The Association between Arrhythmia and Helicobacter pylori Infection: A Meta-Analysis of Case-Control Studies
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Sources and Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Quality Assessment and Data Extraction
2.4. Statistical Analysis
3. Results
3.1. Data Selection
3.2. Study Characteristics and Quality Assessment
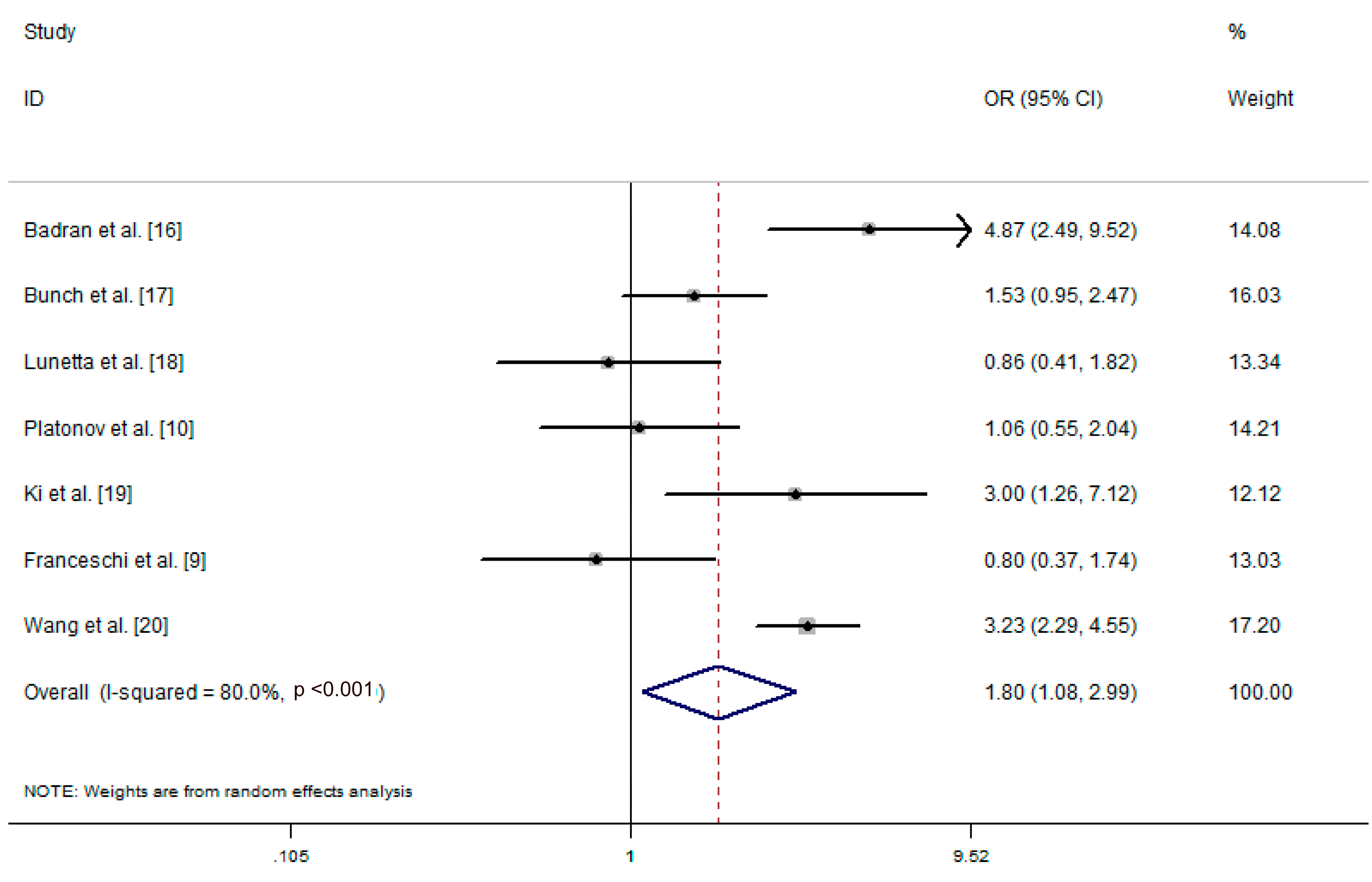
3.3. Data Analysis
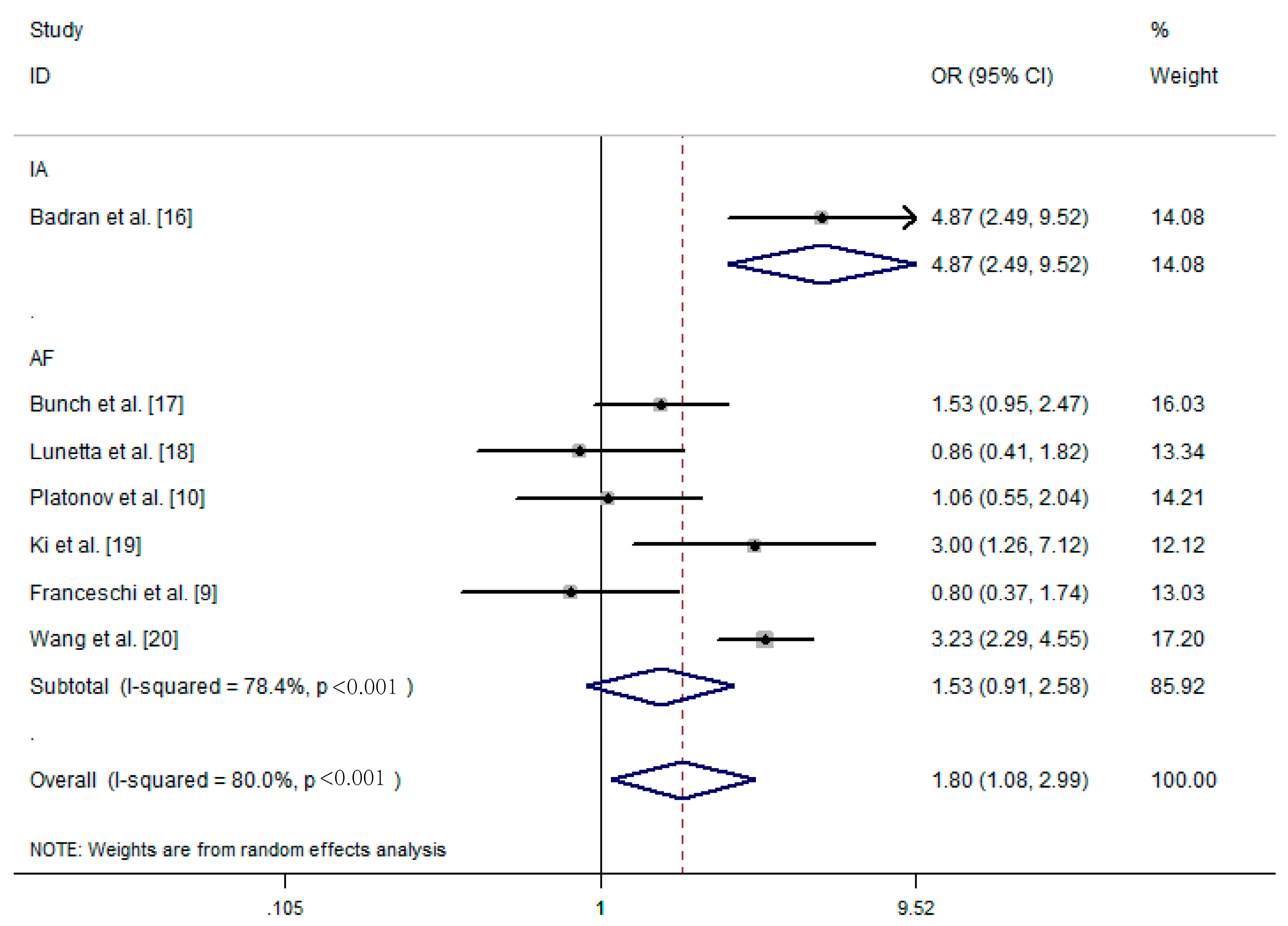
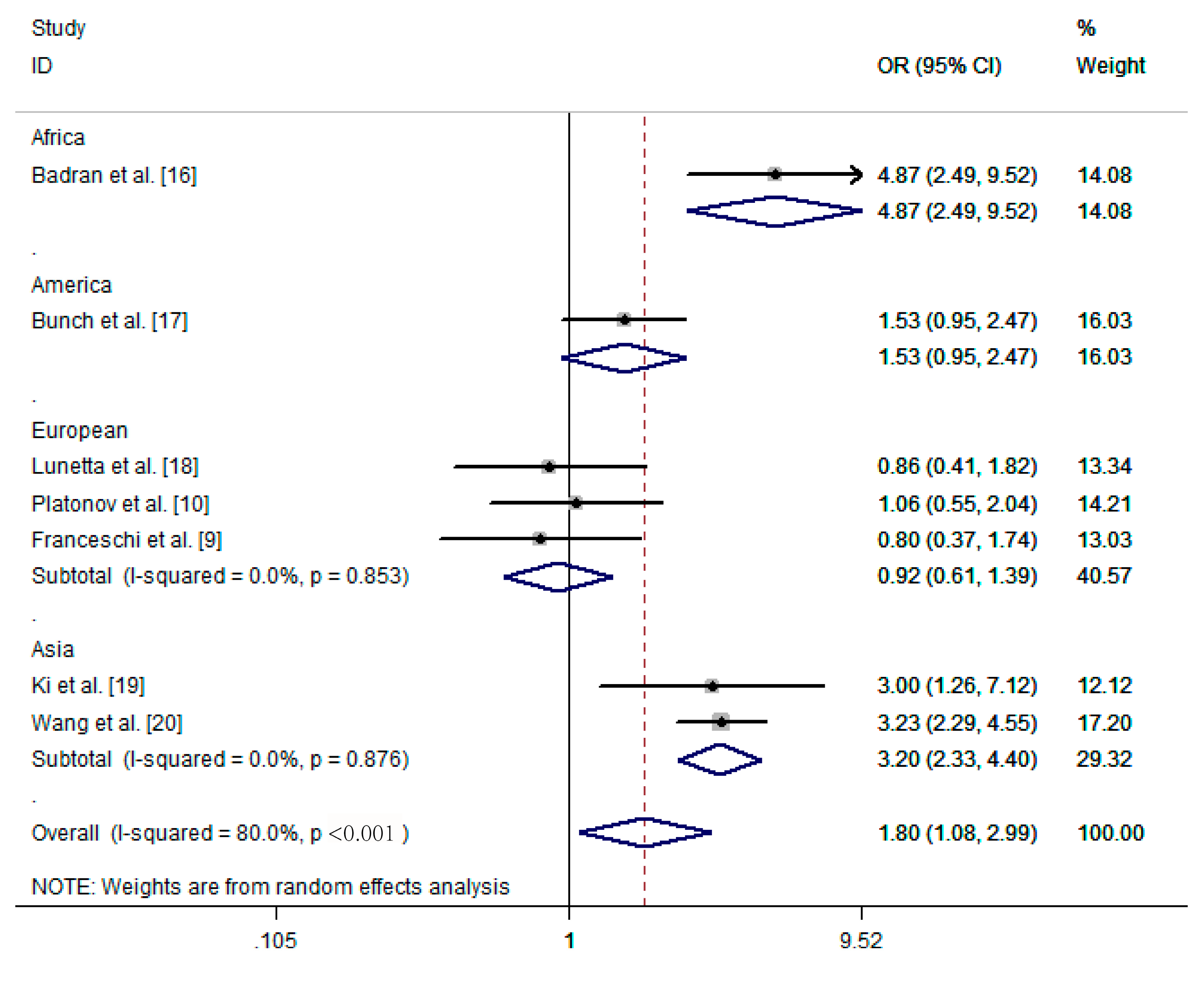
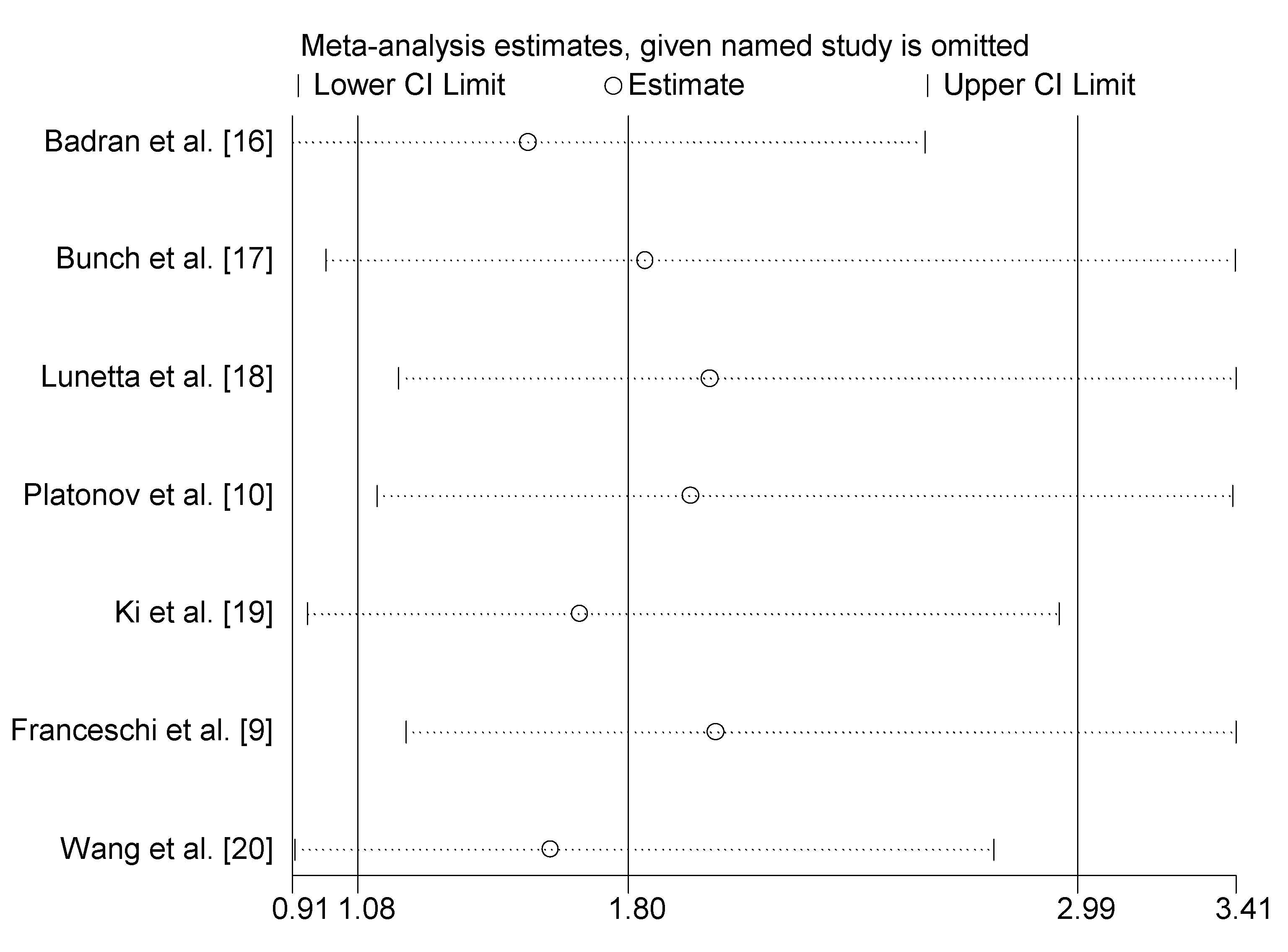
3.4. Subgroup Analysis and Sensitivity Analysis
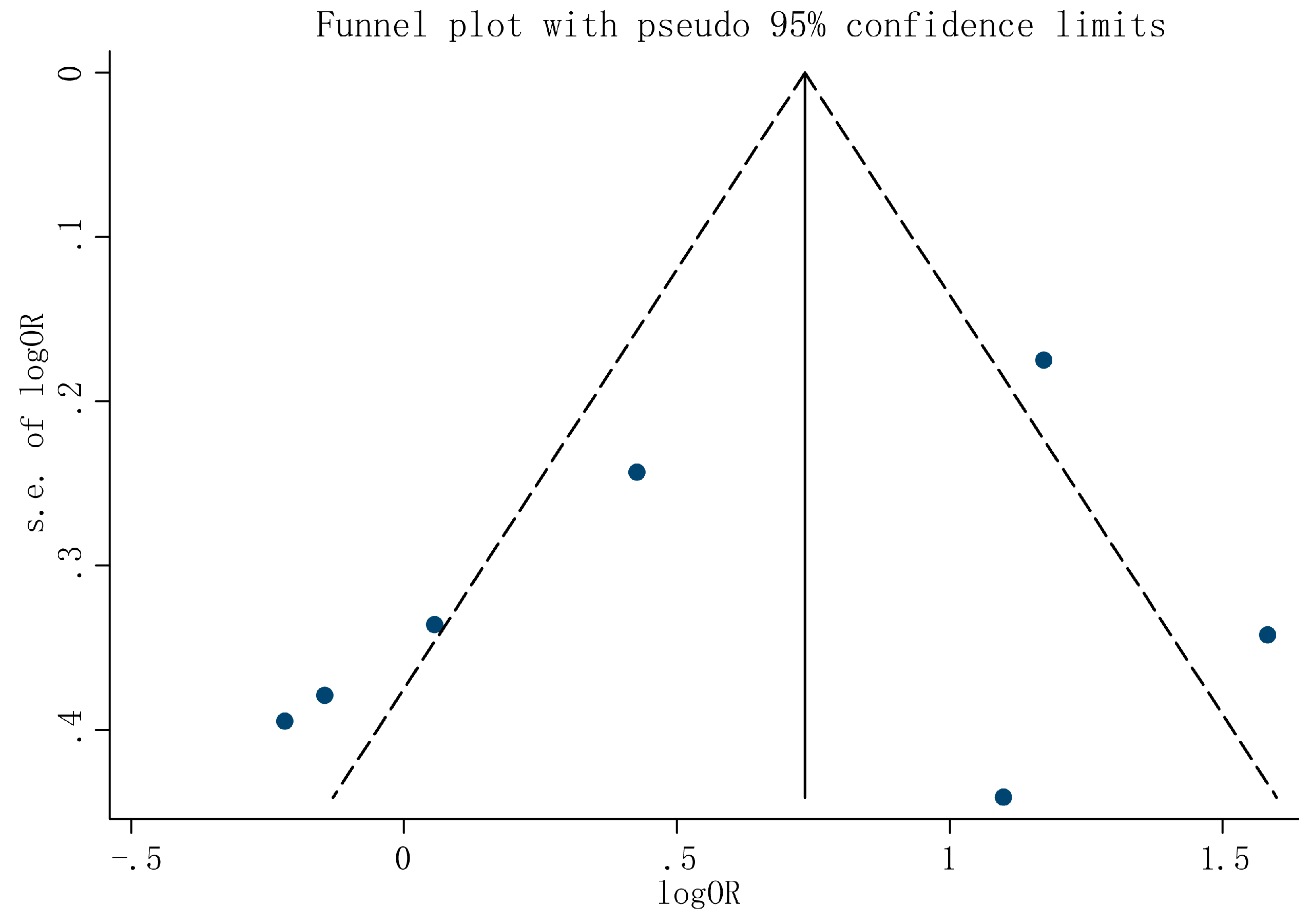
3.5. Publication Bias
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| AF | atrial fibrillation |
| CI | confidence interval |
| I | inconsistency index |
| IA | idiopathic dysrhythmias |
| NG | not given |
| NOS | Newcastle-Ottawa quality assessment scale |
| OR | odds ratio |
| UBT | urea breath test |
| VacA | vacuolating cytotoxin A |
References
- Tse, G. Mechanisms of cardiac arrhythmias. J. Arrhythm. 2016, 32, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Lip, G.Y.; Tse, H.F.; Lane, D.A. Atrial fibrillation. Lancet 2012, 379, 648–661. [Google Scholar] [CrossRef]
- Kapoor, J.R. Management of atrial fibrillation. Lancet 2007, 370, 1608. [Google Scholar] [CrossRef]
