nmh/publications/ncd-profiles-2014/en/ (accessed on 26 July 2016).
- Li, G.; Hu, Y.; Pan, X. Prevalence and incidence of NIDDM in Daqing City. Chin. Med. J. (Engl.) 1996, 109, 599–602. [Google Scholar] [PubMed]
- Leeder, S.; Raymond, S.; Greenberg, H.; Liu, H.; Esson, K. A Race Against Time: The Challenge of Cardiovascular Disease in Developing Economies; Columbia University: New York, NY, USA, 2004. [Google Scholar]
- Yang, G.; Kong, L.; Zhao, W.; Wan, X.; Zhai, Y.; Chen, L.C.; Koplan, J.P. Emergence of chronic non-communicable diseases in China. Lancet 2008, 372, 1697–1705. [Google Scholar] [CrossRef]
- Li, Y.; Chen, Q.Y.; Li, C.L.; Dai, X.; Luo, Z.J.; Xia, N.; Huang, G.M.; Li, S.M.; Qin, W.W.; Peng, Y.H.; et al. Analysis on Relative Influencing Factors of Abnormal Weight in Guangxi. Guangxi Med. J. 2011, 33, 133–137. [Google Scholar]
- Kashima, S.; Inoue, K.; Matsumoto, M.; Akimoto, K. Prevalence and characteristics of non-obese diabetes in Japanese men and women: The Yuport Medical Checkup Center Study Yuport. J. Diabetes 2015, 7, 523–530. [Google Scholar] [CrossRef] [PubMed]
- He, Y.N.; Zhao, L.Y.; Yu, D.M.; Fang, H.Y.; Yu, W.T.; Guo, Q.Y.; Wang, X.; Yang, X.G.; Ma, G.S. Consumption of fruits and vegetables in Chinese adults from 2010 to 2012. Zhonghua Yu Fang Yi Xue Za Zhi 2016, 50, 221–224. [Google Scholar] [PubMed]
- Liu, X.; Piao, J.; Zhang, Y.; Li, M.; Li, W.; Yang, L.; Yang, X. Serum Copper Status in School-Age Children and Pregnant Women in China Nutrition and Health Survey 2010–2012. Biol. Trace Elem. Res. 2016, 173, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.C.; Chen, J.; Li, M.; Li, W.D.; Yang, Y.H.; Yang, L.C.; Wang, R.; Piao, J.H. Study on the anemia status of Chinese urban residents in 2010–2012. Zhonghua Yu Fang Yi Xue Za Zhi 2016, 50, 213–216. [Google Scholar] [PubMed]
- Manore, M.M. Exercise and the Institute of Medicine recommendations for nutrition. Curr. Sports Med. Rep. 2005, 4, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Ainsworth, B.E.; Haskell, W.L.; Whitt, M.C.; Irwin, M.L.; Swartz, A.M.; Strath, S.J.; O’Brien, W.L.; Bassett, D.R., Jr.; Schmitz, K.H.; Emplaincourt, P.O.; et al. Compendium of physical activities: An update of activity codes and MET intensities. Med. Sci. Sports Exerc. 2000, 32 (Suppl. 9), S498–S504. [Google Scholar] [CrossRef] [PubMed]
- Department of Noncommunicable Disease Surveillance. Definition, Diagnosis and Classification of Diabetes Mellitus and Its Complications: Report of a Who Consultation. Part 1. Diagnosis and Classification of Diabetes Mellitus; World Health Organization: Geneva, Switzerland, 1999. [Google Scholar]
- The IDF Consensus Worldwide Definition of the Metabolic Syndrome. Available online: http://www.idf.org/webdata/docs/IDF Metasyndrome definition.pdf (accessed on 5 September 2016).
