Stakeholders’ Perception on National Heatwave Plans and Their Local Implementation in Belgium and The Netherlands
Abstract
:1. Introduction
2. Materials and Methods
2.1. Desk Evaluation of National Heatwave Plans
2.2. Key Informant Interviews
3. Results
3.1. Desk Evaluation of National Heatwave Plans
3.2. Key Informant Interviews
3.2.1. Familiarity with the National Heatwave Plans
3.2.2. Involvement in National Heatwave Plan Development
3.2.3. Heat as a Public Health Priority
3.2.4. Involvement in Warning At-Risk Populations
3.2.5. Success in Reaching the At-Risk Populations
3.2.6. Responsibilities Described in National Heatwave Plan
3.2.7. Collaboration between Stakeholders
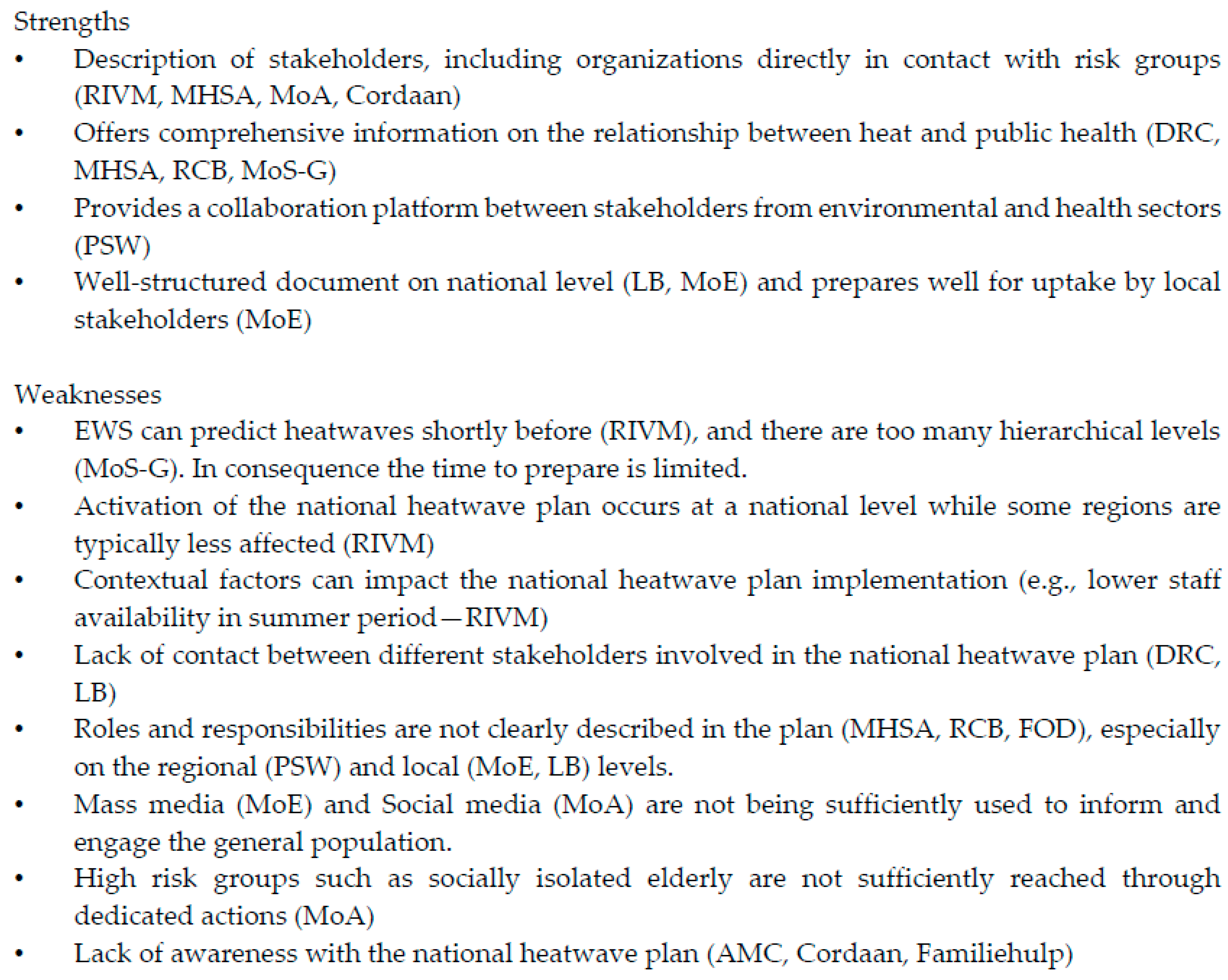
3.2.8. Strengths and Weaknesses of the National Heatwave Plan
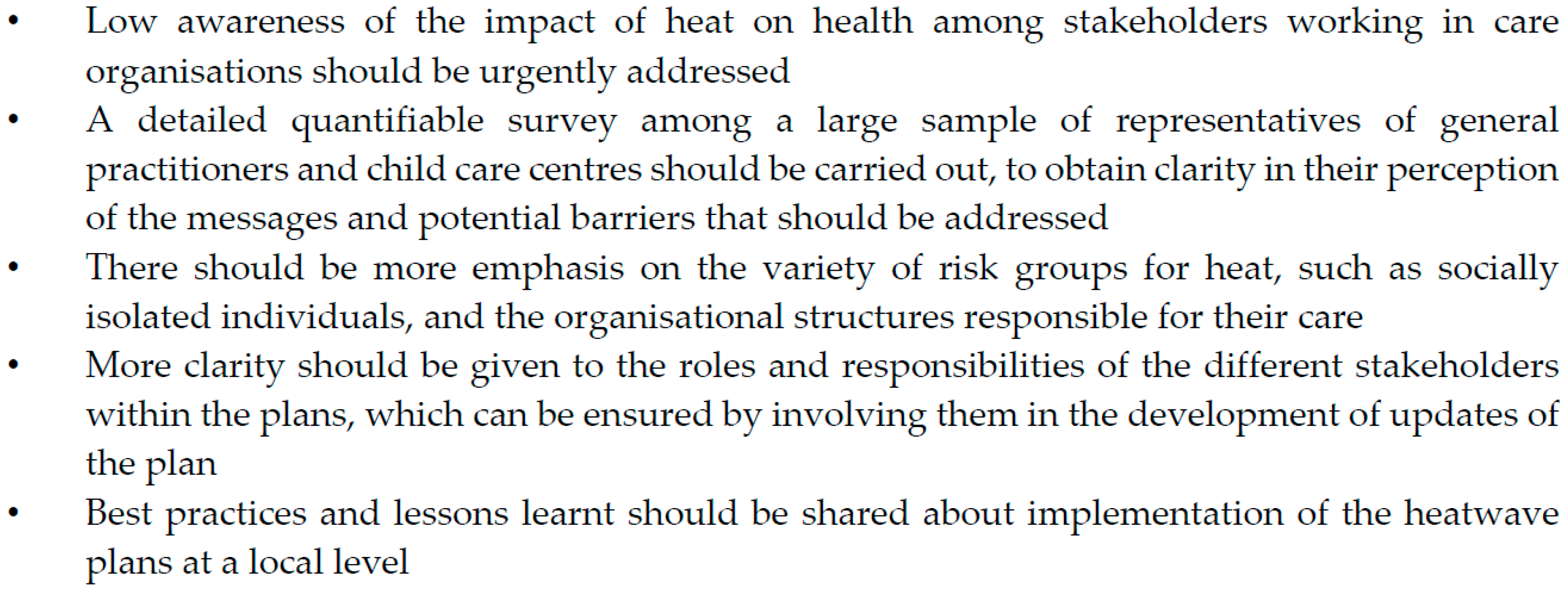
4. Discussion
5. Limitations
6. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Appendix A
Interview Format for Stakeholders with a Role in National Heatwave Plans
Current Roles and Obligations
- 1
- Are you familiar with the content of the National Heat Plan?
- 2
- Was your organisation involved in the development of the plan?
- 3
- Are there other heat plans (e.g., local, organisational) that include your organisation?
- 4
- What role/tasks does your organisation perform with respect to heat exposure, in addition to what is described within the National Heat Plan?
- 5
- How high would you prioritise exposure to heat as a public health threat (e.g., on a scale of 1−10)?
Message to the Public
- 1
- Is your organisation directly involved in warning a population at risk for adverse effects due to heat? If yes:
- What are your target groups?
- Do you feel that you reach a large proportion of these groups?
- Do you feel the National Heat Plan offers enough options to adequately reach this population?
- Do you feel another way of reaching the target populations might be more effective?
- 2
- Do you feel the messages and recommendations that the National Heat Plan presents are sufficiently clear for the population at risk and their caregivers?