- Zysko, D.; Gajek, J.; Mazurek, W. The contribution of inflammatory process in pathogenesis and natural history of atrial fibrillation. Polski Merkur. Lek. Organ Polskiego Tow. Lek. 2005, 18, 227–228. [Google Scholar]
- Salama, N.R.; Hartung, M.L.; Muller, A. Life in the human stomach: Persistence strategies of the bacterial pathogen Helicobacter pylori. Nature reviews. Microbiology 2013, 11, 385–399. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.C.; Chiang, T.H.; Chou, C.K.; Tu, Y.K.; Liao, W.C.; Wu, M.S.; Graham, D.Y. Association between Helicobacter pylori eradication and gastric cancer incidence: A systematic review and meta-analysis. Gastroenterology 2016, 150, 1113.e5–1124.e5. [Google Scholar] [CrossRef] [PubMed]
- Amieva, M.; Peek, R.M., Jr. Pathobiology of Helicobacter pylori-induced gastric cancer. Gastroenterology 2016, 150, 64–78. [Google Scholar] [CrossRef] [PubMed]
- Montenero, A.S.; Mollichelli, N.; Zumbo, F.; Antonelli, A.; Dolci, A.; Barberis, M.; Sirolla, C.; Staine, T.; Fiocca, L.; Bruno, N.; et al. Helicobacter pylori and atrial fibrillation: A possible pathogenic link. Heart (Br. Card. Soc.) 2005, 91, 960–961. [Google Scholar] [CrossRef] [PubMed]