- Joint Committee for Developing Chinese guidelines on Prevention and Treatment of Dyslipidemia in Adults. Chinese guidelines on prevention and treatment of dyslipidemia in adults. Zhonghua Xin Xue Guan Bing Za Zhi 2007, 35, 390–419. [Google Scholar]
- Yoon, K.H.; Lee, J.H.; Kim, J.W.; Cho, J.H.; Choi, Y.H.; Ko, S.H.; Zimmet, P.; Son, H.Y. Epidemic obesity and type 2 diabetes in Asia. Lancet 2006, 368, 1681–1688. [Google Scholar] [CrossRef]
- Flegal, K.M.; Carroll, M.D.; Kit, B.K.; Ogden, C.L. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA 2012, 307, 491–497. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.C.; Malik, V.; Jia, W.; Kadowaki, T.; Yajnik, C.S.; Yoon, K.H.; Hu, F.B. Diabetes in Asia: Epidemiology, risk factors, and pathophysiology. JAMA 2009, 301, 2129–2140. [Google Scholar] [CrossRef] [PubMed]
- Wei, M.; Gaskill, S.P.; Haffner, S.M.; Stern, M.P. Waist circumference as the best predictor of noninsulin dependent diabetes mellitus (NIDDM) compared to body mass index, waist/hip ratio and other anthropometric measurements in Mexican Americans—A 7-year prospective study. Obes. Res. 1997, 5, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Falbe, J.; Cotterman, C.; Linchey, J.; Madsen, K.A. Ethnic Disparities in Trends in High BMI Among California Adolescents, 2003–2012. Am. J. Prev. Med. 2016, 51, e45–e55. [Google Scholar] [CrossRef] [PubMed]
- Gujral, U.P.; Mohan, V.; Pradeepa, R.; Deepa, M.; Anjana, R.M.; Mehta, N.K.; Gregg, E.W.; Narayan, K. Ethnic Variations in Diabetes and Prediabetes Prevalence and the roles of Insulin Resistance and beta-cell Function: The CARRS and NHANES Studies. J. Clin. Transl. Endocrinol. 2016, 4, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Pu, J.; Zhao, B.; Wang, E.J.; Nimbal, V.; Osmundson, S.; Kunz, L.; Popat, R.A.; Chung, S.; Palaniappan, L.P. Racial/Ethnic Differences in Gestational Diabetes Prevalence and Contribution of Common Risk Factors. Paediatr. Perinat. Epidemiol. 2015, 29, 436–443. [Google Scholar] [CrossRef] [PubMed]
- Perry, J.R.; Voight, B.F.; Yengo, L.; Amin, N.; Dupuis, J.; Ganser, M.; Grallert, H.; Navarro, P.; Li, M.; Qi, L. Stratifying type 2 diabetes cases by BMI identifies genetic risk variants in LAMA1 and enrichment for risk variants in lean compared to obese cases. PLoS Genet. 2012, 8, e1002741. [Google Scholar] [CrossRef] [PubMed]
- Bloomgarden, Z.T. Diabetes and cardiovascular disease. Diabetes Care 2011, 34, e24–e30. [Google Scholar] [CrossRef] [PubMed]
- Sowers, J.R.; Epstein, M.; Frohlich, E.D. Diabetes, hypertension, and cardiovascular disease: An update. Hypertension 2001, 37, 1053–1059. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | No. of Participants (%) (n = 3743) | No. of NODB a (%) (n = 159) | No. of NODW b (%) (n = 145) |
|---|---|---|---|
| Sex | |||
| Female | 2160 (57.7) | 75 (47.2) | 54 (37.2) |