- 3
- How well do you think the population at risk changes its behaviour due to recommendations from the heat plan (e.g., on a scale of 1–10)?
Cooperation with Other Stakeholders
- 1
- Which other organisations are you in contact with on the topic of heat:
- During a cold/normal period?
- When the heat plan is activated?
- 2
- Are all these collaborations described in one of the heat plans?
- 3
- Do you feel the responsibilities of the different organisations are clearly described in the heat plans?
- 4
- Do you feel the communication/cooperation between the different stakeholders functions well?
- 5
- Do you feel that the current number of collaborations is sufficient?
- If yes: do you think the number of collaborations should be reduced to simplify the system?
- If no: which collaboration is currently not included in a heat plan, but would, in your opinion, be an important addition?
Future Roles
- 1
- Are you aware of the impact that climate change will have on your country, with respect to heat exposure?
- 2
- Is there/has there been a discussion within your organisation on adaptations that might be needed to cope with the impact of climate change on the intensity and frequency of heat waves?
- 3
- Do you think the current heat plan will suffice when the intensity and frequency of heatwaves will increase, in terms of collaborations with other organisations? If no: Which additional collaborations do you feel would be necessary?
General Conclusion
- 1
- What do you consider to be strong aspects of the national heat plan?
- 2
- What do you consider to be weak aspects of the national heat plan?
- 3
- Do you have any other remarks which could be relevant to our project?
References
- Baccini, M.; Kosatsky, T.; Biggeri, A. Impact of summer heat on urban population mortality in Europe during the 1990s: An evaluation of years of life lost adjusted for harvesting. PLoS ONE 2013, 8, e69638. [Google Scholar] [CrossRef] [PubMed]
- Astrom, D.O.; Forsberg, B.; Rocklov, J. Heat wave impact on morbidity and mortality in the elderly population: A review of recent studies. Maturitas 2011, 69, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Garssen, J.; Harmsen, C.; de Beer, J. The effect of the summer 2003 heat wave on mortality in The Netherlands. Eurosurveillance 2005, 10, 165–168. [Google Scholar] [PubMed]
- Centre for Research on the Epidemiology of Disasters: The International Disaster Database—EM-DAT. Available online: http://www.emdat.be/ (accessed on 1 July 2015).
- Mastrangelo, G.; Fedeli, U.; Visentin, C.; Milan, G.; Fadda, E.; Spolaore, P. Pattern and determinants of hospitalization during heat waves: An ecologic study. BMC Public Health 2007, 7, 200. [Google Scholar] [CrossRef] [PubMed]
- Van Loenhout, J.A.; le Grand, A.; Duijm, F.; Greven, F.; Vink, N.M.; Hoek, G.; Zuurbier, M. The effect of high indoor temperatures on self-perceived health of elderly persons. Environ. Res. 2016, 146, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Parry, M.L.; Canziani, O.F.; Palutikof, J.P.; van der Linden, P.J.; Hanson, C.E. Contribution of Working Group II to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change; Cambridge University Press: Cambridge, UK, 2007. [Google Scholar]
- Bittner, M.I.; Matthies, E.F.; Dalbokova, D.; Menne, B. Are European countries prepared for the next big heat-wave? Eur. J. Public Health 2014, 24, 615–619. [Google Scholar] [CrossRef] [PubMed]
- Lowe, D.; Ebi, K.L.; Forsberg, B. Heatwave early warning systems and adaptation advice to reduce human health consequences of heatwaves. Int. J. Environ. Res. Public Health 2011, 8, 4623–4648. [Google Scholar] [CrossRef] [PubMed]
- Morabito, M.; Profili, F.; Crisci, A.; Francesconi, P.; Gensini, G.F.; Orlandini, S. Heat-related mortality in the Florentine area (Italy) before and after the exceptional 2003 heat wave in Europe: An improved public health response? Int. J. Biometeorol. 2012, 56, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Fouillet, A.; Rey, G.; Wagner, V.; Laaidi, K.; Empereur-Bissonnet, P.; Le Tertre, A.; Frayssinet, P.; Bessemoulin, P.; Laurent, F.; De Crouy-Chanel, P.; et al. Has the impact of heat waves on mortality changed in France since the European heat wave of summer 2003? A study of the 2006 heat wave. Int. J. Epidemiol. 2008, 37, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Boeckmann, M.; Rohn, I. Is planned adaptation to heat reducing heat-related mortality and illness? A systematic review. BMC Public Health 2014, 14, 1112. [Google Scholar] [CrossRef] [PubMed]