- Franceschi, F.; Brisinda, D.; Buccelletti, F.; Ruggieri, M.P.; Gasbarrini, A.; Sorbo, A.; Marsiliani, D.; Venuti, A.; Fenici, P.; Gasbarrini, G.; et al. Prevalence of virulent Helicobacter pylori strains in patients affected by idiopathic dysrhythmias. Intern. Emerg. Med. 2013, 8, 333–337. [Google Scholar] [CrossRef] [PubMed]
- Platonov, P.; Ekesbo, R.; Hansson, A.; Andsberg, E.; Meurling, C.J.; Nilsson, I.; Ljungh, A.; Wadstrom, T.; Olsson, S.B. Permanent atrial fibrillation in patients without structural heart disease is not associated with signs of infection by chlamydia pneumoniae and Helicobacter pylori. Acta Cardiol. 2008, 63, 479–484. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The prisma statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis of observational studies in epidemiology (moose) group. JAMA 2000, 283, 2008–2012. [Google Scholar] [CrossRef] [PubMed]
- Stang, A. Critical evaluation of the newcastle-ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Xiao, M.; Wang, Y.; Gao, Y. Association between Helicobacter pylori infection and pancreatic cancer development: A meta-analysis. PLoS ONE 2013, 8, e75559. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Okamoto, T.; Enomoto, K.; Sakashita, N.; Oyama, K.; Fujii, S.; Sawa, T.; Takeya, M.; Ogawa, H.; Yamabe, H.; et al. Potential association of helicobacter cinaedi with atrial arrhythmias and atherosclerosis. Microbiol. Immunol. 2012, 56, 145–154. [Google Scholar] [CrossRef] [PubMed]