| Male | 1583 (42.3) | 84 (52.8) | 91 (62.8) |
| Age (years) | |||
| 18–35 | 633 (16.9) | 6 (3.8) | 7 (4.8) |
| 36–50 | 1201 (32.1) | 30 (18.9) | 29 (20.0) |
| 51–65 | 1167 (31.2) | 64 (40.3) | 56 (38.6) |
| 66– | 742 (19.8) | 59 (37.1) | 53 (36.6) |
| Ethnicity | |||
| Han | 2827 (75.5) | 130 (81.8) | 113 (77.9) |
| Zhuang | 778 (20.8) | 25 (15.7) | 28 (19.3) |
| Others | 138 (3.7) | 4 (2.5) | 4 (2.8) |
| Education | |||
| Primary school and below | 1595 (42.6) | 96 (60.4) | 83 (57.2) |
| Junior high school | 1410 (37.7) | 36 (22.6) | 36 (24.8) |
| Senior high school and above | 738 (19.7) | 27 (17.0) | 26 (17.9) |
| Per-capita annual income (Yuan) * | |||
| <5000 | 1000 (27.7) | 47 (30.1) | 50 (35.2) |
| 5000–9999 | 1064 (29.5) | 43 (27.6) | 32 (22.5) |
| 10,000–19,999 | 1041 (28.9) | 52 (33.3) | 47 (33.1) |
| ≥20,000 | 503 (13.9) | 14 (9.0) | 13 (9.2) |
| Marriage status | |||
| Unmarried | 208 (5.6) | 2 (1.3) | 2 (1.4) |
| Married | 3174 (84.8) | 137 (86.2) | 125 (86.2) |
| Divorced/Widowed | 361 (9.6) | 20 (12.6) | 18 (12.4) |
| Residence | |||
| Urban | 1497 (40.0) | 68 (42.8) | 63 (43.4) |
| Rural | 2246 (60.0) | 91 (57.2) | 82 (56.6) |
| Physical activity level * | |||
| Sufficient | 1126 (43.2) | 51 (45.9) | 43 (42.6) |
| Insufficient | 1479 (56.8) | 60 (54.1) | 58 (57.4) |
| Smoking * | |||
| No | 2794 (75.2) | 113 (71.1) | 95 (65.5) |
| Yes | 920 (24.8) | 46 (28.9) | 50 (34.5) |
| Alcohol * | |||
| No | 2262 (60.8) | 89 (56.0) | 73 (50.3) |
| Yes | 1458 (39.2) | 70 (44.0) | 72 (49.7) |
| Hypertension * | |||
| No | 2720 (73.0) | 85 (53.5) | 80 (55.2) |
| Yes | 1007 (27.0) | 74 (46.5) | 65 (44.8) |
| Hypertriglyceridemia * | |||
| No | 3107 (84.4) | 110 (70.1) | 107 (74.8) |
| Yes | 575 (15.6) | 47 (29.9) | 36 (25.2) |
| Hypercholesterolemia * | |||
| No | 2876 (78.3) | 123 (78.3) | 118 (82.5) |
| Yes | 799 (21.7) | 34 (21.7) | 25 (17.5) |
| Low HDL c,* | |||
| No | 3118 (84.7) | 118 (75.2) | 110 (76.9) |
| Yes | 565 (15.3) | 39 (24.8) | 33 (23.1) |
| High LDL d,* | |||
| No | 3131 (85.1) | 137 (87.3) | 127 (88.8) |
| Yes | 550 (14.9) | 20 (12.7) | 16 (11.2) |
| Anemia * | |||
| No | 3448 (92.3) | 143 (89.9) | 131 (90.3) |
| Yes | 288 (7.7) | 16 (10.1) | 14 (9.7) |
| BMI (kg/m2) e,* | |||
| <25.0 | 2852 (76.7) | 159 (100.0) | 128 (88.3) |
| ≥25.0 | 866 (23.3) | - | 17 (11.7) |
| Abdominal obesity * | |||
| No | 2763 (74.4) | 128 (80.5) | 145 (100.0) |
| Yes | 950 (25.6) | 31 (19.5) | - |
| Family history of hypertension * | |||
| No | 2052 (78.3) | 79 (74.5) | 70 (75.3) |
| Yes | 570 (21.7) | 27 (25.5) | 23 (24.7) |
| Family history of coronary heart disease * | |||
| No | 2347 (96.1) | 90 (94.7) | 80 (95.2) |
| Yes | 96 (3.9) | 5 (5.3) | 4 (4.8) |
| Family history of cerebral apoplexy * | |||
| No | 2342 (95.8) | 91 (94.8) | 81 (95.3) |