- De’Donato, F.K.; Leone, M.; Scortichini, M.; De Sario, M.; Katsouyanni, K.; Lanki, T.; Basagana, X.; Ballester, F.; Astrom, C.; Paldy, A.; et al. Changes in the effect of heat on mortality in the last 20 years in nine European cities. Results from the PHASE project. Int. J. Environ. Res. Public Health 2015, 12, 15567–15583. [Google Scholar] [CrossRef] [PubMed]
- Sante Publique, Securite de la Chaine Alimentaire et Environnement. Plan Vague de Chaleur et Pics D’Ozone; Federal Public Service for Health, Food Chain Safety and Environment: Brussels, Belgium, 2008. [Google Scholar]
- Brasseur, O.; Berger, N.; Lokietek, S. Evaluation Scientifique de la Surveillance Environnement et Santé Apres 10 ans D’Application du Plan Ozone et Vague de Chaleur en Belgique; NEHAP: Wallonia, Belgium, 2014. [Google Scholar]
- Arnfield, A.J. Review: Two decades of urban climate research: A review of turbulence, exchanges of energy and water, and the urban heat island. Int. J. Climatol. 2003, 23, 1–26. [Google Scholar] [CrossRef]
- Rohleder, P.; Lyons, A.C. Qualitative Research in Clinical and Health Psychology; Palgrave Macmillan: Basingstoke, UK, 2014. [Google Scholar]
- Ministerie van Volksgezondheid, Welzijn en Sport. Nationaal Hitteplan; Ministerie van Volksgezondheid, Welzijn en Sport: The Haag, The Netherlands, 2007. [Google Scholar]
- Department of Health (United Kingdom). Heatwave Plan for England 2008; Department of Health (United Kingdom): London, UK, 2008.
- Abrahamson, V.; Raine, R. Health and social care responses to the Department of Health Heatwave Plan. J. Public Health 2009, 31, 478–489. [Google Scholar] [CrossRef] [PubMed]
- Kunst, A.E.; Britstra, R. Implementation evaluation of the Dutch National Heat Plan among long-term care institutions in Amsterdam: A cross-sectional study. BMC Health Serv. Res. 2013, 13, 135. [Google Scholar] [CrossRef] [PubMed]
- Ramin, B.; Svoboda, T. Health of the homeless and climate change. J. Urban Health 2009, 86, 654–664. [Google Scholar] [CrossRef] [PubMed]
- Abeling, T. According to plan? Disaster risk knowledge and organizational responses to heat wave risk in London, UK. Ecosyst. Health Sustain. 2015, 1, 1–8. [Google Scholar] [CrossRef]
| Belgium | The Netherlands | |||||
|---|---|---|---|---|---|---|
| Levels of Alert | Phase | Activation | Actions for Main Stakeholders | Phase | Activation | Actions for Main Stakeholders |
| Watchfulness | 15 May until 30 September |
| Watchfulness | 1 June until 1 September |
| |
| Warning level 1 |
|
| Pre-warning | Odds of five days >27 °C higher than 20% |
| |
| Warning level 2 |
|
| Warning | Odds of five days >27 °C higher than 90% |
| |
| Alert |
|
| ||||
| Belgium | The Netherlands | |||
|---|---|---|---|---|
| Stakeholders | Type | Tasks | Type | Tasks |
| General practitioners | No tasks specified | Municipalities |
| |
| Hospitals | No tasks specified | Regional Public Health Services (RPHSs) |
| |
| Elderly care | No tasks specified | General practitioners |
| |
| Homecare | No tasks specified | Pharmacies |
| |
| Elderly care |
| |||
| Homecare |
| |||
| Non-Governmental Organisations |
| |||
| Country | Role in NHP | Organisation Name | Organisation Type | Familiarity with NHP | Role within NHP | Heat as a Public Health Priority | Involved in Warning the At-Risk Population | Successfulness in Reaching the Risk Population | Responsibilities Described in NHP | Collaboration between Stakeholders |
|---|---|---|---|---|---|---|---|---|---|---|
| The Netherlands | Activators | National Institute for Public Health and the Environment (RIVM) | National government | Yes | Plan development and activation, awareness through media, contact point for professionals | Medium | Yes (all risk groups) | Yes | No | Good |
| Dutch Red Cross (DRC) | NGO | Yes | Input on plan development, awareness through media (i.e., press releases), mobilisation of volunteers | High | Yes (high risk groups) | Partially | No | Partial (limited involvement in national heatwave plan development) | ||