- Badran, H.M.; Mahfouz, M.E. Cytotoxin-associated gene-a bearing strains of Helicobacter pylori and atrial fibrillation due to ischemic origin: Is there a link? Eur. J. Cardiovasc. Prev. Rehabil. 2007, 14, 518–520. [Google Scholar] [CrossRef] [PubMed]
- Bunch, T.J.; Day, J.D.; Anderson, J.L.; Horne, B.D.; Muhlestein, J.B.; Crandall, B.G.; Weiss, J.P.; Lappe, D.L.; Asirvatham, S.J. Frequency of Helicobacter pylori seropositivity and c-reactive protein increase in atrial fibrillation in patients undergoing coronary angiography. Am. J. Cardiol. 2008, 101, 848–851. [Google Scholar] [CrossRef] [PubMed]
- Lunetta, M.; Fazio, G.; Avena, V.; Corrado, E.; Loredana, S.; Arnone, E.; Novo, G.; Novo, S. Helicobacter pylori and atrial fibrillation: Absence of correlations. J. Cardiovasc. Med. 2009, 10, 4–5. [Google Scholar]
- Ki, M.R.; Shin, D.G.; Park, J.S.; Hong, K.S.; Hong, I.H.; Park, J.K.; Jeong, K.S. Frequency of vacuolating cytotoxin a (VacA)-positive Helicobacter pylori seropositivity and TGF-beta1 decrease in atrial fibrillation. Int. J. Cardiol. 2010, 145, 345–346. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.Z.; Chen, W.; Yang, S.; Wang, J.; Li, Q.; Fu, Q.; Li, S.J.; Chen, B.X. Helicobacter pylori infection in chinese patients with atrial fibrillation. Clin. Interv. Aging 2015, 10, 813–819. [Google Scholar] [CrossRef] [PubMed]