| Yes | 103 (4.2) | 5 (5.2) | 4 (4.7) |
| Family history of diabetes mellitus * | |||
| No | 2332 (95.2) | 93 (97.9) | 82 (97.6) |
| Yes | 118 (4.8) | 2 (2.1) | 2 (2.4) |
| Factor | Univariable Analysis | Full Model | ||||||
|---|---|---|---|---|---|---|---|---|
| NODB | NODW | NODB | NODW | |||||
| OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Sex | ||||||||
| Female | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | ||||
| Male | 1.56 (1.13, 2.14) | 0.006 | 2.38 (1.69, 3.35) | <0.001 | 1.49 (1.02, 2.17) | 0.039 | 1.58 (0.98, 2.55) | 0.059 |
| Age (years) | ||||||||
| 18–35 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | ||||
| 36–50 | 2.68 (1.11, 6.47) | 0.029 | 2.21 (0.96, 5.08) | 0.061 | 2.00 (0.78, 5.16) | 0.149 | 1.95 (0.81, 4.73) | 0.139 |
| 51–65 | 6.06 (2.61, 14.08) | <0.001 | 4.51 (2.04, 9.95) | <0.001 | 3.41 (1.35, 8.62) | 0.010 | 3.68 (1.55, 8.75) | 0.003 |
| 66– | 9.03 (3.87, 21.05) | <0.001 | 6.90 (3.11, 15.29) | <0.001 | 4.65 (1.77, 12.18) | 0.002 | 5.30 (2.14, 13.11) | <0.001 |
| Ethnicity | ||||||||
| Han | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | - | ||||
| Zhuang | 0.69 (0.45, 1.06) | 0.093 | 0.90 (0.59, 1.37) | 0.610 | 0.63 (0.38, 1.02) | 0.058 | - | - |
| Others | 0.62 (0.23, 1.70) | 0.352 | 0.72 (0.26, 1.97) | 0.518 | 0.54 (0.18, 1.56) | 0.252 | - | - |
| Education | ||||||||
| Primary school and below | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | ||||
| Junior high school | 0.41 (0.28, 0.60) | <0.001 | 0.48 (0.32, 0.71) | <0.001 | 0.54 (0.35, 0.85) | 0.007 | 0.64 (0.41, 1.00) | 0.050 |
| Senior high school and above | 0.59 (0.38, 0.92) | 0.019 | 0.66 (0.42, 1.04) | 0.074 | 0.91 (0.55, 1.49) | 0.700 | 1.03 (0.62, 1.71) | 0.941 |
| Per-capita annual income (Yuan) | ||||||||
| <5000 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | ||||
| 5000–9999 | 0.85 (0.56, 1.30) | 0.464 | 0.59 (0.37, 0.93) | 0.022 | 0.97 (0.62, 1.52) | 0.900 | 0.68 (0.43, 1.10) | 0.114 |
| 10,000–19,999 | 1.07 (0.71, 1.60) | 0.756 | 0.90 (0.60, 1.35) | 0.607 | 1.30 (0.84, 2.01) | 0.235 | 1.09 (0.71, 1.69) | 0.688 |
| ≥20,000 | 0.58 (0.32, 1.06) | 0.079 | 0.50 (0.27, 0.94) | 0.030 | 0.67 (0.35, 1.30) | 0.237 | 0.54 (0.28, 1.05) | 0.068 |
| Marital status | ||||||||
| Unmarried | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | ||||
| Married | 4.65 (1.14, 18.90) | 0.032 | 4.23 (1.04, 17.20) | 0.044 | 2.03 (0.44, 9.31) | 0.360 | 1.85 (0.41, 8.36) | 0.425 |
| Divorced/Widowed | 6.04 (1.40, 26.11) | 0.016 | 5.41 (1.24, 23.53) | 0.025 | 1.66 (0.33, 8.35) | 0.541 | 1.48 (0.29, 7.44) | 0.637 |
| Smoking | ||||||||
| No | 1.00 (ref) | 1.00 (ref) | - | 1.00 (ref) | ||||
| Yes | 1.25 (0.88, 1.77) | 0.215 | 1.63 (1.15, 2.32) | 0.006 | - | - | 0.85 (0.54, 1.34) | 0.493 |
| Alcohol | ||||||||
| No | 1.00 (ref) | 1.00 (ref) | - | 1.00 (ref) | ||||