| Intermediaries | Municipal Health Service Amsterdam (MHSA) | Regional government (public health) | Yes | Providing information and advice to professionals | High | Indirectly | Unknown | No | Partial (adequate communication with RIVM, more difficulties in communication with GPs) | |
| Municipality of Amsterdam (MoA) | Local government | Yes, but not with content | Care for certain vulnerable populations (homeless persons, drug users), contact point for general public | High | No | Not applicable | Not reported | Partial (collaboration with MHSA should be improved) | ||
| Care organisation | Academic Medical Centre (AMC) | Hospital | No | Not reported | Low | No response | No response | No response | Poor (lack of collaboration with other stakeholders) | |
| Cordaan | Elderly care and homecare | No | Care for certain vulnerable populations (e.g., elderly, young children, handicapped) | Medium | Yes (elderly, only at care centres) | Yes | Unknown | Poor (lack of collaboration with other stakeholders) |
| Country | Role in NHP | Organisation Name | Organisation Type | Familiarity with NHP | Role within NHP | Heat as a Public Health Priority | Involved in Warning the At-Risk Population | Successfulness in Reaching the Risk Population | Responsibilities Described in NHP | Collaboration between Stakeholders |
|---|---|---|---|---|---|---|---|---|---|---|
| Belgium | Activators | Public Service Wallonia (PSW) | Regional government | Yes | Input on plan development, providing information to professionals | Medium (health sector), High (social sector) | Indirectly | Yes | Yes | Good (social sector), Poor (health sector) |
| Leefmilieu Brussel (LB) | Regional government (environment and health) | Yes | Input on plan development, coordination of regional implementation | High | Indirectly | No | No | Good | ||
| FOD Public health, food safety and environment (FOD) | National government | Yes, but not with content | Commissioned the plan, awareness through media, contact point for professionals, providing advice to professionals | Medium | Yes (all risk groups) | Yes | No | Good | ||
| Intermediaries | Red Cross Brussels (RCB) | NGO | Yes, but not with content | Follow instructions from FOD, providing information to professionals | High | Indirectly | Yes | No | Partial (good collaboration on other issues than heat) | |
| Municipality of Etterbeek (MoE) | Local government | Yes | Coordination of local heatwave plan, awareness towards risk groups, contact point for general public, providing information to professionals | High | Yes (all risk groups) | Partially | No | Partial (lack of involvement of some stakeholders) | ||
| Municipality of Saintt-Gilles (MoS-G) | Local government | Yes | Coordination of local heatwave plan | Medium | Yes (elderly) | Yes | No | Partial (low awareness of responsibilities of other stakeholders) | ||
| Care organisation | Familiehulp | Homecare | No | Care for own employees | No response | No | Not applicable | No response | Poor (lack of collaboration with other stakeholders) |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Van Loenhout, J.A.F.; Rodriguez-Llanes, J.M.; Guha-Sapir, D. Stakeholders’ Perception on National Heatwave Plans and Their Local Implementation in Belgium and The Netherlands. Int. J. Environ. Res. Public Health 2016, 13, 1120. https://doi.org/10.3390/ijerph13111120
Van Loenhout JAF, Rodriguez-Llanes JM, Guha-Sapir D. Stakeholders’ Perception on National Heatwave Plans and Their Local Implementation in Belgium and The Netherlands. International Journal of Environmental Research and Public Health. 2016; 13(11):1120. https://doi.org/10.3390/ijerph13111120
Chicago/Turabian StyleVan Loenhout, Joris Adriaan Frank, Jose Manuel Rodriguez-Llanes, and Debarati Guha-Sapir. 2016. "Stakeholders’ Perception on National Heatwave Plans and Their Local Implementation in Belgium and The Netherlands" International Journal of Environmental Research and Public Health 13, no. 11: 1120. https://doi.org/10.3390/ijerph13111120
APA StyleVan Loenhout, J. A. F., Rodriguez-Llanes, J. M., & Guha-Sapir, D. (2016). Stakeholders’ Perception on National Heatwave Plans and Their Local Implementation in Belgium and The Netherlands. International Journal of Environmental Research and Public Health, 13(11), 1120. https://doi.org/10.3390/ijerph13111120