- MacArthur, C.G.; Tarin, D.; Goodwin, J.F.; Hallidie-Smith, K.A. The relationship of myocarditis to dilated cardiomyopathy. Eur. Heart J. 1984, 5, 1023–1035. [Google Scholar] [PubMed]
- Gesualdo, M.; Scicchitano, P.; Carbonara, S.; Ricci, G.; Principi, M.; Ierardi, E.; Di Leo, A.; Cortese, F.; Ciccone, M.M. The association between cardiac and gastrointestinal disorders: Causal or casual link? J. Cardiovasc. Med. 2016, 17, 330–338. [Google Scholar] [CrossRef] [PubMed]
- Manisty, C.; Roberts, Y.H.; Kaddoura, S. Cardiac manifestations and sequelae of gastrointestinal disorders. Br. J. Cardiol. 2009, 16, 175–180. [Google Scholar]
- Kao, C.Y.; Sheu, B.S.; Wu, J.J. Helicobacter pylori infection: An overview of bacterial virulence factors and pathogenesis. Biomed. J. 2016, 39, 14–23. [Google Scholar] [CrossRef] [PubMed]
- Lazzerini, P.E.; Capecchi, P.L.; Laghi-Pasini, F. Systemic inflammation and arrhythmic risk: Lessons from rheumatoid arthritis. Eur. Heart J. 2016. [Google Scholar] [CrossRef] [PubMed]
- Aukrust, P.; Yndestad, A.; Sandberg, W.J.; Gullestad, L.; Damas, J.K. T cells in coronary artery disease: Different effects of different T-cell subsets. J. Am. Coll. Cardiol. 2007, 50, 1459–1461. [Google Scholar] [CrossRef] [PubMed]