| Yes | 1.23 (0.89, 1.70) | 0.203 | 1.56 (1.12, 2.17) | 0.009 | - | - | 1.04 (0.70, 1.56) | 0.838 |
| Hypertension | ||||||||
| No | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | ||||
| Yes | 2.46 (1.78, 3.39) | <0.001 | 2.28 (1.63, 3.19) | <0.001 | 1.83 (1.26, 2.65) | 0.002 | 1.58 (1.07, 2.32) | 0.022 |
| Hypertriglyceridemia | ||||||||
| No | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | ||||
| Yes | 2.43 (1.70, 3.45) | <0.001 | 1.87 (1.27, 2.76) | 0.002 | 2.67 (1.75, 4.07) | <0.001 | 2.08 (1.31, 3.30) | 0.002 |
| Low HDL | ||||||||
| No | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | ||||
| Yes | 1.89 (1.30, 2.74) | 0.001 | 1.70 (1.14, 2.53) | 0.009 | 1.42 (0.91, 2.21) | 0.126 | 1.52 (0.95, 2.43) | 0.080 |
| BMI (kg/m2) | ||||||||
| <25 | - | 1.00 (ref) | - | 1.00 (ref) | ||||
| ≥25 | - | - | 0.43 (0.26, 0.71) | 0.001 | - | - | 1.20 (0.70, 2.12) | 0.531 |
| Abdominal obesity | ||||||||
| No | 1.00 (ref) | - | 1.00 (ref) | - | ||||
| Yes | 0.69 (0.47, 1.04) | 0.074 | - | - | 1.63 (1.01, 2.63) | 0.044 | - | - |
| NODW | NODB | |||||
|---|---|---|---|---|---|---|
| Smoking Status | No. of Patient | OR (95% CI) | p Value | No. of Patient | OR (95% CI) | p Value |
| Non-smoker | 95 | 1.43 (0.74, 2.77) | 0.29 | 113 | 2.25 (1.32, 3.82) | 0.003 |
| * Smoker | 50 | 3.25 (1.60, 6.59) | 0.001 | 46 | 4.10 (1.93, 8.70) | <0.001 |
| 2.69 (1.13, 6.43) | pinteraction = 0.026 | 1.59 (0.70, 3.61) | pinteraction = 0.27 | |||
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tang, Z.; Fang, Z.; Huang, W.; Liu, Z.; Chen, Y.; Li, Z.; Zhu, T.; Wang, Q.; Simpson, S.; Taylor, B.V.; et al. Non-Obese Diabetes and Its Associated Factors in an Underdeveloped Area of South China, Guangxi. Int. J. Environ. Res. Public Health 2016, 13, 976. https://doi.org/10.3390/ijerph13100976
Tang Z, Fang Z, Huang W, Liu Z, Chen Y, Li Z, Zhu T, Wang Q, Simpson S, Taylor BV, et al. Non-Obese Diabetes and Its Associated Factors in an Underdeveloped Area of South China, Guangxi. International Journal of Environmental Research and Public Health. 2016; 13(10):976. https://doi.org/10.3390/ijerph13100976
Chicago/Turabian StyleTang, Zhenzhu, Zhifeng Fang, Wei Huang, Zhanhua Liu, Yuzhu Chen, Zhongyou Li, Ting Zhu, Qichun Wang, Steve Simpson, Bruce V. Taylor, and et al. 2016. "Non-Obese Diabetes and Its Associated Factors in an Underdeveloped Area of South China, Guangxi" International Journal of Environmental Research and Public Health 13, no. 10: 976. https://doi.org/10.3390/ijerph13100976
APA StyleTang, Z., Fang, Z., Huang, W., Liu, Z., Chen, Y., Li, Z., Zhu, T., Wang, Q., Simpson, S., Taylor, B. V., & Lin, R. (2016). Non-Obese Diabetes and Its Associated Factors in an Underdeveloped Area of South China, Guangxi. International Journal of Environmental Research and Public Health, 13(10), 976. https://doi.org/10.3390/ijerph13100976