- Gebert, B.; Fischer, W.; Weiss, E.; Hoffmann, R.; Haas, R. Helicobacter pylori vacuolating cytotoxin inhibits T lymphocyte activation. Science 2003, 301, 1099–1102. [Google Scholar] [CrossRef] [PubMed]
- Robinson, K.; Kenefeck, R.; Pidgeon, E.L.; Shakib, S.; Patel, S.; Polson, R.J.; Zaitoun, A.M.; Atherton, J.C. Helicobacter pylori-induced peptic ulcer disease is associated with inadequate regulatory T cell responses. Gut 2008, 57, 1375–1385. [Google Scholar] [CrossRef] [PubMed]
- Myint, A.M.; Leonard, B.E.; Steinbusch, H.W.; Kim, Y.K. Th1, th2, and th3 cytokine alterations in major depression. J. Affect. Disord. 2005, 88, 167–173. [Google Scholar] [CrossRef] [PubMed]
- Nagy, P.; Johansson, S.; Molloy-Bland, M. Systematic review of time trends in the prevalence of Helicobacter pylori infection in china and the USA. Gut Pathog. 2016, 8, 8. [Google Scholar] [CrossRef] [PubMed]

| Author/Year | Country/Continent | Study Design | Study Size | Type of Arrhythmia | Diagnostic Method for H. pylori Infection | Arrhythmia Group with Hp (+/−) | Control Group with Hp (+/−) |
|---|---|---|---|---|---|---|---|
| Badran et al. [16] | Egypt/Africa | Case-control study | 162 | IA | Serum H. pylori IgG antibodies | 52/30 | 21/59 |
| Bunch et al. [17] | USA/America | Case-control study | 743 | AF | Serum H. pylori IgG antibodies | 54/29 | 362/298 |
| Lunetta et al. [18] | Italy/European | Case-control study | 180 | AF | Serum H. pylori IgG antibodies | 25/14 | 95/46 |
| Platonov et al. [10] | Sweden/European | Case-control study | 144 | AF | Serum H. pylori IgG antibodies | 41/31 | 40/32 |
| Ki et al. [19] | Korea/Asia | Case-control study | 96 | AF | Serum H. pylori IgG antibodies | 36/24 | 12/24 |
| Franceschi et al. [9] | Italy/European | Case-control study | 104 | AF | 13C urea breath test | 23/31 | 24/26 |
| Wang et al. [20] | China/Asia | Case-control study | 585 | AF | 13C urea breath test | 161/124 | 86/214 |
| Study | Selection | Comparability | Exposure | Scores | |||||
|---|---|---|---|---|---|---|---|---|---|
| Is the Case Definition Adequate | Representativeness of Cases | Selection of Controls | Definition of Controls | Comparability of Cases and Controls on the Basis of the Design or Analysis # | Ascertainment of Exposure | Same Method of Ascertainment for Cases and Controls | Non-Response Rate | ||
| Badran et al. [16] | * | * | * | * | ** | * | * | - | 8 |
| Bunch et al. [17] | * | * | * | * | - | * | * | - | 6 |
| Lunetta et al. [18] | * | * | * | * | ** | * | * | - | 8 |
| Platonov et al. [10] | * | * | * | * | ** | * | * | - | 8 |
| Ki et al. [19] | * | * | - | * | - | * | * | - | 5 |
| Franceschi et al. [9] | * | * | * | * | ** | * | * | - | 8 |
| Wang et al. [20] | * | * | * | * | ** | * | * | - | 8 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yan, J.; She, Q.; Zhang, Y.; Cui, C.; Zhang, G. The Association between Arrhythmia and Helicobacter pylori Infection: A Meta-Analysis of Case-Control Studies. Int. J. Environ. Res. Public Health 2016, 13, 1139. https://doi.org/10.3390/ijerph13111139
Yan J, She Q, Zhang Y, Cui C, Zhang G. The Association between Arrhythmia and Helicobacter pylori Infection: A Meta-Analysis of Case-Control Studies. International Journal of Environmental Research and Public Health. 2016; 13(11):1139. https://doi.org/10.3390/ijerph13111139
Chicago/Turabian StyleYan, Jin, Qiang She, Yifeng Zhang, Chang Cui, and Guoxin Zhang. 2016. "The Association between Arrhythmia and Helicobacter pylori Infection: A Meta-Analysis of Case-Control Studies" International Journal of Environmental Research and Public Health 13, no. 11: 1139. https://doi.org/10.3390/ijerph13111139
APA StyleYan, J., She, Q., Zhang, Y., Cui, C., & Zhang, G. (2016). The Association between Arrhythmia and Helicobacter pylori Infection: A Meta-Analysis of Case-Control Studies. International Journal of Environmental Research and Public Health, 13(11), 1139. https://doi.org/10.3390/ijerph13111139





